Abstract
OBJECTIVES:
Inadequate sleep during infancy is associated with adverse outcomes for infants and families. We sought to improve sleep behaviors and duration through a responsive parenting (RP) intervention designed for obesity prevention.
METHODS:
The Intervention Nurses Start Infants Growing on Healthy Trajectories (INSIGHT) study is a randomized trial comparing a RP intervention with a safety control. Primiparous mother-newborn dyads were randomized after childbirth, and research nurses delivered intervention content at home visits at infant ages 3, 16, 28, and 40 weeks and at a research center visit at 1 year. The RP sleep component included developmentally appropriate messages about bedtime routines, sleep location and behaviors, and responses to wakings. Portions of the Brief Infant Sleep Questionnaire were administered 2, 8, and 52 weeks after birth with expanded sleep-related data collection at 16 and 40 weeks.
RESULTS:
Two hundred and seventy-nine dyads completed the first home visit; 90.7% completed the 1-year visit. Compared with controls, RP group infants were less likely to have prolonged bedtime routines >45 minutes and more likely to have earlier bedtimes at 16 and 40 weeks. They were less likely to be fed immediately before bed and more likely to self-soothe to sleep. At 8, 16, and 40 weeks, RP group nocturnal sleep duration was longer by 35, 25, and 22 minutes, respectively (P < .05 for all). Sleep duration at 1 year was similar between groups.
CONCLUSIONS:
The INSIGHT RP intervention positively influenced developmentally appropriate bedtime routines, sleep-related behaviors, and sleep duration for infants.
What’s Known on This Subject:
Short sleep duration during infancy has been associated with numerous adverse outcomes for infants and their families. Inadequate sleep affects infant cognitive, psychomotor, physical, and socioemotional development, as well as parental emotional health and parenting practices.
What This Study Adds:
A responsive parenting intervention delivered at home nurse visits positively influenced developmentally appropriate bedtime routines, sleep-related behaviors, and nighttime sleep duration in the first year after birth.
Many young children get less sleep than they require,1 and today’s children sleep less than those in previous generations.2 Inadequate sleep is problematic because sleep is associated with cognitive, psychomotor, physical, and socioemotional development, including emotional regulation, mood, and behavior in infancy and childhood.3–6 Furthermore, infant sleep-related behaviors are associated with maternal sensitivity, relationship quality, parental emotional health, and parenting practices.7,8 Inadequate sleep has also emerged as an important risk factor for obesity9,10 with links between sleep and weight beginning in infancy.11–16 Short sleep duration during infancy is also associated with inadequate sleep later in childhood,17 and therefore improving sleep-related behaviors and extending infant sleep duration has the potential to influence the long-term well-being of children and families.
During the first year, infants spend much of their time asleep but experience substantial changes in sleep/wake cycles. For the first few weeks, infants wake every few hours, typically to feed, and normal circadian rhythms are developed.18–23 After this period, how parents put their infant to bed (eg, bedtime routines, falling asleep independently) and respond to night wakings represent sources of variability in infants’ developing sleep patterns24,25 and also affects the frequency and timing of feedings. Previously, we demonstrated that early in infancy, nocturnal sleep duration can be extended by teaching parents caregiving procedures to address non–hunger-related fussiness.26,27 Combined with education on hunger and satiety cues, this reduced nighttime feeds and awakenings. Another recent report describing an Internet-based intervention designed to improve infant and toddler sleep revealed that participants took less time to fall asleep, had less time awake overnight, and had longer sleep durations between awakenings.28 Maternal sleep and mood improved, and positive benefits on infants’ sleep were seen 1 year later.29
Given evidence of sleep’s malleability and its links to weight outcomes, we included sleep-related components within a responsive parenting (RP) intervention designed for the primary prevention of obesity. On the basis of previous research,26–28 the sleep components focused on consolidating sleep and extending night sleep duration by providing guidance on sleep-related parenting behaviors, particularly establishing consistent bedtime routines, encouraging self-soothing and early bedtimes, and strategies to address night waking.30 In this ongoing randomized, controlled trial, the RP intervention is compared with a home safety control intervention that includes a safe sleep component. We assessed intervention effects on infant sleep in the first year with the hypothesis that sleep duration would be longer and positive sleep-related behaviors would be more prevalent compared with controls.
Methods
Participants and Design
Mothers and their newborns were recruited after delivery from 1 maternity ward (Penn State Milton S. Hershey Medical Center, Hershey, PA) into the Intervention Nurses Start Infants Growing on Healthy Trajectories (INSIGHT) study from January 2013 to March 2014 (see Supplemental Information). The study design and inclusion/exclusion criteria have been published previously.30 Major eligibility criteria included term singletons weighing ≥2500 g delivered to English-speaking, primiparous mothers ≥20 years old. Using a computer-generated algorithm, 291 dyads were randomized 2 weeks after delivery to the RP or control groups, stratified on birth weight for gestational age (<50th percentile or ≥50th percentile) and intended feeding mode (breastfeeding or formula). A baseline survey was administered to mothers electronically. Two hundred and seventy-nine mother-infant dyads completed the first home visit and are considered the study cohort for outcomes as specified before study initiation in the protocol.
As described previously, research nurses were trained in administering both the RP and control interventions30 at home visits conducted at infant age 3–4, 16, 28, and 40 weeks, and a research center visit occurred at age 1 year. This study was approved by the Penn State College of Medicine’s Human Subjects Protection Office and registered at http://www.clinicaltrials.gov without sleep noted as an a priori outcome.
RP Intervention Sleep-Related Components
INSIGHT’s RP intervention contained messages addressing infant behavioral states: Drowsy, Sleeping, Fussy, and Alert.30 Lessons include instructing parents to (1) recognize infant hunger and satiety cues; (2) use alternatives to feeding to soothe a fussy, but nonhungry, infant; (3) provide appropriate portions of healthy foods and allow children to determine the amount consumed; (4) improve acceptance of developmentally appropriate foods such as vegetables through repeated exposure and positive role modeling, while discouraging controlling feeding practices; and (5) actively engage infants in playtime to reduce sedentary behaviors.
Developmentally appropriate sleep guidance was delivered at visits within 3 categories: Bedtime Routine, Sleep Location and Behaviors, and Night Waking (Table 1). This guidance was consistent with recommendations for age-appropriate sleep durations,31 helped parents recognize whether fussiness was due to fatigue versus hunger, provided strategies to transition infants from a fussy or drowsy state to sleep without feeding, and included detailed information on bedtimes and routines before bed, particularly the importance of consistent, short bedtime routines that do not finish with feeding to sleep, early bedtimes, and the importance of self-soothing to sleep and after night wakings. Before the 3-week visit, participants received materials by mail; for RP parents, materials included a video32 describing alternative soothing strategies and instructions to view it, practice soothing strategies before the home visit, and use these strategies, particularly at night. At the 16- and 40-week visits, nurses used the Brief Infant Sleep Questionnaire (BISQ)33 to provide each mother with a personalized infant sleep profile,28 including information regarding how much her infant slept relative to recommendations and customized sleep-related feedback.
TABLE 1.
RP Intervention: Sleep Components During First Year
| Intervention Component | 3–4 Weeks | 16 Weeks | 28 Weeks | 40 Weeks |
|---|---|---|---|---|
| Bedtime routine | ||||
| Consistent routine beginning 30–45 min before bedtime | x | x | x | x |
| Choose age-appropriate, calm bedtime activity | x | x | x | x |
| Feeding not the last step before bed | x | x | x | x |
| Cereal in the bottle does not improve sleep | x | x | x | |
| Offer child choices with routine (eg, choice between 2 books) | ||||
| Sleep location and behaviors | ||||
| Age-appropriate sleep duration guidance | x | x | x | x |
| Best bedtime is 7–8 pm | x | x | ||
| Avoid stimulating environment at bedtime (low light, no TV, etc) | x | x | ||
| Use white noise | x | x | ||
| Use swaddle blanket | x | |||
| Pacifier use | x | |||
| Transition to own room by 3 mo | x | x | x | x |
| Consistently put to bed drowsy but still awake by 4 mo | x | x | ||
| Avoid rocking, feeding to sleep | x | x | ||
| Allow infant some time to self-soothe when put down for night | x | x | x | |
| Nap frequency, duration, and routines | x | x | ||
| Strategies for separation anxiety affecting sleep | x | |||
| Night waking | ||||
| Respond differently night vs day | x | |||
| Stop waking infant routinely to feed | x | |||
| Caretaking behaviors other than feeding: 5 S’s34 | x | |||
| Feed before parent’s bedtime: “dream feed” | x | |||
| Avoid “dream feeds” after age 4 mo | x | |||
| Allow infant some time to self-soothe when waking at night | x | x | x | |
| Possible increased frequency around developmental advances | x | x | x | |
| Do not reinforce waking; keep night interactions with child boring | x | x | x | |
| Avoid overnight feeds; infants can sleep 8–12 h without eating | x | |||
| Personalized sleep profile | x | x |
5 S's, swaddling, side (or stomach) position, shhhhing, swinging, sucking.
Control Group Sleep-Related Components
Briefly, INSIGHT’s home safety control intervention contained crib safety and prevention of sudden infant death syndrome components in a 2-week mailing and at the 3–4-week home visit.30 At the 3–4- and 16-week visits, the infant’s sleep surface was examined by the nurse to tailor safety guidance. At the 16- and 28-week visits, sleep safety recommendations addressed developmental changes, such as rolling over and pulling to stand. At 40 weeks, information on prevention of carbon monoxide poisoning was provided.
Measures
Data were collected and managed using REDCap.35 Paper surveys were mailed to those lacking Internet connectivity (n = 20). A detailed listing of measures has been published.30
Background Characteristics
Demographic information collected at enrollment included parent and child race/ethnicity, annual income, and marital status. Data extracted from medical charts included maternal age, prepregnancy weight, gestational weight gain, infant gestational age, and birth anthropometrics.
Sleep
The validated BISQ was used to assess sleep.33 This survey assesses infant sleep location, before-bedtime activities, and sleep patterns. Sleep duration is divided into nighttime (7 pm–7 am) and daytime (7 am–7 pm) and is reported in hours and minutes. Selected questions capturing sleep duration (day and night), location, and night feedings were administered at infant age 2 (baseline), 8, and 52 weeks. An expanded version was completed at 16 and 40 weeks that also included questions on bedtime routine components and duration, infant sleep behaviors and environment, and parenting responses to night wakings. Further questions assessed specific behaviors related to the RP intervention’s sleep guidance. A Bedtime Routines Questionnaire36 was completed at age 52 weeks, with questions about consistency of parenting behaviors before bedtime and consistency of the bedtime environment.
Statistical Analysis
Data were analyzed by using SAS version 9.4 (SAS Institute, Cary, NC). Descriptive statistics were generated for sleep duration, bedtime routine components, sleep location and behaviors, and night wakings. Each outcome variable was assessed for normality. Statistical significance was defined as P ≤ .05. Bedtime routine data were analyzed by χ2 and Mantel-Haenszel tests. Effects of study group on sleep duration were analyzed by t tests; effects of sleep behaviors were analyzed as nested effects, along with study group, in analyses of variance, with Tukey’s honest significant difference post hoc comparisons used to compare sleep behavior effects on sleep duration, wakings, and feedings.
Results
Among 279 participants, there were no differences between RP and control groups on demographic or baseline characteristics including feeding mode (Table 2). Mothers were predominantly white, non-Hispanic, married, employed, well-educated, and privately insured at enrollment. At 1 year, 90.7% remained in the study with no significant difference in attrition by study group.
TABLE 2.
Demographic Characteristics of Mothers and Infants Who Were Randomized and Received First Nurse Home Visit (n = 279)
| RP (n = 140) | Control (n = 139) | |
|---|---|---|
| Infant | ||
| Male sex, n (%) | 75 (54) | 69 (50) |
| Gestational age (wk), mean (SD) | 39.6 (1.2) | 39.5 (1.1) |
| Birth wt (kg), mean (SD) | 3.40 (0.43) | 3.46 (0.43) |
| Birth length (cm), mean (SD) | 50.9 (2.4) | 50.7 (4.5) |
| Mother | ||
| Age, y, mean (SD) | 28.7 (4.6) | 28.7 (4.9) |
| Prepregnancy BMI, mean (SD) | 25.5 (5.0) | 25.3 (5.6) |
| Gestational wt gain (kg), mean (SD) | 15.6 (6.4) | 15.0 (6.0) |
| Diabetes during pregnancy, n (%) | 6 (4.3) | 13 (9.4) |
| Smoked during pregnancy, n (%) | 12 (8.6) | 9 (6.5) |
| Race, n (%) | ||
| Black | 10 (7.1) | 7 (5.0) |
| White | 122 (87.1) | 127 (91.4) |
| Native Hawaiian or Pacific Islander | 1 (0.7) | 0 (0) |
| Asian | 5 (3.6) | 4 (2.9) |
| Other | 2 (1.4) | 1 (0.7) |
| Marital status, n (%) | ||
| Married | 102 (72.9) | 108 (77.7) |
| Not married, living with partner | 25 (17.9) | 19 (13.7) |
| Single | 12 (8.6) | 12 (8.6) |
| Divorced/separated | 1 (0.7) | 0 (0) |
| Annual household income, n (%) | ||
| <$10 000 | 6 (4.3) | 5 (3.6) |
| $10 000–$24 999 | 10 (7.1) | 10 (7.2) |
| $25 000–$49 999 | 5 (3.6) | 23 (16.6) |
| $50 000–$74 999 | 46 (32.9) | 26 (18.7) |
| $75 000–$99 999 | 32 (22.9) | 23 (16.6) |
| ≥$100 000 | 32 (22.9) | 43 (30.9) |
| Do not know or refuse to answer | 9 (6.4) | 9 (6.4) |
| Education, n (%) | ||
| High school graduate or less | 16 (11.4) | 16 (11.5) |
| Some college | 37 (26.4) | 36 (25.9) |
| College graduate | 48 (34.3) | 52 (37.4) |
| Graduate degree or higher | 39 (27.9) | 35 (25.2) |
Bedtime Routine and Sleep Behaviors
At baseline 2 weeks after delivery, there were no significant group differences in bedtime routines, sleep location, or sleep behaviors. By the next assessment (8 weeks), differences began to emerge. Reflecting RP intervention content, more RP infants were usually or always allowed to self-soothe to sleep (put to bed for the night while still awake: 35% vs 16%, P < .001), as opposed to sometimes, rarely, or never.
The more detailed bedtime routine and sleep behavior data collection at ages 16 and 40 weeks revealed many differences between groups (Table 3). As instructed by the nurses, RP infants were more likely to have shorter bedtime routines beginning ≤45 minutes before bed at 16 (51% vs 37%; P = .03) and 40 weeks (57% vs 44%; P = .04). Although there were many similar components of bedtime routines between groups including calm activities, RP infants were more likely to be read to at 16 (47% vs 28%; P = .002) and 40 weeks (61% vs 49%; P = .05). Although nearly all infants were fed as part of their bedtime routine at both 16 and 40 weeks, RP infants were less likely to be fed as the last activity of their bedtime routine at 16 (20% vs 40%; P < .001) and 40 weeks (22% vs 33%; P = .05).
TABLE 3.
Comparison of RP Versus Control on Bedtime Routine and Sleep Behaviors at Ages 16 and 40 Weeks
| 16 wk | 40 wk | |||||
|---|---|---|---|---|---|---|
| RP (n = 134) | Control (n = 128) | P | RP (n = 127) | Control (n = 124) | P | |
| Bedtime routine, % | ||||||
| Duration ≤45 min | 51 | 37 | .03 | 57 | 44 | .04 |
| Components | ||||||
| Read book | 47 | 28 | .002 | 61 | 49 | .05 |
| Rocking | 67 | 59 | .23 | 54 | 54 | .89 |
| Bath | 61 | 55 | .34 | 66 | 69 | .65 |
| Music | 24 | 26 | .57 | 24 | 21 | .59 |
| Watch television | 13 | 12 | .93 | 7 | 12 | .13 |
| Bottle feed/breastfeed | 94 | 90 | .16 | 91 | 92 | .85 |
| Fed as last activity before bed | 20 | 40 | <.001 | 22 | 33 | .05 |
| Cereal in bottle | 13 | 18 | .37 | 15 | 14 | .86 |
| Sleep location and behaviors, % | ||||||
| Bedtime 8 pm or earlier | 46 | 24 | <.001 | 66 | 47 | .002 |
| Sleeps in own room | 59 | 55 | .65 | 80 | 83 | .37 |
| Falls asleep swaddled | 33 | 20 | .01 | 2 | 1 | .57 |
| Falls asleep with pacifier | 36 | 31 | .46 | 35 | 32 | .66 |
| Falls asleep with white noise | 30 | 25 | .42 | 34 | 21 | .02 |
| Falls asleep being held | 36 | 48 | .06 | 21 | 38 | .004 |
| Falls asleep alone in room, in crib (self-soothes) | 44 | 28 | .009 | 59 | 46 | .04 |
| Falls asleep in ≤15 min | 66 | 55 | .07 | 75 | 64 | .06 |
| Night waking, % | ||||||
| ≥2 per night | 37 | 33 | .53 | 28 | 32 | .50 |
| ≥2 night feedings | 34 | 30 | .50 | 14 | 15 | .70 |
| Parenting strategies | ||||||
| Give few minutes to fall back to sleep | 56 | 45 | .09 | 57 | 56 | .93 |
| Pick up and hold/rock back to sleep | 35 | 36 | .76 | 33 | 48 | .02 |
| Rub/pat but do not pick up | 24 | 19 | .29 | 48 | 27 | <.001 |
| Feed back to sleep | 54 | 72 | .002 | 24 | 41 | .005 |
| Give pacifier | 41 | 38 | .50 | 40 | 35 | .42 |
| Change diaper | 65 | 64 | .86 | 35 | 37 | .82 |
| Dream feeds | 39 | 19 | <.001 | 25 | 10 | .001 |
All analyses used χ2 or Fisher exact tests as appropriate.
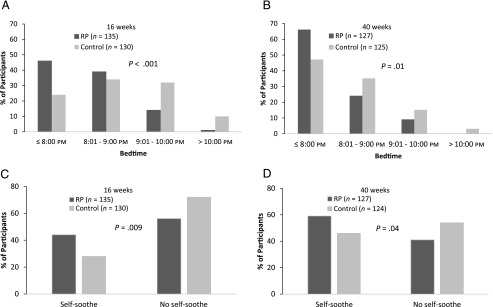
Again reflecting intervention content, RP infants had earlier bedtimes (Fig 1). At 16 weeks, 46% of RP infants went to bed by 8 pm versus 24% of controls (P < .001); the disparity was 66% vs 47% at 40 weeks (P = .002). RP infants were less likely to fall asleep being held at either time point (16 weeks: 36% vs 48%; P = .06; 40 weeks: 21% vs 38%; P = .004) and more likely to self-soothe so sleep (16 weeks: 44% vs 28%; P = .009; 40 weeks: 59% vs 46%; P = .04). RP infants were more likely to be swaddled at 16 weeks (33% vs 20%; P = .01) and listen to white noise at 40 weeks (34% vs 21%; P = .02), whereas pacifier use was similar between groups at both assessment points. RP mothers were also marginally more likely to report that their infants fell asleep within 15 minutes of being put to bed (16 weeks: P = .07; 40 weeks: P = .06).
FIGURE 1.
Intervention effects on bedtime and infant self-soothing to sleep at 16 and 40 weeks.
Data from the abbreviated BISQ at age 1 year indicated that 61% of RP infants were in bed by 8 pm versus 52% for controls (P = .11). Although this did not reach statistical significance, RP mothers reported using the same bedtime routine every night (55% vs 34%; P = .001), a finding supported by the Bedtime Routines Questionnaire, which demonstrated more consistency for the RP group overall (P = .02) and on Routine Behaviors (P = .05) and Routine Environment (P = .03) subscales.
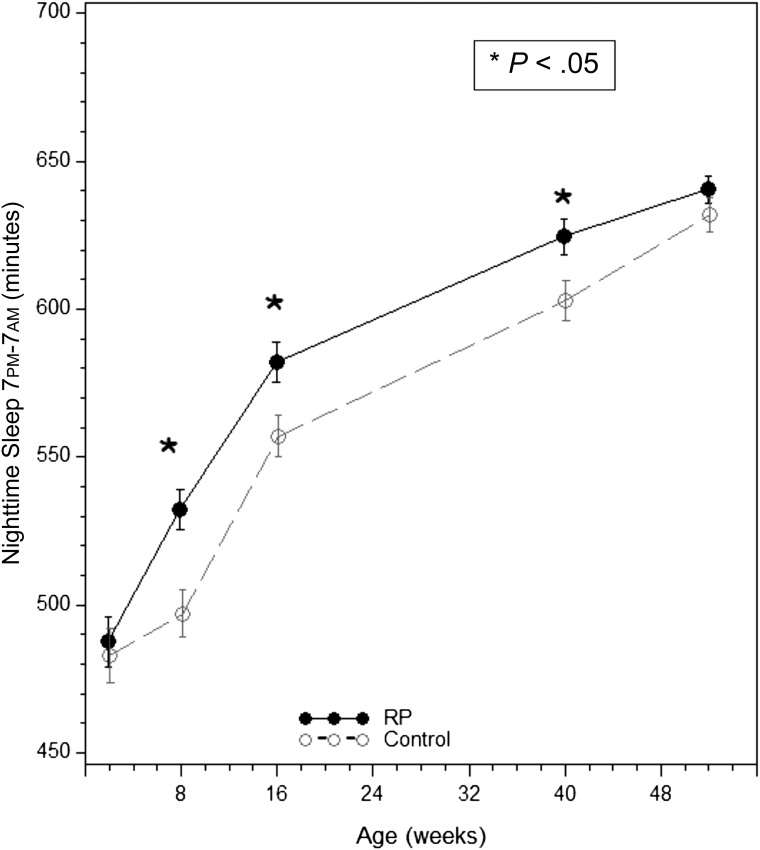
Sleep Duration
At baseline 2 weeks after birth, mean (SD) nighttime, daytime, and total sleep durations in minutes for the entire study cohort were 485.4 (98.4), 464.9 (99.8), and 951.4 (151.0), respectively, with no study group differences (Fig 2). After interventions were initiated, however, there were significant group differences in reported sleep duration. At 8 weeks, total daily sleep duration was marginally longer in RP infants versus control infants (866.3 ± 130.3 vs 839.2 ± 146.6; P = .10). The intervention affected nighttime sleep specifically; RP group infants slept an average of 532.3 (76.0) minutes overnight compared with 497.2 (90.5) minutes in the control group (P < .001). At 16 weeks, a marginally significant disparity for total 24-hour sleep duration favored the RP group (808.8 ± 109.3 minutes vs 785.3 ± 110.2 minutes; P = .08) with differences explained by the significantly longer nighttime sleep duration (582.1 ± 79.5 minutes vs 557.2 ± 78.6 minutes; P = .01). By age 40 weeks, nighttime sleep remained longer for the RP group (624.6 ± 67.6 minutes vs 602.9 ± 76.1 minutes; P = .01), but no differences were detected in total 24-hour sleep between groups. There were no intervention effects on daytime sleep at any time point. At age 1 year, daytime and nighttime sleep durations were similar between study groups, although RP infants were marginally more likely to sleep the recommended 12 to 14 hours per day (odds ratio: 1.89, 95% confidence interval: 0.95–3.78). There was no interaction between feeding mode (breastfeeding vs formula feeding) and study group on sleep duration at any study assessment point.
FIGURE 2.
Total nighttime sleep duration (7 pm–7 am) by study group.
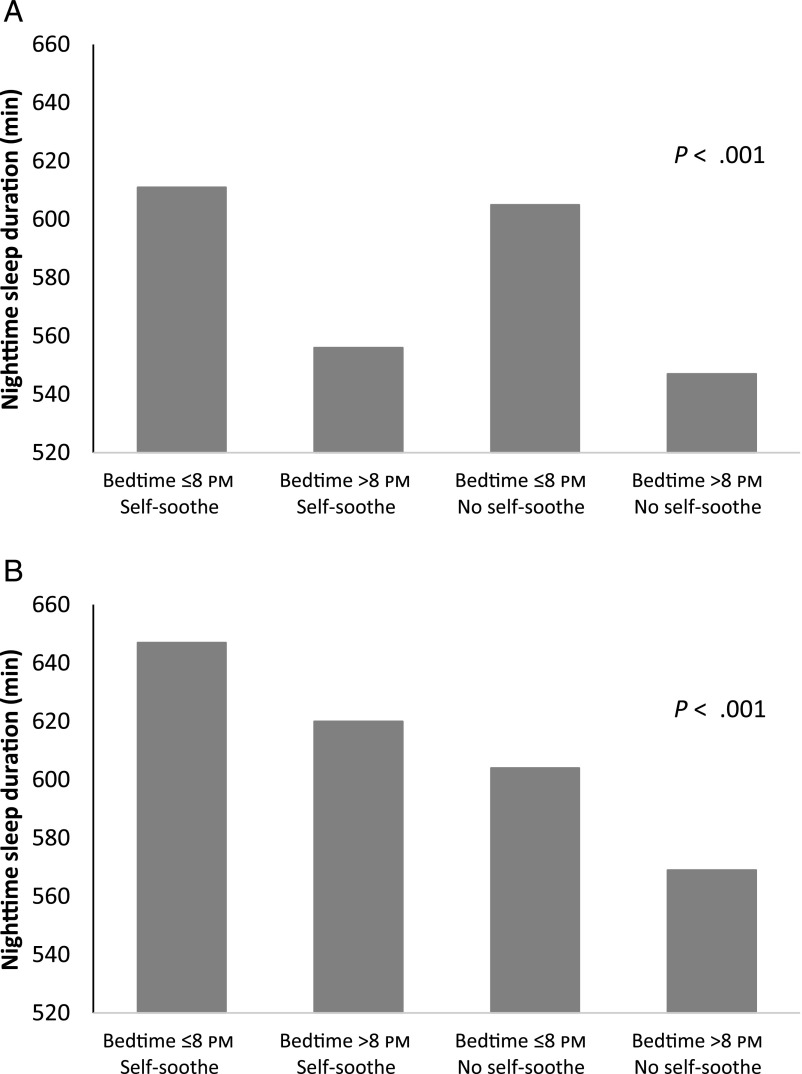
Sleep-related parenting behaviors that were a focus of the RP intervention were associated with increased nighttime sleep duration among the total sample (Fig 3). In particular, 16-week nighttime sleep duration was longest for infants put to bed by 8 pm, regardless of intervention group (607.1 vs 550.0 minutes, P < .001). At 40 weeks, infants self-soothing to sleep and who had a bedtime at 8 pm or earlier slept on average 78 minutes longer at night than those who did not self-soothe and had a bedtime later than 8 pm (P < .001).
FIGURE 3.
Independent and combined effects of bedtime and self-soothing to sleep on nighttime sleep duration among total sample at ages (A) 16 weeks and (B) 40 weeks.
Night Waking and Feeding
At the 2-week baseline and 8-week assessments, no differences existed in parental response to night wakings or number of nighttime feedings. Although night waking and feeding at night were also similar between groups at 16 and 40 weeks, those in the RP group were more likely to “dream feed” (P < .001 and P = .001, respectively), a nighttime feed initiated by the parent before the parent’s bedtime (RP intervention suggestion for infants <4 months). Parenting behaviors in response to night awakenings also differed; consistent with intervention content, RP mothers were less likely to report feeding their infant back to sleep at 16 (54% vs 72%; P = .002) and 40 weeks (24% vs 41%; P = .005). Finally, at 40 weeks, these parents were more likely to report soothing their child with methods other than picking up and holding/rocking their infant to sleep.
Across study groups, self-soothing to sleep and earlier bedtimes predicted fewer night waking, fewer nighttime feeds, and less time awake at night. At 16 weeks, those with bedtimes after 8 pm who did not self-soothe to sleep woke and fed nearly twice as often as those with earlier bedtimes who self-soothed to sleep (1.85 vs 0.95 wakings, 1.70 vs 0.81 feeds; P < .001 for both). At 40 weeks, bedtime was not associated with nighttime feedings or wakings, but self-soothing to sleep was associated with reduced wakings (1.38 vs 0.88; P < .001) and feeds (0.89 vs 0.49; P = .001) compared with those not self-soothing to sleep. Alternatively, those who had bedtime by 8 pm and self-soothed to sleep had less time awake at night compared with those who did not engage in these behaviors (38 vs 85 minutes; P < .001).
Discussion
The INSIGHT RP intervention promoted developmentally appropriate bedtime routines, sleep-related behaviors, and sleep duration, particularly nighttime sleep duration for infants in the first year. In addition to longer reported sleep durations at several time points, RP mothers were more likely to report consistent bedtime routines and earlier bedtimes. Their infants were more likely to self-soothe to sleep without being fed and were less likely to be fed back to sleep after night wakings. These findings are consistent with sleep-related content of the RP intervention, which was designed to promote healthy developmental and behavioral outcomes, including the protective effect on rapid infant weight gain and overweight at age 1 year that we recently reported.37
Improving sleep duration and sleep-related behaviors during infancy can affect infant and family well-being in both the short- and long-term. Infant sleep duration has been associated with toddler sleep duration and numerous other health outcomes.17,29 For example, Mindell and Lee reported that longer nighttime sleep duration for infants is associated with improved parental perception of infant mood,38 and difficult bedtimes and short sleep duration affect socioemotional development during the first 2 years and beyond.3,39 Parental mental health is also adversely affected among infants who have difficult bedtimes or do not sleep well.7,8
We included a sleep component in our RP intervention designed for the primary prevention of obesity because previous studies have shown inverse relationships between sleep duration and both dietary intake and weight among infants and young children.10–13,26,40 In an experiment designed to promote longer nighttime sleep among breastfed infants, treatment group participants slept longer at night and had fewer nocturnal feedings than controls.26 Data from the Gemini study also supported the inverse relationship between sleep duration and energy intake by demonstrating that 16-month-old children with short sleep durations consumed more calories at night, mostly from milk, versus their peers who slept longer.40 Recent experimental evidence showed that within individual children, increasing sleep duration resulted in lower energy intake, lower levels of leptin, and lower weight.15 Although the RP intervention increased nighttime sleep duration, it did not reduce nighttime feedings. However, RP group infants were less likely to be picked up, held, and/or fed back to sleep, which is consistent with our objective to reduce feeding as the default response to night waking or other infant distress.
Limitations of this study include maternal self-report of all sleep outcome data.33 However, the BISQ and other sleep questionnaires have shown strong agreement with actigraphy-derived sleep duration.33,41 Next, social desirability may have influenced some of the findings, given that some survey questions mapped directly onto intervention content. Lastly, the population in central Pennsylvania is relatively homogeneous with all participants coming from 1 center.
Even in this relatively homogeneous sample, findings reveal that although a greater proportion of RP mothers were implementing sleep guidance relative to control, a substantial proportion of RP mothers were not, and future research is needed to identify factors associated with uptake as well as barriers to implementing the RP guidance. Future research could address whether key components of the RP sleep intervention could be delivered as anticipatory guidance in a variety of health care settings and whether findings generalize to sociodemographic groups at increased risk for sleep problems and health disparities.
Conclusions
These findings reveal that sleep-related behaviors are modifiable during infancy and that those in the RP intervention had longer nighttime sleep duration. Clinicians can inform parents that simple strategies, including a consistent bedtime by 8 pm and allowing infants to self-soothe to sleep without being held, rocked, or fed, are associated with significantly longer nighttime sleep durations, fewer nighttime wakings and feeds, and less time awake at night. RP, which has been associated with other positive developmental outcomes,42 shows promise for promoting good sleep hygiene and the primary prevention of sleep problems, which could affect related health and wellness outcomes for infants and families.
Acknowledgments
The authors acknowledge Jessica Beiler, MPH, Jennifer Stokes, RN, Patricia Carper, RN, Amy Shelly, LPN, Gabrielle Murray, RN, Heather Stokes, Nicole Verdiglione, Susan Rzucidlo, MSN, RN, Lindsey Hess, MS, Emily Hohman, PhD, Chelsea Rose, PhD, Katherine Balantekin, PhD, RD, Julia Bleser, MS, and Eric Loken, PhD, for their assistance with this project.
Glossary
- BISQ
Brief Infant Sleep Questionnaire
- INSIGHT
Intervention Nurses Start Infants Growing on Healthy Trajectories
- RP
responsive parenting
Footnotes
Dr Paul co-led all aspects of the study concept, design, and analysis and drafted the initial manuscript; Dr Savage contributed to the design of the study, intervention curriculum development, and data analysis and participated in critical revision of the manuscript; Dr Anzman-Frasca contributed to the design of the study and intervention curriculum development and participated in critical revision of the manuscript; Ms Marini contributed to the design of the study, led the data management, performed the data analyses, and participated in critical revision of the manuscript; Dr Mindell contributed to the intervention curriculum development and participated in critical revision of the manuscript; Dr Birch co-led all aspects of the study concept, design, and analysis and participated in critical revision of the manuscript; and all authors approved the final manuscript as submitted.
This trial has been registered at www.clinicaltrials.gov (identifier NCT NCT01167270).
FINANCIAL DISCLOSURE: Dr Mindell serves as a consultant for Johnson & Johnson Consumer Inc. The other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by grant R01DK088244. Additional support was received from the Children’s Miracle Network at Penn State Children’s Hospital. USDA grant 2011-67001-30117 supported graduate students. REDCap support was received from The Penn State Clinical & Translational Research Institute, Pennsylvania State University CTSA, National Institutes of Health/National Center for Advancing Translational Sciences grant UL1 TR000127. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.National Sleep Foundation “Sleep in America” Poll. Washington, DC: National Sleep Foundation; 2004 [Google Scholar]
- 2.Matricciani LA, Olds TS, Blunden S, Rigney G, Williams MT. Never enough sleep: a brief history of sleep recommendations for children. Pediatrics. 2012;129(3):548–556 [DOI] [PubMed] [Google Scholar]
- 3.Sivertsen B, Harvey AG, Reichborn-Kjennerud T, Torgersen L, Ystrom E, Hysing M. Later emotional and behavioral problems associated with sleep problems in toddlers: a longitudinal study. JAMA Pediatr. 2015;169(6):575–582 [DOI] [PubMed] [Google Scholar]
- 4.Ross CN, Karraker KH. Effects of fatigue on infant emotional reactivity and regulation. Infant Ment Health J. 1999;20(4):410–428 [Google Scholar]
- 5.Spruyt K, Aitken RJ, So K, Charlton M, Adamson TM, Horne RS. Relationship between sleep/wake patterns, temperament and overall development in term infants over the first year of life. Early Hum Dev. 2008;84(5):289–296 [DOI] [PubMed] [Google Scholar]
- 6.Moore M, Mindell JA. The impact of behavioral interventions for sleep problems on secondary outcomes in young children and their families. In: Wolfson A, Montgomery-Downs H, eds. Oxford Handbook of Infant, Child, and Adolescent Sleep and Behavior. New York: Oxford Press; 2013:547–557 [Google Scholar]
- 7.Teti DM, Crosby B, McDaniel BT, Shimizu M, Whitesell CJ. Marital and emotional adjustment in mothers and infant sleep arrangements during the first six months. Monogr Soc Res Child Dev. 2015;80(1):160–176 [DOI] [PubMed] [Google Scholar]
- 8.Hall WA, Hutton E, Brant RF, et al. A randomized controlled trial of an intervention for infants’ behavioral sleep problems. BMC Pediatr. 2015;15(1):181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med. 2014;15(12):1456–1462 [DOI] [PubMed] [Google Scholar]
- 10.Fatima Y, Doi SA, Mamun AA. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev. 2015;16(2):137–149 [DOI] [PubMed] [Google Scholar]
- 11.Taveras EM, Rifas-Shiman SL, Oken E, Gunderson EP, Gillman MW. Short sleep duration in infancy and risk of childhood overweight. Arch Pediatr Adolesc Med. 2008;162(4):305–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tikotzky L, DE Marcas G, Har-Toov J, Dollberg S, Bar-Haim Y, Sadeh A. Sleep and physical growth in infants during the first 6 months. J Sleep Res. 2010;19(1 pt 1):103–110 [DOI] [PubMed] [Google Scholar]
- 13.Bell JF, Zimmerman FJ. Shortened nighttime sleep duration in early life and subsequent childhood obesity. Arch Pediatr Adolesc Med. 2010;164(9):840–845 [DOI] [PubMed] [Google Scholar]
- 14.Taveras EM, Gillman MW, Peña MM, Redline S, Rifas-Shiman SL. Chronic sleep curtailment and adiposity. Pediatrics. 2014;133(6):1013–1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hart CN, Carskadon MA, Considine RV, et al. Changes in children’s sleep duration on food intake, weight, and leptin. Pediatrics. 2013;132(6). Available at: www.pediatrics.org/cgi/content/full/132/6/e1473 [DOI] [PubMed] [Google Scholar]
- 16.Woo Baidal JA, Locks LM, Cheng ER, Blake-Lamb TL, Perkins ME, Taveras EM. Risk factors for childhood obesity in the first 1,000 days: a systematic review. Am J Prev Med. 2016;S0749-3797(15)00752-7. [DOI] [PubMed] [Google Scholar]
- 17.Touchette E, Petit D, Paquet J, et al. Factors associated with fragmented sleep at night across early childhood. Arch Pediatr Adolesc Med. 2005;159(3):242–249 [DOI] [PubMed] [Google Scholar]
- 18.Moore T, Ucko LE. Night waking in early infancy. I. Arch Dis Child. 1957;32(164):333–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parmelee AH Jr, Wenner WH, Schulz HR. Infant sleep patterns: From birth to 16 weeks of age. J Pediatr. 1964;65:576–582 [DOI] [PubMed] [Google Scholar]
- 20.Anders TF, Keener M. Developmental course of nighttime sleep-wake patterns in full-term and premature infants during the first year of life. I. Sleep. 1985;8(3):173–192 [DOI] [PubMed] [Google Scholar]
- 21.James-Roberts IS, Conroy S, Hurry J. Links between infant crying and sleep-waking at six weeks of age. Early Hum Dev. 1997;48(1-2):143–152 [DOI] [PubMed] [Google Scholar]
- 22.Glotzbach SF, Edgar DM, Boeddiker M, Ariagno RL. Biological rhythmicity in normal infants during the first 3 months of life. Pediatrics. 1994;94(4 pt 1):482–488 [PubMed] [Google Scholar]
- 23.Joseph D, Chong NW, Shanks ME, et al. Getting rhythm: how do babies do it? Arch Dis Child Fetal Neonatal Ed. 2015;100(1):F50–F54 [DOI] [PubMed] [Google Scholar]
- 24.Anders TF. Night-waking in infants during the first year of life. Pediatrics. 1979;63(6):860–864 [PubMed] [Google Scholar]
- 25.Adair R, Bauchner H, Philipp B, Levenson S, Zuckerman B. Night waking during infancy: role of parental presence at bedtime. Pediatrics. 1991;87(4):500–504 [PubMed] [Google Scholar]
- 26.Pinilla T, Birch LL. Help me make it through the night: behavioral entrainment of breast-fed infants’ sleep patterns. Pediatrics. 1993;91(2):436–444 [PubMed] [Google Scholar]
- 27.Paul IM, Savage JS, Anzman SL, et al. Preventing obesity during infancy: a pilot study. Obesity (Silver Spring). 2011;19(2):353–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mindell JA, Du Mond CE, Sadeh A, Telofski LS, Kulkarni N, Gunn E. Efficacy of an internet-based intervention for infant and toddler sleep disturbances. Sleep. 2011;34(4):451–458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mindell JA, Du Mond CE, Sadeh A, Telofski LS, Kulkarni N, Gunn E. Long-term efficacy of an internet-based intervention for infant and toddler sleep disturbances: one year follow-up. J Clin Sleep Med. 2011;7(5):507–511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paul IM, Williams JS, Anzman-Frasca S, et al. The Intervention Nurses Start Infants Growing on Healthy Trajectories (INSIGHT) study. BMC Pediatr. 2014;14:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Birch LL, Parker L, Burns A, eds. Early Childhood Obesity Prevention Policies. Washington, DC: National Academy of Sciences; 2011 [Google Scholar]
- 32.Karp H. Happiest Baby on the Block: The New Way to Calm Crying and Help Your Baby Sleep Longer New York, NY: Bantam; 2006
- 33.Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004;113(6). Available at: www.pediatrics.org/cgi/content/full/113/6/e570 [DOI] [PubMed] [Google Scholar]
- 34.Karp H. The happiest baby on the block. New York, NY: Bantam Books; 2002 [Google Scholar]
- 35.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Henderson JA, Jordan SS. Development and preliminary evaluation of the bedtime routines questionnaire. J Psychopathol Behav Assess. 2010;32(2):271–280 [Google Scholar]
- 37.Savage JS, Birch LL, Marini M, Anzman-Frasca S, Paul IM. INSIGHT parenting intervention reduces rapid infant weight gain and overweight at age 1 year. JAMA Pediatr. 2016, In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mindell JA, Lee C. Sleep, mood, and development in infants. Infant Behav Dev. 2015;41:102–107 [DOI] [PubMed] [Google Scholar]
- 39.Hysing M, Sivertsen B, Garthus-Niegel S, Eberhard-Gran M. Pediatric sleep problems and social-emotional problems. A population-based study. Infant Behav Dev. 2016;42:111–118 [DOI] [PubMed] [Google Scholar]
- 40.McDonald L, Wardle J, Llewellyn CH, et al. Sleep and nighttime energy consumption in early childhood: a population-based cohort study. Pediatr Obes. 2015;10(6):454–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Werner H, Molinari L, Guyer C, Jenni OG. Agreement rates between actigraphy, diary, and questionnaire for children’s sleep patterns. Arch Pediatr Adolesc Med. 2008;162(4):350–358 [DOI] [PubMed] [Google Scholar]
- 42.Eshel N, Daelmans B, de Mello MC, Martines J. Responsive parenting: interventions and outcomes. Bull World Health Organ. 2006;84(12):991–998 [DOI] [PMC free article] [PubMed] [Google Scholar]