Introduction
Dermoid cysts are frequently used to describe three closely related histologic cysts; the dermoid, epidermoid and teratoma, which are rare findings in the floor of the mouth. Bultin in 1885 was the first to report a case [1]. New and Erish in 1937 studied a series of 1,495 cases of dermoid cysts and only 24 (1.6% of cases) of them were in the floor of the mouth [2]. Katz (1974) reviewed literature and reported 1.8% cases of dermoids to arise from the floor of the mouth [3]. Among dermoid cysts, epidermoid cysts of the floor of the mouth are still rare, and King in 1994 among 198 cases of dermoid cysts in the region described 108 cases of dermoids itself, 32 of epidermoid and 7 teratomas [4]. We report a giant recurrent epidermoid cyst located in the midline of the floor of the mouth and a novel surgical approach to ensure complete excision because of its recurrent status.
Case Report
A 22 year old male patient presented with complaints of progressively increasing swelling of the floor of the mouth and suprahyoid neck of 18 months duration. He gave history of a similar swelling 2 years back which was operated through the intraoral route but recurred within 2 months. The swelling was initially only in the floor of the mouth, however with gradual enlargement, it progressively became more prominent in the upper part of the neck in the midline. There was associated progressive dysarthria and dysphagia. The symptoms had rapidly progressed in the previous two weeks. There was no dyspnoea.
Examination revealed a tense tender cystic swelling involving the anterior floor of the mouth pushing the tongue upwards and backwards, therby distorting and compressing the oropharyngeal airway. The neck swelling was 10×8 cm in the submental triangle, tense, cystic, with smooth surface. Local temperature was mildly elevated. The swelling did not move on swallowing or on tongue protrusion. Indirect laryngoscopy could not be done due to posterosuperior displacement of the tongue. Flexible Fiberoptic Laryngoscopy revealed a grossly reduced and distorted oropharynx. The hypopharynx and larynx were normal.
Complete blood count, biochemistry and X-ray chest were within normal limit. FNAC of the swelling was done through both an intra-oral and extra-oral route and sugested an inflamed epidermoid cyst. Contrast enhanced CT Scan showed a 10×8 cm cystic swelling of the sub-lingual space below the genioglossus pushing the mylohyoid downwards, extending posteriorly upto the base of tongue, compressing the oropharyngeal airway (Fig. 1, Fig. 2).
Fig. 1.
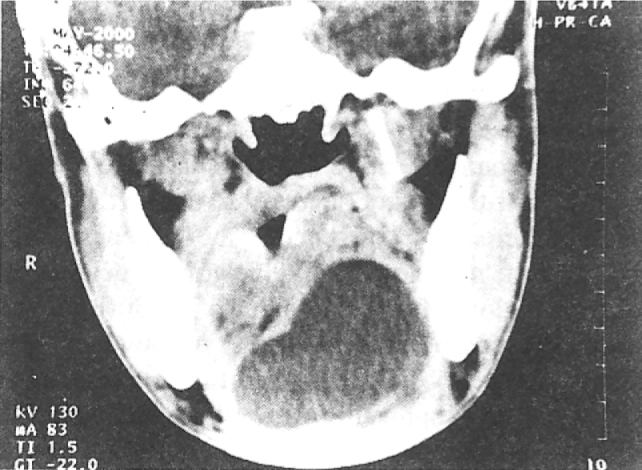
CT scan showing elevated base of tongue with compromised oropharyngeal airway due to giant dermoid cyst floor of mouth
Fig. 2.

Giant epidermoid cyst floor of mouth with compromised airway
Because of the extremely large size of the cyst, failure of nasal intubation and problem of sharing the oral cavity with endotracheal tube, an extra-oral approach was chosen for surgical excsion. Through a midline lip-splitting incision the cyst was approached by carrying out a symphyseal mandibulotomy and swinging the mandible. The cyst was excised completely and the wound was closed in layers after stablizing the mandible with miniplates. Postoperative period was uneventful. Histopathology of the cyst confirmed a diagnosis of an inflamed epidermoid cyst.
Discussion
Dermoid cysts are rare congenital lesions derived from ectodermal differentiation [5]. Histologically, they are divided into three types according to their contents. If there are no dermic annexes present, the cyst is called epidermoid, if there are annexes such as sebacious glands, sudoriferous glands or hair follicle, the cyst is called dermoid [4]. The third type is called teratoma and is formed by a covering containing structures derived from the three germ layers-ectoderm, endoderm and mesoderm, and it can contain dermic annexes, segments of muscles and bone or respiratory and gastrointestinal mucosa [6, 7, 8].
The pathogenesis of dermoid cysts is still undefined [9] with two theories to explain its origin. The commonly accepted one is the congenital theory, which suggests that the cyst originates from the median pluripotent tissue incarcerated during the fusion of the first and second brachial arch in the third and fourth week of intrauterine life. The second is the aquired theory in which the implantation of epithelial cells in deep tissues during intrauterine life is secondary to trauma (amniocentesis) or accidental.
Dermoid cysts are most frequently manifested between the second to sixth decade of life, although cases of younger and older patients have been reported. All the authors agree that there is no sex-related preference. In general, the patient becomes aware of the pathology due to the gradual deterioration of loco regional functional signals i.e. difficulties related to speech, chewing and swallowing. These symptoms are closely correlated to the size of the lesion. The development of the cyst is usually slow and does not involve painful symptoms, but it may become rapid and painful in the presence of concomitant infection [10].
Epidermoid and dermoid cysts are rare benign tumors that may occur anywhere in the body and can reach very large sizes. About 7% of them are found in the head and neck region and only 1.6% are located within the oral cavity [12]. The most frequent location in the head and neck area is the peri-orbital region followed by peri- or intra-oral sites. The majority of cases in the head and neck are found in individuals over 20 years of age, without a sex predilection. The intraoral cyst generally develops in the floor of the mouth and it can be found either lateral to the tongue or in the midline of the oral floor.
Colp in 1925 classified the cysts according to their relation with muscles. They can be located over the geniohyoid muscle and below the genioglossus muscle, bowing the submental region or below geniohyoid muscle and above the mylohyoid muscle bowing the submental region. They can also be located laterally in submandibular space above mylohyoid muscle laterally under tongue [4]. A CT Scan is essential in defining its exact location and planning surgery [11]. A scan done in our case showed the cyst to be lying above mylohyoid muscle extending posteriorly upto the base of tongue and below the genioglossus muscle. Lesion extended across midline pushing the median raphe and the genioglossus to the right. There was no mandibular erosion or adenopathy.
The location of the cyst is a determining factor for surgical approach. Most authors prefer to use the intraoral approach for sublingual cysts and submental approach for the submental and submandibular cysts [6]. Seward 1965 and Rapidis 1981 advocated the intraoral approach for all cases, except when there are large blood vessels adjacent to the cysts. Other authors suggest extraoral approach for large cysts, so that damage to subjacent structures may be prevented [4].
In our case because of the size, reccurrence and secondary infection and sharing of oral cavity with an endotracheal tube an extra oral lip splitting incision with medial mandibulotomy and mandibular swing was used to ensure complete excision.
In patients presenting with lesions of the floor of the mouth, FNAC should be the diagnostic procedure of first choice [14]. Several neck cysts and neoplasms should be considered in the differential diagnosis such as:ranula, thyroglossal tract cyst, cystic hygroma, cervical lymphoepithelial cyst, and cellulitis among others [15].
The treatment of choice for these cysts is surgery. We present one such rare case because of its size of 10×8 cm and being a recurrent swelling, required a unique mid line approach of lip splitting and medial mandibulotomy with mandibular swing to ensure complete excision. This approach has not been described in literature for this benign lesion.
References
- 1.Bultin HT. Diseases of longue. Cassal; London: 1885. p. 237. [Google Scholar]; Apud, Al-Khayat M, Kenyon GS. Midline sublingual dermoid cyst. J Laryngol Otol. 1990;104:578–580. doi: 10.1017/s0022215100113210. [DOI] [PubMed] [Google Scholar]
- 2.New GB, Erish JB. Dermoid cysts of the head and neck. J Laryngol Otol. 1990;104:578–580. [Google Scholar]; Apud M, Al-Khayat, Kenyon GS. Midline sublingual dermoid cysts. J Laryngol Otol. 1990;104:578–580. doi: 10.1017/s0022215100113210. [DOI] [PubMed] [Google Scholar]
- 3.Kantz AD. Midline dermoid tumors of the neck. Arch Surg. 1974;109:822–823. doi: 10.1001/archsurg.1974.01360060088024. [DOI] [PubMed] [Google Scholar]
- 4.King RC, Smith BR, Burk JL. Dermoid cysts in the floor of the mouth. Oral Surg, Oral Med, Oral Pathol. 1994;78:567–576. doi: 10.1016/0030-4220(94)90166-x. [DOI] [PubMed] [Google Scholar]
- 5.Riera SC, Domenech CE, Valladares MJ. Dermoid cyst of the mouth floor. Acta Otorrinolaringol Esp. 1999;50(1):78–80. [PubMed] [Google Scholar]
- 6.Faerber TH, Hiatt WR, Dunlap C. Congenital teratoid cysts of the floor of mouth. J Oral Maxillofac Surg. 1988;46:487–490. doi: 10.1016/0278-2391(88)90419-3. [DOI] [PubMed] [Google Scholar]
- 7.Eppley BL, Bell MJ, Selaroff A. Simultaneous occurrence of dermoid and heterotropic intestinal cysts in the floor of the mouth of a newborn. J Oral Maxillofac Surg. 1985;43:880–883. doi: 10.1016/0278-2391(85)90227-7. [DOI] [PubMed] [Google Scholar]
- 8.Takato T, Masaru I, Yoshiyuki Y. Heterotropic gastrointestinal cysts of the oral cavity. Ann Plast Surg. 1989;47:733–736. [Google Scholar]
- 9.Triantafillidou E, Karakasis D, Laskin J. Swelling of the floor of the mouth. J Oral Maxillofac Surg. 1989;47:733–736. doi: 10.1016/s0278-2391(89)80016-3. [DOI] [PubMed] [Google Scholar]
- 10.Bonilla JA, Szeremeta W, Yellon RF, Nazif MM. Teratoid cyst of the floor of the mouth. Int J Pediatr Otorhinolaryngol. 1996;5(1):38. doi: 10.1016/s0165-5876(96)01380-8. [DOI] [PubMed] [Google Scholar]; Bonilla JA, Szeremeta W, Yellon RF, Nazif MM. Teratoid cyst of the floor of the mouth. Int J Pediatr Otorhinolaryngol. 1996;5(1):71–75. doi: 10.1016/s0165-5876(96)01380-8. [DOI] [PubMed] [Google Scholar]
- 11.Turetschek K, Hospodka H, Steiner E. Case report: epidermoid cyst of the floor of the mouth:diagnostic imaging by sonography, computed tomography and magnetic resonance imaging. Br J Radiol. 1995;68(806):205–207. doi: 10.1259/0007-1285-68-806-205. [DOI] [PubMed] [Google Scholar]
- 12.Seward GR. Dermoid cysts of the floor of the mouth. Br J Oral Surg. 1965;3:36–47. doi: 10.1016/s0007-117x(65)80005-1. [DOI] [PubMed] [Google Scholar]; Apud RC, King, Smith BR, Burk JL. Dermoid cyst in the floor of the mouth. Oral Surg, Oral Med, Oral Pathol. 1994;78:567–576. doi: 10.1016/0030-4220(94)90166-x. [DOI] [PubMed] [Google Scholar]
- 14.Carmer H, Lampe H, Downing P. Dermoid cyst of the floor of the mouth diagnosed by fine needle aspiration cytology: a case report. Acta Cytol. 1996;40(2):319–326. doi: 10.1159/000333760. [DOI] [PubMed] [Google Scholar]
- 15.Lohaus M, Hansmann J, Witzsel A, Flechtenmacher C, Mende U, Reisser C. Uncommon Sonographic findings of an epidermoid cyst in the head and neck. HNO. 1999;47(8):737–740. doi: 10.1007/s001060050454. [DOI] [PubMed] [Google Scholar]
Uncited Reference
- 13.Rapidis AD, Angelopoulos AP, Scouteris C. Dermoid cyst of floor of the mouth: report of a case. Br J Oral Surg. 1981;19:43–51. doi: 10.1016/0007-117x(81)90020-2. [DOI] [PubMed] [Google Scholar]


