Abstract
Background
Recently, the range of tobacco products available in the United States and the patterns of tobacco product use have changed. While cigarette smoking prevalence has declined, dental professionals are likely to encounter many more users of new and alternative tobacco products among their patients.
Approach
This paper reviews conventional and new tobacco products currently available, their adverse oral and systemic health effects, and their prevalence of use in the US.
Results
Tobacco products other than cigarettes currently account for a substantial portion of tobacco use. For this reason, tobacco prevention and cessation counseling provided by dental professionals must address all tobacco products, including cigarettes, cigars, waterpipes (hookahs), and electronic cigarettes, as well as conventional and new smokeless tobacco products. Cigarette smoking and smokeless tobacco use are associated with immediate and long-term adverse health effects, including nicotine addiction, oral and systemic disease, and death. Novel products may attract new tobacco users, potentially leading to addiction that results in enduring tobacco product use and associated adverse health effects.
Practical Implications
Dental professionals regularly treat patients who use tobacco or who are at risk of initiating use. Therefore, it is essential that dental professionals are knowledgeable about tobacco products currently available and are able to answer patients' questions and to provide them with evidence-based tobacco-related counseling.
Keywords: Tobacco use trends, tobacco products, electronic cigarettes, smokeless tobacco, alternative tobacco products, continuing dental education, dental professional
Introduction
Since the Surgeon General's 1964 Report on Smoking and Health, smoking prevalence in the United States (US) has dropped from 42.4% in 1965 to 17.9% in 2013 among adults.1, 2 While this decline demonstrates great progress in tobacco control, tobacco use remains the single leading cause of preventable death nationally.1, 3 Each year, an estimated 480,000 people die prematurely from tobacco related illnesses,1 resulting in related direct medical costs reaching nearly $170 billion dollars annually.4
Despite overwhelming evidence linking tobacco use to systemic and oral disease, 21.3% of all US adults and 24.6% of all US high school adolescents report currently using at least one tobacco product.5, 6 Over 3,800 adolescents and young adults initiate tobacco use each day, and 80% of individuals who begin using regularly before age 18 will continue tobacco use into adulthood.1 Adolescents and young adults are also more likely than older adults to initiate use of multiple tobacco products. In 2014, a study of adolescents and young adults found that among current tobacco users, 25% reported using at least two tobacco products and 21% reported using more than two tobacco products.7 With these trends, 5.6 million US adolescents under the age of 18 today will subsequently die prematurely from tobacco related disease.3
The tobacco industry has expanded its product range. Besides cigarettes, products including conventional smokeless tobacco (oral snuff and chewing tobacco), snus, compressed dissolvable tobacco, cigars, waterpipes (hookah), and electronic cigarettes (e-cigarettes) account for a substantial portion of current product use. Recently, the two largest cigarette companies, Reynolds America (maker of Camel) and Altria (maker of Marlboro) expanded their offerings to include traditional and new smokeless tobacco products and e-cigarettes.8-10 Aggressive marketing includes claims that these products are “safe” or “harmless” alternatives to cigarettes. Such promotional tactics can be misleading, as these products are associated with tobacco use initiation and progression to regular use, with resulting nicotine addiction, especially among vulnerable populations, such as youth.11
Dental professionals are well positioned to help patients stop using tobacco and to prevent non-using patients from initiating use. To facilitate effective patient education and advice, this paper summarizes the most common types of tobacco products currently on the market, their actual and potential adverse health effects, and prevalence of use among various US populations.
Cigarettes
Description
Cigarettes consist of finely chopped tobacco leaves rolled in a paper wrapper (Figure 1a). During inhalation, smokers absorb nicotine and carcinogens, such as N-nitrosamines, aromatic hydrocarbons, and polonium-210.3, 12 Nicotine absorbed in the bloodstream enhances addiction potential, leading to tobacco and nicotine dependence. Additionally, smokers are exposed to tar, carbon monoxide, and over 7000 chemical toxins in tobacco smoke, which enter the bloodstream and are distributed throughout the body.3
Figure 1. Selected Tobacco Products Available in the United States.
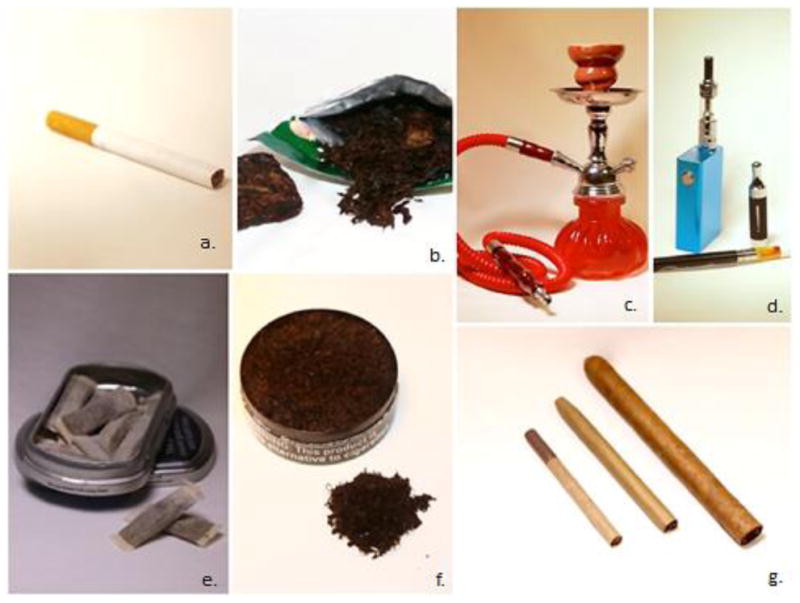
a.) Cigarette, b.) Chewing Tobacco, c.) Tobacco Waterpipe, d.) E-Cigarettes, e.) Snus, f.) Oral Snuff (Dip), and g.) Little Cigar, Cigarillo, and Cigar (In order from left to right).
Adverse health effects
Cigarette smoking has numerous short-term and long-term adverse health consequences for nearly every human organ system (Table 1). Cigarettes also affect individuals exposed to environmental tobacco smoke exhaled during cigarette smoking or accumulated residue on nearby surfaces, that has been linked to cancer, periodontal disease, respiratory and cardiovascular diseases, and adverse health effects among children and infants.1, 13
Table 1. Adverse health effects of cigarette smoking*.
| ORAL DISEASES AND CONDITIONS** |
|
|
|
| CARDIOVASCULAR DISEASE |
|
|
|
| RESPIRATORY DISEASE |
|
|
|
| INCREASED CANCER RISK |
|
|
|
| OBSTETRIC AND PEDIATRIC |
|
|
|
| OTHER CHRONIC DISEASES |
|
Modified from the US Department of Health and Human Services. “The health consequences of smoking—50 years of progress: A report of the surgeon general.” Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health 17 (2014).
Winn, Deborah M. “Tobacco use and oral disease.” Journal of dental education 65.4 (2001): 306-312.
Prevalence of use
Current adult cigarette use (reported as everyday or some days) in the US has dropped considerably in the last decade, from 20.9% in 2005 to 17.9% in 2013;2 yet smoking continues to be higher among males (20.5%) and in groups traditionally associated with economic or social disadvantage, such as those with household incomes below poverty level (29.2%), those with a General Education Development (GED) certificate (41.4%), and racial/ethnic minorities that include American Indian/Alaskan Natives (26.1%).2 In addition, lesbian, gay, bisexual, or transgender (LGBT) adults report much higher use (26.6%) than heterosexual adults (17.6%).2
Although declining, any cigarette use among US adolescents is alarming. According to the most recent data collected from the National Youth Tobacco Survey (NYTS), 9.2% of high school students and 2.5% of middle school students reported current use of cigarettes.6 However, 2013 data from the Youth Risk Behavior Surveillance (YRBS) survey reports a higher prevalence of current use among high school students (15.7%).14 According to data from the NYTS, among high school students, males (10.6%) and non-Hispanic White students (10.8%) reported a higher prevalence of smoking than females (7.9%) and non-Hispanic Black students (4.5%).6
Conventional and New Smokeless Tobacco (ST) Products
Description
Conventional ST products are oral snuff and chewing tobacco. Oral snuff is finely ground tobacco, packaged either loose or in tea bag–like sachets (Figure 1f). Typically, snuff users place a small amount (pinch) of oral snuff, also called a dip, in the reflex between the buccal mucosa and gingiva for about 30 minutes.15 Chewing tobacco is coarsely shredded tobacco, sometimes sold in bricks and twists (Figure 1b). Chewing tobacco users place a loose-leaf tobacco chaw, or compressed tobacco plug, against the buccal mucosa and chew it. Both dip and chewing tobacco users usually expectorate the tobacco-saliva juice, but more addicted users sometimes intentionally swallow it.16 Both oral snuff and chewing tobacco contain cancer-causing chemicals, including N-nitrosamines, aromatic hydrocarbons, formaldehyde, and polonium-210.17
Snus is a newer ST product in the US, modeled after Swedish snus, a relatively low-carcinogen, high-nicotine content oral tobacco snuff (Figure 1e).18-21 Snus is moist, finely ground tobacco, typically contained in small tea-bag-like sachets and used like oral snuff. Although Swedish and US snus share a name and appearance, they are manufactured differently. Swedish snus is heat treated for 2-3 days, generating a relatively sterile product. However, US snus is fermented, yielding higher carcinogen content.22 Although Swedish snus is usually known for having higher levels of total nicotine, the level of bio-available, or free nicotine varies greatly across brands of US and Swedish snus.23
Dissolvable compressed tobacco is a new ST product made from finely milled tobacco and available as orbs, sticks, and strips. These products closely resemble mints, toothpicks, or breath strips, and dissolve orally.24 Both snus and dissolvable tobacco products are marketed as spit-less (“dry”) products available in flavors, such as menthol, spice, alcohol, fruit, and candy. Their use is easily concealed, increasing their appeal to adolescents and young adults.19-21 Dissolvable tobacco products are available in a select number of locations in the US, whereas the sale of snus is generally widespread.
Adverse health effects
ST use is associated with increased risks of oral25 and pancreatic cancer,26 other oral mucosal lesions (e.g., oral leukoplakia),27-29 nicotine dependence,30 and possibly cardiovascular disease.31, 32 ST use also causes oral conditions such as gingival keratosis, tooth discoloration, halitosis, enamel erosion, gingival recession, alveolar bone damage, periodontal disease, dental caries due to sugars in the product, and tooth loss.33, 34 In addition, adolescent ST users are at greater risk of initiating smoking.35-38
There is uncertainty regarding the health effects of snus and dissolvable tobacco. Dissolvable tobacco products contain nicotine, flavoring compounds, binders, and humecants.24 Some of these compounds have the potential to cause adverse oral and systemic health effects, although little health data related to product use is available. Snus products may contain lower tobacco-specific nitrosamines (TSNA) levels than conventional ST products, but TSNA levels vary across brands.39 Snus and dissolvable tobacco products contain high nicotine levels, increasing addiction risk.
Prevalence of use
Unlike cigarettes, there has been little progress in reducing ST use in the US. ST remains a product almost exclusively used by males. For example, in 2013 and 2014, adult males (7.1%) and high school males (9.9%) reported significantly higher use prevalence than females (adult: 0.4%; high school: 1.2%).5, 6 Among adult males, the highest prevalence of use has been reported among non-Hispanic American Indian/Alaska Natives (16.2%) and Non-Hispanic Whites (4.7%).1
Among adolescents, ST use is especially high among rural adolescent male athletes and cigarette smokers, with use ranging from 18-42%.40-43 In addition, use among adolescents remains higher among non-Hispanic Whites (7.8%) than Hispanics (3.1%) and non-Hispanic Blacks (1.1).6 In 2014, snus use among US high school students was 3.0% for males and 0.8% for females, while dissolvable tobacco use was 0.8% for males.6 This lower prevalence of dissolvable tobacco use could be due to its' limited availability in the US.
Electronic Cigarettes
Description
Electronic cigarettes (e-cigarettes), also known as e-cigs, e-hookahs, hookah pens, or vapor pens, are electronic nicotine delivery systems (ENDS) that provide nicotine without combusting tobacco. Upon inhaling (often termed “vaping”) or pressing a button, e-cigarettes heat and convert a liquid mixture (often called e-liquid) into an aerosol (commonly termed vapor).44 Many e-cigarette users refer to this process as “vaping” and themselves as “vapers.” In fact, when asked about tobacco use, e-cigarette users may not refer to their use of e-cigarettes as “smoking,” or themselves as “smokers.” Many e-cigarettes often resemble conventional cigarettes, cigars, pens, or pipes, but e-cigarettes vary greatly in design (Figure 1d), including disposable or rechargeable forms, ranging in price from <$10 to >$200. Many rechargeable e-cigarettes can be re-filled and modified to deliver customized e-liquid or other drugs, such as marijuana.45 E-liquids typically contain propylene or polyethylene glycol, glycerin, additives, and nicotine and are available in over 7,700 flavors,44, 46 which may attract young users.10 Because e-cigarettes and e-liquid are not directly derived from the tobacco leaf, e-cigarettes are not universally considered a tobacco product. However, the FDA has issued a proposed rule that would extend the agency's authority to regulate e-cigarettes and other products including cigars, hookah, pipes, and dissolvable tobacco that meet the legal definition of a tobacco product.
Adverse health effects
E-cigarettes are relatively new devices; thus, no long-term evidence related to oral and systemic health effects exist. More than 460 e-cigarette brands are available in the US, with rapidly evolving product design, little to no regulation, and inconsistent quality control.47, 48 Differences in the labeled and true nicotine levels in e-liquid solutions,49-51 and the mode of heating and converting e-liquid into an aerosol create extensive variability in nicotine levels and other chemicals delivered to users;52 posing challenges when examining health effects.
Current evidence describing potential toxin exposure from e-cigarettes comprises mainly studies of first and second-generation devices. E-cigarette aerosols have been shown to contain nicotine, ultrafine particles, tobacco specific nitrosamines, and other toxic compounds such as acetaldehyde, acrolein, and toluene, although at significantly lower levels than cigarettes.44, 49, 53-55 Similar ultrafine particles in tobacco smoke and polluted air have been associated with respiratory and cardiovascular disease risks via pulmonary and systemic inflammation.56, 57 Moreover, adverse event reports suggest that e-cigarettes may increase risk of adverse health effects including seizure, increased heartbeat, disorientation, airway resistance, congestive heart failure, pneumonia, and second degree burns from faulty devices.48 However, no causal relationship has been determined. In 2014, 41.7% of the combined calls to poison control centers related to conventional cigarettes and e-cigarettes were for e-cigarette exposures, with 51.1% of those exposures among children aged 0 to 5 years.58 Recently, a report from Public Health England stated that e-cigarettes are 95% less harmful than cigarettes;59 however, the studies used to support this finding have been scrutinized for having conflicts of interest and weak methodology.60 In addition, many of the expert panelists who generated the “95% safer” claim were later shown to have connections to the tobacco industry and are established champions of e-cigarettes as “harm reduction” devices; a strategy readily embraced by the tobacco industry.61 To date, no studies have reported the oral health effects of e-cigarettes. However, due to the nicotine level in most e-cigarette products, it is possible that e-cigarettes may adversely affect oral tissues and immune response.62-66 Further research regarding the oral and systemic health effects of e-cigarettes is needed.
Prevalence of use
E-cigarettes have significantly grown in popularity over the past 5 years, particularly among youth and young adults. According to data from the NYTS, e-cigarettes are now the most commonly used tobacco product among adolescents in the US, surpassing cigarettes.6 Among US high school students, current e-cigarette use (past 30 days) tripled from 4.5% in 2013 to 13.4% in 2014.6, 67 Similar increases were observed among middle school students (1.1% to 3.9%).6 Although most adolescent e-cigarette users are dual users with cigarettes, many adolescents who have tried e-cigarettes have never tried cigarettes.68 E-cigarette users have also reported much higher (43.9%) intentions to smoke cigarettes than never users of e-cigarettes.69 This trend suggests that US adolescents may be initiating tobacco use with e-cigarettes, increasing nicotine dependence risk, and initiating dual use with cigarettes or other tobacco products.5
Among adults, e-cigarette use is highest among 18-24 year olds (8.3%) and lowest among individuals 65 years or older (1.1%).5 Use is highest among adults without a high school diploma (8.1%), followed by those with some college (5.4%).5 In 2013, e-cigarette use was notably elevated among LGBT individuals (9.7%) compared to heterosexual individuals (4.1%).5
Waterpipe (Hookah) Tobacco Smoking
Description
Smoking tobacco from a waterpipe, also known as a hookah, is an ancient form of smoking, traditionally used by men in the Middle East, North Africa, and Asia,70 but growing in popularity globally, including among women. A typical waterpipe consists of a head, body, water bowl, and one or more hoses, each containing a mouthpiece (Figure 1c). Tobacco is placed in the head and heated using charcoal or embers.71,72 Users inhale smoke through the mouthpiece after it passes through the water bowl, carried by the hose.71 Waterpipes are often used in groups and social gatherings where individuals take turns smoking from the same waterpipe.70
Waterpipe tobacco, also known as “shisha” or “maassel” typically consists of shredded tobacco leaves, often pre-packaged and sold as various fruit, spice, or candy-flavored varieties that may give off a pleasant aroma when heated.71 Waterpipe tobacco products are not regulated in the US, and are available for purchase via internet vendors, dedicated supply shops, and hookah cafes. Waterpipe equipment including modified mouthpieces, chemical additives, and mesh fittings, are often sold under unsubstantiated claims of reducing or eliminating hookah smoke's negative health effects.72 These claims, as well as the social aspects, affordability, and establishment of hookah cafes, contribute to its appeal among youth and young adults.73
Adverse health effects
Although research is limited, existing evidence suggests that waterpipe smoking has negative health effects similar to those of cigarettes. Waterpipe tobacco smoking has been associated with lung cancer, oral cancer, respiratory disease, low birth weight, and periodontal disease.74, 75 Smoke generated from waterpipe tobacco contains high toxic compound levels, including heavy metals, TSNAs, and carbon monoxide,76, 77 as well as nicotine. Furthermore, studies have shown that during a typical 60-minute waterpipe smoking session71, 78 users take roughly 200 puffs with an average puff volume of 500ml.79 Therefore, this typical waterpipe smoking session involves inhaling over 100 times the volume of smoke compared to that from a single cigarette (10–13 puffs with an average puff volume of about 45 ml)72,80 In addition, waterpipe smoking may also lead to the initiation of cigarette use,81 further increasing the risk of disease.
Prevalence of use
Similar to e-cigarettes, waterpipe smoking popularity is increasing in the US, particularly among adolescents and young adults. In the US, 3% of middle school students and 14.3% of high school students reported ever using hookah waterpipes in 2014.6 Among high school students, current waterpipe use (past 30-day) significantly increased from 2011 to 2014 (4.1% to 9.4%), becoming their second most commonly used tobacco product.6 Similarly, waterpipe smoking is the second most commonly used product among young adults age 18-24 years (18.2%).5 It has been estimated that 1 in 5 college students report waterpipe smoking within the past year.82 Use is also higher among adult males (4.8%) than adult females (2.7%) and LGBT individuals have reported higher use (10.7%) than individuals identifying as heterosexual (3.5%).5
Cigars, Cigarillos, and Little Cigars
Description
Cigars, including traditional premium cigars, cigarillos, and little cigars, are tightly rolled tobacco bundles wrapped in a tobacco leaf or other manufactured tobacco wrapper (Figure 1g). Cigars are dried, aged, and fermented through chemical and bacterial reactions, conferring a different taste and smell than cigarettes.83 Traditional premium or large cigars contain over 0.5 ounces of tobacco. Regular cigars, often called cigarillos, or cheroots, look like smaller versions of traditional large cigars, and are usually sold in packs.84 The smallest cigars, often called “little cigars” resemble cigarettes and typically come in packs of 20.83
Unlike cigarettes, cigars are not subject to US federal regulation. The FDA has banned flavored cigarettes, but cigarillos and little cigars are sold in a variety of flavors, including chocolate, fruit, and candy. Cigars can be marketed and sold at lower cost than cigarettes due to fewer restrictions on their manufacturing and much lower taxes.85 Ease of purchase, low cost, availability in flavors, and the misconception that cigars are “safer” than cigarettes all contribute to cigars' appeal to adolescents and young adults.86, 87
Adverse health effects
Smoke produced from cigars contains the same, if not more, toxic and carcinogenic compounds as cigarettes.84 The pH of cigar smoke is usually less acidic than that of cigarettes, allowing for absorption of nicotine in the oral mucosa. For this reason, many cigar users claim that they do not inhale cigar smoke into their lungs. However, partial inhalation is common and the lack of complete inhalation increases the environmental smoke produced, exposing individuals nearby to the same toxins and carcinogens as the cigar user.85 Due to the fermentation process, cigar tobacco has high nitrogen compound levels that when burnt release several TSNAs.84 In addition, cigar smoke contains high concentrations of harmful substances such as nitrogen oxides, ammonia, carbon monoxide, and tar.83-85 Cigar smoking is associated with oral, lip, laryngeal, esophageal, pancreatic and lung cancers.84, 85, 88 In addition, daily cigar smokers have an increased risk of coronary heart disease, aortic aneurysms, chronic obstructive pulmonary disease,84, 88, 89 and periodontal disease.90 Cigars also expose users to nicotine, increasing risks of addiction, continued use, and dual use with other tobacco products.85
Prevalence of use
Cigar use is much higher among adult men (10.1%) than adult women (1.5%).5 In addition, racial and ethnic minorities and those with lower socio-economic status demonstrate high levels of cigar use. In 2013, non-Hispanic adults of multiple races reported the highest use of cigars (9.6%), followed by non-Hispanic Black adults (6.5%). In the same year, adults with annual household incomes below $20,000 reported the highest cigar use (7.4%).5
Although cigar use has decreased among the adolescent population in general, substantial gender, racial and ethnic, and regional differences in cigar use exist. Cigars continue to be the most commonly used tobacco product among non-Hispanic Black high school students (8.8%), and high school males are more likely to smoke cigars (10.8%) than females (5.5%).6 In 2011, 35.9% of high school cigar users reported using flavored little cigars,87 and in certain states, adolescent cigar use is higher than cigarette use.14
Harm Reduction Controversy
The availability of non-combustible tobacco products (i.e., smokeless tobacco and e-cigarettes) has stimulated controversy among health professionals and researchers regarding harm reduction. Harm reduction is invoked in reference to products designed for continued tobacco use, but with promised reduced risk of tobacco-related diseases.31 Harm reduction proponents argue that using e-cigarettes91 or ST may produce fewer toxins than burned cigarettes, decreasing smoking-related health risks,92, 93 or helping users to quit smoking.94-96 Opposing views argue that even if a specific product is associated with less toxin exposure than cigarettes, harm may not be reduced if uptake of non-combustible products results in subsequent smoking initiation, relapse to smoking, or continued use of both products. Many maintain that there is no safe form of tobacco and that FDA approved nicotine replacement products (nicotine gum, patch, lozenge, inhaler, and nasal spray) in combination with cessation counseling behavior change are the safest and most effective treatments for smoking cessation.31 Moreover, there is insufficient evidence that e-cigarettes or ST help individuals to stop smoking.97-99 In contrast, among US adult males, ST use is very strongly associated with current smoking, and dual-users (users of both products) have high levels of tobacco dependence.100 Unsuccessful past-year quit attempts by daily smokers are more prevalent among dual-users (41.2%) than among smokers who had never used ST (29.6%).100 More than twice as many US youth currently use two or more tobacco products than use cigarettes alone.101, 102 Many argue that there is a need to assess potential harm at both the population and individual levels, because there is strong evidence that ST use among adolescent males leads to smoking.31, 35-37 In addition, the use of snus among adolescents and young adults has been associated with cigarette initiation.81 New longitudinal evidence also suggests that young teens who try e-cigarettes are more likely to initiate use of cigarettes, cigars, and hookah than peers who have never used e-cigarettes.103 However, future research is needed to determine whether e-cigarette use leads to regular use of combustible tobacco products. There is a pressing need for further study of the overall health implications of non-combustible tobacco products at the individual and population levels.
Implications for Dental Professionals
The expanding market of available tobacco products poses new challenges for dental professionals. Dentists and dental hygienists must now address a wide range of tobacco products when screening patients, documenting use of traditional and new tobacco products in health records, and providing effective tobacco prevention and cessation counseling. Dental professionals must take caution when considering tobacco industry claims of “harmlessness” and reduced risk related to new and emerging tobacco products. When “light” cigarettes were first introduced in the US market, well intended government agencies and health professionals reinforced their marketing only to discover later that use of “light” cigarettes had no associated health benefits compared to use of regular cigarettes.104 Accurately communicating to patients the current scientific evidence related to various tobacco products will allow patients the opportunity to make informed decisions whether to continue, quit, or refrain from using.
The effort to reduce tobacco use in the US must also include involvement at the local, state, and national levels. Dental professionals need to encourage local government agencies, dental and dental hygiene organizations, community leaders, insurers, schools, and families to support tobacco control efforts in their community. This support of tobacco control includes supporting laws restricting the marketing of tobacco products, programs that provide comprehensive tobacco cessation counseling, tobacco cessation training for health professionals, school-based tobacco use prevention programs, dental and dental hygiene programs that include tobacco dependence education in their curriculum, and other activities. By working together in multi-disciplinary partnerships, dental professionals can help reduce, and potentially eliminate, the burden of tobacco on society.
Conclusion
Tobacco products other than cigarettes account for a substantial portion of tobacco use. Although this review is not exhaustive of all tobacco products (e.g., bidis and pipes have not been included), it highlights many common types of tobacco products, their potential and actual adverse health effects, and their prevalence of use in the US. Such information is critical for dental professionals to provide effective tobacco use prevention and cessation counseling. By counseling patients individually and advocating for community tobacco control efforts, dental professionals have the opportunity to prevent a lifetime of addiction among their patients, save lives, improve quality of life, and reduce the burden of tobacco use on the health of the public. For more resources and information related to tobacco products, tobacco-use prevalence in the United States, current tobacco-use cessation counseling recommendations, and strategies for implementing in-office tobacco education and tobacco-use cessation counseling, please see the list of resources (Table 2).
Table 2.
Resources: For additional information related to tobacco products, tobacco use prevalence in the US, current tobacco cessation counseling recommendations, and strategies for implementing in-office tobacco education and cessation counseling, we recommend the following resources:
|
Acknowledgments
Support to Dr. Chaffee was provided from the NIH National Center for Advancing Translational Sciences (KL2TR000143). The supporting organization had no role in the conduct of this research. The information presented is solely the responsibility of the authors and does not necessarily represent the official views of the supporting organization. The authors declare that there is no conflict of interest, financial or otherwise, related to the publication of this research. Dr. Walsh passed away while this article was in press. Her many contributions to enhance tobacco control by dental professionals will have a lasting impact
References
- 1.US Department of Health and Human Services The health consequences of smoking—50 years of progress: A report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. p. 17. [Google Scholar]
- 2.Jamal A, Agaku IT, O'Connor E, King BA, Kenemer JB, Neff L. Current cigarette smoking among adults—United States, 2005–2013. MMWR Morb Mortal Wkly Rep. 2014;63:1108–12. [PMC free article] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services The health consequences of smoking: A report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. p. 62. [Google Scholar]
- 4.Xu X, Bishop EE, Kennedy SM, Simpson SA, Pechacek TF. Annual healthcare spending attributable to cigarette smoking: An update. Am J Prev Med. 2015;48:326–33. doi: 10.1016/j.amepre.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agaku IT, King BA, Husten CG, et al. Tobacco product use among adults--United States, 2012-2013. MMWR Morb Mortal Wkly Rep. 2014;63:542–7. [PMC free article] [PubMed] [Google Scholar]
- 6.Arrazola RA, Singh T, Corey CG, et al. Tobacco use among middle and high school students—United States, 2011-2014. MMWR Morb Mortal Wkly Rep. 2015;64:381–5. [PMC free article] [PubMed] [Google Scholar]
- 7.Soneji S, Sargent J, Tanski S. Multiple tobacco product use among US adolescents and young adults. Tob Control. 2014 doi: 10.1136/tobaccocontrol-2014-051638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Altria group, inc. agrees to acquire UST inc., world's leading moist smokeless tobacco manufacturer, for $69.50 per share in cash. Richmond, VA: Altria Group, Inc.; UST Inc.; 2008. Available from: http://investor.altria.com/phoenix.zhtml?c=80855&p=irol-newsArticle&ID=1194435. [Google Scholar]
- 9.Reynolds American. Reynolds American completes acquisition of Conwood. Winston-Salem, NC; 2006. [press release] Available from: http://www.reynoldsamerican.com/About-Us/Press-Releases/Press-Release-Details-/2006/Reynolds-American-Completes-Acquisition-of-Conwood/default.aspx. [Google Scholar]
- 10.Legacy fh. Vaporized - E-cigarettes, advertising, and youth. Legacy, UC San Francisco: Center for Tobacco Control Research and Education. 2014 Available from: http://escholarship.org/uc/item/7cq84675.
- 11.US Department of Health and Human Services. Preventing tobacco use among youth and young adults: A report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. p. 2. [Google Scholar]
- 12.Boyle P, Ariyaratne Y, Barrington R, et al. Tobacco: Deadly in any form or disguise. The Lancet. 2006;367:1710–2. doi: 10.1016/S0140-6736(06)68747-3. [DOI] [PubMed] [Google Scholar]
- 13.Gold DR, Wang X, Wypij D, Speizer FE, Ware JH, Dockery DW. Effects of cigarette smoking on lung function in adolescent boys and girls. N Engl J Med. 1996;335:931–7. doi: 10.1056/NEJM199609263351304. [DOI] [PubMed] [Google Scholar]
- 14.Kann L, Kinchen S, Shanklin SL, et al. Youth risk behavior surveillance–United States, 2013. MMWR Surveill Summ. 2014;63:1–168. [PubMed] [Google Scholar]
- 15.Severson HH, Eakin EG, Lichtenstein E, Stevens VJ. The inside scoop on the stuff called snuff: An interview study of 94 adult male smokeless tobacco users. J Subst Abuse. 1990;2:77–85. doi: 10.1016/s0899-3289(05)80047-1. [DOI] [PubMed] [Google Scholar]
- 16.Ebbert JO, Patten CA, Schroeder DR. The fagerström test for nicotine dependence-smokeless tobacco (FTND-ST) Addict Behav. 2006;31:1716–21. doi: 10.1016/j.addbeh.2005.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janbaz KH, Qadir MI, Basser HT, Bokhari TH, Ahmad B. Risk for oral cancer from smokeless tobacco. Contemp Oncol (Pozn) 2014;18:160–4. doi: 10.5114/wo.2014.40524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US Federal Trade Commission. Smokeless tobacco report for the years 2002-2005. Washington: Federal Trade Commission; 2007. [Google Scholar]
- 19.Hatsukami DK, Ebbert JO, Feuer RM, Stepanov I, Hecht SS. Changing smokeless tobacco products: New tobacco-delivery systems. Am J Prev Med. 2007;33:S368–78. doi: 10.1016/j.amepre.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 20.Carpenter CM, Connolly GN, Ayo-Yusuf OA, Wayne GF. Developing smokeless tobacco products for smokers: An examination of tobacco industry documents. Tob Control. 2009;18:54–9. doi: 10.1136/tc.2008.026583. [DOI] [PubMed] [Google Scholar]
- 21.King D, Burritt C. Philip Morris USA to unveil smokeless Marlboro product. [Accessed September 9, 2014];Bloomberg News. 2007 [Google Scholar]
- 22.Foulds J, Ramstrom L, Burke M, Fagerstrom K. Effect of smokeless tobacco (snus) on smoking and public health in sweden. Tob Control. 2003;12:349–59. doi: 10.1136/tc.12.4.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stepanov I, Jensen J, Hatsukami D, Hecht SS. New and traditional smokeless tobacco: Comparison of toxicant and carcinogen levels. Nicotine Tob Res. 2008;10:1773–82. doi: 10.1080/14622200802443544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rainey CL, Conder PA, Goodpaster JV. Chemical characterization of dissolvable tobacco products promoted to reduce harm. J Agric Food Chem. 2011;59:2745–51. doi: 10.1021/jf103295d. [DOI] [PubMed] [Google Scholar]
- 25.Boffetta P, Hecht S, Gray N, Gupta P, Straif K. Smokeless tobacco and cancer. The Lancet Oncology. 2008;9:667–75. doi: 10.1016/S1470-2045(08)70173-6. [DOI] [PubMed] [Google Scholar]
- 26.Alguacil J, Silverman DT. Smokeless and other noncigarette tobacco use and pancreatic cancer: A case-control study based on direct interviews. Cancer Epidemiol Biomarkers Prev. 2004;13:55–8. doi: 10.1158/1055-9965.epi-03-0033. [DOI] [PubMed] [Google Scholar]
- 27.Little SJ, Stevens VJ, LaChance PA, Severson HH, Bartley MH, Leben JR. Smokeless tobacco habits and oral mucosal lesions in dental patients. J Public Health Dent. 1992;52:269–76. doi: 10.1111/j.1752-7325.1992.tb02288.x. [DOI] [PubMed] [Google Scholar]
- 28.Grady D, Greene J, Daniels TE, et al. Oral mucosal lesions found in smokeless tobacco users. J Am Dent Assoc. 1990;121:117–23. doi: 10.14219/jada.archive.1990.0139. [DOI] [PubMed] [Google Scholar]
- 29.Ernster VL, Grady DG, Greene JC, et al. Smokeless tobacco use and health effects among baseball players. JAMA. 1990;264:218–24. [PubMed] [Google Scholar]
- 30.Ebbert JO, Carr AB, Dale LC. Smokeless tobacco: An emerging addiction. Med Clin North Am. 2004;88:1593–605. doi: 10.1016/j.mcna.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 31.Hatsukami DK, Lemmonds C, Tomar SL. Smokeless tobacco use: Harm reduction or induction approach? Prev Med. 2004;38:309–17. doi: 10.1016/j.ypmed.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 32.Hatsukami DK, Slade J, Benowitz NL, et al. Reducing tobacco harm: Research challenges and issues. Nicotine Tob Res. 2002;4(Suppl 2):S89–101. doi: 10.1080/1462220021000032852. [DOI] [PubMed] [Google Scholar]
- 33.Tomar SL, Winn DM, Swango PA, Giovino GA, Kleinman DV. Oral mucosal smokeless tobacco lesions among adolescents in the United States. J Dent Res. 1997;76:1277–86. doi: 10.1177/00220345970760060701. [DOI] [PubMed] [Google Scholar]
- 34.Walsh P, Joel BE. The oral effects of smokeless tobacco. J Can Dent Assoc. 2000;66:22–5. [PubMed] [Google Scholar]
- 35.Forrester K, Biglan A, Severson HH, Smolkowski K. Predictors of smoking onset over two years. Nicotine Tob Res. 2007;9:1259–67. doi: 10.1080/14622200701705357. [DOI] [PubMed] [Google Scholar]
- 36.Severson HH, Forrester KK, Biglan A. Use of smokeless tobacco is a risk factor for cigarette smoking. Nicotine Tob Res. 2007;9:1331–7. doi: 10.1080/14622200701705209. [DOI] [PubMed] [Google Scholar]
- 37.Walsh MM, Langer TJ, Kavanagh N, et al. Smokeless tobacco cessation cluster randomized trial with rural high school males: Intervention interaction with baseline smoking. Nicotine Tob Res. 2010;12:543–50. doi: 10.1093/ntr/ntq022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haddock CK, Weg MV, DeBon M, et al. Evidence that smokeless tobacco use is a gateway for smoking initiation in young adult males. Prev Med. 2001;32:262–7. doi: 10.1006/pmed.2000.0802. [DOI] [PubMed] [Google Scholar]
- 39.Stepanov I, Biener L, Knezevich A, et al. Monitoring tobacco-specific N-nitrosamines and nicotine in novel marlboro and camel smokeless tobacco products: Findings from round 1 of the new product watch. Nicotine Tob Res. 2012;14:274–81. doi: 10.1093/ntr/ntr209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Walsh MM, Ellison J, Hilton JF, Chesney M, Ernster VL. Spit (smokeless) tobacco use by high school baseball athletes in California. Tob Control. 2000;9(Suppl 2):II32–9. doi: 10.1136/tc.9.suppl_2.ii32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gansky SA, Ellison JA, Kavanagh C, Isong U, Walsh MM. Patterns and correlates of spit tobacco use among high school males in rural California. J Public Health Dent. 2009;69:116–24. doi: 10.1111/j.1752-7325.2008.00109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mumford EA, Levy DT, Gitchell JG, Blackman KO. Smokeless tobacco use 1992-2002: Trends and measurement in the current population survey-tobacco use supplements. Tob Control. 2006;15:166–71. doi: 10.1136/tc.2005.012807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Howard-Pitney B, Winkleby MA. Chewing tobacco: Who uses and who quits? findings from NHANES III, 1988-1994. National health and nutrition examination survey III. Am J Public Health. 2002;92:250–6. doi: 10.2105/ajph.92.2.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grana R, Benowitz N, Glantz SA. E-cigarettes: A scientific review. Circulation. 2014;129:1972–86. doi: 10.1161/CIRCULATIONAHA.114.007667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Givens A, Chang P. I-team: E-cigarettes, used to smoke marijuana, spark new concerns. [Accessed December 2, 2014];NBC New York. 2013 Available from: http://www.nbcnewyork.com/news/local/ECigarettes-Drugs-Marijuana-Vapor-Pens-Smoking-I-Team-227269001.html.
- 46.Brandon TH, Goniewicz ML, Hanna NH, et al. Electronic nicotine delivery systems: A policy statement from the American association for cancer research and the american society of clinical oncology. Clin Cancer Res. 2015;21:514–25. doi: 10.1158/1078-0432.CCR-14-2544. [DOI] [PubMed] [Google Scholar]
- 47.Trtchounian A, Talbot P. Electronic nicotine delivery systems: Is there a need for regulation? Tob Control. 2011;20:47–52. doi: 10.1136/tc.2010.037259. [DOI] [PubMed] [Google Scholar]
- 48.Chen IL. FDA summary of adverse events on electronic cigarettes. Nicotine Tob Res. 2013;15:615–6. doi: 10.1093/ntr/nts145. [DOI] [PubMed] [Google Scholar]
- 49.Goniewicz ML, Knysak J, Gawron M, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23:133–9. doi: 10.1136/tobaccocontrol-2012-050859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cheah NP, Chong NW, Tan J, Morsed FA, Yee SK. Electronic nicotine delivery systems: Regulatory and safety challenges: Singapore perspective. Tob Control. 2014;23:119–25. doi: 10.1136/tobaccocontrol-2012-050483. [DOI] [PubMed] [Google Scholar]
- 51.Cameron JM, Howell DN, White JR, Andrenyak DM, Layton ME, Roll JM. Variable and potentially fatal amounts of nicotine in e-cigarette nicotine solutions. Tob Control. 2014;23:77–8. doi: 10.1136/tobaccocontrol-2012-050604. [DOI] [PubMed] [Google Scholar]
- 52.Williams M, Talbot P. Variability among electronic cigarettes in the pressure drop, airflow rate, and aerosol production. Nicotine Tob Res. 2011;13:1276–83. doi: 10.1093/ntr/ntr164. [DOI] [PubMed] [Google Scholar]
- 53.Pellegrino RM, Tinghino B, Mangiaracina G, et al. Electronic cigarettes: An evaluation of exposure to chemicals and fine particulate matter (PM) Ann Ig. 2012;24:279–88. [PubMed] [Google Scholar]
- 54.Ingebrethsen BJ, Cole SK, Alderman SL. Electronic cigarette aerosol particle size distribution measurements. Inhal Toxicol. 2012;24:976–84. doi: 10.3109/08958378.2012.744781. [DOI] [PubMed] [Google Scholar]
- 55.Zhang Y, Sumner W, Chen DR. In vitro particle size distributions in electronic and conventional cigarette aerosols suggest comparable deposition patterns. Nicotine Tob Res. 2013;15:501–8. doi: 10.1093/ntr/nts165. [DOI] [PubMed] [Google Scholar]
- 56.Pope IIICA, Ezzati M, Dockery DW. Fine-particulate air pollution and life expectancy in the united states. N Engl J Med. 2009;360:376–86. doi: 10.1056/NEJMsa0805646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mehta S, Shin H, Burnett R, North T, Cohen AJ. Ambient particulate air pollution and acute lower respiratory infections: A systematic review and implications for estimating the global burden of disease. Air Quality, Atmosphere & Health. 2013;6:69–83. doi: 10.1007/s11869-011-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chatham-Stephens K, Law R, Taylor E, et al. Notes from the field: Calls to poison centers for exposures to electronic cigarettes--United States, 2010-2014. MMWR Morb Mortal Wkly Rep. 2014;63:292–3. [PMC free article] [PubMed] [Google Scholar]
- 59.McNeill A, Brose L, Calder R, Hitchman S, Hajek P, McRobbie H. E-cigarettes: An evidence update. Public Health England. 2015 doi: 10.1016/S0140-6736(15)00079-3. https://www.gov.uk/government/publications/e-cigarettes-an-evidence-update. [DOI] [PubMed]
- 60.Polosa R. E-cigarettes: Public health england's evidence based confusion? The Lancet. 2015 doi: 10.1016/S0140-6736(15)00133-6. [DOI] [PubMed] [Google Scholar]
- 61.Gornall J. Public health england's troubled trail. BMJ. 2015;351:h5826. doi: 10.1136/bmj.h5826. [DOI] [PubMed] [Google Scholar]
- 62.Darby I, Hodge P, Riggio M, Kinane D. Clinical and microbiological effect of scaling and root planing in smoker and non-smoker chronic and aggressive periodontitis patients. J Clin Periodontol. 2005;32:200–6. doi: 10.1111/j.1600-051X.2005.00644.x. [DOI] [PubMed] [Google Scholar]
- 63.Wendell KJ, Stein SH. Regulation of cytokine production in human gingival fibroblasts following treatment with nicotine and lipopolysaccharide. J Periodontol. 2001;72:1038–44. doi: 10.1902/jop.2001.72.8.1038. [DOI] [PubMed] [Google Scholar]
- 64.Payne J, Johnson G, Reinhardt R, Dyer J, Maze C, Dunning D. Nicotine effects on PGE2 and IL-1β release by LPS-treated human monocytes. J Periodont Res. 1996;31:99–104. doi: 10.1111/j.1600-0765.1996.tb00470.x. [DOI] [PubMed] [Google Scholar]
- 65.Pabst MJ, Pabst KM, Collier JA, et al. Inhibition of neutrophil and monocyte defensive functions by nicotine. J Periodontol. 1995;66:1047–55. doi: 10.1902/jop.1995.66.12.1047. [DOI] [PubMed] [Google Scholar]
- 66.Checchi L, Ciapetti G, Monaco G, Ori G. The effects of nicotine and age on replication and viability of human gingival fibroblasts in vitro. J Clin Periodontol. 1999;26:636–42. doi: 10.1034/j.1600-051x.1999.261002.x. [DOI] [PubMed] [Google Scholar]
- 67.Centers for Disease Control and Prevention (CDC) Notes from the field: electronic cigarette use among middle and high school students—United States, 2011–2012. MMWR 2013. 2014;62:729–30. [PMC free article] [PubMed] [Google Scholar]
- 68.Centers for Disease Control and Prevention (CDC) Notes from the field: Electronic cigarette use among middle and high school students - United States, 2011-2012. MMWR Morb Mortal Wkly Rep 2013. 62:729–30. [PMC free article] [PubMed] [Google Scholar]
- 69.Bunnell RE, Agaku IT, Arrazola RA, et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National youth tobacco survey, 2011-2013. Nicotine Tob Res. 2015;17:228–35. doi: 10.1093/ntr/ntu166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rice VH. Water pipe smoking among the young: The rebirth of an old tradition. Nurs Clin North Am. 2012;47:141–8. doi: 10.1016/j.cnur.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.American Lung Association An emerging deadly trend: Waterpipe tobacco use. Washington: American Lung Association; 2007. PDF–222 KB) [Google Scholar]
- 72.Waterpipe tobacco smoking: Health effects, research needs and recommended actions by regulators Geneva. World Health Organization; Switzerland: World Health Organization; 2005. [Google Scholar]
- 73.Martinasek MP, McDermott RJ, Martini L. Waterpipe (hookah) tobacco smoking among youth. Current problems in pediatric and adolescent health care. 2011;41:34–57. doi: 10.1016/j.cppeds.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 74.Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: A systematic review. Int J Epidemiol. 2010;39:834–57. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- 75.Knishkowy B, Amitai Y. Water-pipe (narghile) smoking: An emerging health risk behavior. Pediatrics. 2005;116:e113–9. doi: 10.1542/peds.2004-2173. [DOI] [PubMed] [Google Scholar]
- 76.Maziak W, Ward KD, Afifi Soweid RA, Eissenberg T. Tobacco smoking using a waterpipe: A re-emerging strain in a global epidemic. Tob Control. 2004;13:327–33. doi: 10.1136/tc.2004.008169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shihadeh A. Investigation of mainstream smoke aerosol of the argileh water pipe. Food and Chemical Toxicology. 2003;41:143–52. doi: 10.1016/s0278-6915(02)00220-x. [DOI] [PubMed] [Google Scholar]
- 78.Smith-Simone S, Maziak W, Ward KD, Eissenberg T. Waterpipe tobacco smoking: Knowledge, attitudes, beliefs, and behavior in two U.S. samples. Nicotine Tob Res. 2008;10:393–8. doi: 10.1080/14622200701825023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shihadeh A, Azar S, Antonios C, Haddad A. Towards a topographical model of narghile water-pipe café smoking: A pilot study in a high socioeconomic status neighborhood of beirut, lebanon. Pharmacology Biochemistry and Behavior. 2004;79:75–82. doi: 10.1016/j.pbb.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 80.Djordjevic MV, Stellman SD, Zang E. Doses of nicotine and lung carcinogens delivered to cigarette smokers. J Natl Cancer Inst. 2000;92:106–11. doi: 10.1093/jnci/92.2.106. [DOI] [PubMed] [Google Scholar]
- 81.Soneji S, Sargent JD, Tanski SE, Primack BA. Associations between initial water pipe tobacco smoking and snus use and subsequent cigarette smoking: Results from a longitudinal study of US adolescents and young adults. JAMA Pediatr. 2014 doi: 10.1001/jamapediatrics.2014.2697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Grekin ER, Ayna D. Waterpipe smoking among college students in the United States: A review of the literature. Journal of American College Health. 2012;60:244–9. doi: 10.1080/07448481.2011.589419. [DOI] [PubMed] [Google Scholar]
- 83.American Cancer Society. Am Cancer Soc. Atlanta, GA: American Cancer Society; 2014. [Accessed September, 15 2014]. Cigar smoking. Available from: http://www.cancer.org/acs/groups/cid/documents/webcontent/002965-pdf.pdf. [Google Scholar]
- 84.National Cancer Institute (NCI) Cigars: Health effects and trends, smoking and tobacco control monograph 9. Bethesda, MD: National Institutes of Health, National Cancer Institute; 1998. Available from: http://cancercontrol.cancer.gov/brp/tcrb/monographs/9/m9_complete.PDF. [Google Scholar]
- 85.Baker F, Ainsworth SR, Dye JT, et al. Health risks associated with cigar smoking. JAMA. 2000;284:735–40. doi: 10.1001/jama.284.6.735. [DOI] [PubMed] [Google Scholar]
- 86.Tavernise S. In all flavors, cigars draw in young smokers. The New York Times. 2013 Available from: http://www.nytimes.com/2013/08/18/health/in-all-flavors-cigars-draw-in-young-smokers.html?_r=0.
- 87.King BA, Tynan MA, Dube SR, Arrazola R. Flavored-little-cigar and flavored-cigarette use among US middle and high school students. Journal of Adolescent Health. 2014;54:40–6. doi: 10.1016/j.jadohealth.2013.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chang CM, Corey CG, Rostron BL, Apelberg BJ. Systematic review of cigar smoking and all cause and smoking related mortality. BMC Public Health. 2015;15:390. doi: 10.1186/s12889-015-1617-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Iribarren C, Tekawa IS, Sidney S, Friedman GD. Effect of cigar smoking on the risk of cardiovascular disease, chronic obstructive pulmonary disease, and cancer in men. N Engl J Med. 1999;340:1773–80. doi: 10.1056/NEJM199906103402301. [DOI] [PubMed] [Google Scholar]
- 90.Albandar JM, Streckfus CF, Adesanya MR, Winn DM. Cigar, pipe, and cigarette smoking as risk factors for periodontal disease and tooth loss. J Periodontol. 2000;71:1874–81. doi: 10.1902/jop.2000.71.12.1874. [DOI] [PubMed] [Google Scholar]
- 91.Polosa R, Rodu B, Caponnetto P, Maglia M, Raciti C. A fresh look at tobacco harm reduction: The case for the electronic cigarette. Harm Reduct J. 2013;10:19. doi: 10.1186/1477-7517-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Frost-Pineda K, Appleton S, Fisher M, Fox K, Gaworski CL. Does dual use jeopardize the potential role of smokeless tobacco in harm reduction? Nicotine Tob Res. 2010;12:1055–67. doi: 10.1093/ntr/ntq147. [DOI] [PubMed] [Google Scholar]
- 93.Rodu B. The scientific foundation for tobacco harm reduction, 2006-2011. Harm Reduct J. 2011:8. doi: 10.1186/1477-7517-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tonnesen P, Mikkelsen K, Bremann L. Smoking cessation with smokeless tobacco and group therapy: An open, randomized, controlled trial. Nicotine Tob Res. 2008;10:1365–72. doi: 10.1080/14622200802238969. [DOI] [PubMed] [Google Scholar]
- 95.Rodu B, Phillips CV. Switching to smokeless tobacco as a smoking cessation method: Evidence from the 2000 national health interview survey. Harm Reduct J. 2008;5:18, 7517–5-18. doi: 10.1186/1477-7517-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tilashalski K, Rodu B, Cole P. Seven year follow-up of smoking cessation with smokeless tobacco. J Psychoactive Drugs. 2005;37:105–8. doi: 10.1080/02791072.2005.10399753. [DOI] [PubMed] [Google Scholar]
- 97.Grana RA, Popova L, Ling PM. A longitudinal analysis of electronic cigarette use and smoking cessation. JAMA internal medicine. 2014;174:812–3. doi: 10.1001/jamainternmed.2014.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Vickerman KA, Carpenter KM, Altman T, Nash CM, Zbikowski SM. Use of electronic cigarettes among state tobacco cessation quitline callers. Nicotine Tob Res. 2013;15:1787–91. doi: 10.1093/ntr/ntt061. [DOI] [PubMed] [Google Scholar]
- 99.Tomar SL, Fox CH, Connolly GN. Electronic cigarettes: The tobacco industry's latest threat to oral health? J Am Dent Assoc. 2015;146:651–3. doi: 10.1016/j.adaj.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 100.Tomar SL, Alpert HR, Connolly GN. Patterns of dual use of cigarettes and smokeless tobacco among US males: Findings from national surveys. Tob Control. 2010;19:104–9. doi: 10.1136/tc.2009.031070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lee YO, Hebert CJ, Nonnemaker JM, Kim AE. Youth tobacco product use in the United States. Pediatrics. 2015;135:409–15. doi: 10.1542/peds.2014-3202. [DOI] [PubMed] [Google Scholar]
- 102.Bombard JM, Rock VJ, Pederson LL, Asman KJ. Monitoring polytobacco use among adolescents: Do cigarette smokers use other forms of tobacco? Nicotine Tob Res. 2008;10:1581–9. doi: 10.1080/14622200802412887. [DOI] [PubMed] [Google Scholar]
- 103.Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314:700–7. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wilkenfeld J, Henningfield J, Slade J, Burns D, Pinney J. It's time for a change: Cigarette smokers deserve meaningful information about their cigarettes. J Natl Cancer Inst. 2000;92:90–2. doi: 10.1093/jnci/92.2.90. [DOI] [PubMed] [Google Scholar]


