Abstract
Purpose
Pain is multi-dimensional and may be better addressed through a holistic, biopsychosocial approach. Massage therapy is commonly practiced among patients seeking pain management; however, its efficacy is unclear. This systematic review and meta-analysis is the first to rigorously assess the quality of massage therapy research and evidence for its efficacy in treating pain, function-related and health-related quality of life outcomes across all pain populations.
Methods
Key databases were searched from inception through February 2014. Eligible randomized controlled trials were assessed for methodological quality using SIGN 50 Checklist. Meta-analysis was applied at the outcome level. A diverse steering committee interpreted the results to develop recommendations.
Results
Sixty high quality and seven low quality studies were included in the review. Results demonstrate massage therapy effectively treats pain compared to sham [standardized mean difference (SMD) = −.44], no treatment (SMD = −1.14), and active (SMD = −0.26) comparators. Compared to active comparators, massage therapy was also beneficial for treating anxiety (SMD = −0.57) and health-related quality of life (SMD = 0.14).
Conclusion
Based on the evidence, massage therapy, compared to no treatment, should be strongly recommended as a pain management option. Massage therapy is weakly recommended for reducing pain, compared to other sham or active comparators, and improving mood and health-related quality of life, compared to other active comparators. Massage therapy safety, research challenges, how to address identified research gaps, and necessary next steps for implementing massage therapy as a viable pain management option are discussed.
Keywords: Systematic Review, Meta-Analysis, Massage Therapy, Pain, Function, Health-Related Quality of Life
Introduction
Public Health Significance of Pain
Pain is currently recognized as the most compelling reason for an individual to seek medical attention from a general practitioner, and accounts for approximately 80% of physician visits [1,2]. It is often represented as a complex process, affecting individuals differently as the severity, frequency, and duration of pain conditions can vary within each condition [3,4]. Pain is an experience that is multi-dimensional; not only does it impact individuals physically, but also socially, mentally, emotionally, and spiritually [1,5,6]. As pain persists and worsens, it can interfere with daily activities, significantly impair performance of social responsibilities in work and family life, and negatively affect psychological health and quality of life. In fact, evidence supports the close interaction between pain and various function outcomes (e.g., functional, emotional, psychosocial domains) which often affect and intensify each other [7–16]. Effective pain management thus requires therapies that treat both pain and related sequela by addressing the whole patient through a holistic biopsychosocial model.
Massage Therapy for Pain
There has been a rise in the use of complementary and integrative medicine (CIM) therapies [17,18] due to the high prevalence of pain, unsatisfactory results from conventional pain treatment, and the need to address the whole patient. One of the most prevalent and popular CIM treatments is massage therapy, which involves the manipulation of soft-tissue to alleviate pain and discomfort [19]. In addition to physical relaxation, proponents of massage therapy claim that it promotes mental relaxation and addresses the psychological aspects of the patients’ health conditions [20]. Integration of massage therapy in acute care hospital settings has been shown to effectively enhance patients’ ability to cope with both physical and emotional aspects of pain [21]. Massage therapy is also widely used and sought after, because while it is not totally devoid of risks or complications, it is generally recognized as a safe therapeutic modality with few risks or adverse effects [22].
Despite its popularity and wide use, there continues to be ongoing debate regarding the efficacy of massage therapy for pain. In a 2013 systematic review, Kumar et al. concluded that there is an emerging body of evidence to support massage for low back pain but because of the lack of methodological rigor in the primary research interpretation should be cautioned [23]. Similarly, in the 2010 systematic review exploring manual therapies, Bronfort et al. emphasized the importance of methodological quality and concluded that there exists moderate quality of evidence for massage on chronic low back and neck pain [24]. In 2015, Furlan et al. concluded that the quality of the evidence was “low to very low” in support of massage being effective for reducing pain and improving function [25]. Additional reviews exist on specific types of massage with various specific pain conditions, each with varying levels of evidence being reported [26–28].
Research highlights the challenges within this field, the diversity of types of massage therapies and comparators being used, and the heterogeneity of their therapeutic effects [29]. In 2010, the Pain Management Task Force (PMTF) identified massage therapy as one of the integrative therapies most ready for implementation based on current literature regarding efficacy, safety, and acceptability as well as licensing and credentialing concerns. They maintained, however, that there are still key questions (e.g., whether it is safe, whether it works for the purposes for which it is used) that have yet to be answered through well-designed scientific studies [30]. With the move toward more patient-centric healthcare, and the realization that pain affects the whole person and needs to be addressed in a more holistic fashion, there is a need to confirm the efficacy of massage therapy for treating patient-reported function-related outcomes across all pain populations to better inform clinicians, healthcare practice and policies as to whether massage therapy can be considered as a therapeutic option for pain management.
Purpose
This systematic review and meta-analysis provides an objective and transparent analysis of the research on massage therapy for treating patient-reported functional outcomes related to individuals experiencing pain from a whole person perspective. This analysis was designed to contribute to the field in the following ways: (a) begin to more clearly define concepts of massage therapy and function as it relates to pain and other clinical outcomes in order to guide future research; (b) determine the efficacy of massage therapy for treating individuals who would typically visit their general health practitioner with complaints of pain (e.g., patients diagnosed with various pain conditions across the spectrum of acute to chronic pain) that is affecting function-related (e.g., pain intensity/severity, activity, sleep, mood, stress) and other (e.g., health-related quality of life, pain pressure threshold, physiological outcomes) outcomes of daily life; (c) describe the characteristics and safety issues of massage therapy currently reported in the literature; (d) propose a recommended set of Standards for Reporting Interventions in Clinical Trials of Massage (STRICT-M) and analyze these criteria to guide future work and replicability; (e) synthesize the evidence to draw conclusions based on the current state of the science from which recommendations can be made for its application; and (f) identify gaps in order to guide a future research agenda.
Methodology
Overview of Methodological Approach
A systematic review and meta-analysis was conducted using Samueli Institute’s systematic review process known as the Rapid Evidence Assessment of Literature (REAL©) [31], which has been used by a variety of organizations to date [32–36]. Specifically, (a) the Evidence for Massage Therapy (EMT) Working Group, composed of a diverse group of stakeholders including a full steering committee and subject matter experts, contributed to defining the review’s protocol to maximize the meaning and impact; (b) the systematic review team followed the protocol to independently evaluate the quantity and quality of the available English, peer-reviewed literature in order to (c) present the results to the EMT Working Group who then interpreted the evidence to suggest recommendations for the field. The protocol for this systematic review is registered with PROSPERO under registration number CRD42014008867.
Concepts and Definitions
Pain
For purposes of this review, the authors considered pain as an unpleasant sensory and emotional acute or chronic subjective experience associated with actual or potential tissue damage or described in terms of such damage [30].
Function
Given the multi-dimensionality of pain and its subsequent effect on various function-related outcomes, the authors believe it is important to address pain through a biopsychosocial approach to best address the whole patient. In fact, a number of outcome tools are beginning to address pain in this manner [37–39]. As such, the authors view function as also encompassing pain, activity, sleep, mood and stress, as well as health-related quality of life (HrQoL), pain pressure threshold and physiological (i.e., outcomes relating to one’s physiology including the physical and chemical phenomena and processes involved) outcomes.
Massage Therapy
The authors reviewed various definitions and taxonomies of massage therapy in order to propose a common language system [28,29,40–43] through the following definition:
The systematic manipulation of soft tissue with the hands that positively affects and promotes healing, reduces stress, enhances muscle relaxation, improves local circulation, and creates a sense of well-being.
Study Eligibility Criteria
Articles were included if they met all of the following criteria: (a) human population experiencing pain as defined above; (b) massage therapy, as defined above, administered (i) alone as a therapy; (ii) as part of a multi-modal intervention where massage effects can be separately evaluated; or (iii) with the addition of techniques commonly used with massage, as pre-defined by the EMT Working Group (i.e., external application of water, heat, cold, lubricants, background music, aromas, essential oils, and with the addition of tools that may mimic the actions that can be performed by the hands); (c) sham, no treatment or active comparator (i.e., those in which participants are actively receiving any type of intervention); (d) assessment of at least one relevant functional outcome (as defined above), and; (e) the study being a peer-reviewed randomized controlled trial (RCT) study design published in the English language. Additionally, interventions were included if they were not necessarily labeled as massage or massage therapy but included the use of manual forces and soft-tissue deformation as well as gliding, torsion, shearing, elongation, oscillating, percussive, and joint movement methods (i.e., touch, compression, gliding, percussion, friction, vibration, kneading, movement, positioning, stretching, holding). Note that interventions solely performed by tools (e.g., chair massage) were excluded.
Search Strategy
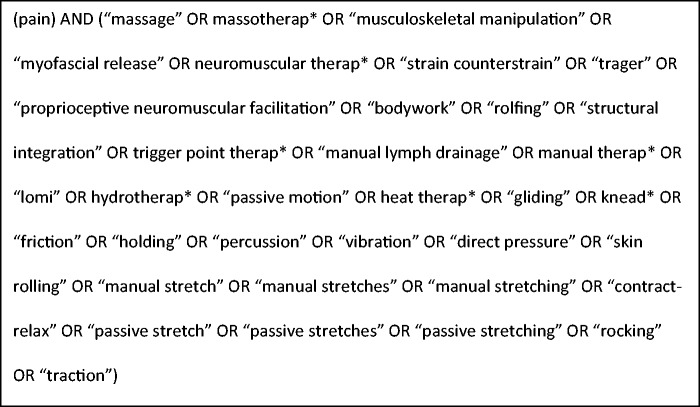
PubMed, CINAHL, Embase, and PsycInfo, were searched from database inception through February 2014. Authors explored MeSH within MEDLINE and consulted with subject matter experts to develop the search strategy (see Figure 1 for PubMed search string).
Figure 1.
PubMed search string.
Study Selection
Four reviewers (LX, AP, CP, EY) relied upon the eligibility criteria to independently screen titles and abstracts yielded from the search. A Cohen’s kappa for inter-rated agreement of > 0.90 was maintained throughout the review. Disagreements about inclusion were resolved through discussion and consensus, by one of the review managers (CB, CC) or, ultimately, by the EMT Working Group.
Methodological Quality Assessment and Data Extraction
Methodological quality (i.e., risk of bias/internal validity) was independently assessed by four reviewers (LX, AP, CP, EY) using the Scottish Intercollegiate Guidelines Network (SIGN) 50 Checklist [44] for RCTs, a validated and reliable assessment tool widely used in the literature. External and model validity was assessed using the External Validity Assessment Tool (EVAT©) [45] which measures the generalizability of research to other individuals (i.e., external validity) and other settings (i.e., model validity) outside the confines of a study.
Data was extracted to describe each included study according to the pain condition, sample entered/completed, intervention and control/comparison description and dosage, relevant function measures and corresponding results and statistics, effect size calculations, and author’s main conclusions. The authors also noted whether power calculations to achieve sufficient effect sizes and adverse events were reported. Mobius Analytics Systematic Review System (Mobius Analytics Inc, Ottawa, Ontario) was utilized for all data entry and execution of the systematic review.
Proposed STRICT-M Checklist and Analysis
The Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) [46] is a formal extension of the Consolidated Standards of Reporting Trials (CONSORT) Statement [47] that expands the general content of the intervention description specific to acupuncture. It is designed to improve the completeness of reporting interventions in controlled acupuncture trials so that such trials can provide a transparent account of both acupuncture and control/comparison protocols. The authors adapted STRICTA criteria to relate to massage therapy interventions, and performed an analysis across these criteria. Specifically, the criteria addresses design elements such as the intervention’s rationale, technique, treatment regimen and dosing; other components of treatment; practitioner background; and control/comparator interventions deemed important for quality control of massage therapy studies. The authors refer to this as a proposed Standards for Reporting Interventions in Clinical Trials of Massage (STRICT-M) Checklist.
Data Synthesis and Analysis
Meta-Analysis
When reported, the sample size, mean or pre-post difference, and standard deviation for each treatment group was extracted. Effect sizes were calculated for each comparison (i.e., massage vs. active comparator, massage vs. sham, and massage vs. no treatment) for the following outcomes: pain intensity/severity, activity, stress, mood (i.e., anxiety), sleep (i.e., fatigue), and HrQoL, where available. If a study had more than one active comparator (e.g., physical therapy and acupuncture), the biostatistician randomly chose one active comparator for analysis by flipping a coin. A minimum of three studies was required to perform a meta-analysis for each subset of data. An unbiased estimate was calculated using the Cohen’s d effect size for subgroup analyses that pooled data across several scales [48,49]. A pooled random-effects estimate of the overall effect size was estimated for all studies judged clinically similar enough to warrant a meta-analysis. The individual trial outcomes were weighted by both within- and between-study variation in this synthesis. For a reduction in pain intensity/severity, anxiety, and fatigue outcomes, a negative effect size favors the massage therapy treatment group. For improved activity (i.e., increase in range of motion) and HrQoL, a positive effect size favors the massage therapy treatment group. Publication bias was assessed using the Egger regression asymmetry test [50,51]. Heterogeneity was assessed using l2 and tested via Q statistics. For pain intensity/severity, a clinical translation into the Visual Analogue Scale (VAS), 0-100, was conducted for clinical interpretation using a standard deviation of 25 points. The authors considered a 20-mm difference on the VAS as clinically relevant [52]. These translations should be interpreted with caution. All meta-analyses were conducted with Comprehensive Meta-analysis version 2.2 (Meta-Analysis.com, Englewood, NJ).
Evidence Synthesis
The EMT Working Group and systematic review team convened to review the evidence from the systematic review and meta-analysis, in order to grade the (i) confidence in the estimate of the effect; (ii) magnitude of the effect; and (iii) safety as being reported in the results; and provide an overall recommendation concerning the benefit/risk for massage therapy. The conclusions reached and recommendations made are in no way to be construed as clinical practice guidelines, but rather recommendations about the benefit/risk of massage therapy based solely on the evidence garnered from the systematic review.
Results
Characteristics of Included Studies
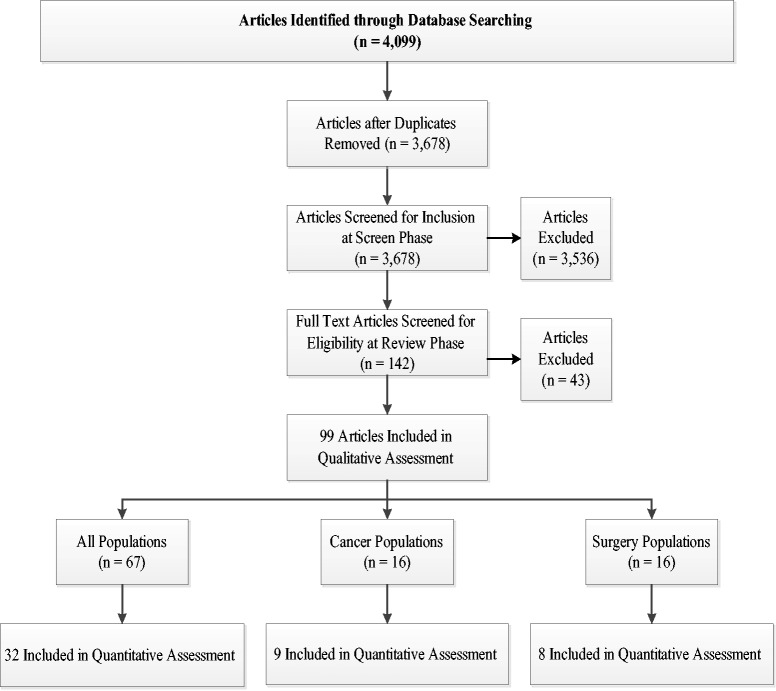
Out of the 3,678 articles yielded from the search strategy, 67 articles met the systematic review’s inclusion criteria and included populations that would typically seek a primary healthcare physician for support related to pain. In addition, 16 studies on cancer and 16 studies on surgical pain populations emerged from the initial search, and are reported on in subsequent articles within this series [53,54] (see Figure 2 for Flow Chart).
Figure 2.
Flow chart.
The 67 included articles were published between the years of 1999–2013, and investigated the use of massage therapy on musculoskeletal pain, headache, visceral pain, chronic pain, including fibromyalgia, spinal cord pain, and venous insufficiency populations. Massage techniques were performed by at least one practitioner or therapist and primarily consisted of massage therapy, myofascial release therapy, traditional Thai massage, and ischemic compression compared to a variety of active (e.g., joint manipulation, physical therapy, acupuncture), sham, or no treatment controls. Studies measured the efficacy of massage on pain, activity, sleep, mood, stress, HrQoL, pain pressure threshold and physiological outcomes. Treatment dosages varied from a single 1.5 minute session to a total of 40–60-minute daily sessions over the course of 20 weeks. Among the 67 studies, 32.2% of the participants were male and 67.8% were female with a mean age of 42.7 years (range = 20–83 years across studies). See Supplementary Data, Table S1 for characteristics of included studies as detailed above.
Methodological Quality of Included Studies
According to the SIGN 50 criteria used to assess the risk of bias, the majority (n = 60) of studies were considered to be high ( ++, n = 10) or acceptable (+, n = 50) quality, with seven low (0) quality studies. Most articles addressed an appropriate and clearly focused question, randomization, dropout rates, baseline similarities, group differences, outcome reliability, and validity adequately or well. Criteria surrounding allocation concealment and intention-to-treat analyses, however, were mostly poorly addressed, indicating that the authors of these reports failed either to successfully carry out, or to describe these processes at all. Of the six multi-site studies [55–60], most (n = 5) addressed site similarities well, with only one doing so adequately. See Table 1 for full methodological assessment results.
Table 1.
SIGN 50 checklist quality assessment [44]
| Percentage (N) |
|||
|---|---|---|---|
| SIGN Criteria | Poor | Adequate | Well |
| Appropriate and clearly focused question | – | 70.1% (47) | 29.9% (20) |
| Randomization | 38.8% (26) | 22.4% (15) | 38.8% (26) |
| Allocation concealment | 65.7% (44) | 20.9% (14) | 13.4% (9) |
| Percentage of dropouts | 16.4% (11) | 10.5% (7) | 73.1% (49) |
| Baseline similarities | 1.5% (1) | 16.4% (11) | 82.1% (55) |
| Group differences | 13.4% (9) | 76.1% (52) | 10.5% (7) |
| Outcome reliability/validity | 10.4% (7) | 26.9% (18) | 62.7% (42) |
| Intention-to-treat analyses | 56.7% (38) | 14.9% (10) | 28.4% (19) |
| Multi-site similarities | – | 16.7% (1) | 83.3% (5) |
SIGN = Scottish Intercollegiate Guidelines Network.
SIGN criteria was modified to exclude blinding and was weighted accordingly because of this.
EVAT measures the source population, recruitment and model validity in terms of the reporting of staff, places and facility descriptions. Overall, the majority of studies described recruitment (73.1%) and participation (58.8%) aspects of external validity adequately in that the populations being studied and the source from which they came are understood well enough that results can be generalized to other patients in real-life settings. Conversely, most (71.4%) studies described model validity poorly making it difficult to understand the staff, places and facilities being used in these studies. See Table 2.
Table 2.
EVAT quality assessment [45]
| Percentage (N) |
||||
|---|---|---|---|---|
| Poor | Adequate | Well | NA | |
| Recruitment | 23.9% (16) | 73.1% (49) | 3.0% (2) | (0) |
| Participation | 21.6% (11) | 58.8% (30) | 19.6% (10) | (16) |
| Model validity | 71.4% (30) | 19.1% (8) | 9.5% (4) | (25) |
EVAT = External Validity Assessment Tool.
STRICT-M Analysis
According to the proposed STRICT-M requirements (see Table 3) the majority of studies addressed the massage rationale (62.7%), as well as the particular massage technique used within the studies (98.5%), with many including specific massage terms (56.7%), and describing both the amount of pressure applied (52.2%) and location (82.1%) of massage. The amount of time spent massaging each location (34.3%) as well as the response sought (22.4%) were not reported by many. Although dosing varied widely across studies, it was well-reported by many studies including the specified number (89.6%) and frequency (67.2%) of treatment sessions over a specified time frame (83.6%) as well as the duration of each individual treatment session (74.6%).
Table 3.
STRICT-M analysis
| Percentage (N) | |
|---|---|
| 1. Massage Rationale | |
| a. Reasoning for treatment provided | 62.7% (42) |
| b. Extent to which treatment varied | 59.7% (40) |
| 2. Details of Massage Technique | |
| a. Name and description of massage technique | 98.5% (66) |
| b. Details of intervention using terms | 56.7% (38) |
| c. Location of massage | 82.1% (55) |
| d. Amount of time spent massage each location | 34.3% (23) |
| e. Description of pressure | 52.2% (35) |
| f. Response sought | 22.4% (15) |
| 3. Treatment Regimen Related to Dosing | |
| a. Number of treatment sessions over what time | 89.6% (60) |
| b. Time frame (total duration) | 83.6% (56) |
| c. Frequency | 67.2% (45) |
| d. Duration of each treatment | 74.6% (50) |
| 4. Other Components of Treatment | |
| a. Details of massage-related interventions | 76.9% (10 out of 13) |
| b. Massage equipment | – |
| c. Setting | 43.3% (29) |
| 5. Practitioner Background | |
| a. Type of practitioner | 95.5% (64) |
| b. Qualifications | 14.9% (10) |
| 6. Control or Comparator Interventions | |
| a. Rationale for control | 32.8% (22) |
| b. Name and description of control | 89.6% (60) |
| c. Number of control sessions | 52.2% (35) |
| d. Time frame (total duration) | 52.2% (35) |
| e. Frequency | 41.8% (28) |
| f. Duration of each treatment | 49.3% (33) |
76.9% of the studies that used additional massage-related interventions, per the authors’ definition (i.e., heat therapy, aromatherapy, essential oils, breathing exercises, music, relaxation, wrist splint), described these interventions well. Setting was described by less than half of the studies (43.3%). Though massage was primarily performed in a clinic (n = 14), private practice (n = 8), or hospital/medical center (n = 5) setting, massage was also offered at home (n = 3), work (n = 1), and rehabilitative settings (n = 2).
Twenty-three studies included only one provider, while 24 included more than one provider and 20 did not specify the number of study providers. Of those that included more than one provider, 17 specified the exact number of providers, which ranged from two to 27 individuals, while seven did not report such specifics. The number of providers per site and interaction between multiple providers was only described by three studies; practitioners in one study were responsible for providing all treatments for their assigned patient, while other studies included a mix of providers who were responsible for treatments, evaluations or for serving as a backup therapist.
Almost all studies described the type of massage practitioner (95.5%); however, provider qualifications were only described by 14.9% of studies. Most practitioners were massage therapists (n = 24), physical/physiotherapists (n = 14), or some type of unspecified therapist (n = 9); other types of practitioners included doctors/physicians (n = 5), examiners/operators (n = 5), nurses (n = 4), chiropractors (n = 3), as well as a teacher with assistants (n = 1). Based on the few studies that reported practitioner qualifications, years’ experience ranged from 5 to 15 years and practitioners underwent anywhere from 25 to 95 hours of supervised clinical experience and 450 to 950 hours of didactic training; most practitioners also received anywhere from one to eight hours of training in their respective study’s particular protocol.
Control or comparator interventions were named and described (89.6%) by many studies; although the number of sessions (52.2%) and total study duration (52.2%) were reported by several studies, the rationale (32.8%), frequency (41.8%), and duration of treatment (49.3%) were described by less than half the studies.
Adverse Events
Based on a review of the literature, massage is generally a safe intervention. Most reported adverse events are minor and have low incident rates [22]. The most common adverse events associated with massage include increased pain, muscle soreness, and stiffness [61]. Of the 67 studies included for review, 24 addressed adverse events in their reports. Eleven [56–58,62–69] reported specific adverse events and 13 [59,60,70–80] reported no adverse events occurred. Reported adverse events included soreness, pain, nausea, discomfort, sweating, and low blood pressure. Only one study [56] reported pain as a serious adverse event. Two studies [63,66] reported serious adverse events (i.e., nausea, shortness of breath, chest pain, prolapsed intervertebral disc) that were considered unrelated to the treatment condition in the report.
Evidence Synthesis
Thirty-two studies provided sufficient data to be included and pooled in the meta-analysis. The meta-analysis assessed the effect on musculoskeletal pain populations across outcomes related to pain, activity, anxiety and HrQoL and compared (a) massage vs. sham, (b) massage vs. no treatment, and (c) massage vs. other active comparator(s). Treatment comparators used for meta-analysis are denoted beside the author names in the forest plots (see Figures 3A–H for plotted meta-analysis results). Publication bias was assessed across all subgroup analyses and while this does not appear to be a concern, it cannot be ruled out due to the small number of trials pooled across subgroups (see Figures 3A–H for Egger’s test p-values). Only one study included in the pooled analyses was of low methodological quality. Because of this, no sensitivity analysis for methodological quality was conducted for the meta-analysis; overall quality was accounted for across all studies for the entire systematic review during synthesis and interpretation to determine the confidence in the estimate of the effect (Table 4). Because there were not sufficient numbers available for pooling across populations experiencing headache, visceral pain, chronic pain or fatigue (e.g., fibromyalgia), spinal cord pain, and venous insufficiency, effect sizes for pain were calculated for individual studies, within these subgroups, that had relevant, available data (see Supplementary Data Table S1). All studies examining the efficacy of massage therapy in musculoskeletal pain populations, regardless of whether they were included in the meta-analysis, were considered for the overall evidence synthesis. The synthesis was performed in categories with at least three studies (see Table 4).
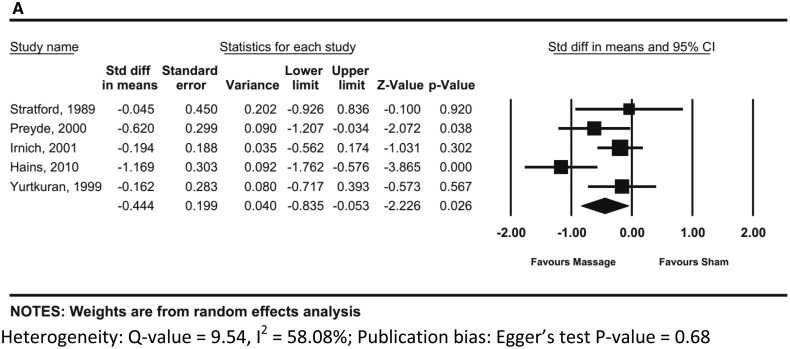
Figure 3A.
Results of massage vs. sham meta-analysis for musculoskeletal pain populations: pain intensity/severity at post-treatment (sample size analyzed, N = 290).
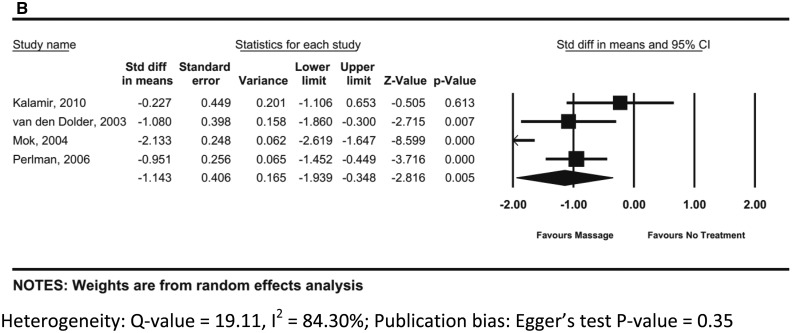
Figure 3B.
Results of massage vs. no treatment meta-analysis for musculoskeletal pain populations: pain intensity/severity at post-treatment (sample size analyzed, N = 219).
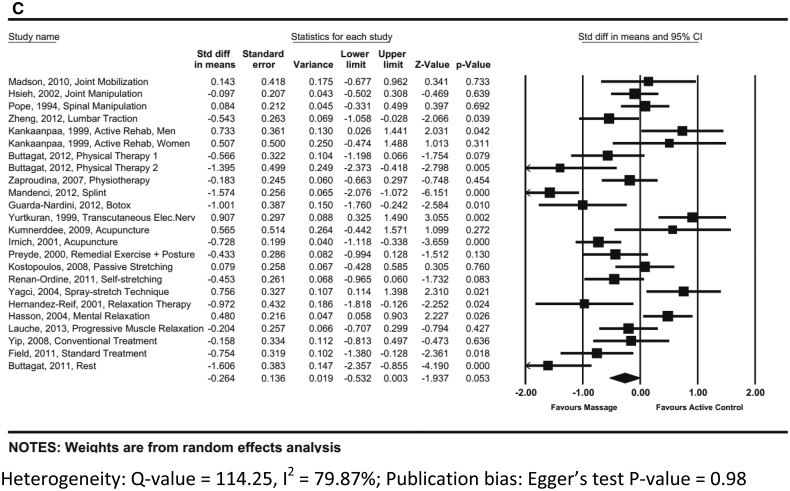
Figure 3C.
Results of massage vs. active comparator(s) meta-analysis for musculoskeletal pain populations: pain intensity/severity at post-treatment (sample size analyzed, N = 1349).
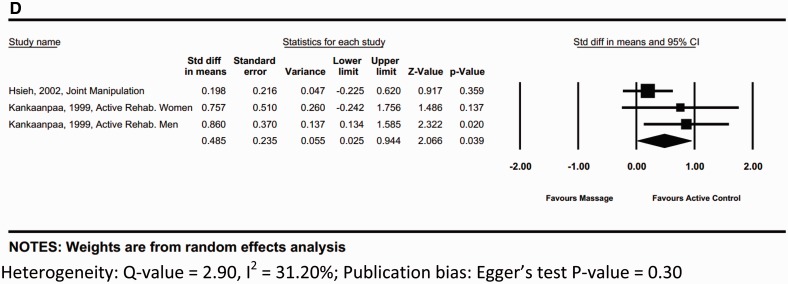
Figure 3D.
Results of massage vs. active comparator(s) meta-analysis for musculoskeletal pain populations: pain intensity/severity at a 6-month follow-up (sample size analyzed, N = 136).
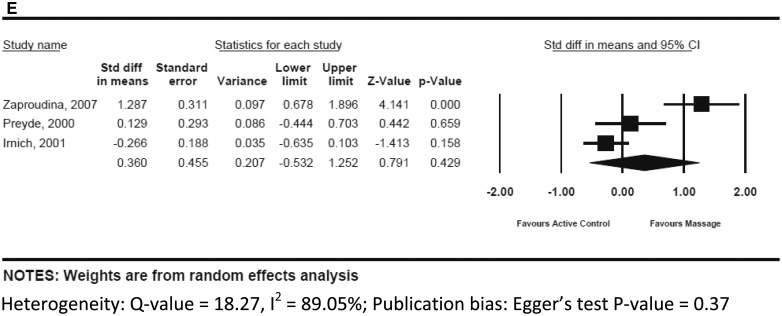
Figure 3E.
Results of massage vs. sham meta-analysis for musculoskeletal pain populations: activity (range of motion) at post-treatment (sample size analyzed, N = 211).
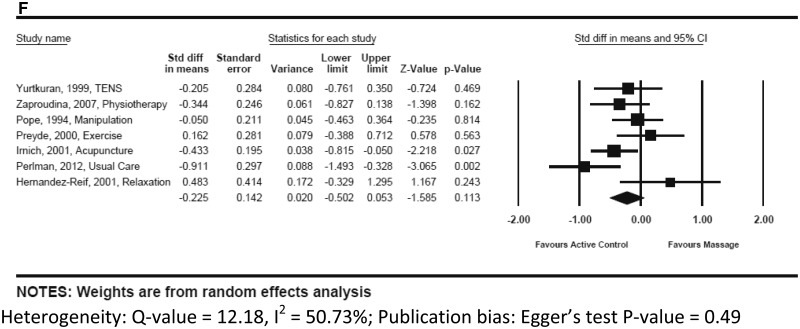
Figure 3F.
Results of massage vs. active comparator meta-analysis for musculoskeletal pain populations: activity (range of motion) at post-treatment (sample size analyzed, N = 450).
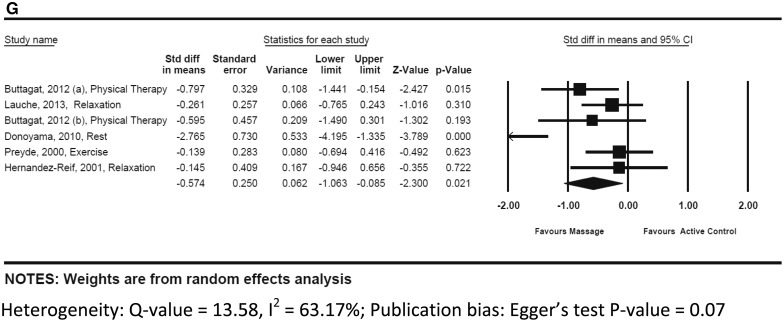
Figure 3G.
Results of massage vs. active comparator(s) meta-analysis for musculoskeletal pain populations: mood (anxiety) at post-treatment (sample size analyzed, N = 210).
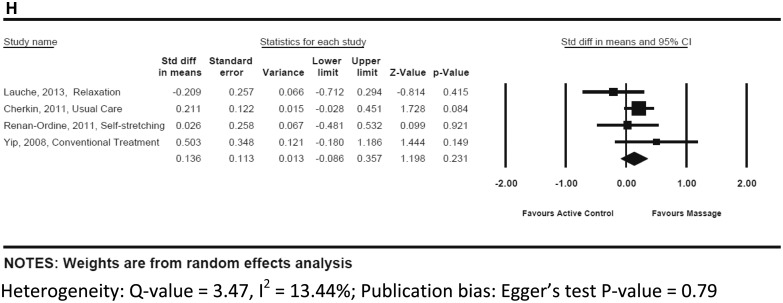
Figure 3H.
Results of massage vs. active comparator(s) meta-analysis for musculoskeletal pain populations: healthrelated quality of life at post-treatment (sample size analyzed, N = 424).
Table 4.
Evidence synthesis for musculoskeletal pain conditions
| Outcome/Comparison | Number of Participants Completed (N) | Confidence in the Estimate of the Effect* | Effect Size† | Reported Studies Safety GRADE (N)‡ | Strength of the Recommendation§ |
|---|---|---|---|---|---|
| PAIN ¶ | |||||
| vs. Sham | 655 (9) | B | −0.44 (95% CI, −0.84,−0.05), five studies | +2 (3) | Weak, in favor |
| vs. No Treatment | 245 (4) | A | −1.14 (95% CI, −1.94,−0.35), four studies | +2 (2) | Strong, in favor |
| vs. Active Comparator(s) | 3557 (34) | B | −0.26 (95% CI, −0.53, 0.003), 24 studies | +1 (14) | Weak, in favor |
| ACTIVITY ‖ | |||||
| vs. Sham | 584 (7) | B | 0.36 (95% CI, −0.53, 1.25), three studies | +2 (2) | No recommendation |
| vs. Active Comparator(s) | 3063 (25) | B | −0.23 (95% CI, −0.50, 0.05), seven studies | +1 (12) | No recommendation |
| STRESS, MOOD, HEALTH-RELATED QUALITY OF LIFE | |||||
| vs. Active Comparator(s) | 2527 (21) | B | Anxiety¶: −0.57 (95% CI, −1.06, −0.09), six studies | +1 (11) | Weak, in favor |
| B | Health-related quality of life‖: 0.14 (95% CI, −0.09, 0.36), four studies | Weak, in favor | |||
Definitions for scoring are based on Samueli Institute’s Overall Synthesis Evaluation Criteria (adapted from other standard synthesis methods).
*(A) Further research is very unlikely to change our confidence in the estimate of effect; (B) Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate; (C) Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate; (D) Any estimate of effect is very uncertain.
†Calculated as the standardized mean difference using Cohen’s d effect size estimation where 0.2 is considered a small, 0.5 a medium, and 0.8 a large overall effect.
‡Safety ranges from (+2) appears safe with infrequent adverse events and interactions to (− 2) appears to have serious safety concerns that include frequent and serious adverse events and/or interactions.
§Ranges from Strong Recommendation in Favor indicating that the EMT Working Group is very certain that benefits do outweigh risks and burdens to Strong Recommendation Against indicating that the EMT Working Group is very certain that benefits do not outweigh the risks and burdens.
¶Negative effect indicates improvement in massage intervention compared to control intervention.
‖Positive effect size indicates improvement in massage intervention compared to control intervention.
Musculoskeletal Pain Intensity/Severity
Massage vs. Sham
Nine studies involving a total of 655 individuals with musculoskeletal pain compared the efficacy of a massage intervention to a sham treatment for pain intensity/severity. Five of these studies (290 participants), most using the visual analog scale (VAS), were included in the meta-analysis and resulted in an overall standardized mean difference (SMD) of −0.44 (95% CI, −0.84 to −0.05; I2 = 58.08%). Translated into the VAS, the reduction in pain intensity is −11.10 (95% CI, −20.88 to 1.33) [52]. See Figure 3A. Note that this is a more conservative estimate of the overall SMD as a sixth study had an outlying SMD and was subsequently excluded from the analysis [71].
While all the massage and control techniques used in these studies met the definition for massage therapy and “sham,” respectively, there was still significant heterogeneity across studies with varying doses, techniques, practitioner experience and settings that may influence outcomes. Safety was only reported in three of the nine studies; based on these studies, massage appeared to be safe with infrequent adverse events or interactions, however, due to the lack of reporting, safety, overall, is not well understood. In addition, there is considerable debate and variations of what researchers consider as a “sham” treatment for comparison of massage therapy. Further research, moreover, is likely to have an important impact on the confidence in the estimate of the effect. Given this, and the high quality of the studies, a weak recommendation in favor of massage compared to sham was provided by the EMT Working Group (see Table 4).
Massage vs. No Treatment
Four acceptable quality studies involving a total of 245 participants compared a massage intervention to no treatment (typically a wait-list control). The overall SMD across these studies (219 participants) was −1.14 (95% CI, −1.94 to −0.35; I2 = 84.30%). See Figure 3B. All but one of these studies showed very large effects in favor of massage for treating pain intensity post-treatment. It is interesting to note, however, that this particular study did show a large effect at 6 months follow-up, with a SMD of -1.71 at 6 months compared to -0.23 at post treatment) [78]. Translated into the VAS, the reduction in pain intensity is -28.58 (95% CI, -48.48 to -8.70) across the four studies at post-treatment. Two of the four studies reported either no adverse events occurred or slight discomfort. Even though the studies displayed some inconsistency and wide heterogeneity (I2 = 84.30%), further research is very unlikely to change the confidence in the estimate of this effect, and a strong recommendation was made by the EMT Working Group in favor of massage therapy compared to no treatment for reducing pain intensity/severity for those with musculoskeletal pain (see Table 4).
Massage vs. Active Comparator(s)
Thirty-four studies (involving a total of 3557 participants) compared the efficacy of massage therapy to an active comparator for pain intensity/severity. Twenty-four of these studies (1349 participants) were pooled for meta-analysis resulting in a SMD of −0.26 (95% CI, −0.53 to 0.003; I2 = 79.87%). Translated into the VAS, the reduction in pain intensity is −6.60 (95% CI, −13.30 to 0.08). There was large heterogeneity among the types of active comparators included in this analysis, as demonstrated in Figure 3C. All but two of the 34 studies were either high or acceptable quality with the majority of studies demonstrating a reduction in pain intensity/severity either between or within groups. Based on the 14 of the 34 studies reporting on safety, massage therapy appears relatively safe. Further research is likely to have an important impact on the confidence in the estimate of the effect. As such, the EMT Working Group provided a weak recommendation for massage therapy compared to other active comparators (see Table 4).
Three of these studies had sufficient data for pooling an effect at a 6-month follow-up. See Figure 3D. All studies favored the active comparator at a 6-month follow-up (SMD = 0.49; 95% CI, 0.03 to 0.94; I2 = 31.20%) though it is important to realize that the variability in dosing and duration of both massage and active comparators may have had an effect on the therapeutic benefit. Further investment into understanding appropriate dosing is needed to better understand long-term effects. At this point, it is challenging to identify an “appropriate” intervention with which to compare massage therapy.
Activity
Massage vs. Sham
There were seven studies, involving 584 individuals with musculoskeletal pain, examining the efficacy of massage therapy on activity outcomes compared to sham. Three of these studies (211 participants) were pooled for meta-analysis resulting in an overall SMD of 0.36 (95% CI, −0.53 to 1.25; I2 = 89.05%). See Figure 3E. Based on the two studies that reported safety, massage therapy appears safe with infrequent adverse events. Although all seven studies were of either high or acceptable quality, results were mixed overall, suggesting further research is likely to change the confidence in the estimate of the effect. For this reason, no recommendation regarding massage vs. sham for the treatment of activity outcomes is provided at this time (see Table 4).
Note that, while there was an increase in range of motion with massage therapy as compared to sham, it is important to acknowledge the heterogeneity among the studies pooled. Studies tended to use different methods for measuring activity, highlighting the need for standardization and consensus building for what constitutes “activity” as an objective functional outcome and how it is measured across pain populations for different types of interventions.
Massage vs. Active Comparator(s)
Twenty-five studies (3063 total participants) compared the efficacy of massage therapy on activity to an active comparator. Seven of these studies (450 participants) were pooled for meta-analysis resulting in an overall SMD of −0.23 (95% CI, −0.50 to 0.05; I2 = 50.73%), favoring the active comparator (see Figure 3F). Based on the twelve studies that reported on safety, massage appears to be relatively safe. While most studies were either high or acceptable quality, results were mixed, indicating that further research is likely to have an important impact on the confidence in the estimate of the effect. Note that there are various active comparators used throughout this analysis. It is challenging to interpret this data in a meaningful way without understanding the appropriate comparators and incorporating STRICT-M guidelines to aid with transparent reporting of both massage and controls. For example, one study [58] reports that acupuncture may be more effective than massage therapy for improving activity outcomes, but massage may be more beneficial than relaxation [81]. While these patients all have musculoskeletal pain, the exact area of pain differs (e.g., low back pain, knee pain, neck pain) and, as such, the various location of massage and amount of pressure may affect the patient’s range of motion at follow-up. The variability associated with this outcome makes it challenging to assess these pooled studies. No recommendation is made at this time for massage when compared to an active comparator (see Table 4).
Stress, Mood, and Health-Related Quality of Life
There were not enough studies reporting on stress, mood or HrQoL outcomes that compared massage therapy to either a sham or no treatment control to pool for a meta-analysis. These are important patient-reported outcomes that are necessary, in addition to pain outcomes, to understand a patient’s overall health. Efficient, standardized ways of measuring essential patient-reported outcomes need to be developed.
Massage vs. Active Comparator(s)
There were 21 studies (involving 2527 total participants) comparing massage therapy to an active comparator that measure at least one outcome of stress, mood (mainly anxiety), and/or HrQoL. All but one was rated as either high or acceptable quality. Based on the one study that reported safety, massage appears to be relatively safe.
Anxiety
Six of these studies (210 participants) had sufficient data on anxiety, primarily via the State Anxiety Inventory, to pool for meta-analysis, resulting in an overall SMD of −0.57 (95% CI, −1.06 to −0.09; I2 = 63.17%) favoring massage therapy (see Figure 3G). The majority of these comparators consisted of either relaxation, physical therapy, or an exercise. It appears that massage therapy is more efficacious than any of these comparators for reducing anxiety among patients suffering from musculoskeletal pain. The Egger’s test for publication bias was significant, indicating that there is a cause for concern when interpreting this data. Further research adding to and investigating the appropriate comparators is needed and essential for comparative effectiveness research. A weak recommendation in favor of massage therapy is provided given the current literature base for reducing anxiety in this patient population.
Health-Related Quality of Life
Four studies (424 participants) assessing HrQoL using either the SF-36 or SF-12 general health or physical health status parameters were pooled for meta-analysis, resulting in a SMD of 0.14 (95% CI, −0.09 to 0.36; I2 = 13.44%) in favor of massage therapy; note, a positive effect demonstrates an improvement in HrQoL (see Figure 3H). Again, both the style of massage therapy and types of comparators used varied. Studies were either high or acceptable quality, and the majority showed statistically significant between or within group differences favoring massage therapy. Due to the small number of studies, however, the EMT Working Group concluded that future research is likely to have an important impact on the confidence in the estimate of the effect, and thus provided a weak recommendation in favor of massage therapy for enhancing HrQoL. HrQoL is an important metric when understanding patient-reported outcomes and should be commonly considered in future studies.
Discussion
This systematic review and meta-analysis found that massage therapy may be beneficial, with minimal safety concerns, for treating various pain and function-related outcomes in pain populations. Specifically, results demonstrate the efficacy of massage therapy compared to sham, no treatment and active comparators. Compared to active comparators, massage therapy was also beneficial for treating anxiety and health-related quality of life. This is the first systematic review attempting to investigate different outcomes of patient-reported functional domains (e.g., sleep, stress, mood, activity) and HrQoL across the spectrum of pain conditions from a patient-centric perspective. Additionally, this review examines the complexity of different taxonomies of massage to propose a more coherent definition of massage for the field, and suggests a set of reporting requirements essential for translatability and reproducibility for future work. There are methodological flaws that are apparent across studies addressed in this report, as well as large heterogeneity that cannot be ignored across studies which ultimately lowers the overall quality of the evidence; the latter, however, is expected to improve with education and adherence to clear reporting requirements. It is worth acknowledging that this review also only assessed the evidence reported in peer-reviewed RCTs available to date. Valuable knowledge can be gained through the evaluation of other study designs (e.g., qualitative research). In addition, although a growing body of evidence based research emphasizes the importance of human touch in facilitating healing and recovery from pain, the underlying mechanisms by which massage affects the body are still being investigated [82–84]. Until then, the development of clinical guidelines is cautioned against for massage therapy.
Methodology
Overall, the majority of these studies were high or acceptable quality. While most aspects of internal validity were adequately addressed, many studies failed either to successfully carry out or describe allocation concealment and intention-to-treat processes. The majority of most studies, moreover, failed to describe model validity (i.e., staff, places and facilities used) making it difficult to completely understand how these studies may be replicated and massage therapy implemented.
Because blinding helps reduce the introduction of potential biases, it is an essential component of clinical trials. Of the 67 studies included in this review, a large number did not mention blinding procedures. While this review excluded blinding from its risk of bias assessment due to these challenges, the authors did track whether studies mentioned blinding procedures; regardless of whether blinding is possible, authors should always clearly state who was blinded, or if blinding was not carried out, discuss attempts made toward blinding or why blinding was not possible.
Standards for Reporting Interventions in Clinical Trials of Massage: Proposal to Develop STRICT-M Checklist
Currently, there are no standard criteria or guidelines for reporting massage clinical trials. This is a noticeable gap across all studies assessed in this review. For example, while type of practitioner was mentioned in almost all studies, practitioner qualifications were only mentioned by 14.9%. Although practitioners’ qualifications are likely associated with trial efficacy, specifically an improvement in outcomes [85], this concept is difficult to explore as this information is typically underreported [41,86]. Similarly, setting was only described by 43.3% of the studies, resulting in poor model validity and an inability to fully understand how the review’s findings could be generalized to other settings. While components of the massage interventions, for the most part, were well-described, the control groups lacked such data. Replication and validation of the trial’s results are nearly impossible without this essential reporting information. Researchers and clinicians, moreover, are unable to make firm recommendations to patients and policy based on inconsistent or missing data.
The authors propose that in addition to adhering to the CONSORT guidelines for uniform reporting, the field should consider the development of a set of reporting standards (e.g., the authors’ proposed STRICT-M, see Table 3) for reporting of massage trials and include specific items regarding the various details of the massage intervention. Doing so would help standardize the language used to describe massage, thus enabling readers to better understand how massage is defined and how the intervention, if deemed efficacious, could be replicated in real-life. As noted in the evidence synthesis, there is a large amount of heterogeneity among the included studies that needs to be accounted for as it greatly restricted the EMT Working Group from making solid conclusions about the value of massage therapy. Adhering to guidelines, similar to the proposed STRICT-M Checklist outlined in this report, would help move this field forward.
Proposed Definition of Massage Therapy
There is wide variety in the types, styles, dosaging, naming conventions, and practitioner qualifications of interventions labeled as “massage therapy.” For example, while drug trials undergo systematic phase trials to determine consistent and adequate dosing, massage trials do not carry out such processes and often do not provide rationale for dose-related variables [41] resulting in inconsistent dosages. Further, not only do practitioners vary by type, with massage falling within the scope of practice for many different healthcare providers (e.g., massage therapists, nurses, physicians, chiropractors, physical therapists) but their qualifications vary, as each state has their own set of requirements with some requiring a set amount of education hours and others having no such standards. Given this wide range of variability, it is no surprise that there are numerous different types of treatments that fall under the umbrella term “massage.”
In order to encompass the wide spectrum of techniques called “massage,” the EMT Working Group spent considerable time during protocol development defining and conceptualizing what constitutes “massage therapy.” It is important that steps toward creating a common language are taken so that future researchers are better able to select techniques appropriate to their research and draw more meaningful conclusions. In 2006, Sherman et al. created a new classification system to describe the work massage therapists provide when giving a massage to patients with musculoskeletal pain [29]. It is the hope that using consistent terminology will facilitate standardized reporting of massage interventions, so that more sound research can be conducted and more definitive conclusions can be drawn.
In addition, there is debate as to what constitutes an appropriate control for massage therapy. For example, no treatment control groups do not control for nonspecific effects of attention and touch; resulting in massage interventions tending to be more successful than such controls. Wait list controls do not control for placebo effects and treatment as usual controls may assign individuals to care that they may have already previously tried and found unsuccessful. Consequently, massage should be assessed against controls that are equal and, for all intents and purposes, identical in order to ensure effects are truly attributable to massage. Sham controls (e.g., sham massage, light touch) are promising; however, there is debate about whether touch control is a true placebo as touch can elicit nonspecific psychological effects. In this review, the authors lumped any sham treatment (e.g., light touch, simple touch, sham massage, sham acupuncture, sham ultrasound), recognizing that there exists heterogeneity across these studies. Future research should focus on identifying appropriate sham controls to truly ascertain the effect of massage therapy beyond that of placebo, and how much the effect could be due to the therapeutic alliance encountered [87]. These are questions that still remain.
Comparative Effectiveness
Comparative effectiveness research is an important part of future work for massage therapy. However, investing in comparative effectiveness research in this area is cautioned until standard guidelines (e.g., STRICT-M Checklist) are developed to improve reporting and allow for replication and standardized outcomes addressing the full patient perspective are used. Cost, patient preferences and values, safety, and benefits all need to be taken into account before developing a comparative effectiveness protocol. In fact, before delving into such research, the authors recommend first forming a panel to design a large, multi-site protocol that addresses the gaps (e.g., heterogeneity of intervention and control/comparator groups, lack of consistent reporting) described throughout this report in order to clearly understand the efficacy of massage therapy. Once efficacy has been determined, a committee can begin identifying appropriate and cost-worthy comparators. This review included many small scale trials comparing massage to various other active comparators, however, clear descriptions and justification for the use of such comparators were noticeably absent in many trials. Research needs to focus on identifying which comparators are most cost-effective and feasible in order to begin utilizing the same comparators in studies. Until then, comparators will remain heterogeneous which presents challenge with interpretation and inevitably stalls the field from moving forward.
Patient-Reported Function Outcomes
In order to document societal cost savings and approach healthcare from the patient perspective, it is critical for massage, and the CIM community at large, to utilize standardized, state-of the science, patient-reported outcomes as they conduct research in order to enhance the rigor of the field. Not only would a wide variety of stakeholders in the US healthcare system take note, but replication and meta-analysis pooling of standard outcomes for future research would become possible. Often, the best way patients can judge the effectiveness of treatments is by self-reported symptoms, functioning and well-being. The National Institutes of Health’s (NIH’s) Patient Reported Outcomes Measurement Information System (PROMIS) [38] has developed reliable and valid patient-reported items to evaluate medical interventions for persons with a wide range of chronic diseases and demographic characteristics. The Pain Assessment Screening Tool and Outcomes Registry (PASTOR) [37] is an example of a clinical pain assessment tool that utilizes PROMIS domains in order to standardize approaches to pain management. Such assessment tools are not only patient-centered as they are based on patients’ perspectives and have the ability to be tailored to the specific individual, but are also typically less time consuming than using multiple outcome assessment tools. As the field moves toward patient-centered care and with the growing realization that pain is complex and needs to be approached through a more holistic view (i.e., accounting for functional outcomes as they relate to pain), researchers should consider using assessment tools based on PROMIS domains in order to produce meaningful, translatable results that can be combined across studies.
This current review considered PROMIS and PASTOR domains when evaluating patient- reported outcomes of the included studies. While the majority of the included studies reported using valid and reliable outcomes (see Table 1), a complete examination of these outcomes was outside the scope of the current review and requires further investigation. Because different studies have different critical outcomes, and researchers differ in their preferences for what outcome measures are sensitive to the population at hand, heterogeneity is a large issue with interpreting results. A standardized, validated, uniform tool that combines all functional domains at an individual level is necessary to dissolve the problem of heterogeneity and allow for easier pooling and interpretation of studies.
While the authors relied on a cut-off point of 20-mm for the VAS as a clinically important reduction in pain, this was noted to be interpreted with caution. As detailed throughout, what constitutes clinical importance may be better addressed through the whole-person perspective, beyond that of a reduction in pain to something more globally measured and including psychological, physical, social, spiritual functioning in addition to pain.
Patient Preferences
According to the 2007 National Health Interview Survey (NHIS) [88], 10,000 individuals 18 years of age and over reported using massage therapy, most commonly for musculoskeletal conditions in 2002; this number has since grown with over 18,000 reporting massage use in 2007. Despite the flaws in methodological and reporting quality and the wide heterogeneity among the available studies published to date, patients are actively seeking support through massage therapy. Unfortunately, very little is known about users’ preferences and the decision-making process for engaging in such a therapy.
There has also been very little research in terms of cost and how or if this influences patient preferences. Three studies [63,75,89] captured in this review performed cost analyses. One study [89] reported comprehensive massage therapy had the most benefit but cost more than soft-tissue manipulation alone. Another study [75] demonstrated that costs of outpatient services were lower in the massage group than Traditional Chinese Medical acupuncture and self-care educational materials. Although this difference was not statistically significant, authors report that initial massage costs might be offset by reduction in subsequent care, and that the combination of massage and self-care materials might prove to be particularly cost-effective. Conversely, the final study [63] determined that there was no evidence that massage treatments reduced costs of back pain related healthcare services during a one year post-treatment period.
Research shows that patients with strong relative expectations for a specific treatment tend to have better functional outcomes if they received that treatment [90], but measures recording patient expectation are often missing from clinical trials. Only three studies captured in this review measured participants’ expectation regarding treatment success. Two studies [63,66] reported fairly high expectations for massage. The third article [91] measured participants’ confidence in the interventions’ success but failed to report the relevant results.
Clinical Practice Guidelines
Clinical guidelines are an essential ingredient for informing appropriate healthcare decisions. They have the power to translate scientific research findings into recommendations for clinical practice and potentially enhance healthcare quality and outcomes [92]. Clinical practice guidelines take into account not only the scientific research findings collated through systematic reviews on efficacy, but also the benefit/harm ratios, cost, acceptability and feasibility. This review has outlined next steps to guide future research in filling in the current research gaps in order to allow for translation to occur. Once these gaps are appropriately addressed, the field will be able to move toward developing clinical practice guidelines that can be trusted. Patients deserve to have this work completed; pain management is a rising concern and clinicians need to fill their “tool bags” with complementary options that will benefit their patients’ overall wellbeing. The field of massage therapy can be empowered to charge forward with the recommendations outlined in this review in order to begin to move toward effective translation.
Next Steps for Researchers and Decision Makers in Chronological Order
Consider this review’s proposed definition of massage therapy to help resolve the confusion regarding what constitutes “massage therapy.”
Educate researchers about and ensure adherence to the CONSORT Checklist to enhance reporting and quality of future work.
Study the proposed STRICT-M Checklist, invest resources to formally develop STRICT-M for the field and adapt these criteria for future protocol development.
Study PROMIS and PASTOR to learn their functionality; consider the whole-patient perspective in all clinical research and use these tools in future work.
Invest resources in a large, multi-site study examining the efficacy of massage therapy compared to an appropriate sham treatment once items 1–4 are accomplished and ensure those components are embedded in the robust protocol; track patient preferences and values, expectations of patients and clinicians, and safety.
Explore appropriate comparators for comparative effectiveness research once efficacy is clearly demonstrated in item 5; assemble a diverse group of stakeholders, including patients, to provide input during protocol development; track cost, patient preferences and values, expectation, and safety; conduct appropriate comparative effectiveness research.
Develop clinical practice guidelines for the field of massage therapy.
Conclusion
There is evidence to suggest that massage therapy may be beneficial for improving various patient-reported functional outcomes for populations experiencing pain. There is clear evidence supporting the efficacy of massage therapy compared to no treatment for pain intensity suggesting that massage therapy, rather than no treatment at all, should be offered to a patient for pain management. Compared to sham or active comparator(s), massage therapy is beneficial across various function outcomes including anxiety and HrQoL. However, further work is needed to better promote massage therapy for pain populations; specifically, future research should consider this review’s definition of massage therapy moving forward; ensure research literacy and abide by CONSORT guidelines for reporting and ensuring methodological quality; adapt the proposed STRICT-M Checklist for essential reporting around the intervention to allow for reproducibility and translation; and use standardized assessment tools that utilize PROMIS outcomes that address the whole patient perspective in clinical trial work. Incorporating these elements into a robust, large, multi-site protocol with adequate resources and stakeholder involvement will allow for replicability, hopefully reduced heterogeneity, and ultimately, translation to occur.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Viviane Enslein for her administrative contribution to the project, Cindy Lentino for her editorial contribution, and Christopher Baur for assisting with data extraction.
The Evidence for Massage Therapy (EMT) Working Group included the following individuals at the time of writing (see doi: 10.1093/pm/pnw092 for working group affiliations): Chester Buckenmaier III, MD, COL (ret), USA; Pamela Buckenmaier, RN, LMT; Jerrilyn Cambron, DC, PhD; Christopher Deery, LMT; Jan Schwartz, MA, BCTMB; Ruth Werner, BCTMB; Pete Whitridge, BA, LMT.
Contributor Information
Evidence for Massage Therapy (EMT) Working Group:
Chester Buckenmaier, III, Pamela Buckenmaier, Jerrilyn Cambron, Christopher Deery, Jan Schwartz, Ruth Werner, and Pete Whitridge
References
- 1. National Center for Health Statistics. Health, United States, 2006, with chartbook on trends in the health of Americans. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2006.
- 2. Jamison R, Edwards R. Integrating pain management in clinical practice. J Clin Psychol Med Settings 2012;19(1):49–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. May A. Chronic pain may change the structure of the brain. Pain 2008;137(1):7–15. [DOI] [PubMed] [Google Scholar]
- 4. Lee C, Crawford C, Teo L, Spevak C. An analysis of the various chronic pain conditions captured in a systematic review of active self-care complementary and integrative medicine therapies for the management of chronic pain symptoms. Pain Med 2014;15(suppl 1):S96–103. [DOI] [PubMed] [Google Scholar]
- 5. Gureje O, Von Korff M, Simon G, Gater R. Persistent pain and well-being: A world health organization study in primary care. JAMA 1998;280(2):147–51. [DOI] [PubMed] [Google Scholar]
- 6. Oliveros O, Trachtenberg F, Haines D, et al. Pain over time and its effects on life in thalassemia. Am J Hematol 2013;88(11):939–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Simons L, Elman I, Borsook D. Psychological processing in chronic pain: A neural systems approach. Neurosci Biobehav Rev 2014;39:61–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smith B, Zautra A. The effects of anxiety and depression on weekly pain in women with arthritis. Pain 2008;138(2):354–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Phyomaung P, Dubowitz J, Cicuttini F, et al. Are depression, anxiety and poor mental health risk factors for knee pain? A systematic review. BMC Musculoskelet Disord 2014;15:10.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. De Heer E, Gerritis M, Beekman A, et al. The association of depression and anxiety with pain: A study from nesda. PLoS One 2014;9(10):e106907..doi:10.1371/journal.pone.0106907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tavoli A, Montazeri A, Roshan R, Tavoli Z, Melyani M. Depression and quality of life in cancer patients with and without pain: The role of pain beliefs. BMC Cancer 2008;8:177..doi:10.1186/1471-2407-8-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bair M, Robinson R, Katon W, Kroenke K. Depression and pain comorbidity: A literature review. Arch Intern Med 2003;163(20):2433–45. [DOI] [PubMed] [Google Scholar]
- 13. Quartana P, Campbell C, Edwards R. Pain catastrophizing: A critical review. Expert Rev Neurother 2009;9(5):745–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Finan P, Goodin B, Smith M. The association of sleep and pain: An update and a path forward. J Pain 2013;14(12):1539–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tang N, Goodchild C, Sanborn A, Howard J, Salkovskis P. Deciphering the temporal link between pain and sleep in a heterogeneous chronic pain patient sample: A multilevel daily process study. Sleep 2012;35(5):675–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lynch-Jordan A, Kashikar-Zuck S, Szabova A, Goldschneider K. The interplay of parent and adolescent catastrophizing and its impact on adolescents’ pain, functioning, and pain behavior. Clin J Pain 2013;29(8):681–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Furlan A, Yazdi F, Tsertsvadze A, et al. A systematic review and meta-analysis of efficacy, cost-effectiveness, and safety of selected complementary and alternative medicine for neck and low-back pain. Evid Based Complement Alternat Med 2012;953139 doi:10.1155/2012/953139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Broom A, Kirby E, Sibbritt D, Adams J, Refshauge K. Use of complementary and alternative medicine by mid-age women with back pain: A national cross-sectional survey. BMC Complement Alternat Med 2012;12(98). doi:10.1186/1472-6882-12-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Moyer C, Rounds J, Hannum J. A meta-analysis of massage therapy research. Psychol Bull 2004;130(1):3–18. [DOI] [PubMed] [Google Scholar]
- 20. Sagar S, Dryden T, Wong R. Massage therapy for cancer patients: A reciprocal relationship between body and mind. Curr Oncol 2007;14(2):45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Adams R, White B, Beckett C. The effects of massage therapy on pain management in the acute care setting. Int J Ther Massage Bodywork 2010;3(1):4–11. [PMC free article] [PubMed] [Google Scholar]
- 22. Yin P, Gao N, Wu J, Litscher G, Xu S. Adverse events of massage therapy in pain-related conditions: A systematic review. Evid Based Complement Alternat Med 2014;11:480956 doi:10.1155/2014/480956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kumar S, Beaton K, Hughes T. The effectiveness of massage therapy for the treatment of nonspecific low back pain: A systematic review of systematic reviews. Int J Gen Med 2013;6:733–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bronfort G, Haas M, Evans R, Leininger B, Triano J. Effectiveness of manual therapies: The UK evidence report. Chiropr Osteopat 2010;18:3 doi:10.1186/1746-1340-18-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Furlan AD, Giraldo M, Baskwill A, Irvin E, Imamura M. Massage for low-back pain. Cochrane Database Syst Rev 2015;9:CD001929..doi: 10.1002/14651858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Netchanok S, Wendy M, Marie C, Siobhan O. The effectiveness of Swedish massage and traditional Thai massage in treating chronic low back pain: A review of the literature. Complement Ther Clin Pract 2012;18(4):227–34. [DOI] [PubMed] [Google Scholar]
- 27. van den Dolder PA, Ferreira PH, Refshauge KM. Effectiveness of soft tissue massage and exercise for the treatment of non-specific shoulder pain: A systematic review with meta-analysis. Br J Sports Med 2014;48(16):1216–26. [DOI] [PubMed] [Google Scholar]
- 28. Smith C, KM L, Collins C, Jones L. Massage, reflexology and other manual methods for pain management in labour. Cochrane Database Syst Rev 2012;2:CD009290 doi:10.1002/14651858. [DOI] [PubMed] [Google Scholar]
- 29. Sherman K, Dixon M, Thompson D, Cherkin D. Development of a taxonomy to describe massage treatment for musculoskeletal pain. BMC Complement Alternat Med 2006;6(24):6–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Office of the Army Surgeon General: Pain Management Task Force. Pain Management Task Force Final Report: Providing a Standardized DoD and VHA Vision And Approach To Pain Management To Optimize the Care for Warriors and Their Families. Washington, DC: Office of the Army Surgeon General; 2010.
- 31. Crawford C, Boyd C, Jain S, Khorsan R, Jonas W. Rapid evidence assessment of the literature: Streamlining the systematic review process and creating utility for evidence-based health care. BMC Res Notes 2015;8:631..doi:10.1186/s13104-015-1604-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Costello B, Lentino C, Boyd C, et al. The effectiveness of melatonin for promoting healthy sleep: A rapid evidence assessment of the literature. Nutr J 2014;13:106..doi:10.1186/1475-2891-13-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Buckenmaier C, III, Crawford C, Lee C, Schoomaker E. Are active self-care complementary and integrative therapies effective for management of chronic pain? A rapid evidence assessment of the literature and recommendations for the field. Pain Med 2014;15(suppl 1):S1–S113.24734855 [Google Scholar]
- 34. Lee C, Crawford C, Wallerstedt D, et al. The effectiveness of acupuncture research across components of the trauma spectrum response (tsr): A systematic review of reviews. Syst Rev 2012;1(46):doi:10.1186/2046-4053-1-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. York A, Crawford C, Walter A, et al. Acupuncture research in military and veteran populations: A rapid evidence assessment of the literature. Med Acupunct 2011;23(4):229–36. [Google Scholar]
- 36. Zeno S, Crawford C, Lee C, Purvis D, Deuster P. The effectiveness of warm-up exercises for physical fitness testing (in the military). Med Sci Sports Exerc 2013;45(7):1369–76. [DOI] [PubMed] [Google Scholar]
- 37. Defense & Veterans Center for Integrative Pain Management (DVCIPM). Pain assessment screening tool and outcomes registry (pastor) Secondary Pain assessment screening tool and outcomes registry (pastor). 2015. Available at: http://www.dvcipm.org/clinical-resources/pain-assessment-screening-tool-and-outcomes-registry-pastor(accessed November 1, 2015).
- 38. National Institutes of Health. Promis: Patient reported outcomes measurement information system. Secondary Promis: Patient reported outcomes measurement information system. 2015. Available at: http://commonfund.nih.gov/promis/overview(accessed November 1, 2015).
- 39. Management, DaVCfIP. Defense and veterans pain rating scale (dvprs). Secondary Defense and veterans pain rating scale (dvprs). Available at: http://www.dvcipm.org/clinical-resources/pain-rating-scale(accessed November 1, 2015).
- 40. Furlan A, Imamura M, Dryden T, Irvin E. Massage for low-back pain. Cochrane Database Syst Rev 2008;4:1–104. [DOI] [PubMed] [Google Scholar]
- 41. Haraldsson B, Gross A, Myers C, et al. Group, CO . Massage for mechanical neck disorders. Cochrane Database Syst Rev 2006;3:1–75. [DOI] [PubMed] [Google Scholar]
- 42. Massage Therapy Body of Knowledge Task Force. Body of knowledge. Secondary Body of knowledge. 2015. Available at: www.mtbok.org(accessed November 1, 2015).
- 43. Coalition of National Massage Therapy Organizations. The entry level analysis project. Secondary The entry level analysis project. 2015. Available at: www.elapmassage.org (accessed November 1, 2015).
- 44. Scottish Intercollegiate Guidelines Network (SIGN). A guideline developer’s handbook. Secondary A guideline developer’s handbook. 2001. Available at: http://www.sign.ac.uk/methodology/checklists.html(accessed November 1, 2015).
- 45. Khorsan R, Crawford C. How to assess the external validity and model validity of therapeutic trials: A conceptual approach for systematic review methodology. Evidence Based Complement Alternat Med 2014:694804..doi:10.1155/2014/694804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. MacPherson H, Altman D, Hammerschlag R, et al. Revised standards for reporting interventions in clinical trials of acupuncture (stricta): Extending the consort statement. Acupunct Med 2010;28(2):83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. The CONSORT Group. The consolidated standards of reporting trials (consort) statement. Secondary The consolidated standards of reporting trials (consort) statement. 2010. Available at: http://www.consort-statement.org/(accessed November 1, 2015).
- 48. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edition. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 49. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7(3):177–88. [DOI] [PubMed] [Google Scholar]
- 50. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Higgins J, Thompson S, Deeks J, Altman D. Measuring inconsistency in meta-analyses. BMJ 2003;327(7414):557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Farrar JT, Portenoy RK, Berlin JA, Kinman JL, Strom BL. Defining the clinically important difference in pain outcome measures. Pain 2000;88(3):287–94. [DOI] [PubMed] [Google Scholar]
- 53. Boyd C, Crawford C, Paat C, et al. The impact of massage therapy on function in pain populations—a systematic review and meta-analysis of randomized controlled trials: Part II, cancer pain populations. Pain Med. doi:10.1093/pm/pnw100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Boyd C, Crawford C, Paat C, et al. The impact of massage therapy on function in pain populations—a systematic review and meta-analysis of randomized controlled trials: Part III, surgical pain populations. Pain Med. doi:10.1093/pm/pnw101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Cino K. Aromatherapy hand massage for older adults with chronic pain living in long-term care. J Holist Nurs 2014;32(4):304–13. [DOI] [PubMed] [Google Scholar]
- 56. FitzGerald MP, Payne CK, Lukacz ES, et al. Randomized multicenter clinical trial of myofascial physical therapy in women with interstitial cystitis/painful bladder syndrome and pelvic floor tenderness. J Urol 2012;187(6):2113–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hsieh CJ, Adams AH, Tobis J, et al. Effectiveness of four conservative treatments for subacute low back pain: A randomized clinical trial. Spine 2002;27(11):1142–8. [DOI] [PubMed] [Google Scholar]
- 58. Irnich D, Behrens N, Molzen H, et al. Randomised trial of acupuncture compared with conventional massage and “sham” laser acupuncture for treatment of chronic neck pain. BMJ 2001;322(7302):1574–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Little P, Lewith G, Webley F, et al. Randomised controlled trial of alexander technique lessons, exercise, and massage (ateam) for chronic and recurrent back pain. BMJ 2008;337(7667):438–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Perlman AI, Ali A, Njike VY, et al. Massage therapy for osteoarthritis of the knee: A randomized dose-finding trial. PLoS One 2012;7(2):e30248..doi: 10.1371/journal.pone.0030248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Paanalahti K, Holm L, Nordin M, et al. Adverse events after manual therapy among patients seeking care for neck and/or back pain: A randomized controlled trial. BMC Musculoskelet Disord 2014;15(77):1471–2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Berggreen S, Wiik E, Lund H. Treatment of myofascial trigger points in female patients with chronic tension-type headache–A randomized controlled trial. Adv Physiother 2012;14(1):10–7. [Google Scholar]
- 63. Cherkin DC, Sherman KJ, Kahn J, et al. A comparison of the effects of 2 types of massage and usual care on chronic low back pain: A randomized, controlled trial. Ann Int Med 2011;155(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Guarda-Nardini L, Stecco A, Stecco C, Masiero S, Manfredini D. Myofascial pain of the jaw muscles: Comparison of short-term effectiveness of botulinum toxin injections and fascial manipulation technique. Cranio 30(2):95–102. [DOI] [PubMed] [Google Scholar]
- 65. Kumnerddee W. Effectiveness comparison between thai traditional massage and chinese acupuncture for myofascial back pain in thai military personnel: A preliminary report. J Med Assoc Thai 2009;92(suppl 1):S117–23. [PubMed] [Google Scholar]
- 66. Lauche R, Materdey S, Cramer H, et al. Effectiveness of home-based cupping massage compared to progressive muscle relaxation in patients with chronic neck pain–A randomized controlled trial. PLoS One 2013;8(6):e65378..doi: 10.1371/journal.pone.0065378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Perlman AI, Sabina A, Williams AL, Njike VY, Katz DL. Massage therapy for osteoarthritis of the knee: A randomized controlled trial. Arch Int Med 2006;166(22):2533–8. [DOI] [PubMed] [Google Scholar]
- 68. Renan-Ordine R, Alburquerque-Sendin F, de Souza DP, Cleland JA, Fernandez-de-Las-Penas C. Effectiveness of myofascial trigger point manual therapy combined with a self-stretching protocol for the management of plantar heel pain: A randomized controlled trial. J Orthop Sports Phys Ther 2011;41(2):43–50. [DOI] [PubMed] [Google Scholar]
- 69. Sherman KJ, Cherkin DC, Hawkes RJ, Miglioretti DL, Deyo RA. Randomized trial of therapeutic massage for chronic neck pain. Clin J Pain 2009;25(3):233–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Aguilera FJM, Martín DP, Masanet RA, et al. Immediate effect of ultrasound and ischemic compression techniques for the treatment of trapezius latent myofascial trigger points in healthy subjects: A randomized controlled study. J Manipulative Physiol Ther 2009;32(7):515–20. [DOI] [PubMed] [Google Scholar]
- 71. Ajimsha MS, Chithra S, Thulasyammal RP. Effectiveness of myofascial release in the management of lateral epicondylitis in computer professionals. Arch Phys Med Rehabil 2012;93(4):604–9. [DOI] [PubMed] [Google Scholar]
- 72. Buttagat V, Eungpinichpong W, Chatchawan U, Arayawichanon P. Therapeutic effects of traditional thai massage on pain, muscle tension and anxiety in patients with scapulocostal syndrome: A randomized single-blinded pilot study. J Bodyw Mov Ther 2012;16(1):57–63. [DOI] [PubMed] [Google Scholar]
- 73. Castro-Sanchez AM, Mataran-Penarrocha GA, Arroyo-Morales M, et al. Effects of myofascial release techniques on pain, physical function, and postural stability in patients with fibromyalgia: A randomized controlled trial. Clin Rehabil 2011;25(9):800–13. [DOI] [PubMed] [Google Scholar]
- 74. Chase T, Jha A, Brooks CA, Allshouse A. A pilot feasibility study of massage to reduce pain in people with spinal cord injury during acute rehabilitation. Spinal Cord 2013;51(11):847–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Cherkin DC, Eisenberg D, Sherman KJ, et al. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self-care education for chronic low back pain. Arch Intern Med 2001;161(8):1081–8. [DOI] [PubMed] [Google Scholar]
- 76. Hains G, Descarreaux M, Hains F. Chronic shoulder pain of myofascial origin: A randomized clinical trial using ischemic compression therapy. J Manipulative Physiol Ther 2010;33(5):362–9. [DOI] [PubMed] [Google Scholar]
- 77. Hasson D, Arnetz B, Jelveus L, Edelstam B. A randomized clinical trial of the treatment effects of massage compared to relaxation tape recordings on diffuse long-term pain. Psychother Psychosom 2004;73(1):17–24. [DOI] [PubMed] [Google Scholar]
- 78. Kalamir A, Pollard H, Vitiello A, Bonello R. Intra-oral myofascial therapy for chronic myogenous temporomandibular disorders: A randomized, controlled pilot study. J Manual Manipulative Ther 2010;18(3):139–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ramos-Gonzalez E, Moreno-Lorenzo C, Mataran-Penarrocha GA, et al. Comparative study on the effectiveness of myofascial release manual therapy and physical therapy for venous insufficiency in postmenopausal women. Complement Ther Med 2012;20(5):291–8. [DOI] [PubMed] [Google Scholar]
- 80. Yip YB, Tam AC. An experimental study on the effectiveness of massage with aromatic ginger and orange essential oil for moderate-to-severe knee pain among the elderly in Hong Kong. Complement Ther Med 2008;16(3):131–8. [DOI] [PubMed] [Google Scholar]
- 81. Hernandez-Reif M, Field T, Krasnegor J, Theakston H. Lower back pain is reduced and range of motion increased after massage therapy. Int J Neurosci 2001;106(3-4):131–45. [DOI] [PubMed] [Google Scholar]
- 82. Field T. Massage therapy research review. Complement Ther Clin Pract 2014;20(4):224–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Crane JD, Ogborn DI, Cupido C, et al. Massage therapy attenuates inflammatory signaling after exercise-induced muscle damage. Sci Transl Med 2012;4(119):119ra13..doi:10.1126/scitranslmed.3002882. [DOI] [PubMed] [Google Scholar]
- 84. Field T. Touch for socioemotional and physical well-being: A review. Develop Rev 2010;30(4):367–83. [Google Scholar]
- 85. Furlan A, Brosseau L, Imamura M, Irvin E. Massage for low back pain. Cochrane Database Syst Rev 2002;2:CD001929. [DOI] [PubMed] [Google Scholar]
- 86. Ezzo J. What can be learned from cochrane systematic reviews of massage that can guide future research. J Alternat Complement Med 2007;13(2):291–5. [DOI] [PubMed] [Google Scholar]
- 87. Jonas WB. Reframing placebo in research and practice. Philos Trans R Soc Lond B Biol Sci 2011;366(1572):1896–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Barnes P,, Bloom B, Nahin R. Complementary and Alternative Medicine Use Among Adults and Children: United states, 2007. Natl Health Stat Rep 2008;12:1–23. [PubMed] [Google Scholar]
- 89. Preyde M. Effectiveness of massage therapy for subacute low-back pain: A randomized controlled trial. CMAJ 2000;162(13):1815–20. [PMC free article] [PubMed] [Google Scholar]
- 90. Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: Patient expectations and treatment effects. Spine 2001;26(13):1418–24. [DOI] [PubMed] [Google Scholar]
- 91. Haas M, Spegman A, Peterson D, Aickin M, Vavrek D. Dose response and efficacy of spinal manipulation for chronic cervicogenic headache: A pilot randomized controlled trial. Spine J 2010;10(2):117–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Institute of Medicine. Clinical Practice Guidelines We Can Trust. Washington, DC: The National Academies Press; 2011. [Google Scholar]
- 93. Blikstad A, Gemmell H. Immediate effect of activator trigger point therapy and myofascial band therapy on non-specific neck pain in patients with upper trapezius trigger points compared to sham ultrasound: A randomised controlled trial. Clin Chiropr 2008;11(1):23–9. [Google Scholar]
- 94. Buttagat V, Eungpinichpong W, Chatchawan U, Kharmwan S. The immediate effects of traditional thai massage on heart rate variability and stress-related parameters in patients with back pain associated with myofascial trigger points. J Bodyw Mov Ther 2011;15(1):15–23. [DOI] [PubMed] [Google Scholar]
- 95. Buttagat V, Eungpinichpong W, Kaber D, Chatchawan U, Arayawichanon P. Acute effects of traditional Thai massage on electroencephalogram in patients with scapulocostal syndrome. Complement Ther Med 2012;20(4):167–74. [DOI] [PubMed] [Google Scholar]
- 96. Hains G, Hains F. Patellofemoral pain syndrome managed by ischemic compression to the trigger points located in the peri-patellar and retro-patellar areas: A randomized clinical trial. Clin Chiropr 2010;13(3):201–9. [Google Scholar]
- 97. Madson TJ, Cieslak KR, Gay RE. Joint mobilization vs massage for chronic mechanical neck pain: A pilot study to assess recruitment strategies and estimate outcome measure variability. J Manipulative Physiol Ther 2010;33(9):644–51. [DOI] [PubMed] [Google Scholar]
- 98. Walach H, Guthlin C, Konig M. Efficacy of massage therapy in chronic pain: A pragmatic randomized trial. J Alternat Complement Med 2003;9(6):837–46. [DOI] [PubMed] [Google Scholar]
- 99. Donoyama N, Munakata T, Shibasaki M. Effects of anma therapy (traditional Japanese massage) on body and mind. J Bodyw Mov Ther 2010;14(1):55–64. [DOI] [PubMed] [Google Scholar]
- 100. Field T, Diego M, Delgado J, Garcia D, Funk CG. Hand pain is reduced by massage therapy. Complement Ther Clin Pract 2011;17(4):226–9. [DOI] [PubMed] [Google Scholar]
- 101. Field T, Diego M, Delgado J, Garcia D, Funk CG. Rheumatoid arthritis in upper limbs benefits from moderate pressure massage therapy. Complement Ther Clin Pract 2013;19(2):101–3. [DOI] [PubMed] [Google Scholar]
- 102. Hou CR, Tsai LC, Cheng KF, Chung KC, Hong CZ. Immediate effects of various physical therapeutic modalities on cervical myofascial pain and trigger-point sensitivity. Arch Phys Med Rehabil 2002;83(10):1406–14. [DOI] [PubMed] [Google Scholar]
- 103. Kankaanpaa M, Taimela S, Airaksinen O, Hanninen O. The efficacy of active rehabilitation in chronic low back pain. Effect on pain intensity, self-experienced disability, and lumbar fatigability. Spine 1999;24(10):1034–42. [DOI] [PubMed] [Google Scholar]
- 104. Kostopoulos D, Nelson AJ, Jr, Ingber RS, Larkin RW. Reduction of spontaneous electrical activity and pain perception of trigger points in the upper trapezius muscle through trigger point compression and passive stretching. J Musculoskelet Pain 2008;16(4):267–79. [Google Scholar]
- 105. Lara-Palomo IC, Aguilar-Ferrandiz ME, Mataran-Penarrocha GA, et al. Short-term effects of interferential current electro-massage in adults with chronic non-specific low back pain: A randomized controlled trial. Clin Rehabil 2013;27(5):439–49. [DOI] [PubMed] [Google Scholar]
- 106. Maigne JY, Chatellier G. Comparison of three manual coccydynia treatments: A pilot study. Spine 2001;26(20):E479–83. [DOI] [PubMed] [Google Scholar]
- 107. Madenci E, Altindag O, Koca I, Yilmaz M, Gur A. Reliability and efficacy of the new massage technique on the treatment in the patients with carpal tunnel syndrome. Rheumatol Int 2012;32(10):3171–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Mok E, Woo CP. The effects of slow-stroke back massage on anxiety and shoulder pain in elderly stroke patients. Complement Ther Nurs Midwifery 2004;10(4):209–16. [DOI] [PubMed] [Google Scholar]
- 109. Plews-Ogan M, Owens JE, Goodman M, Wolfe P, Schorling J. A pilot study evaluating mindfulness-based stress reduction and massage for the management of chronic pain. J Gen Int Med 2005;20(12):1136–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Pope MH, Phillips RB, Haugh LD, et al. A prospective randomized three-week trial of spinal manipulation, transcutaneous muscle stimulation, massage and corset in the treatment of subacute low back pain. Spine 1994;19(22):2571–7. [DOI] [PubMed] [Google Scholar]
- 111. Roach S, Sorenson E, Headley B, San Juan JG. Prevalence of myofascial trigger points in the hip in patellofemoral pain. Arch Phys Med Rehabil 2013;94(3):522–6. [DOI] [PubMed] [Google Scholar]
- 112. Stratford PW, Levy DR, Gauldie S, Miseferi D, Levy K. The evaluation of phonophoresis and friction massage as treatments for extensor carpi radialis tendinitis. Randomized Controlled Trial Physiother Can 1989;41(2):93–9. [Google Scholar]
- 113. van den Dolder PA, Roberts DL. A trial into the effectiveness of soft tissue massage in the treatment of shoulder pain. Aust J Physiother 2003;49(3):183–8. [DOI] [PubMed] [Google Scholar]
- 114. Yağcı N, Uygur F, Bek N. Comparison of connective tissue massage and spray-and-stretch technique in the treatment of chronic cervical myofascial pain syndrome. Pain Clinic 2004;16(4):469–74. [Google Scholar]
- 115. Yurtkuran M, Kocagil T. Tens, electroacupuncture and ice massage: Comparison of treatment for osteoarthritis of the knee. Am J Acupunct 1999;27(3-4):133–40. [PubMed] [Google Scholar]
- 116. Zaproudina N, Hanninen OO, Airaksinen O. Effectiveness of traditional bone setting in chronic neck pain: Randomized clinical trial. J Manipulative Physiol Ther 2007;30(6):432–7. [DOI] [PubMed] [Google Scholar]
- 117. Zheng Z, Wang J, Gao Q, et al. Therapeutic evaluation of lumbar tender point deep massage for chronic non-specific low back pain. J Tradit Chin Med 2012;32(4):534–7. [DOI] [PubMed] [Google Scholar]
- 118. Hoehler FK, Tobis JS, Buerger AA. Spinal manipulation for low back pain. JAMA 1981;245(18):1835–8. [PubMed] [Google Scholar]
- 119. Moraska A. Therapist education impacts the massage effect on postrace muscle recovery. Med Sci Sports Exerc 2007;39(1):34–7. [DOI] [PubMed] [Google Scholar]
- 120. Schwellnus MP, Mackintosh L, Mee J. Deep transverse frictions in the treatment of iliotibial band friction syndrome in athletes: A clinical trial. Physiotherapy 1992;78(8):564–8. [Google Scholar]
- 121. Youssef EF, Shanb AS. Mobilization versus massage therapy in the treatment of cervicogenic headache: A clinical study. J Back Musculoskelet Rehabil 2013;26(1):17–24. [DOI] [PubMed] [Google Scholar]
- 122. Bodes-Pardo G, Pecos-Martin D, Gallego-Izquierdo T, et al. Manual treatment for cervicogenic headache and active trigger point in the sternocleidomastoid muscle: A pilot randomized clinical trial. J Manipulative Physiol Ther 2013;36(7):403–11. [DOI] [PubMed] [Google Scholar]
- 123. Demirturk F, Akarcali I, Akbayrak T, Citak I, Inan L. Results of two different manual therapy techniques in chronic tension-type headache. Pain Clin 2002;14(2):121–8. [Google Scholar]
- 124. Han SH, Hur MH, Buckle J, Choi J, Lee MS. Effect of aromatherapy on symptoms of dysmenorrhea in college students: A randomized placebo-controlled clinical trial. J Alternat Complement Med 2006;12(6):535–41. [DOI] [PubMed] [Google Scholar]
- 125. Hernandez-Reif M, Martinez A, Field T, et al. Premenstrual symptoms are relieved by massage therapy. J Psychosom Obstet Gynaecol 2000;21(1):9–15. [DOI] [PubMed] [Google Scholar]
- 126. Lämås K, Lindholm L, Stenlund H, Engström B, Jacobsson C. Effects of abdominal massage in management of constipation—A randomized controlled trial. Int J Nurs Studies 2009;46(6):759–67. [DOI] [PubMed] [Google Scholar]
- 127. Ou MC, Hsu TF, Lai AC, Lin YT, Lin CC. Pain relief assessment by aromatic essential oil massage on outpatients with primary dysmenorrhea: A randomized, double-blind clinical trial. J Obstet Gynaecol Res 2012;38(5):817–22. [DOI] [PubMed] [Google Scholar]
- 128. Seers K, Crichton N, Martin J, Coulson K, Carroll D. A randomised controlled trial to assess the effectiveness of a single session of nurse administered massage for short term relief of chronic non-malignant pain. BMC Nursing 2008;7:10 doi:10.1186/1472-6955-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Field TM, Sunshine W, Hernandez-Reif M, et al. Massage therapy effects on depression and somatic symptoms in chronic fatigue syndrome. J Chronic Fatigue Syndr 1997;3(3):43–51. [Google Scholar]
- 130. Brattberg G. Connective tissue massage in the treatment of fibromyalgia. Eur J Pain 1999;3(3):235–44. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.