Abstract
Objective
Given the millions of children who experience potentially traumatic injuries each year and the need to maximize emotional and physical health outcomes following pediatric injury, the current study examined the individual and collective contributions of the malleable variables of appraisals and coping in predicting PTSS in children following injury.
Method
This study combined data from three prospective investigations of recovery from pediatric injury (N = 688), in which children ages 8–17 years were recruited shortly after an injury (within 4 weeks). At baseline (T1), children completed measures of their threat appraisals of the injury event and PTSS. Six to twelve weeks later (T2) children completed a measure of coping and PTSS. Finally, PTSS was assessed again 6 months post-injury (T3).
Results
Structural equation modeling analyses provide evidence that appraisals and coping contribute to PTSS. Further, results suggest that escape coping mediates the relationship between threat appraisals and PTSS.
Conclusions
Early interventions designed to prevent or reduce PTSS after pediatric injury may be more successful if they primarily target modifying escape coping behaviors. To best inform clinical practice, future research should examine factors influencing the development of children’s appraisals and coping behaviors in the context of potentially traumatic events.
Keywords: appraisals, coping, PTSD, PTSS, child injury
Twenty million children and adolescents incur injuries annually in the United States, leading to 8.7 million emergency department visits and 241,000 inpatient admissions (Grossman, 2000). Following injury, many youth experience emotional and functional impairment such as new fears, mood changes, or decreased quality of life (Holbrook et al., 2005; Landolt, Vollrath, Gnehm, Sennhauser, 2009; Zatzick et al., 2008). Of particular concern, 16–19% of youth with injuries develop significant posttraumatic stress disorder symptoms (PTSS), which can persist for months to years (Kahana, Feeny, Youngstrom, & Drotar, 2006; Kassam-Adams, Marsac, Hildenbrand, & Winston, 2013). For a diagnosis of posttraumatic stress disorder (PTSD), youth must be exposed to a potentially traumatic event (e.g., injury and medical care) and report symptoms of re-experiencing or intrusion, avoidance, arousal, changes in mood or cognitions, and impaired functioning (American Psychiatric Association, 2013). Significant posttraumatic stress symptoms (PTSS), regardless of PTSD diagnostic status, are linked to negative outcomes in youth including poorer physical (e.g., somatic complaints), social (e.g., limitations in activities), and emotional functioning (e.g., sadness) (Holbrook et al., 2005; Stoddard & Saxe, 2001). Predictors of significant PTSS in youth after injury include prior trauma, sex, parental distress, social support, pre-existing psychopathology, and distress during and immediately after the event (Gerring et al., 2002; Kassam-Adams & Winston, 2004; McLaughlin et al., 2012). The high prevalence and impact of PTSS for youth with injuries necessitates research to more thoroughly understand the development of PTSS to inform preventive interventions.
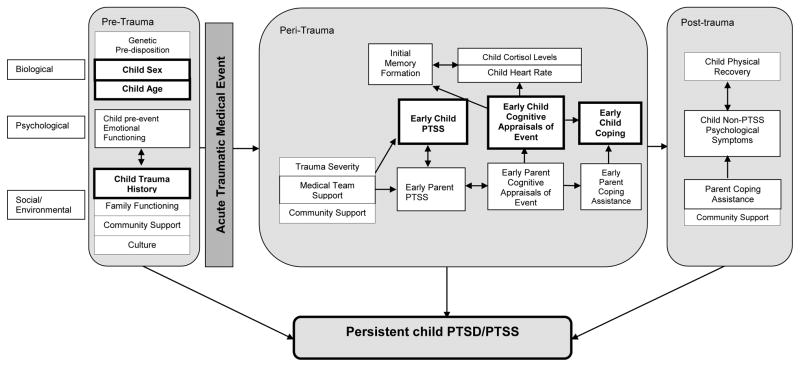
To examine factors contributing to the development and persistence of PTSS following acute medical trauma, Marsac and colleagues (2014) proposed a biopsychosocial theoretical model focusing on the role of peri-trauma processes during acute medical events. In this model, biological, psychological, and social factors before (pre-), during (peri-), and after (post-) the medical event have independent and interactional relationships that influence the development and maintenance of PTSS. Three of the central psychological constructs for understanding persistent PTSS highlighted by this model are child PTSS cognitive appraisals, and coping in the peri-trauma period (See Figure 1 and Marsac et al. (2014) for a full description of this model). Examining these psychological components via prospective studies of injured children can support identification of malleable peri-trauma variables (e.g., cognitive appraisals, coping) during injury and the early stages of recovery. Improved understanding of appraisals and coping may lead to more effective interventions to prevent the development of or lessen existing PTSS.
Figure 1.
Theoretical model for the development of child PTSD/PTSS following acute medical trauma*
*This figure is modified from the original to show the focused variables in this study. Specifically, variables included in this study are indicated in bold. The original figure can be found at the following: Marsac, M. L., Kassam-Adams, N., Delahanty, D. L., Widaman, K., F., & Barakat, L. P. (2014). Posttraumatic stress following acute medical trauma in children: a proposed model of bio-psycho-social processes during the peri-trauma period. Clinical Child and Family Psychology Review, 17(4), 399–411. doi: 10.1007/s10567-014-0174-2.
Folkman and Lazarus were the first to propose that cognitive appraisals play a substantial role in shaping the ways in which individuals engage in coping behaviors in the face of stressful events (Folkman & Lazarus, 1985; Lazarus, 1991; Lazarus & Folkman, 1984). Specifically, they posited that a primary appraisal occurs immediately upon exposure to a stressor, when an individual interprets the event as threatening. Using information collected during the primary appraisal process, the individual selects a coping technique (Folkman & Lazarus, 1985). Similarly, information processing models of anxiety and traumatic stress apply this appraisal process to the development of PTSS, such that threatening appraisals of the traumatic event (in this case, injury) can lead to behavioral strategies (e.g., avoidance) that directly contribute to PTSS and/or prevent the development of longer-term realistic and adaptive appraisals (Ehlers & Clark, 2000; Meiser-Stedman, 2002). These models have been expanded from adults to children, with consideration of possible developmental changes in how children encode and resolve trauma memories (Dalgleish, Meiser-Stedman, & Smith, 2005; Meiser-Stedman 2002; Ponnamperuma and Nicolson, 2015; Salmon & Bryant 2002). For example, one investigation found global negative appraisals (i.e., how they experienced their worst events in the past month) to be the best predictor of PTSS in adolescents who experienced multiple traumas resulting from a tsunami, explaining 22% of the variance in concurrent PTSS (Ponnamperuma & Nicolson, 2015). Hitchcock and colleagues (2015) also identified a strong role for appraisals (i.e., disturbing and permanent change/ feelings of fragility/believing the world to be scary post-trauma exposure) of a single incident trauma and its consequences in predicting PTSS in youth: Appraisals mediated the relationship between social support and PTSS. In examining specific types of appraisals in youth with injuries, perception of threat, negative appraisals about vulnerability to future harm, and negative interpretation of intrusive memories and rumination are related to worse emotional health (Bryant, Salmon, Sinclair, & Davidson, 2007; Ehlers, Mayou, & Bryant, 2003; Stallard & Smith, 2007).
The way in which a child copes with his or her injury is likewise related to PTSS, however the exact nature of this relationship remains unclear (Landolt, Vollrath, & Ribi, 2002; Stallard, Velleman, Langsford, & Baldwin, 2001; Zehnder, Prchal, Vollrath, & Landolt, 2006). While a number of classification schemes for coping exist, here we focus on control coping (i.e. engaging in behaviors to address the problem or feelings associated with the problem: cognitive restructuring, problem-solving, social support, relaxation) versus escape coping (i.e., engaging in behaviors in an attempt to avoid the problem: distraction, social withdrawal, self-criticism, blaming others, wishful thinking, resignation, emotional outburst; Cheng & Chan, 2003). For example, after a motor vehicle crash, children who met criteria for a PTSD diagnosis used more coping strategies overall (particularly avoidant/escape strategies) than children without PTSD (Stallard et al., 2001). Other investigations have found a weak relationship between use of active and support-seeking coping and PTSS among children with an injury or new illness, whereas use of religious coping predicted fewer PTSS one year later (Landolt et al., 2002; Zehnder et al., 2006). Only one study has examined the relative associations of appraisals and coping with concurrent PTSS in injured children; life threat, injustice, and permanency of change appraisals and negative cognitive coping (rumination, suppression, distraction) together accounted for 64% of the variance in PTSS 8 months after injury (Stallard & Smith, 2007). Thus, while research consistently identifies a relationship for overall coping and PTSS, there is variability in how specific types of coping relate to PTSS. To our knowledge, there have been no investigations of how appraisals and coping during peri-trauma independently and together predict future PTSS.
Current Study
The goal of the current study was to fill this gap in the literature by investigating threat appraisals and coping during the peri-trauma period and examining their independent contributions and interplay in predicting subsequent significant PTSS in youth recovering from injury. We hypothesized that 1) children’s threat appraisals during the peri-trauma period would predict greater PTSS, 2) control coping behaviors would predict fewer PTSS, 3) escape coping would predict greater PTSS, and 4) control and escape coping would mediate the relationship between peri-trauma threat appraisals and PTSS. Moreover, we sought to determine the relative contributions of appraisals and coping in predicting PTSS over time.
Methods
We aggregated data from three prospective studies that shared similar eligibility criteria, enrollment protocols, and assessment procedures (see below). Study 1 (n = 276) was designed to identify risk factors for PTSS following pediatric injury resulting from motor vehicle incidents (Kassam-Adams & Winston, 2004). Study 2 (n = 292) examined the efficacy of a stepped preventative care intervention for children hospitalized for pediatric injury (Kassam-Adams et al., 2011). Study 3 (n = 120) recruited children treated for injuries to assess the impact of informational materials for parents (Marsac, Donlon, Winston, & Kassam-Adams, 2013). In Studies 2 and 3, no significant group differences emerged on intervention outcomes; thus, groups were collapsed for analyses presented in this paper. Participants did not overlap across studies.
Participants
In each study, participants were recruited after seeking medical treatment for injury at a Level I Pediatric Trauma Center in the northeastern United States. Youth ages 8 to 17 years with sufficient English language proficiency and cognitive ability to comprehend and answer questions were eligible to participate. Injuries resulting from family violence or abuse were excluded. There were no differences in child sex across studies; youth in Study 1 were, on average, significantly younger (M = 11.3) than those in Study 2 (M = 12.1). Study 1 also had a higher proportion of Black youth than Studies 2 or 3. See Table 1 for demographic information.
Table 1.
Participant Demographics
| Study 1 n = 276 |
Study 2 n = 292 |
Study 3 n = 120 |
Total sample n = 688 |
|
|---|---|---|---|---|
|
| ||||
| CHILDREN | N (%) | N (%) | N (%) | N (%) |
|
| ||||
| Sex | ||||
| Male | 207 (75) | 210 (71.9) | 82 (68.3) | 499 (72.5) |
| Female | 69 (25) | 82 (28.1) | 38 (31.7) | 189 (27.5) |
|
| ||||
| Racial Background | ||||
| White | 108 (40.4) | 168 (57.5) | 69 (58) | 345 (50.9) |
| Black/ African American | 154 (57.7) | 89 (30.5) | 49 (41.2) | 292 (43.1) |
|
| ||||
| Ethnicity | ||||
| Hispanic | 5 (1.87) | 23 (7.87) | -- | 28 (5.3) |
| Non-Hispanic | 262 (98.1) | 269 (92.1) | -- | 503 (94.7) |
|
| ||||
| Unintentional Injury Circumstance | ||||
| Traffic (MVA/ RTA) | 199 (72.1) | 40 (13.7) | 19 (15.8) | 258 (37.6) |
| Fall | 77 (27.9) | 60 (20.6) | 30 (25.0) | 167 (24.3) |
| Sports | -- | 173 (59.4) | 66 (55.0) | 239 (34.7) |
| Other | -- | 9 (3.1) | 2 (1.6) | 11 (1.6) |
|
| ||||
| M (SD) | M (SD) | M (SD) | M (SD) | |
|
| ||||
| Age (years) | 11.3 (2.52) | 12.1 (2.46) | 11.9 (2.76) | 11.8 (2.56) |
|
| ||||
| CAREGIVERS | N (%) | N (%) | N (%) | N (%) |
|
| ||||
| Relationship to child | ||||
| Mother | 162 (77.9) | 249 (85.3) | 94 (79.7) | 505 (81.7) |
| Father | 26 (12.5) | 39 (13.4) | 22 (18.6) | 87 (14.1) |
| Other caregiver | 20 (9.6) | 4 (1.4) | 2 (1.7) | 26 (4.2) |
Procedure
For each of the studies from which the current dataset was derived, children were enrolled shortly after their injury, typically within several days (up to 4 weeks post-injury). Procedures were conducted in accordance with protocols approved by an institutional review board. Parents or legal guardians provided informed consent, and children provided assent. At baseline (T1), children and their parents provided demographic information, and children completed assessments of appraisals of the injury event and PTSS. The T2 (6–12 weeks) follow-up assessment included in-person or telephone administration of coping and PTSS measures. The T3 follow-up assessment included PTSS measures. See Table 2 for an overview of measures across studies. See Kassam-Adams and Winston (2004), Kassam-Adams et al. (2011), and Marsac et al. (2013) for more detailed information regarding each study’s procedures.
Table 2.
Timing of assessments and measures across studies.
| T1 (< 4 weeks since injury) | T2 (6–12 weeks) | T3 (6 months) | |
|---|---|---|---|
| Study 1 | Trauma History (TESI) Appraisals (STEPP) PTSS (CASQ, CATS) |
Coping (not assessed) PTSS (not assessed) |
PTSS (CAPS-CA, CATS) |
| Study 2 | Trauma History (STEPP) Appraisals (STEPP) PTSS (CPSS) |
Coping (KidCope) PTSS (CPSS) |
PTSS (CPSS) |
| Study 3 | Trauma History (STEPP) Appraisals (STEPP) PTSS (not assessed) |
Coping (KidCope) PTSS (ASC-Kids) |
PTSS (CPSS) |
Notes. TESI = Traumatic Events Screening Inventory. STEPP = Screening Tool for Early Predictors of PTSD. PTSS = posttraumatic stress symptoms. CASQ = Child Acute Stress Questionnaire. CATS = Child and Adolescent Trauma Survey Symptom Scale. CPSS = Child PTSD Symptom Scale. CAPS-CA = Clinician-Administered PTSD Scale for Children and Adolescents. ASC-Kids = Acute Stress Checklist for Children.
Measures
See Supplemental Table 1 for internal consistency of measures within and across the studies.
Trauma History
Traumatic Events Screening Inventory (TESI; Study1)
The TESI is asks for exposure to 15 types of potentially traumatic events (e.g. violence, hospitalizations) prior to the current index injury event (National Center for PTSD, 1996). For this study, if either the child or parent reported one or more prior traumatic events, trauma history was coded as positive.
Screening Tool for Early Predictors of PTSD (STEPP; Studies 2 and 3)
The STEPP (Winston, Kassam-Adams, Garcia-Espana, Ittenbach, & Cnaan, 2003) is a brief measure designed to predict later PTSS. In the current study, one STEPP item was used to assess trauma history: “Have you/your child ever seen or experienced anything very scary or terrible? If yes, what?” If either the child or parent endorsed this item, trauma history was coded as positive.
Appraisals
Screening Tool for Early Predictors of PTSD (STEPP; Studies 1, 2, and 3) (Winston et al., 2003)
See above. In the current study, two STEPP items assessed threat appraisals: “Did you feel really afraid?” (perceived fear) and “Did you think you might die?”(subjective life threat). Children responded yes or no to each item.
Coping
KidCope (Studies 1, 2, and 3)
The KidCope (Spirito, Stark, & Williams, 1988) is a 15-item measure. The KidCope has demonstrated moderate to high test-retest reliability and moderate associations with other measures of coping in children (Spirito et al., 1988). In the current study, we applied the factor-structure identified by Cheng and Chan (2003) to create Escape and Control coping latent variables. To ensure this factor-structure was appropriate, we conducted a confirmatory factor analysis. Our data demonstrated a reasonable fit to this model (χ2[86, N=688]=192.2, p<.001; CFI=.88; RMSEA=.04).
PTSD Symptoms (PTSS) Status
The three combined studies did not use a consistent measure of PTSS. Thus, in these analyses, PTSS status was calculated for each participant at each time point resulting in dichotomous scores of “presence of significant PTSS” versus “absence of significant PTSS”. In the measures section below, each measure that was used in determining PTSS status is described. Following procedures suggested by Kassam-Adams et al., 2012, in cases where multiple PTSS instruments were administered at the same time point (i.e., Study 1), the most psychometrically sound and empirically-supported measure was used to determine PTSS status (i.e., CASQ for T1; CAPS-CA for T3). Given that even subsyndromal PTSS are associated with functional impairments (Holbrook et al., 2005; Stoddard & Saxe, 2001), in this study, PTSS status was determined based on criteria described by Winston and colleagues (2003) (i.e., one moderate to severe symptom from each of the three DSM-IV-TR categories endorsed).
Clinician-Administered PTSD Scale for Children and Adolescents (CAPS-CA; Study 1)
The CAPS-CA (Nader et al., 2004) is a semi-structured interview that assesses DSM-IV diagnostic criteria for PTSD. Interviewers evaluate the frequency and intensity of each PTSD symptom, and the impact of these symptoms on functioning. Psychometric data indicate good internal consistency for each CAPS-CA subscale, and concurrent validity with other measures of PTSD (Newman, McMackin, Morrissey, & Erwin, 1997).
Child and Adolescent Trauma Survey (CATS) Symptom Scale (Study 1)
The symptom scale of the CATS is a 12-item brief measure of PTSS severity (March, 1999). Items are rated on a 4-point Likert-type scale and address the core symptom categories of PTSD (reexperiencing, avoidance, and hyperarousal). The CATS symptom severity score correlates highly with other measures of PTSD and clinician assessment. The CATS has demonstrated excellent psychometric properties (March, Amaya-Jackson, Murray, & Schulte, 1998).
Child Acute Stress Questionnaire (CASQ; Study 1)
The CASQ [originally created by adapting the Stanford Acute Stress Reaction Questionnaire (SASRQ; Cardeña, Koopman, Classen, Waelde, & Spiegel, 2000; Winston et al., 2002)] is an interviewer-administered questionnaire that assesses PTSS. Items are rated on a 3-point Likert-type scale and correspond to one of the four Acute Stress Disorder symptom categories. Initial psychometric data for the CASQ indicate excellent internal consistency, test-retest reliability, and factor analytical support for construct validity (Winston et al., 2002). The SASRQ scoring was applied in this sample.
Child PTSD Symptom Scale (CPSS; Studies 2 and 3)
The CPSS (Foa, Johnson, Feeny, & Treadwell, 2001) is a self-report instrument that yields both a PTSD symptom severity score and a determination of PTSD diagnostic status. Seventeen CPSS items correspond to the DSM-IV symptom criteria, rated on a four-point Likert scale (“not at all” to “five or more times a week”). The CPSS has shown excellent internal consistency, test–retest reliability, and convergent validity with structured clinical interview measures of PTSD (Foa et al., 2001).
Acute Stress Checklist for Children (ASC-Kids; Study 3)
The ASC-Kids (Kassam-Adams, 2006) is a brief, self-report measure of acute traumatic stress reactions in youth. It is on based acute stress disorder diagnostic criteria and associated features within the first month after exposure to a potentially traumatic event. Most items are rated on a 3-point Likert scale. The ASC-Kids has demonstrated strong test-retest reliability and internal consistency, as well as concurrent and predictive validity with other traumatic stress measures (Kassam-Adams, 2006).
Statistical Analysis
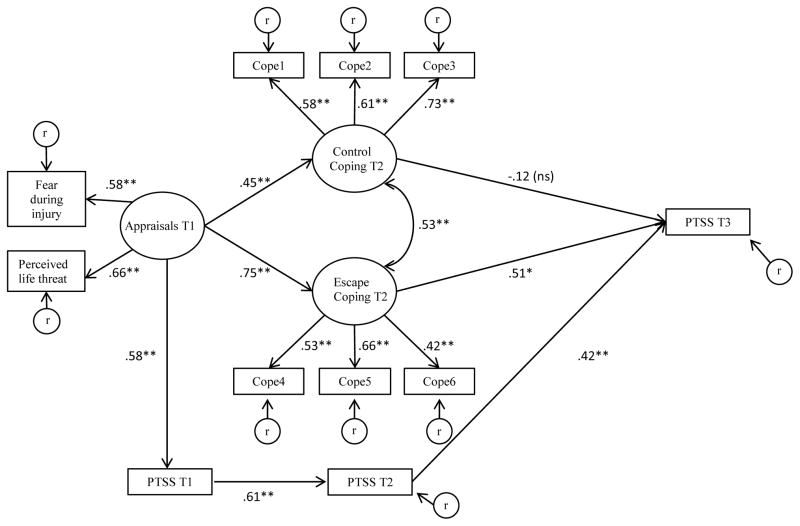
See Supplemental Table 2 for descriptive analyses including average time to assessments and frequencies of participants with a trauma history, significant PTSS, threat appraisals, and averages of types of coping. Structural equation modeling (SEM) was used to evaluate the study hypotheses, and test the overall fit of the theoretical model presented in Figure 2. Data was collected prospectively, over three time points, allowing for analyses to examine how appraisals and coping predicted PTSS status over time. Data analysis was conducted using Mplus (Muthén & Muthén, 1998–2011). SEM allowed us to model associations among both latent and manifest variables. Latent variables included Threat appraisals, Escape coping, and Control coping. For the appraisal latent variable, scale items were used as indicators. For the coping latent variables, we created six item parcels, (three for escape coping, three for control coping). Items within those two constructs were randomly assigned to each parcel (which is the average of those items). The decision to use item parcels were guided by multiple rationale. First, relative to individual items, item parcels themselves have superior psychometric qualities (higher reliability and more likely to be representative of the underlying construct). Second, the use of item parcels allowed the structural equation model to focus specifically on evaluating the fit of our theoretical model ((see Little, Cunningham, Shahar, & Widaman (2002) for more information on the appropriate use of item parcels in structural equations models). Manifest variables included PTSS status (i.e., presence vs. absence of significant symptoms) at each time point. We examined the bivariate associations among demographic variables (i.e., age, sex, trauma history) and each of the variables in the model. See Supplemental Table 3 for the correlation matrix. These analyses revealed small but significant positive correlations between age and sex with some of the model variables; we included these variables as covariates in our structural models.
Figure 2.
Model results examining the independent and inter-relationships of appraisals and coping with PTSS status over time.
Fit indices: χ2[74, N=688]=209.62, p <.001; CFI=.90; RMSEA=.052 (90% CI .043 –.060); Escape coping mediates the relationship between appraisals and PTSS at T3, z =2.00, p <.05; bootstrapped estimate, 0.38 (95% CI: 0.059–0.709), p < .05. Model includes covariates of study group, age, sex, and trauma history (all non-significant predictors of T3 PTSS). PTSS= Posttraumatic Stress Symptoms; T1 = < 4 weeks since injury; T2 = 6–12 weeks; T3 = 6 months.
Due to our use of categorical outcome variables in the model, we selected Weighted Least Squares for parameter estimation because the conventional estimator, Maximum Likelihood, requires the assumption of multivariate normality (Olsson, Foss, Troye, & Howell, 2000), which cannot be met with categorical manifest variables. Overall model fit was evaluated using three indices: the chi-square statistic, the comparative fit index (CFI), and the root mean square error of approximation (RMSEA). Values of the chi-square statistic increase with increasing misfit between a model and the empirical data. Although a non-significant chi-square is desirable, this statistic is highly influenced by sample size. Thus, other fit indices are typically examined. The CFI is a widely used relative fit index comparing the fit of an independence model (in which all variables are unrelated) to the fit of the theoretical model. CFI values of .90 or greater are desirable and indicate adequate fit (Hu & Bentler, 1999). Finally, the RMSEA provides a measure of absolute fit between the observed and model-implied covariance matrices. RMSEA values below .06 are indicative of good model fit (Hu & Bentler, 1999). We next tested our hypotheses of mediation of coping between appraisals and PTSS using bootstrapping procedures and the Sobel test for mediation.
Results
As demonstrated in Figure 2, we specified an autoregressive model in which T1 PTSS status (i.e., presence of significant PTSS vs absence of significant PTSS) predicts T2 PTSS status, which in turn predicts T3 PTSS status. Latent variables measuring Threat appraisals (T1), Escape coping (T2), and Control coping (T2) were added to this base autoregressive model as prospective predictors of PTSS at T3. Conceptually, our model tests whether these appraisal and coping latent variables predict PTSS status over time while controlling for previous PTSS (hypotheses 1–3). More specifically, the effect of Threat appraisals at T1 on later PTSS status was hypothesized to be mediated by coping at T2 (hypothesis 4).
Results suggested that the hypothesized model provided good fit to the data (χ2[74, N = 688] = 209.62, p < .001; CFI = .90; RMSEA = .052 [90% CI .043 –.060]). All factor loadings were statistically significant (all ps < .001), with standardized estimates > .42. Standardized effects are presented in Figure 2. Threat appraisals and PTSS status at T1 were significantly associated (β = .58, p < .001). Threat appraisals at T1 were also prospectively associated with Control coping (β = .45, p < .001) and Escape coping (β = .75, p < .001) at T2, with higher levels of Threat appraisals at T1 associated with higher levels of both Control and Escape coping at T2. Although Escape coping was in turn predictive of T3 PTSS status (β = .51, p < .05), Control coping was not (β = −.12, p > .05). We next tested whether Escape coping significantly mediated the effect of T1 Threat appraisals on T3 PTSS. First, we removed Escape coping from the model (retaining all other variables) to estimate the direct effect of T1 appraisals on T3 PTSS (β =.34, p < .05). Next, we tested the indirect effect: The bootstrapped estimate of the indirect effect was 0.38 (95% CI: 0.059–0.709), p < .05. and the Sobel test for mediation was significant (z = 2.00, p < .05). See Supplemental Table 4 for factor loadings, structural paths, and covariance.
Discussion
Many children suffer significant PTSS following pediatric injury (Kahana et al., 2006), underscoring the importance of understanding factors associated with the development of persistent PTSS in order to improve preventive interventions. Cognitive and information processing models have been applied to the development of PTSS, such that appraisals following a potentially traumatic event can lead to behavioral strategies that directly contribute to PTSS (Ehlers & Clark, 2000; Meiser-Stedman, 2002). Originally evaluated in adults, evidence has shown that negative appraisals of a trauma event and one’s reactions to the traumatic event independently predict long-term PTSD (Ehring, Ehlers, & Glucksman, 2008). Recent evidence has supported the extension of these findings to children (Hitchcock et al, 2015). However, mechanisms through which appraisal affect PTSS are not yet fully articulated. Toward this end, the current investigation evaluated a hypothesized model involving two potential mechanisms to target for intervention: peri-trauma threat appraisals and early coping. To our knowledge, this is the first study in children after medical trauma (in this case, injury) to examine the roles of appraisals and coping independently and collectively with regards to PTSS over time. Results supported hypothesized relationships as well as the overall proposed model, with one exception: Control coping was not significantly associated with PTSS over time. Four primary findings emerged as a result of this investigation. First, threat appraisals of the injury event were concurrently related to PTSS status (i.e., presence vs. absence of significant PTSS) at baseline (T1). Second, escape coping predicted PTSS status and mediated the relationship between appraisals and T3 PTSS status. Third, T1 PTSS status was predictive of PTSS status at T2 (6–12 weeks later), and T2 PTSS status was predictive of T3 PTSS status (6 month follow-up). Finally, taken together, the proposed model fit the data well (see Figure 2), providing empirical evidence to support key components of the model suggested by Marsac et al. 2014 (see Figure 1) and the relationships suggested by Ehlers and Clark (2000) and Meiser-Stedman (2002).
Consistent with previous research, appraisals were related to concurrent PTSS in this study, even with an only two-item appraisal assessment focused on threat during the injury (rather than global or ongoing appraisals)(Bryant et al., 2007; Ehlers et al., 2003; Meiser-Stedman et al., 2009; Stallard & Smith, 2007). Current results that threat appraisal serve as predictors of future PTSS are consistent with and extend previous research that suggests global appraisals help to predict future PTSS (Hitchcock et al., 2015). This highlights the complexity of assessment and modification of children’s appraisals post-injury. Findings also extend past research by identifying escape coping as a mediator between threat appraisals and later PTSS, thereby highlighting the important relations between these variables posited by Marsac et al.’s (2014) model. Given the independent role of escape coping in predicting PTSS status over time, results suggest that it may be more effective to develop interventions that target either coping alone or coping and appraisals together than to focus on appraisals alone. While escape coping was related to greater PTSS, control coping was not significantly related to PTSS. Thus, findings from this study suggest “what not to do” (i.e., distraction, social withdrawal, self-criticism, blaming others, wishful thinking, resignation, emotional outburst), but do not identify specific types of positive coping behaviors that may help prevent PTSS.
Of interest although the present investigation excluded children whose injuries resulted from abuse it, results are consistent with previous findings examining PTSS in adolescent victims of sexual abuse that indicate negative appraisals are associated with more avoidant/escape as well as active coping strategies. However, while escape coping mediated the relationship between threat appraisals and PTSS in the current study, this mediation was not identified in evaluating PTSS in adolescent victims of sexual abuse (Bal, Crombez, De Bourdeaudhuij, & Van Oost, P., 2009). Thus, while some research on children experiencing abuse may apply to children with unintentional injury, there may be differences in how coping can hinder or facilitate recovery.
Similar to findings from prior investigations, results from this study indicated a relationship between PTSS status across time (Kassam-Adams & Winston, 2004). Given the consistent findings about the relationship of PTSS over time, it may be that identifying peri-trauma PTSS could be helpful in determining who is at most risk and in most of need of close follow-up or intervention. However, previous research has suggested that while PTSS is related over time, early PTSS is not a sensitive predictor of later PTSS (Kassam-Adams & Winston, 2004). Thus, in trying to determine PTSS risk, other factors (such as appraisals and coping as demonstrated in this study as well as additional variables suggested in Figure 1) ought to be further investigated.
Clinical implications of our results support the application of a cognitive behavioral model in the treatment of children exposed to injury or medical trauma, as has been suggested by Meiser-Stedman (2002). In general, though more research is needed, evidence from this study suggests that appraising the injury event as threatening and engaging in escape coping may place children at risk for PTSS. Thus, using cognitive behavioral techniques such as cognitive restructuring specific to threat appraisals may be beneficial in helping children shift (unrealistic) appraisals of event reminders. Other cognitive behavioral techniques that directly target escape coping (e.g., addressing self-blame, reducing avoidance) may also help prevent PTSS. The current sample was not a clinical one and specific positive coping behaviors were not identified; thus more research is needed to understand treatment implications for children experiencing clinical levels of PTSS.
This study provides empirical support for the importance of children’s appraisals and coping with regard to subsequent PTSS, yet several limitations should be noted. First, due to the different methodologies across studies, PTSS was examined as a dichotomous variable, limiting statistical power. However, results were quite promising in spite of this limitation. Second, the assessment of appraisals was limited to two items. While the general findings on appraisals and PTSS were consistent with past research using validated assessment tools, the newer findings of the mediating role of escape coping should be interpreted with caution. Third, the relationship between escape coping and PTSS is challenging to assess due to overlap in the constructs. While this study provides initial evidence for a predictive relationship between escape coping and PTSS, future investigations should continue to delve further into these constructs. Fourth, internal consistency of the Kidcope was low in some of the samples; however, because low reliability attenuates relationships between variables, the paths observed in the paper are actually underestimates of how important each of these associations are. Finally, although the current study assessed PTSS over time, it did not take into account changing appraisals or coping behaviors over time. Future research should examine how all three variables change and interact over time, which would help to inform intervention development. Finally, as suggested by Marsac et al. (2014) and Ehlers and Clark (2003), numerous additional constructs should be considered in understanding the development of PTSS that were not evaluated in this investigation. In particular, the role of biological (e.g., physiological reactions) and social variables (e.g., SES, role of parents/caregivers) warrant additional investigation.
Conclusions
Given the paucity of empirically-supported preventive interventions for children exposed to acute trauma (Cohen, 2010; Foa, Friedman, Keane, & Cohen, 2008), research is needed to identify the mechanisms of action with the greatest potential to ameliorate PTSS to best guide intervention development (Kassam-Adams, 2014). For pediatric injury, malleable peri-trauma psychological processes (such as appraisals and coping) provide a unique opportunity for secondary prevention of PTSS. Future research should examine additional biopsychosocial factors (e.g., demographic, physiological, social/environmental) following acute medical events to provide a fuller picture of the development of PTSS, as well as the ways in which children develop appraisals and coping behaviors for stressful or potentially traumatic experiences.
Supplementary Material
Acknowledgments
This work was supported by the following grants: 1K23MH093618-01A1 (NIMH), R40MC00138 (MCHB of the HRSA), H34MC04365 (EMC), and R49CE987 (CDC).
Contributor Information
Meghan L. Marsac, The Center for Injury Research and Prevention, The Children’s Hospital of Philadelphia, Department of Psychiatry, University of Pennsylvania.
Jeffrey Ciesla, Department of Psychology, Kent State University.
Lamia P. Barakat, Division of Oncology, The Children’s Hospital of Philadelphia, Department of Pediatrics, University of Pennsylvania.
Aimee K. Hildenbrand, The Center for Injury Research and Prevention, The Children’s Hospital of Philadelphia, Department of Psychology, Drexel University.
Douglas L. Delahanty, Department of Psychology, Kent State University.
Keith Widaman, Department of Psychology, University of California-Davis.
Flaura K. Winston, The Center for Injury Research and Prevention, The Children’s Hospital of Philadelphia; Department of Pediatrics, University of Pennsylvania.
Nancy Kassam-Adams, The Center for Injury Research and Prevention, The Children’s Hospital of Philadelphia; Department of Pediatrics, University of Pennsylvania.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. American Psychiatric Publishing; 2013. [Google Scholar]
- Bal S, Crombez G, De Bourdeaudhuij I, Van Oost P. Symptomatology in adolescents following initial disclosure of sexual abuse: The roles of crisis support, appraisals and coping. Child Abuse & Neglect. 2009;33(10):717–727. doi: 10.1016/j.chiabu.2008.11.006. [DOI] [PubMed] [Google Scholar]
- Bryant R, Salmon K, Sinclair E, Davidson P. A prospective study of appraisals in childhood posttraumatic stress disorder. Behaviour Research and Therapy. 2007;45:2502–2507. doi: 10.1348/014466506X160704. [DOI] [PubMed] [Google Scholar]
- Cardeña E, Koopman C, Classen C, Waelde L, Spiegel D. Psychometric properties of the Stanford Acute Stress Reaction Questionnaire (SASRQ): A valid and reliable measure of acute stress. Journal of Traumatic Stress. 2000;13:719–734. doi: 10.1023/A:1007822603186. [DOI] [PubMed] [Google Scholar]
- Cheng S, Chan A. Factorial structure of the Kidcope in Hong Kong adolescents. Journal of Genetic Psychology. 2003;164:261–266. doi: 10.1080/00221320309597982. [DOI] [PubMed] [Google Scholar]
- Cohen J. Practice parameter for the assessment and treatment of children and adolescents with posttraumatic stress disorder. Journal of American Academic Child Adolescent Psychiatry. 2010;49(4):414–430. doi: 10.1016/j.jaac.2009.12.020. [DOI] [PubMed] [Google Scholar]
- Dalgleish T, Meiser-Stedman R, Smith P. Cognitive aspects of posttraumatic stress reactions and their treatment in children and adolescents: An empirical review and some recommendations. Behavioural and Cognitive Psychotherapy. 2005;33:459–486. doi: 10.1017/S1352465805002389. [DOI] [Google Scholar]
- Ehlers A, Clark D. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38(4):319–345. doi: 10.1016/S0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Mayou R, Bryant B. Cognitive predictors of posttraumatic stress disorder in children: results of a prospective longitudinal study. Behaviour Research and Therapy. 2003;41(1):1–10. doi: 10.1016/S0005-7967(01)00126-7. [DOI] [PubMed] [Google Scholar]
- Ehring T, Ehlers A, Glucksman E. Do cognitive models help in predicting the severity of posttraumatic stress disorder, phobia, and depression after motor vehicle accidents? A prospective longitudinal study. Journal of Consulting and Clinical Psychology. 2008;76:219–230. doi: 10.1037/0022-006X.76.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa E, Friedman M, Keane T, Cohen J, editors. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. 2. New York: Guilford Publication; 2008. [Google Scholar]
- Foa EB, Johnson KM, Feeny NC, Treadwell KR. The Child PTSD Symptom Scale: A preliminary examination of its psychometric properties. Journal of Clinical Child Psychology. 2001;30(3):376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus R. If it changes it must be a process: Study of emotion and coping during three stages of a college examination. Journal of Personality and Social Psychology. 1985;48(1):150–170. doi: 10.1037/0022-3514.48.1.150. [DOI] [PubMed] [Google Scholar]
- Gerring JP, Slomine B, Vasa RA, Grados M, Chen A, Rising W, … Ernst M. Clinical predictors of posttraumatic stress disorder after closed head injury in children. Journal Of The American Academy of Child & Adolescent Psychiatry. 2002;41(2):157–165. doi: 10.1097/00004583-200202000-00009. [DOI] [PubMed] [Google Scholar]
- Grossman D. The history of injury control and the epidemiology of child and adolescent injuries. The Future of Children. 2000;10(1):23–52. doi: 10.2307/1602824. [DOI] [PubMed] [Google Scholar]
- Hitchcock C, Ellis AA, Williamson P, Nixon RD. The prospective role of cognitive appraisals and social support in predicting children’s posttraumatic stress. Journal of Abnormal Child Psychology. 2015 doi: 10.1007/s10802-015-0034-7. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holbrook T, Hoyt D, Coimbra R, Potenza B, Sise M, Anderson J. Long-term posttraumatic stress disorder persists after major trauma in adolescents: New data on risk factors and functional outcome. Journal of Trauma-Injury Infection and Critical Care. 2005;58(4):764–769. doi: 10.1097/00005373-200408000-00096. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis:Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Kahana S, Feeny N, Youngstrom E, Drotar D. Posttraumatic stress in youth experiencing illnesses and injuries: An exploratory meta-analysis. Traumatology. 2006;12(2):148–161. doi: 10.1177/1534765606294562. [DOI] [Google Scholar]
- Kassam-Adams N. The Acute Stress Checklist for Children (ASC-Kids): Development of a child self-report measure. Journal of Traumatic Stress. 2006;19(1):129–139. doi: 10.1002/jts.20090. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N. Design, delivery, and evaluation of early interventions for children exposed to acute trauma. European Journal of Psychotraumatology. 2014;5 doi: 10.3402/ejpt.v5.22757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam-Adams N, García-España JF, Marsac ML, Kohser KL, Baxt C, … Winston F. A pilot randomized controlled trial assessing secondary prevention of traumatic stress integrated into pediatric trauma care. Journal of Traumatic Stress. 2011;24(3):252–259. doi: 10.1002/jts.20640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam-Adams N, Marsac ML, Hildenbrand AK, Winston FK. Posttraumatic stress following pediatric injury: Update on diagnosis, risk factors, and intervention. JAMA Pediatrics. 2013;167(12):1158–1165. doi: 10.1001/jamapediatrics.2013.2741. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N, Palmieri PA, Rork K, Delahanty DL, Kenardy J, Kohser KL, … McGrath C. Acute stress symptoms in children: results from an international data archive. Journal of American Academy of Child and Adolescent Psychiatry. 2012;51(8):812–820. doi: 10.1016/j.jaac.2012.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam-Adams N, Winston FK. Predicting child PTSD: The relationship between acute stress disorder and PTSD in injured children. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(4):403–411. doi: 10.1097/00004583-200404000-00006. [DOI] [PubMed] [Google Scholar]
- Landolt M, Vollrath M, Ribi K. Predictors of coping strategy selection in paediatric patients. Acta paediatr. 2002;91:945–960. doi: 10.1111/j.1651-2227.2002.tb02884.x. [DOI] [PubMed] [Google Scholar]
- Landolt MA, Vollrath ME, Gnehm HE, Sennhauser FH. Post-traumatic stress impacts on quality of life in children after road traffic accidents: prospective study. Austrailian and New Zealand Journal of Psychiatry. 2009;43(8):746–753. doi: 10.1080/00048670903001919. [DOI] [PubMed] [Google Scholar]
- Lazarus R. Emotion and adaptation. New York: Oxford Univesity Press; 1991. [Google Scholar]
- Lazarus R, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing Co; 1984. [Google Scholar]
- Little TD, Cunningham WA, Shahar G, Widaman KF. To parcel or not to parcel: Exploring the question, weighing the merits. Structural Equation Modeling. 2002;9(2):151–173. doi: 10.1207/S15328007SEM0902_1. [DOI] [Google Scholar]
- March JS. Assessment of pediatric posttraumatic stress disorder. In: Saigh PA, Bremner JD, editors. Posttraumatic stress disorder: A comprehensive text. Needham Heights, MA: Allyn & Bacon, Inc; 1999. pp. 199–218. [Google Scholar]
- March JS, Amaya-Jackson L, Murray MC, Schulte A. Cognitive-behavioral psychotherapy for children and adolescents with posttraumatic stress disorder after a single-incident stressor. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(6):585–593. doi: 10.1097/00004583-199806000-00008. [DOI] [PubMed] [Google Scholar]
- Marsac ML, Donlon KA, Winston FK, Kassam-Adams N. Child coping, parent coping assistance, and post-traumatic stress following paediatric physical injury. Child: Care, Health, and Development. 2013;39(2):171–177. doi: 10.1111/j.1365-2214.2011.01328.x. [DOI] [PubMed] [Google Scholar]
- Marsac ML, Kassam-Adams N, Delahanty DL, KFW, Barakat LP. Posttraumatic stress following acute medical trauma in children: a proposed model of bio-psycho-social processes during the peri-trauma period. Clinical child and family psychology review. 2014;17(4):399–411. doi: 10.1007/s10567-014-0174-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Koenen KC, Hill ED, Petukhova M, Sampson NA, Zaslavsk AM, Kessler RC. Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. Journal Of The American Academy of Child & Adolescent Psychiatry. 2013;52(8):815–830. doi: 10.1016/j.jaac.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meiser-Stedman R. Towards a cognitive -behavioral model of PTSD in children and adolescents. Clinical Child and Family Psychology. 2002;5(4):217–232. doi: 10.1023/a:1020982122107. [DOI] [PubMed] [Google Scholar]
- Meiser-Stedman R, Dalgleish T, Glucksman E, Yule W, Smith P. Maladaptive cognitive appraisals mediate the evolution of posttraumatic stress reactions: A 6-month follow-up of child and adolescent assault and motor vehicle accident survivors. Journal of Abnormal Psychology. 2009;118(4):9. doi: 10.1037/a0016945. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2011. [Google Scholar]
- Nader KO, Newman E, Weathers FW, Kaloupek DG, Kriegler JA, Blake DD. National Center for PTSD Clinician-Administered PTSD Scale for Children and Adolescents (CAPS-CA) Interview Booklet. Los Angeles: Western Psychological; 2004. [Google Scholar]
- National Center for PTSD. Pediatrics. Hanover, NH: Dartmouth Hitchcock Medical Center; 1996. Traumatic Events Screening Inventory (TESI) Version 8.3. [Google Scholar]
- Newman E, McMackin R, Morrissey C, Erwin B. Addressing PTSD and trauma-related symptoms among criminally involved male adolescents. Stresspoints. 1997;11:7. [Google Scholar]
- Olsson UH, Foss T, Troye SV, Howell RD. The performance of ML, GLS, and WLS estimation in structural equation modeling under conditions of misspecification and nonnormality. Structural Equation Modeling. 2000;7:557–595. doi: 10.1207/S15328007SEM0704_3. [DOI] [Google Scholar]
- Ponnamperuma T, Nicolson NA. Negative trauma appraisals and PTSD symptoms in Sri Lankan adolescents. Journal of Abnormal Child Psychology. 2015 doi: 10.1007/s10802-015-9985-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spirito A, Stark L, Williams C. Development of a brief coping checklist for use with pediatric populations. Journal of Pediatric Psychology. 1988;13:555–574. doi: 10.1093/jpepsy/13.4.555. [DOI] [PubMed] [Google Scholar]
- Stallard P, Smith E. Appraisals and cognitive coping styles associated with chronic post-traumatic symptoms in child road traffic accident survivors. Journal of child psychology and psychiatry, and allied disciplines. 2007;48(2):194–201. doi: 10.1111/j.1469-7610.2006.01692.x. [DOI] [PubMed] [Google Scholar]
- Stallard P, Velleman R, Langsford J, Baldwin S. Coping and psychological distress in children involved in road traffic accidents. British Journal of Clinical Psychology. 2001;40:197–208. doi: 10.1348/014466501163643. [DOI] [PubMed] [Google Scholar]
- Stoddard F, Saxe G. Ten year research review of physical injuries. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(10):1128–1145. doi: 10.1097/00004583-200110000-00007. [DOI] [PubMed] [Google Scholar]
- Winston FK, Kassam-Adams N, Garcia-Espana F, Ittenbach R, Cnaan A. Screening for risk of persistent posttraumatic stress in injured children and their parents. JAMA. 2003;290(5):643–649. doi: 10.1001/jama.290.5.643. [DOI] [PubMed] [Google Scholar]
- Zatzick DF, Jurkovich GJ, Fan MY, Grossman D, Russo J, Katon W, Rivara FP. Association between posttraumatic stress and depressive symptoms and functional outcomes in adolescents followed up longitudinally after injury hospitalization. Archives Pediatric Adolescent Medicine. 2008;162(7):642–648. doi: 10.1001/archpedi.162.7.642. [DOI] [PubMed] [Google Scholar]
- Zehnder D, Prchal A, Vollrath M, Landolt M. Prospective study of the effectiveness of coping in pediatric patients. Child Psychiatry and Human Development. 2006;36:351–368. doi: 10.1007/s10578-005-0007-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.