Introduction
Varicose veins are a common venous anomaly, where as phlebeetasia is rare. It is an abnormal dilation of an isolated vein. Any vein may be affected and the condition is usually asymptomatic [1]. Internal jugular phlebeetasia (IJP) is abnormal dilation of internal jugular vein (IJV). This report aims at clinical awareness of the condition.
Case Report
4 year old girl observed a painless, fusiform swelling on the lower part of anterior aspect of right side of the neck of 15 days duration. This swelling became visible only on coughing (Fig 1). The child had no other complaint. General physical examination revealed no abnormality. Routine investigations were within normal limits.
Fig. 1.
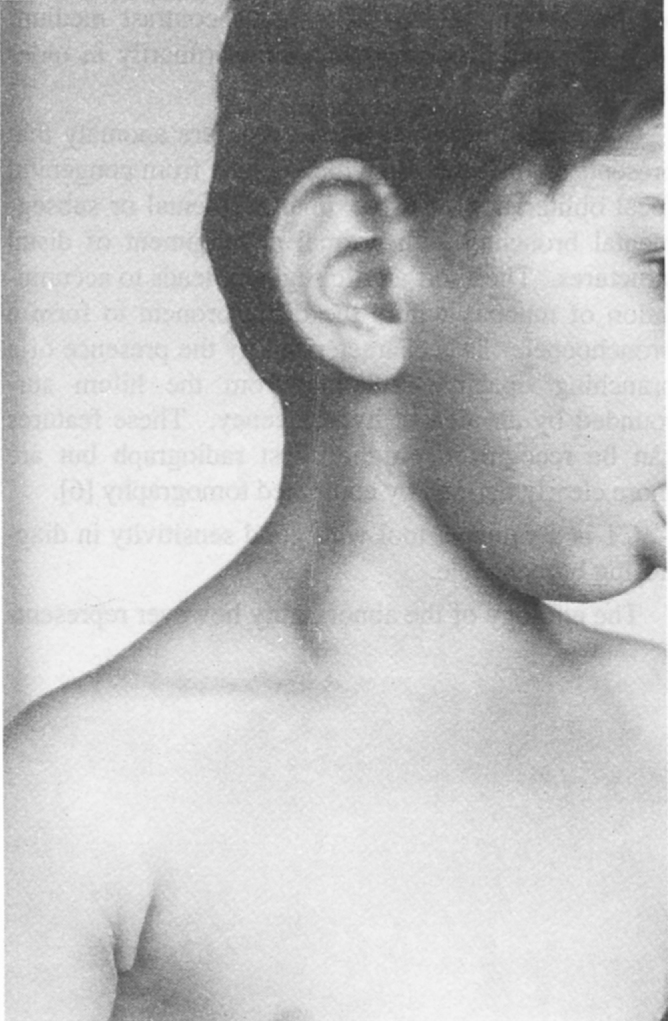
Swelling in the neck visible only while coughing
Ultrasound examination revealed the calibre of right internal jugular vein in the lower part of neck substantially more as compared to that on the left and it further increased when the child was asked to cough. The common carotid arteries were normal. On colour Doppler flow imaging a slow flow signal flowing in the direction opposite to that of the common carotid artery was seen. Contrast CT scan confirmed the dilated right internal jugular vein in the lower part of neck (Fig 2) measuring on cross section 16X10 mm on the right as compared to 7X6 mm on left. Direct puncture venography demonstrated the dilated right internal jugular vein in the lower part of neck before joining the right innominate vein.
Fig. 2.
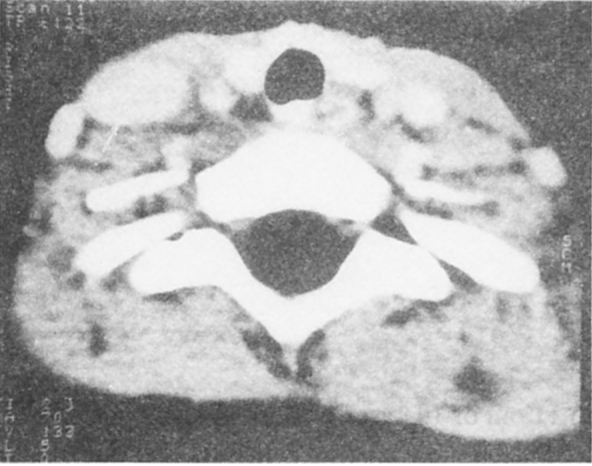
CT scan section at the level of thyroid shows gross dilatation of right internal jugular vein (arrow) as compared to that on the left.
Discussion
IJP is abnormal dilation of IJV. It presents as a soft fluctuant, fusiform swelling lying in the anterior aspect of the lower part of the neck which changes in size and becomes visible and prominent during coughing (as seen in this case), crying, sneezing, straining or during the Valsalva manoeuvre. The swelling closely mimics the signs of either a laryngocoele or a pharyngocoele and due to its rarity, is frequently misdiagnosed [2]. A case of phlebectasia of IJV in a child presenting with voice change has also been reported [1]. Indudharan [3] reported a 7 year old child who presented with a soft fluctuant swelling on the neck which became more prominent during the Valsalva manoeuvre. He underwent adeno-tonsillectomy based on a mistaken diagnosis of ballooning of the pharynx secondary to enlarged adenoids and tonsils obstructing the nasopharyngeal and oropharyngeal airways. Investigations revealed the swelling to be a markedly dilated IJV.
IJP is rare and mostly involves the right side. It is usually a childhood disease between 5-11 years of age, no sex preponderance is observed. However it can occur at any age and affects both genders [4]. Kao WR et al reported a 66 year old female patient complaining of a bulging mass on her right neck and the diagnosis was confirmed as IJP [5].
The cause of the jugular phlebectasia remains unclear. However, microscopic examination of a dissected portion of the dilated IJV showed paucity or absence of muscle layer, therefore, it is assumed to be a congenital muscle defect of the venous wall [6, 7, 8].
Ultrasonographic examination of the jugular mass demonstrates an echo-free space, the calibre of which markedly increases when the patient is made to cough as seen in this case, when moved from the sitting to the recumbent position or on performing a Valsalva manoeuvre. Colour Doppler flow imaging shows a slow flow signal flowing in the direction opposite to that of the common carotid artery [9].
Ultrasound and colour Doppler imaging are useful for diagnosing IJP, CT and venography confirm the diagnosis [10].
No treatment is indicated for this self-limiting benign condition, except for few patients who complain of symptoms or for cosmetic reasons. The treatment is excision of the affected jugular vein. This produces no gross side-effects [7] and therefore, the diagnosis has to be made with certainty from the clinical features and imaging techniques employing colour Doppler, contrast CT [4] and perhaps a direct puncture venography as carried out in this case.
Every patient with a swelling in the neck that enlarges in size after the Valsalva manoeuvre, straining, coughing or sneezing should be suspected of having jugular phlebectasia [7]. Even though most of these lesions have been excised surgically, the treatment of choice should be conservative as long as it is asymptomatic [4].
References
- 1.Lubianca-Neto JF, Mauri M, Prati C. Internal jugular phelbectasia ill children. Am J Otolaryngol. 1999;20:415–418. doi: 10.1016/s0196-0709(99)90085-6. [DOI] [PubMed] [Google Scholar]
- 2.Bowdler DA, Singh SD. Internal jugular phlebectasia. Int J Pediatr Otorhinolaryngol. 1986;12:165–171. doi: 10.1016/s0165-5876(86)80073-8. [DOI] [PubMed] [Google Scholar]
- 3.Indudharan R, Quah BS, Shuaib IL. Internal Jugular phlebectasia—an unusual cause of neck swelling. Ann Trop Paediatr. 1999;19:105–108. doi: 10.1080/02724939992725. [DOI] [PubMed] [Google Scholar]
- 4.al-Dousary S. Internal jugular phlebectasia. Int J Pediatr Otorhinolaryngol. 1973;38:273–280. doi: 10.1016/s0165-5876(96)01455-3. [DOI] [PubMed] [Google Scholar]
- 5.Kuo WR, Chien CC, Chai CY, Huang HR, Jan YS, Hung YC, Juan KH. Internal jugular phlebectasia. Kao Hsiung I Hsuch Ko Hsueh Tsa Chih. 1992;8:503–509. [PubMed] [Google Scholar]
- 6.Yokomori K, Kubo K, Kanamori Y, Takemura T, Yamamoto T. Internal Jugular phlebectasia in two siblings:manometric and histopathologic studies of the pathogenesis. J Pediatr Surg. 1990;25:762–765. doi: 10.1016/s0022-3468(05)80014-4. [DOI] [PubMed] [Google Scholar]
- 7.Pul N, Pul M. External jugular phlebectasia in children. Eur J Pediatr. 1995;154:275–276. doi: 10.1007/BF01957361. [DOI] [PubMed] [Google Scholar]
- 8.Gurpinar A, Kiristioglu I, Dogruyol H. Jugular phlebectasia. Eur J Pediatr Surg. 1999;9:182–183. doi: 10.1055/s-2008-1072238. [DOI] [PubMed] [Google Scholar]
- 9.Shimizu M, Takagi Y, Yoshio H, Takeda R, Matsui O. Usefulness of ultrasonography and Doppler color flow imaging in the diagnosis of internal jugular phlebectasia. Heart Vessels. 1992;7:95–98. doi: 10.1007/BF01744455. [DOI] [PubMed] [Google Scholar]
- 10.Yashiro N, Iio M. Internal jugular phlebectasia in children. Radiat Med. 1984;2:136–139. [PubMed] [Google Scholar]


