Abstract
Background
Serious mental illness is one of the leading causes of disability worldwide. Emerging mobile health (mHealth) and eHealth interventions may afford opportunities for reaching this at-risk group.
Aim
To review the evidence on using emerging mHealth and eHealth technologies among people with serious mental illness.
Methods
We searched MEDLINE, PsychINFO, CINAHL, Scopus, Cochrane Central, and Web of Science through July 2014. Only studies reporting outcomes for mHealth or eHealth interventions, defined as remotely delivered using mobile, online, or other devices, targeting people with schizophrenia, schizoaffective disorder, or bipolar disorder, were included.
Results
Forty-six studies spanning 12 countries were included. Interventions were grouped into four categories: 1) illness self-management and relapse prevention; 2) promoting adherence to medications and/or treatment; 3) psychoeducation, supporting recovery, and promoting health and wellness; and 4) symptom monitoring. The interventions were consistently found to be highly feasible and acceptable, though clinical outcomes were variable but offered insight regarding potential effectiveness.
Conclusions
Our findings confirm the feasibility and acceptability of emerging mHealth and eHealth interventions among people with serious mental illness; however, it is not possible to draw conclusions regarding effectiveness. Further rigorous investigation is warranted to establish effectiveness and cost benefit in this population.
Keywords: mobile health, mhealth, ehealth, serious mental illness, mental health, remote technology
Introduction
Serious mental illness (SMI), including schizophrenia, schizoaffective disorder, and bipolar disorder, is one of the leading causes of disability worldwide (Kessler et al., 2009). Compared to the general population, people with SMI are disproportionately affected by comorbid medical conditions, increased cardiovascular risk, poor health behaviors, and socioeconomic concerns such as homelessness, unemployment, and poverty, contributing to significantly reduced life expectancy (Druss et al., 2011). People with SMI also experience functional impairment, social isolation, and negative symptoms such as anxiety, depression, low motivation, and cognitive impairment (Kessler et al., 2003). These symptoms affect their ability to engage in illness self-management or access community resources (Fagiolini & Goracci, 2009), and contribute to increased risk of suicide (Pompili et al., 2008) and elevated rates of hospital admissions and acute care use (Simone et al., 2013). These concerns are further exacerbated because people with SMI often receive inadequate and highly variable health care (Druss et al., 2002), and face barriers to preventive and routine services (Dickerson et al., 2003). Innovative approaches for illness self-management, treatment, and symptom monitoring are urgently needed to address the poor health and medical care experienced by people with SMI.
The use of technology such as telepsychiatry, telephone support services, or videoconferencing between patients and mental health providers has been used to address gaps in mental health services and improve patient outcomes (Hailey et al., 2008; Hilty et al., 2013). However, these approaches are limited by the necessary involvement of costly providers for direct telephone consultation. They also do little to address daily lifestyle behaviors that are more likely to be improved through continuous monitoring, self-help and skill building, and symptom management over time (Bauer & Moessner, 2012). In contrast, emerging mobile health (mHealth) and eHealth interventions, including mobile, online, and other remote devices such as monitoring systems or wearable technologies, have the advantage of reaching at-risk individuals at any time or place without relying on costly mental health providers, and they may afford opportunities for reaching people with SMI.
There remains uncertainty about whether emerging mHealth and eHealth interventions are suitable for reaching individuals with SMI. For instance, concerns have been raised about the usability and acceptability of web-based or mobile applications given the cognitive limitations and social challenges faced by many people with SMI. Web-based platforms for the general public are believed to have poor usability among persons with SMI (Rotondi et al., 2013), as evidenced by difficulties experienced by this patient population when navigating smoking cessation websites (Brunette et al., 2012). To address concerns related to usability, many technology-based interventions are specifically developed for people with SMI by incorporating simple visual interfaces, using familiar phrasing and content presented at a low reading level, and avoiding tasks requiring abstract reasoning (Ben-Zeev, Kaiser, et al., 2013).
Socioeconomic disadvantages are also a barrier to using emerging technology interventions. Until recently, Internet use among people with SMI has been low, (Borzekowski et al., 2009); however, increasing availability and use of mobile devices and online services has been observed in this population group. A survey of low-income individuals with SMI found that over 70% owned cellphones, of which one third used their devices to access the Internet (Ben-Zeev, Davis, et al., 2013). Also, evidence suggests that individuals with SMI are more likely to share personal views through blogging, build friendships on social media (Gowen et al., 2012), and use the Internet for accessing health information (Berger et al., 2005) than people without mental illness.
A growing number of studies have explored the feasibility and potential effectiveness of mobile and web-delivered interventions among people with psychotic disorders as highlighted in recent reviews of emerging technologies for delivering treatment (Alvarez-Jimenez et al., 2014) and supporting illness self-management (van der Krieke et al., 2014). It is not clear from the current evidence whether these technologies are equally feasible across SMI diagnoses. In addition, many prior review articles have included telehealth interventions involving direct interaction with mental health providers through telepsychiatry, videoconferencing, or other technology-assisted communication tools (Hilty et al., 2013), or they have included articles published only within a limited time frame (Lal & Adair, 2014).
Our objective was to expand on prior reviews of the literature and assess the feasibility and acceptability of remotely delivered mHealth and eHealth interventions targeting a sample of participants that is more representative diagnostically of people with SMI served in public sector mental health settings, which includes diagnoses of schizophrenia, schizoaffective disorder, and bipolar disorder. In the current review we explored the use of remotely delivered mHealth and eHealth interventions among individuals with SMI for broad application, including symptom monitoring and assessment, promoting illness self-management, delivering psychoeducation, and supporting positive health behavior change.
METHODS
Search Strategy
We searched the following databases through July 2014: MEDLINE, PsychINFO, CINAHL, Scopus, Cochrane Central, and Web of Science. We used the terms schizophrenia, psychotic disorder, psychosis, bipolar disorder, mood disorder, bipolar, schizoaffective, severe mental illness, and serious mental illness. These terms were combined with telemetry, telemedicine, telepsychiatry, telehealth, telecare, telemental health, ehealth, mhealth, mobile health, mobile, mobile technology, mobile phone, smartphone, cellular phone, cellphone, text messaging, text message, SMS, internet health, internet, online, social media, website, web-based, web browser, remote consultation, remote sensing, artificial intelligence, game theory, user-computer interface, computer simulation, speech recognition software, computer-assisted therapy, wireless technology, and remote sensing technology. Each term was entered as a key word and corresponding medical subject heading (MeSH) term. No language limits were applied. We screened reference lists of included studies for additional relevant articles and searched Google Scholar using the same terms to identify relevant articles missed in our initial database search.
Study Selection Criteria
We only considered studies for inclusion that had participants with a serious mental illness, defined in this review as schizophrenia, schizoaffective disorder, psychosis, or bipolar disorder. Participant diagnoses were reported in the study methods, and could include self-reported diagnosis to include studies that used web-based recruitment strategies. Studies had a minimum of 10 participants. Studies must have evaluated a mHealth or eHealth technology-based intervention delivered remotely, which included remote monitoring, online interventions such as forums or Internet support groups, mobile phone-based interventions such as smartphone applications, personal digital assistants (PDA), or short message service (SMS) interventions, and other remotely delivered devices for monitoring or tracking health related outcomes.
Interventions were also user-led and not dependent entirely on clinician delivery. Clinician-led interventions were excluded because we were interested in the feasibility and acceptability of remote interventions that do not rely on costly providers. Therefore we excluded telepsychiatry interventions (e.g., consultation over the phone, videoconference), face-to-face interventions delivered in clinical or research settings, in-person interventions delivered by mental health providers, or interventions supervised by a clinician or researcher. All study designs were included, but reporting of outcomes was necessary. Outcomes were broadly defined and ranged from feasibility, acceptability, safety, and usability, to efficacy and effectiveness. Design studies, research protocols, theoretical articles, and discussion articles were also excluded.
Data Extraction and Analysis
We extracted the following characteristics from included studies: country of origin, study design, sample size, sample diagnoses, study duration, intervention description, and main outcomes. Interventions were grouped according to their primary purpose. Four broad categories were created: 1) illness self-management and relapse prevention; 2) promoting adherence to medications and/or treatment; 3) delivering psychoeducation, supporting recovery, and promoting health and wellness; and 4) symptom monitoring. The lead author reviewed all of the abstracts and screened the full-text articles. Then, all authors reviewed the reasons for study exclusion and the findings from included studies independently and as a group to ensure that all inclusion criteria were met and to summarize the evidence and to reach consensus on a list of key findings to inform future research targeting people with SMI.
Results
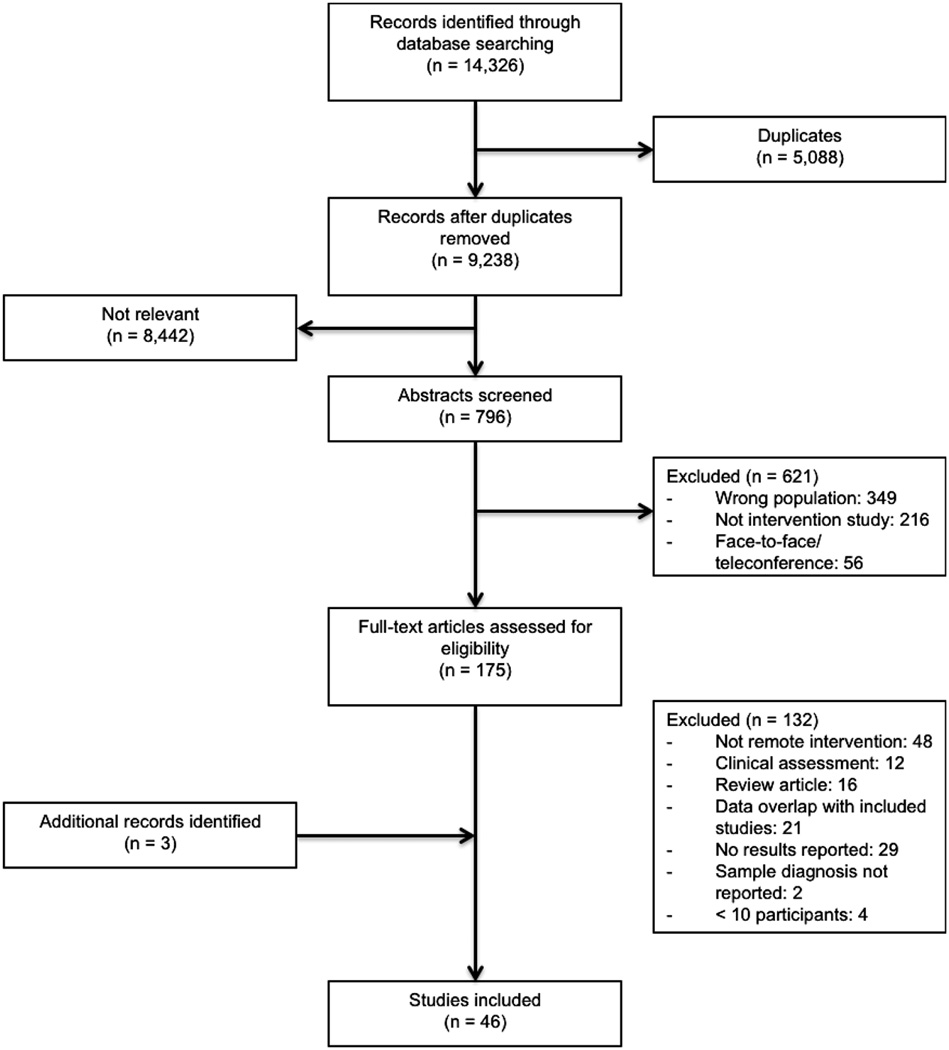
Our initial database search yielded over 9,000 articles after removal of duplicates, of which 796 were relevant and a careful review of the abstracts was necessary. Of the 175 full-text articles screened, 43 were included and 3 additional articles were retrieved through searching reference lists and Google Scholar. Figure 1 illustrates the database search results, abstract screening, reasons for study exclusion, and final study selection.
Figure 1.
The final 46 studies described 38 unique interventions or replication studies of previously described interventions, spanning 12 countries (Australia, Austria, Canada, Czech Republic, Denmark, Japan, Netherlands, Niger, Slovakia, Spain, United Kingdom, and United States). Of the different interventions, 45% targeted individuals with schizophrenia, schizoaffective disorder, or psychosis, 31% targeted individuals with bipolar disorder, and 24% targeted either individuals with schizophrenia spectrum disorders or bipolar disorder. Mobile interventions using smartphones, SMS, or PDAs were most common (50%), followed by non-mobile web delivered services (32%), as highlighted in Figure 2. We made the distinction between mobile versus non-mobile web-based interventions, because mobile platforms could be used to deliver online programs. The different interventions ranged in duration from 1 week to 1 year, though feasibility and acceptability did not appear to differ according to study duration.
Figure 2.

The methodological quality of included studies varied considerably, as evidenced by the range of study designs, differing analytic approaches such as intent-to-treat or as-treated analyses, and small samples sizes. We decided that all studies, even those of poorer methodological quality, offer important insights into broadly understanding the feasibility and acceptability of mHealth and eHealth interventions for SMI, and for informing future research. Therefore, all studies that met the inclusion criteria were included in synthesizing and interpreting the findings and were arranged into four broad categories as depicted in Tables 1–4 (studies are organized alphabetically by study author in each table).
Table 1.
Summary of remote technology intervention studies for illness self-management and relapse prevention in persons with SMI
| Study | Origin | Design | N | Diagnosis | Study Duration |
Intervention | Main Feasibility and Acceptability Findings |
|---|---|---|---|---|---|---|---|
| Ben-Zeev et al., (2014) | United States | Pre-post | 33 | Schizophrenia; schizoaffective disorder |
4 weeks | FOCUS smartphone intervention provides automated real-time illness management support to facilitate symptom management, mood regulation, medication adherence, social functioning, and improved sleep. |
Majority of participants found FOCUS feasible (n=32 used it 86.5% of time) and acceptable. Significant reductions in general psychopathology symptoms, positive symptoms of schizophrenia, and depression. |
| Godleski et al., (2012) | United States | Pre-post | 76 | Schizophrenia | 6 months | Health Buddy automated home messaging device presents disease management content for rating symptoms, providing alerts, and illness information. Responses monitored remotely by a nurse practitioner each day. |
46 participants used device 5–7 times per week; 20 used device 1–4 times per week. Significant decreases in hospital admissions and emergency room visits compared to 6-months prior to enrolment. 54% very satisfied with device. |
| Granholm et al., (2012) | United States | Pre-post | 55 | Schizophrenia; schizoaffective disorder |
12 weeks | MATS SMS intervention targets medication adherence, socialization, or hallucinations and uses individualized messages with branching logic according to participant responses. |
Completers (n=42) had 86% response rate. Significant improvement in medication adherence, increases in social interactions, and reduction in severity of hallucinations. |
| Kasckow et al., (2011) | United States | Pilot RCT | 38 | Schizophrenia; schizoaffective disorder |
3 months | Intensive case management and Health Buddy automated home messaging device with content for depressive and suicidal symptoms monitored 24/7 by a nurse. Compared to intensive case management only control group. |
Adherence to the device was over 80%, 15 of 19 used device regularly. Significant decrease in suicidal ideation. Feasible for monitoring post-discharge suicide risk. |
| Komatsu et al., (2013) | Japan | RCT | 45 | Schizophrenia | 12 months | ITAREPS is a SMS intervention that identifies symptoms of relapse to enable early intervention by notifying the care team and prevent hospitalization. Compared to usual care control group. |
ITAREPS resulted in significant decreases in risk of rehospitalization and a lower number of inpatient days compared to control group. |
| Pratt et al., (2014) | United States | Pre-post | 38 | Schizophrenia; schizoaffective disorder; bipolar disorder |
6 months | Health Buddy automated home messaging device for managing psychiatric instability with remote nurse monitoring. |
Significant decrease in hospital admissions and emergency room visits. Significant improvements in psychiatric symptoms, illness self-management skills, quality of life, depressive symptoms, and mental health status were also observed. |
| Pratt et al., (2013) | United States | Pre-post | 70 | Schizophrenia; bipolar disorder |
6 months | Health Buddy automated home messaging device programmed with content for managing both psychiatric and medical illnesses (such as diabetes and COPD) with remote nurse monitoring. |
Most (89%) participated in ≥ 70% of daily sessions. Significant improvements for managing depression and diastolic blood pressure, and understanding medical conditions. Fewer urgent and primary care visits observed in some participants. |
|
Spaniel et al., (2008) and (2008) |
Czech Republic |
Pre-post | 73 | Schizophrenia; schizoaffective disorder; psychotic disorder |
1 year | ITAREPS is a SMS intervention for remote monitoring and disease management that identifies symptoms of relapse to enable early intervention by notifying the care team and prevent hospitalization. |
ITAREPS resulted in significant reduction in hospitalizations and number of hospital days. Non- hospitalized participants adhered to the ITAREPS program more than participants who were hospitalized. |
| Spaniel et al., (2012) | Czech Republic & Slovakia |
RCT | 146 | Schizophrenia; schizoaffective disorder |
12 months | ITAREPS was used to detect early warning signs of relapse and prompt clinicians to respond through early pharmacological intervention. Compared to ITAREPS without clinician prompting control group. |
No between-group differences in hospitalizations. High non-adherence among clinicians who were prompted by ITAREPS to provide pharmacological intervention. As-treated analysis showed significant decreases in hospitalizations. |
| Todd et al., (2014) | United Kingdom |
RCT | 122 | Bipolar disorder | 6 months | Living with Bipolar (LWB) web-based self- management intervention includes education, supports recovery, and provides motivational email support. Compared to wait-list control group. |
Feasibility demonstrated by high rates of recruitment and retention. Significant improvements in quality of life, wellbeing, depression, social function and recovery in LWB compared to wait-list control. |
Table 4.
Summary of remote technology intervention studies for symptom monitoring in persons with SMI
| Study | Origin | Design | N | Diagnosis | Study Duration |
Intervention | Main Feasibility and Acceptability Findings |
|---|---|---|---|---|---|---|---|
| Ainsworth et al., (2013) | United Kingdom |
Cross-over RCT |
24 | Schizophrenia; schizoaffective disorder |
3 weeks | Diagnostic assessment of symptoms delivered through a smartphone application compared to SMS text messaging. |
The smartphone application allowed participants to complete significantly more data points and took less time. No differences in feedback for each modality. |
| Bauer et al., (2004) | United States; Canada |
Single arm prospective study |
96 | Bipolar disorder | 3 months | Participants use the ChronoRecord computer- based system to record mood, medications, sleep, life events, and menstrual data daily and weight weekly. |
Participants showed high acceptance of the program, and 83% (N=80) returned 8662 days of data, mean of 114.7 (SD=9.3) days. Self-reported ratings were strongly correlated with clinician ratings. |
| Ben-Zeev et al., (2012) | United States | Single arm prospective study |
24 | Schizophrenia | 1 week | Ecological Momentary Assessment via PDAs to track self-stigma, psychotic symptoms, negative affect, positive affect, activity, and social and physical environment multiple times daily. |
Participants’ activity was associated with self-stigma, and increases in negative affect and psychotic symptom severity predicted greater self-stigma. Complete data for 88% of the observations. Mobile technologies emerged as effective for monitoring self- stigma. |
| Bopp et al., (2010) | United Kingdom |
Single arm prospective study |
62 | Bipolar disorder | 36 weeks | Participants provided mood ratings in response to weekly SMS text messages or email prompts to track trajectory of symptom ratings. |
Adherence was 75%. Participants reported depressive symptoms (47.7%), manic symptoms (7%), both depressive and manic symptoms (8.8%), and euthymic mood (36.5%). SMS-based symptom monitoring was acceptable. |
| Depp et al., (2012) | United States | Pilot RCT | 40 | Bipolar disorder | 12 weeks | Mobile survey of momentary mood and symptoms delivered twice daily on a smartphone compared to paper-and-pencil mood charts completed daily. |
Mobile phones were associated with lower compliance, but greater ability to capture variability and clinical validity in symptom ratings compared to paper-and-pencil. |
| Faurholt-Jepsen et al., (2014) | Denmark | Uncontrolled pilot study |
17 | Bipolar disorder | 3 months | MONARCA Android smartphone application prompted participants to self-monitor mood, symptoms, and other activities each evening, and objective activities such as speech duration, social activity, and physical activity each day. |
Objective smartphone measures of physical and social activity correlated with depressive symptoms. Self-monitored depressive symptoms correlated with clinician ratings. |
| Grunerbl et al., (2012) | Austria | Uncontrolled pilot study |
10 | Bipolar disorder | 8 weeks | Android smartphone application collects data continuously on location and movement, level of activity, and social interaction, and prompts participants to answer questions about activities of daily living, psychological state, physical state, and amount of activity each day. |
Feasible to use smartphone sensors for remotely gathering behavioral data on participants with bipolar disorder. |
|
Lieberman et al., (2011) and (2010) |
United States | Single arm prospective study |
64 | Bipolar disorder | 90 days | MoodChart is an automated Internet-based program that provides social rhythm therapy by prompting participants daily to rate mood, anxiety, and depression, and to record daily activities. |
Adherence to rating was high. Social rhythm stability increased by 31% and decreased symptoms of abnormal mood. |
|
Palmier-Claus et al., (2012), (2013), (2013), and (2014) |
United Kingdom |
Single arm prospective study |
44 | Schizophrenia; schizoaffective disorder; |
1 week | ClinTouch is an Android smartphone application that prompts participants to complete self-reported assessment of psychotic and other symptoms 6 times daily. |
Ambulatory monitoring several times daily emerged as feasible for symptom assessment. 82% of participants completed at least 33% of possible assessments. Several measures collected by ClinTouch including hopelessness, delusions, anxiety, and depression were correlated with clinical assessments supporting the validity of this approach. |
1) Illness self-management and relapse prevention
Eleven studies focused on illness self-management and relapse prevention (see Table 1). Among these were 4 modified versions of the Health Buddy automated home messaging device delivered across diverse mental health settings (Godleski et al., 2012; Kasckow et al., 2011; Pratt et al., 2013; Pratt et al., 2014), 3 separate evaluations of the Information Technology Aided Relapse Prevention Programme in Schizophrenia (ITAREPS) (Komatsu et al., 2013; Spaniel et al., 2012; Spaniel, Vohlidka, Hrdlicka, et al., 2008; Spaniel, Vohlidka, Kozeny, et al., 2008), and a trial of an online platform for self-managing bipolar disorder (Todd et al., 2014). Measures of feasibility and acceptability included frequency of intervention use over time, response rates, study retention, proportion of devices that were returned undamaged, and participant reported usability (see Table 1). Important clinical outcomes were also reported. For example, the Health Buddy automated home messaging device appeared to decrease hospital admissions and emergency room visits (Godleski et al., 2012; Pratt et al., 2014), while reductions in mental health severity were observed in studies of mobile interventions targeting symptom management in schizophrenia (Ben-Zeev et al., 2014; Granholm et al., 2012).
2) Promoting adherence to medications and/or treatment
Eight studies were aimed at promoting adherence to medications and/or treatment (see Table 2). Four of these studies described SMS interventions for providing automated text message reminders to take medications or to attend appointments with mental health providers (Beebe et al., 2014; Maiga, 2011; Montes et al., 2012; Sims et al., 2012). These SMS studies did not emphasize feasibility outcomes, and instead reported improvement in adherence or attendance outcomes, which may reflect the established use of SMS as a strategy for promoting adherence. One study (published in French) described a SMS appointment reminder intervention targeting individuals with psychosis seen at the national hospital in Niamey, Niger (Maiga, 2011). This intervention resulted in better attendance compared to the control group, and was the only study from a low-income country. Of the 4 remaining studies, two used electronic medication bottle caps that record each bottle opening to monitor medication adherence (Acosta et al., 2009; Frangou et al., 2005), one involved ingestible digital tablets tracked using a wearable sensor (Kane et al., 2013), and one was a PDA delivered intervention for improving treatment adherence in bipolar disorder (Wenze et al., 2014). In these studies, feasibility and acceptability were measured through qualitative interviews with patients and health professionals, study completion and adherence rates, and frequency of intervention use (see Table 2).
Table 2.
Summary of remote technology intervention studies for promoting adherence to medications and/or treatment in persons with SMI
| Study | Origin | Design | N | Diagnosis | Study Duration |
Intervention | Main Feasibility and Acceptability Findings |
|---|---|---|---|---|---|---|---|
| Acosta et al., (2009) | Spain | Single arm prospective study |
79 | Schizophrenia | 3 months | Medication Event Monitoring System (MEMS) is an electronic medication bottle cap that records each bottle opening to assess compliance with oral antipsychotic treatments. |
There were 18 noncompliant and 56 compliant participants. Noncompliant participants had worse symptoms, but did not differ on sociodemographic characteristics compared to compliant participants. The psychiatrist, patients and relatives overestimated treatment adherence compared to MEMS. |
| Beebe et al., (2014) | United States | Pilot RCT | 30 | Schizophrenia; schizoaffective disorder |
3 months | Participants were randomized to daily text messages, weekly telephone calls, or both, targeting symptoms and medication adherence. |
Symptom scores were lowest among the combined text message and telephone call group, but scores differed significantly at baseline. No differences in adherence. |
| Frangou et al., (2005) | United Kingdom |
RCT | 108 | Schizophrenia | 8 weeks | @HOME remote monitoring platform uses electronic medication bottle caps to record bottle openings and alert clinicians about nonadherence. @HOME was compared with self-reported adherence and pill counting control groups. |
@HOME contributed to significantly greater medication adherence, improved clinical rating, and significant decreases in emergency visits and medical appointments. @HOME was feasible and acceptable to patients and providers. |
| Kane et al., (2013) | United States | Single arm prospective study |
28 | Bipolar disorder; schizophrenia |
4 weeks | Digital Health Feedback System (DHFS) includes digital tablets with ingestion sensors linked to a wearable sensor on the torso to monitor medication adherence. Wearable sensor also collects activity, sleep and heart rate. |
DHFS emerged as feasible for monitoring medication adherence and physiologic measures. 89% of participants found DHFS useful. |
| Maiga (2011) | Niger | RCT | 100 | Psychosis | 4 months | The intervention group received reminder SMS text messages and phone calls 2 days before monthly follow-up appointments. The control group received no appointment reminders. |
The intervention group attended significantly more monthly follow-up visits than the control group. |
| Montes et al., (2012) | Spain | RCT | 340 | Schizophrenia | 6 months | The intervention group received automated daily SMS reminders to take their medication for 3 months. The control group received no SMS reminders. |
86 participants excluded from the analysis due to study protocol deviations or incorrect use of the SMS intervention. Among 254 participants included in the final analysis, the 100 who received SMS reminders had significant improvement in medication adherence at 3 and 6 month follow up. |
| Sims et al., (2012) | United Kingdom |
Controlled study |
1,256 | Schizophrenia spectrum; mood or affective; |
3.5 months | SMS reminders to attend appointments across 4 community mental health centers. Reminders were sent 7 and 5 days prior, or 7 and 3 days prior. Comparison group received no reminders. |
There were 2,817 appointments for 1,256 participants. Attendance was significantly higher among intervention participants. |
| Wenze et al., (2014) | United States | Uncontrolled pilot study |
14 | Bipolar spectrum disorders |
2 weeks | Ecological momentary intervention (EMI) consisting of 2 sessions delivered daily via PDAs to improve treatment adherence. Participants answer questions about appointments, medications, adherence behaviors, and other concerns related to treatment, symptoms and suicidal ideation. |
Participants completed 92% of EMI sessions. EMI emerged as feasible and acceptable, participants found the sessions useful, and depression scores decreased significantly. |
3) Psychoeducation, supporting recovery, and promoting health and wellness
Fourteen studies described 11 different interventions for psychoeducation, supporting recovery, or promoting health and wellness (see Table 3). Many of these interventions were web-based and involved education, developing coping skills, and providing social support. For example, two online education interventions focused on developing parenting skills for parents with SMI (Jones et al., 2014; Kaplan et al., 2014), while four online interventions included a peer component such as peer-to-peer online social networking (Alvarez-Jimenez et al., 2013; Gleeson et al., 2014), peer support (Kaplan et al., 2011), or peer coaching (Simon et al., 2011). One study focused on promoting physical activity using wearable activity tracking devices linked to smartphones (Naslund et al., 2015). Feasibility and acceptability were measured by the frequency of intervention use, attrition rates from the intervention groups, and whether there were concerns related to privacy with using the devices (see Table 3). Few studies included clinical or health outcomes other than measures of illness symptoms (Rotondi et al., 2010; Rotondi et al., 2005), depression (Alvarez-Jimenez et al., 2013; Baikie et al., 2012; Proudfoot et al., 2012), distress (Kaplan et al., 2011), quality of life (Poole et al., 2012; Smith et al., 2011), or ability to reach goals (Pijnenborg et al., 2010), likely reflecting that the data collection was conducted online in several of these studies and was limited to self-report.
Table 3.
Summary of remote technology intervention studies for psychoeducation, supporting recovery, and promoting health and wellness in persons with SMI
| Study | Origin | Design | N | Diagnosis | Study Duration |
Intervention | Main Feasibility and Acceptability Findings |
|---|---|---|---|---|---|---|---|
|
Alvarez-Jimenez et al., (2013); Gleeson et al., (2014) |
Australia | Uncontrolled pilot study |
20 | First episode psychotic disorder or mood disorder |
1 month | HORYZONS online platform includes psychosocial interventions targeting risk factors for relapse, peer-to-peer online social networking, and expert moderation. |
60% of participants used HORYZONS, 70% used it for at least 3 weeks, and 95% used the peer-to-peer social networking component. Depressive symptoms significantly decreased. No clinical, privacy or security concerns emerged. |
| Baikie et al., (2012) | Australia | RCT | 848 | Bipolar disorder; schizoaffective disorder |
4 months | Participants randomized to expressive writing (share and explore deepest thoughts and emotions), positive writing (share most positive experience), or control writing (generic topic). |
High attrition (74%) partly due to concerns about sharing traumatic experiences. No differences between groups. Decreased depression and improved mental health symptoms across all groups. |
| Jones et al., (2014) | United Kingdom |
Pilot RCT | 39 | Bipolar disorder | 10 weeks | Web-based self-directed parenting intervention for bipolar parents provides instruction for managing child behavior. Compared to waitlist control. |
High attrition in the intervention group (42% completed). Significant improvement in child behavior and perceived parenting measures. |
| Kaplan et al., (2014) | United States | RCT | 60 | Schizophrenia spectrum disorder; affective disorder |
3 months | Web-based education and social support intervention designed to enhance parenting skills, improve coping skills and decrease parental stress for mothers with SMI. Compared to an online healthy lifestyle intervention. |
Intervention enhanced parenting skills, improved coping skills, and decreased parental stress. No improvement in efficacy or support. Mothers with SMI are interested and capable of receiving online parenting education and support. |
| Kaplan et al., (2011) | United States | RCT | 300 | Schizophrenia spectrum disorder; affective disorder |
12 months | Intervention with unmoderated, unstructured Internet peer support. Participants randomized to experimental Internet peer support via a listserv; experimental Internet peer support via a bulletin board; or a waitlist control condition. |
No differences between groups for recovery, quality of life, empowerment, social support, and distress. Greater participation in Internet peer support resulted in higher levels of distress; positive experiences with Internet peer support associated with more distress. |
| Naslund et al., (2014) | United States | Uncontrolled pilot study |
10 | Schizophrenia; bipolar disorder |
5 months | Wearable activity monitoring devices (FitBit Zip or Nike FuelBand) and Apple iPhone 4S smartphones to access the mobile application for these devices. |
Participants wore the devices 89% of the days enrolled in the study and reported high satisfaction. Shows feasibility and acceptability. |
| Pijnenborg et al., (2010) | Netherlands | Controlled trial |
62 | Schizophrenia; schizoaffective disorder; psychotic disorder |
18 weeks | Automated SMS text message prompts to support daily goals and functioning, taking medication, attending mental health care appointments, or grocery shopping. Compared to a waitlist control. |
Percentage of goals achieved was greater in the intervention group, but decreased after withdrawing the SMS prompts. Keeping appointments and participating in leisure activities increased with prompts, but no change in medication adherence. |
| Proudfoot et al., (2012) | Australia | RCT | 407 | Bipolar disorder | 8 weeks | Participants randomized to: online Bipolar Education Program (BEP) aimed at providing education and skill building; BEP enhanced with email support from peers; or a control condition consisting of basic facts about bipolar disorder. |
No differences between groups. Increased perceptions of control, decreased perceptions of stigmatization, and improvements in anxiety and depression across all groups. Higher adherence to BEP with peer support compared to BEP alone. |
|
Rotondi et al., (2010) and (2005) |
United States | RCT | 31* | Schizophrenia; schizoaffective disorder |
12 months | Schizophrenia Online Access to Resources (SOAR) is a web-based psychoeducation program for persons with schizophrenia and their supporters (family and friends) that provides engagement, education about illness and treatment, support, and coping strategies. Compared to usual care. |
Significant reduction in positive symptoms and significant increase in knowledge about schizophrenia. Participants showed strong engagement and sustained use of the SOAR intervention. |
| Simon et al., (2011) | United States | RCT | 118 | Bipolar disorder | 3 weeks | MyRecoveryPlan online program includes education, self-monitoring, and social networking. Participants were assigned to MyRecoveryPlan with peer coaching or MyRecoveryPlan only group. |
Participants who received peer coaching were more likely to continue using the program, and used several of the program modules more often when compared to participants who only received the program. |
|
Smith et al., (2011) and Poole et al., (2012) |
United Kingdom |
RCT | 50 | Bipolar disorder | 10 months | Beating Bipolar web-based psychoeducational intervention provides instruction about bipolar disorder, medications, relapse prevention and early intervention. Compared to usual care. |
Significant improvement in the psychological domain of the quality of life scale. No differences in other outcomes. Intervention was feasible and acceptable to participants with access to a computer. |
This study also included 24 supporters (family and friends) of the participants with schizophrenia.
4) Symptom monitoring
Thirteen studies describing 9 interventions focused on symptom monitoring (see Table 4). Seven interventions were delivered using smartphones or other mobile platforms. Many interventions relied on automated prompting of participants to report symptoms at specific times during the day including mood, psychological state, or positive and negative affect (Ainsworth et al., 2013; Ben-Zeev et al., 2012; Bopp et al., 2010; Depp et al., 2012; Faurholt-Jepsen et al., 2014; Palmier-Claus et al., 2012; Palmier-Claus, Ainsworth, et al., 2013; Palmier-Claus, Rogers, et al., 2013; Palmier-Claus et al., 2014), except for one smartphone program designed to continuously collect data on movement, location, physical activity, and social interactions in combination with question prompts (Grünerbl et al., 2012). There was one computer-based intervention for recording mood and measures of medications, sleep, life events, menstrual data, and weight (Bauer et al., 2004), and one online intervention for daily rating of mood, anxiety, and depression (Lieberman et al., 2010; Lieberman et al., 2011). These studies focused primarily on determining feasibility and acceptability, as measured by the frequency participants reported symptoms or responded to automated prompts, number of data points collected, participant reported feedback, as well as reliability and compliance of using remote symptom monitoring compared to clinician or paper-and-pencil ratings (see Table 4).
Discussion
This review included 46 studies of remotely delivered mHealth and eHealth interventions targeting people with SMI. The interventions were grouped into four categories based on their primary purpose: 1) illness self-management and relapse prevention; 2) promoting adherence to medications and/or treatment; 3) psychoeducation, supporting recovery, and promoting health and wellness; and 4) symptom monitoring. The interventions were delivered across mobile and non-mobile web-based platforms, home-based systems, and other remote tracking devices. Feasibility and acceptability outcomes mainly included frequency of intervention use over time, study retention, response rates, and participant reported feedback and usability. Other feasibility outcomes included the proportion of devices returned undamaged, concerns related to privacy, and intervention reliability as compared to traditional approaches. Studies of newer technologies, such as smartphones, remote tracking devices, or wearable technologies, were more likely to emphasize feasibility outcomes when compared to established interventions such as SMS reminders or home-based monitoring systems. However, across all studies there was a consistent and strong finding that these emerging technologies are both highly feasible and acceptable for use among people with SMI.
Clinical outcomes were heterogeneous, ranging from self-reported symptoms, quality of life, perceived social support, and distress, to measures of service use and emergency department visits. Several studies achieved positive findings, highlighting that remotely delivered interventions are potentially effective for people with SMI. However, it is not possible to draw conclusions from this review about the effectiveness of these interventions, because of the varying sample sizes, range of study designs, and different outcomes reported. More rigorous research is necessary to confirm effectiveness. It is also important to note the rapid progression of research in this field, given that 11 of the 46 included studies (24%) were published since 2014.
Our findings provide further evidence that emerging remote technologies can be used to reach and engage this high-risk population as reflected through high rates of adherence and use of the different interventions. Strong support for feasibility and acceptability of remote technologies is important given the serious health concerns facing people with SMI and the urgent need to identify new strategies for promoting illness self-management, engagement in services, self-monitoring, and skill building. Not surprisingly, nearly all included studies were from high income countries, though one study reported positive findings from a SMS appointment reminder intervention in Western Africa (Maiga, 2011). This study leveraged the rapid increase in mobile phone use occurring in many countries in Africa (Zurovac et al., 2013), and offers important early evidence that mobile technologies may play an important role in improving mental health care in low-resource settings (Brian & Ben-Zeev, 2014).
A strength of our review was the inclusion of a diagnostically heterogeneous sample of people with SMI, including schizophrenia, schizoaffective disorder, and bipolar disorder. Importantly, we did not observe differences in feasibility and acceptability between SMI diagnoses, suggesting that emerging mHealth and eHealth interventions are applicable to the diverse patient populations seen in public sector mental health settings. Additionally, we only included remotely delivered mHealth and eHealth interventions, either through mobile, online, or other devices, thereby making a clear distinction from interventions that involve direct and costly interaction with mental health providers through videoconferencing or other forms of technology-assisted communication.
Several limitations should be considered. First, we cannot compare the effectiveness of remotely delivered interventions with in-person or face-to-face services. Given that this is an emerging field and that the outcomes were highly variable across studies, summarizing the quantitative findings into a meta-analysis to determine effectiveness is not yet possible. We did not evaluate the methodological quality of the included studies. We considered this unnecessary because the large number of feasibility and pilot studies identified in our search would have been considered of low methodological quality due to small samples sizes and lack of control groups. Lastly, we did not formally search the grey literature, and it is possible that there may be unpublished findings of remote technology interventions in people with SMI.
Our review expands on prior literature reviews (Alvarez-Jimenez et al., 2014; van der Krieke et al., 2014) by including a larger and broader number of studies that employed a more diverse range of mHealth and eHealth interventions, but similar conclusions regarding feasibility and acceptability were reached, offering further support for using these technologies in people with SMI. It is also important to acknowledge limitations with emerging technologies. Even with increasing affordability and availability of mobile devices and other new technologies, cost remains a significant barrier to ownership and use among many low-income people with SMI (Ben-Zeev, Davis, et al., 2013).
Greater use of the Internet and mobile phones has been observed among low-income and disadvantaged groups, such as people with SMI, however significant gaps in use remain when compared to the general population (McInnes et al., 2013). Furthermore, the success of many of the remote interventions identified in our review relies on continuous and reliable wireless connections to the Internet. While the actual devices can often be inexpensive, there are significant expenses associated with continuing access to data services through monthly plans, which limits access and use among low-income population groups (Viswanath et al., 2012). As the evidence supporting mHealth and eHealth interventions for people with SMI continues to advance, consideration of how the target population will be able to use and access these services is crucial. For example, incentive or discount programs could help address gaps in affordability (Viswanath et al., 2012), with the aim of widely disseminating emerging technologies to at-risk individuals.
An important implication from our findings is that researchers should move beyond simply investigating whether emerging devices are feasible for use among people with SMI. It is clear that people with SMI can use and are interested in using smartphones or services delivered online, while evidence highlights that people with SMI use mobile devices, the Internet, and social media websites (Ben-Zeev, Davis, et al., 2013; Naslund et al., 2014). If adaptations are made to simplify web services or deliver appropriate content (Rotondi et al., 2013), then feasibility and usability of mHealth and eHealth interventions does not appear to be a concern in this population. Rather than focusing on usability or acceptability, future research should be dedicated to exploring the effectiveness of remote technologies for addressing complex health concerns among people with SMI through controlled studies with sufficient statistical power. Formal cost analyses are also needed to determine potential savings from using mHealth and eHealth interventions when compared to in-person or existing telemental health services.
Our review contributes to this field by providing a comprehensive summary of mHealth and eHealth interventions for targeting the high-risk group of people with SMI. Our review can be summarized by three conclusions. First, these emerging technologies are feasible and acceptable for use among people with SMI. Second, remotely delivered interventions appear highly promising for reaching this at-risk group as indicated by preliminary findings of effectiveness. Finally, further rigorous investigation is warranted to establish effectiveness and economic benefit of emerging remote interventions in people with SMI.
Acknowledgments
This work was supported by the United States Centers for Disease Control Health Promotion and Disease Prevention Research Center (Grant number: CDC U48DP005018) and a grant from the National Institute of Mental Health (Grant number: NIMH R01 MH104555). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Declaration of interest: The authors report no competing interests.
References
- Acosta FJ, Bosch E, Sarmiento G, et al. Evaluation of noncompliance in schizophrenia patients using electronic monitoring (MEMS®) and its relationship to sociodemographic, clinical and psychopathological variables. Schizophrenia Research. 2009;107(2–3):213–217. doi: 10.1016/j.schres.2008.09.007. [DOI] [PubMed] [Google Scholar]
- Ainsworth J, Palmier-Claus JE, Machin M, et al. A comparison of two delivery modalities of a mobile phone-based assessment for serious mental illness: native smartphone application vs text-messaging only implementations. Journal of Medical Internet Research. 2013;15(4):e60. doi: 10.2196/jmir.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez-Jimenez M, Alcazar-Corcoles M, González-Blanch C, et al. Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophrenia Research. 2014;156(1):96–106. doi: 10.1016/j.schres.2014.03.021. [DOI] [PubMed] [Google Scholar]
- Alvarez-Jimenez M, Bendall S, Lederman R, et al. On the HORYZON: moderated online social therapy for long-term recovery in first episode psychosis. Schizophrenia Research. 2013;143(1):143–149. doi: 10.1016/j.schres.2012.10.009. [DOI] [PubMed] [Google Scholar]
- Baikie KA, Geerligs L, Wilhelm K. Expressive writing and positive writing for participants with mood disorders: an online randomized controlled trial. Journal of Affective Disorders. 2012;136(3):310–319. doi: 10.1016/j.jad.2011.11.032. [DOI] [PubMed] [Google Scholar]
- Bauer M, Grof P, Gyulai L, et al. Using technology to improve longitudinal studies: self-reporting with Chrono Record in bipolar disorder. Bipolar Disorders. 2004;6(1):67–74. doi: 10.1046/j.1399-5618.2003.00085.x. [DOI] [PubMed] [Google Scholar]
- Bauer S, Moessner M. Technology-enhanced monitoring in psychotherapy and e-mental health. Journal of Mental Health. 2012;21(4):355–363. doi: 10.3109/09638237.2012.667886. [DOI] [PubMed] [Google Scholar]
- Beebe L, Smith KD, Phillips C. A comparison of telephone and texting interventions for persons with schizophrenia spectrum disorders. Issues in Mental Health Nursing. 2014;35(5):323–329. doi: 10.3109/01612840.2013.863412. [DOI] [PubMed] [Google Scholar]
- Ben-Zeev D, Brenner CJ, Begale M, et al. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophrenia Bulletin. 2014:1–10. doi: 10.1093/schbul/sbu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D, Davis KE, Kaiser S, et al. Mobile technologies among people with serious mental illness: opportunities for future services. Administration and Policy in Mental Health and Mental Health Services Research. 2013;40(4):340–343. doi: 10.1007/s10488-012-0424-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D, Frounfelker R, Morris SB, Corrigan PW. Predictors of self-stigma in schizophrenia: new insights using mobile technologies. Journal of Dual Diagnosis. 2012;8(4):305–314. doi: 10.1080/15504263.2012.723311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D, Kaiser SM, Brenner CJ, et al. Development and Usability Testing of FOCUS: A Smartphone System for Self-Management of Schizophrenia. Psychiatric Rehabilitation Journal. 2013;36(4):289–296. doi: 10.1037/prj0000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger M, Wagner TH, Baker LC. Internet use and stigmatized illness. Social Science & Medicine. 2005;61(8):1821–1827. doi: 10.1016/j.socscimed.2005.03.025. [DOI] [PubMed] [Google Scholar]
- Bopp JM, Miklowitz DJ, Goodwin GM, et al. The longitudinal course of bipolar disorder as revealed through weekly text messaging: a feasibility study. Bipolar Disorders. 2010;12(3):327–334. doi: 10.1111/j.1399-5618.2010.00807.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borzekowski D, Leith J, Medoff D, et al. Use of the Internet and other media for health information among clinic outpatients with serious mental illness. Psychiatric Services. 2009;60(9):1265–1268. doi: 10.1176/ps.2009.60.9.1265. [DOI] [PubMed] [Google Scholar]
- Brian RM, Ben-Zeev D. Mobile health (mHealth) for mental health in Asia: Objectives, strategies, and limitations. Asian Journal of Psychiatry. 2014;10:96–100. doi: 10.1016/j.ajp.2014.04.006. [DOI] [PubMed] [Google Scholar]
- Brunette MF, Ferron JC, Devitt T, et al. Do smoking cessation websites meet the needs of smokers with severe mental illnesses? Health Education Research. 2012;27(2):183–190. doi: 10.1093/her/cyr092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depp CA, Kim DH, Vergel De Dios L, et al. A pilot study of mood ratings captured by mobile phone versus paper-and-pencil mood charts in bipolar disorder. Journal of Dual Diagnosis. 2012;8(4):326–332. doi: 10.1080/15504263.2012.723318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson FB, McNary SW, Brown CH, et al. Somatic healthcare utilization among adults with serious mental illness who are receiving community psychiatric services. Medical Care. 2003;41(4):560–570. doi: 10.1097/01.MLR.0000053440.18761.F0. [DOI] [PubMed] [Google Scholar]
- Druss BG, Rosenheck RA, Desai MM, Perlin JB. Quality of preventive medical care for patients with mental disorders. Medical Care. 2002;40(2):129–136. doi: 10.1097/00005650-200202000-00007. [DOI] [PubMed] [Google Scholar]
- Druss BG, Zhao L, Von Esenwein S, et al. Understanding excess mortality in persons with mental illness: 17-year follow up of a nationally representative US survey. Medical Care. 2011;49(6):599–604. doi: 10.1097/MLR.0b013e31820bf86e. [DOI] [PubMed] [Google Scholar]
- Fagiolini A, Goracci A. The effects of undertreated chronic medical illnesses in patients with severe mental disorders. Journal of Clinical Psychiatry. 2009;70(3):22–29. doi: 10.4088/JCP.7075su1c.04. [DOI] [PubMed] [Google Scholar]
- Faurholt-Jepsen M, Frost M, Vinberg M, et al. Smartphone data as objective measures of bipolar disorder symptoms. Psychiatry Research. 2014;217(1–2):124–127. doi: 10.1016/j.psychres.2014.03.009. [DOI] [PubMed] [Google Scholar]
- Frangou S, Sachpazidis I, Stassinakis A, Sakas G. Telemonitoring of medication adherence in patients with schizophrenia. Telemedicine and e-health. 2005;11(6):675–683. doi: 10.1089/tmj.2005.11.675. [DOI] [PubMed] [Google Scholar]
- Gleeson JF, Lederman R, Wadley G, et al. Safety and privacy outcomes from a moderated online social therapy for young people with first-episode psychosis. Psychiatric Services. 2014;65(4):546–550. doi: 10.1176/appi.ps.201300078. [DOI] [PubMed] [Google Scholar]
- Godleski L, Cervone D, Vogel D, Rooney M. Home telemental health implementation and outcomes using electronic messaging. Journal of Telemedicine and Telecare. 2012;18(1):17–19. doi: 10.1258/jtt.2011.100919. [DOI] [PubMed] [Google Scholar]
- Gowen K, Deschaine M, Gruttadara D, Markey D. Young adults with mental health conditions and social networking websites: seeking tools to build community. Psychiatric Rehabilitation Journal. 2012;35(3):245–250. doi: 10.2975/35.3.2012.245.250. [DOI] [PubMed] [Google Scholar]
- Granholm E, Ben-Zeev D, Link PC, et al. Mobile Assessment and Treatment for Schizophrenia (MATS): a pilot trial of an interactive text-messaging intervention for medication adherence, socialization, and auditory hallucinations. Schizophrenia Bulletin. 2012;38(3):414–425. doi: 10.1093/schbul/sbr155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grünerbl A, Oleksy P, Bahle G, et al. Towards smart phone based monitoring of bipolar disorder. Paper presented at the Proceedings of the Second ACM Workshop on Mobile Systems, Applications, and Services for HealthCare.2012. [Google Scholar]
- Hailey D, Roine R, Ohinmaa A. The effectiveness of telemental health applications: a review. The Canadian Journal of Psychiatry/La Revue canadienne de psychiatrie. 2008;53(11):769–778. doi: 10.1177/070674370805301109. [DOI] [PubMed] [Google Scholar]
- Hilty DM, Ferrer DC, Parish MB, et al. The effectiveness of telemental health: a 2013 review. Telemedicine and e-Health. 2013;19(6):444–454. doi: 10.1089/tmj.2013.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones S, Calam R, Sanders M, et al. A pilot web based positive parenting intervention to help bipolar parents to improve perceived parenting skills and child outcomes. Behavioural and Cognitive Psychotherapy. 2014;42(3):283–296. doi: 10.1017/S135246581300009X. [DOI] [PubMed] [Google Scholar]
- Kane JM, Perlis RH, DiCarlo LA, et al. First experience with a wireless system incorporating physiologic assessments and direct confirmation of digital tablet ingestions in ambulatory patients with schizophrenia or bipolar disorder. Journal of Clinical Psychiatry. 2013;74(6):e533–e540. doi: 10.4088/JCP.12m08222. [DOI] [PubMed] [Google Scholar]
- Kaplan K, Salzer MS, Solomon P, et al. Internet peer support for individuals with psychiatric disabilities: a randomized controlled trial. Social Science & Medicine. 2011;72(1):54–62. doi: 10.1016/j.socscimed.2010.09.037. [DOI] [PubMed] [Google Scholar]
- Kaplan K, Solomon P, Salzer MS, Brusilovskiy E. Assessing an Internet-based parenting intervention for mothers with a serious mental illness: a randomized controlled trial. Psychiatric Rehabilitation Journal. 2014;37(3):222–231. doi: 10.1037/prj0000080. [DOI] [PubMed] [Google Scholar]
- Kasckow J, Gurklis J, Haas G. A telehealth intervention for suicidal patients with schizophrenia. Schizophrenia Bulletin [abstracts from the 13th International Congress on Schizophrenia Research, ICOSR Colorado Springs, CO United States. April 2–6 2011] 2011:308–309. [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, et al. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiologia e psichiatria sociale. 2009;18(1):23–33. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Archives of general psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Komatsu H, Sekine Y, Okamura N, et al. Effectiveness of Information Technology Aided Relapse Prevention Programme in Schizophrenia excluding the effect of user adherence: a randomized controlled trial. [Journal: Article] Schizophrenia Research. 2013;150(1):240–244. doi: 10.1016/j.schres.2013.08.007. [DOI] [PubMed] [Google Scholar]
- Lal S, Adair CE. E-mental health: a rapid review of the literature. Psychiatric Services. 2014;65(1):24–32. doi: 10.1176/appi.ps.201300009. [DOI] [PubMed] [Google Scholar]
- Lieberman DZ, Kelly TF, Douglas L, Goodwin FK. A randomized comparison of online and paper mood charts for people with bipolar disorder. Journal of Affective Disorders. 2010;124(1–2):85–89. doi: 10.1016/j.jad.2009.10.019. [DOI] [PubMed] [Google Scholar]
- Lieberman DZ, Swayze S, Goodwin FK. Best practices: an automated internet application to help patients with bipolar disorder track social rhythm stabilization. Psychiatric Services. 2011;62(11):1267–1269. doi: 10.1176/ps.62.11.pss6211_1267. [DOI] [PubMed] [Google Scholar]
- Maiga DD. Interest of using a mobile phone in response to appointments for patients with acute functional psychoses at the psychiatric ward of Niamey National Hospital - Niger - West Africa. Information Psychiatrique. 2011;87(2):127–132. [Google Scholar]
- McInnes DK, Li AE, Hogan TP. Opportunities for engaging low-income, vulnerable populations in health care: a systematic review of homeless persons’ access to and use of information technologies. American Journal of Public Health. 2013;103(S2):e11–e24. doi: 10.2105/AJPH.2013.301623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montes JM, Medina E, Gomez-Beneyto M, Maurino J. A short message service (SMS)-based strategy for enhancing adherence to antipsychotic medication in schizophrenia. Psychiatry Research. 2012;200(2–3):89–95. doi: 10.1016/j.psychres.2012.07.034. [DOI] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Barre LK, Bartels SJ. Feasibility of popular m-Health technologies for activity tracking among individuals with serious mental illness. Telemedicine and e-Health. 2015;21(3):1–4. doi: 10.1089/tmj.2014.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Grande SW, Aschbrenner KA, Elwyn G. Naturally occurring peer support through social media: the experiences of individuals with severe mental illness using YouTube. PLoS One. 2014;9(10):e110171. doi: 10.1371/journal.pone.0110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmier-Claus JE, Ainsworth J, Machin M, et al. The feasibility and validity of ambulatory self-report of psychotic symptoms using a smartphone software application. BMC Psychiatry. 2012;12:172. doi: 10.1186/1471-244X-12-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmier-Claus JE, Ainsworth J, Machin M, et al. Affective instability prior to and after thoughts about self-injury in individuals with and at-risk of psychosis: a mobile phone based study. Archives of Suicide Research. 2013;17(3):275–287. doi: 10.1080/13811118.2013.805647. [DOI] [PubMed] [Google Scholar]
- Palmier-Claus JE, Rogers A, Ainsworth J, et al. Integrating mobile-phone based assessment for psychosis into people's everyday lives and clinical care: a qualitative study. BMC Psychiatry. 2013;13:34. doi: 10.1186/1471-244X-13-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmier-Claus JE, Taylor PJ, Ainsworth J, et al. The temporal association between self-injurious thoughts and psychotic symptoms: a mobile phone assessment study. Suicide & Life-Threatening Behavior. 2014;44(1):101–110. doi: 10.1111/sltb.12064. [DOI] [PubMed] [Google Scholar]
- Pijnenborg GH, Withaar FK, Brouwer WH, et al. The efficacy of SMS text messages to compensate for the effects of cognitive impairments in schizophrenia. British Journal of Clinical Psychology. 2010;49(Pt 2):259–274. doi: 10.1348/014466509X467828. [DOI] [PubMed] [Google Scholar]
- Pompili M, Lester D, Innamorati M, et al. Assessment and treatment of suicide risk in schizophrenia. Expert Review of Neurotherapeutics. 2008;8(1):51–74. doi: 10.1586/14737175.8.1.51. [DOI] [PubMed] [Google Scholar]
- Poole R, Simpson SA, Smith DJ. Internet-based psychoeducation for bipolar disorder: a qualitative analysis of feasibility, acceptability and impact. BMC Psychiatry. 2012;12:139. doi: 10.1186/1471-244X-12-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt SI, Bartels SJ, Mueser KT, et al. Feasibility and effectiveness of an automated telehealth intervention to improve illness self-management in people with serious psychiatric and medical disorders. Psychiatric Rehabilitation Journal. 2013;36(4):297–305. doi: 10.1037/prj0000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt SI, Naslund JA, Wolfe RS, et al. Automated telehealth for managing psychiatric instability in people with serious mental illness. Journal of Mental Health. 2014:1–5. doi: 10.3109/09638237.2014.928403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proudfoot J, Parker G, Manicavasagar V, et al. Effects of adjunctive peer support on perceptions of illness control and understanding in an online psychoeducation program for bipolar disorder: a randomised controlled trial. Journal of Affective Disorders. 2012;142(1–3):98–105. doi: 10.1016/j.jad.2012.04.007. [DOI] [PubMed] [Google Scholar]
- Rotondi AJ, Anderson CM, Haas GL, et al. Web-based psychoeducational intervention for persons with schizophrenia and their supporters: one-year outcomes. Psychiatric Services. 2010;61(11):1099–1105. doi: 10.1176/ps.2010.61.11.1099. [DOI] [PubMed] [Google Scholar]
- Rotondi AJ, Eack SM, Hanusa BH, et al. Critical design elements of e-Health applications for users with severe mental illness: singular focus, simple architecture, prominent contents, explicit navigation, and inclusive hyperlinks. Schizophrenia Bulletin. 2013:1–9. doi: 10.1093/schbul/sbt194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotondi AJ, Haas GL, Anderson CM, et al. A clinical trial to test the feasibility of a telehealth psychoeducational intervention for persons with schizophrenia and their families: intervention and 3-month findings. Rehabilitation Psychology. 2005;50(4):325–336. doi: 10.1037/0090-5550.50.4.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon GE, Ludman EJ, Goodale LC, et al. An online recovery plan program: can peer coaching increase participation? Psychiatric Services. 2011;62(6):666–669. doi: 10.1176/appi.ps.62.6.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simone C, Carolin L, Max S, Reinhold K. Associations between community characteristics and psychiatric admissions in an urban area. Social Psychiatry and Psychiatric Epidemiology. 2013;48(11):1797–1808. doi: 10.1007/s00127-013-0667-1. [DOI] [PubMed] [Google Scholar]
- Sims H, Sanghara H, Hayes D, et al. Text message reminders of appointments: a pilot intervention at four community mental health clinics in London. Psychiatric Services. 2012;63(2):161–168. doi: 10.1176/appi.ps.201100211. [DOI] [PubMed] [Google Scholar]
- Smith DJ, Griffiths E, Poole R, et al. Beating Bipolar: exploratory trial of a novel Internet-based psychoeducational treatment for bipolar disorder. Bipolar disorders. 2011;13(5–6):571–577. doi: 10.1111/j.1399-5618.2011.00949.x. [DOI] [PubMed] [Google Scholar]
- Spaniel F, Hrdlicka J, Novak T, et al. Effectiveness of the information technology-aided program of relapse prevention in schizophrenia (ITAREPS): a randomized, controlled, double-blind study. Journal of Psychiatric Practice. 2012;18(4):269–280. doi: 10.1097/01.pra.0000416017.45591.c1. [DOI] [PubMed] [Google Scholar]
- Spaniel F, Vohlidka P, Hrdlicka J, et al. ITAREPS: information technology aided relapse prevention programme in schizophrenia. Schizophrenia Research. 2008;98(1–3):312–317. doi: 10.1016/j.schres.2007.09.005. [DOI] [PubMed] [Google Scholar]
- Spaniel F, Vohlidka P, Kozeny J, et al. The Information Technology Aided Relapse Prevention Programme in Schizophrenia: an extension of a mirror-design follow-up. International Journal of Clinical Practice. 2008;62(12):1943–1946. doi: 10.1111/j.1742-1241.2008.01903.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd NJ, Jones SH, Hart A, Lobban FA. A web-based self-management intervention for bipolar disorder ‘Living with bipolar’: a feasibility randomised controlled trial. Journal of Affective Disorders. 2014;169:21–29. doi: 10.1016/j.jad.2014.07.027. [DOI] [PubMed] [Google Scholar]
- van der Krieke L, Wunderink L, Emerencia AC, et al. E–mental health self-management for psychotic disorders: state of the art and future perspectives. Psychiatric Services. 2014;65(1):33–49. doi: 10.1176/appi.ps.201300050. [DOI] [PubMed] [Google Scholar]
- Viswanath K, Nagler RH, Bigman-Galimore CA, et al. The communications revolution and health inequalities in the 21st century: implications for cancer control. Cancer Epidemiology Biomarkers & Prevention. 2012;21(10):1701–1708. doi: 10.1158/1055-9965.EPI-12-0852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenze SJ, Armey MF, Miller IW. Feasibility and acceptability of a mobile intervention to improve treatment adherence in bipolar disorder: a pilot study. Behavior Modification. 2014;38(4):497–515. doi: 10.1177/0145445513518421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zurovac D, Otieno G, Kigen S, et al. Ownership and use of mobile phones among health workers, caregivers of sick children and adult patients in Kenya: cross-sectional national survey. Global Health. 2013;9:20. doi: 10.1186/1744-8603-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]


