Abstract
Background
Despite increased attention to dentists’ role in curbing opioid misuse, abuse, and diversion, information regarding prescribing practices and the frequency of multiple concurrent opioid prescriptions among dental patients is limited.
Methods
Prescription drug monitoring program (PDMP) data for South Carolina representing dispensed medication for patients prescribed at least one opioid by a dentist over the most recently available two-year frame (2012–2013) was reviewed. Descriptive analyses examined: (1) types, frequency of dental opioid prescriptions; and, (2) frequency of existing multiple concurrent opioid prescriptions among dental patients.
Results
Nearly all dispensed dental opioid prescriptions (99.9%; n = 653,650) were for immediate release opioids and were initial fills (96.2%). Hydrocodone (76.1%) and oxycodone (12.2%) combination products were the most frequently dispensed opioids prescribed by dentists. Individuals under 21 years of age received 11.2% of dentist prescribed opioids dispensed. Patients with multiple concurrent opioid prescriptions were identified within 30-day (n=113,818), 90-day (n=166,124), and 180-day (n=205,576) timeframes.
Conclusions
Dentists prescribed a high volume of immediate release opioids dispensed in South Carolina. A notable minority of dental patients had incident(s) of multiple pre-existing opioid prescriptions, a factor implicated in patient misuse, abuse, overdose, and diversion
Practical Implications
Use of a PDMP prior to prescribing provides a record of controlled substances dispensed to a patient, and may inform prescribing, coordination of care, and addiction screening or referral. Patients should be provided information regarding misuse behaviors and their risks, as well as the importance of secure storage and disposal of leftover opioid medications.
Keywords: Oxycodone, Patient Education, Prescriptions, Drug
As the legitimate use of opioids for pain management has increased, so has the incidence of opioid misuse and diversion. (1) The most recent data available from the National Survey on Drug Use and Health (NSDUH) indicate that approximately 4.5 million persons aged 12 or older reported past month non-medical use of pain relievers, including taking more than prescribed, combining with other substances (e.g., alcohol, sedatives), taking for reasons other than to reduce physical pain (e.g., to reduce anxiety, increase energy, improve sleep), lending to others, borrowing or diverting from others, multiple requests for early refills, reporting medications lost or stolen, and obtaining medications from multiple sources. (2) Opioids are the most prescribed medication of any drug category in the U.S., exceeding 250 million prescriptions annually. (3) Legitimate prescriptions, and the diversion (intentional and unintentional) of those prescriptions, constitute a major source of abused opioids. (4–7)
Unintended diversion (obtaining the medication from a family member or friend) has also been consistently cited as a leading source of opioids among the burgeoning population of adolescent abusers. (8) Consequences and costs of prescription opioid misuse can include the development of more chronic and severe substance use disorders, overdose, and unintentional fatality. (9–11) Recent analysis indicates that emergency department visits related to opioid overdose have quadrupled over the past two decades. (12) Documented increases in treatment admissions, morbidity, and mortality related to opioids are very strongly correlated with national increases in overall consumption levels of opioids. (13)
Opioids are frequently used for acute pain management associated with dental procedures in emergency and clinical settings. (14,15) National surveillance data suggests that dentists follow primary care physicians as the second leading prescriber of immediate release opioids and, as such, dentists have been identified as having an important role in opioid abuse prevention efforts. (16,17) However, research on dental prescribing practices is scant. Initial reports focused on opioid prescribing by oral and maxillofacial surgeons (N=563) following third molar extraction, a common dental procedure performed at an estimated annual rate of 3.5 million. (18) Results indicated that the majority (85.0%) of dentists almost always prescribed an opioid, most often hydrocodone with acetaminophen, with instructions to take for pain “as needed.” Data regarding dental opioid prescribing are now a decade old and largely reliant on self-report, so the extent to which they apply to current practices is unclear. More recently, Ashrafioun and colleagues provided an initial estimate of the prevalence of nonmedical opioid use and diversion among dental patients receiving care at an academic outpatient dental clinic. (19) Results indicated that more than one-third (37.9%) of patients reported some form of nonmedical use of prescription opioids and 6.5% of respondents reported diverting their medication to others. Results suggest that dental patients may be at heightened risk for misusing or diverting their opioid medications; however, data are notably limited by non-representative samples and reliance on self-report.
Despite increased attention to physician prescribing practices, as well as the role of the dental prescriber in promoting (and preventing) opioid misuse, abuse, and diversion, no objective, representative data currently exists regarding dental opioid prescribing practices and the frequency of multiple concurrent opioid prescriptions amongst dental patients. (16,20,21) Dentists typically have limited exposure to addictions training/education and are not regular users of opioid risk mitigation strategies, such as prescription drug monitoring programs (PDMPs). (22,23) PDMPs collect data from pharmacies on dispensed controlled substances and make it available to authorized prescribers and pharmacists. (24) This information may be valuable in identifying patients with pre-existing concurrent opioid prescriptions, a documented risk indicator for abuse, diversion (intentional or unintentional), and overdose. (25–27) The aims of the current study are to use data from a statewide PDMP to examine: (A) types and frequency of opioids prescribed by dentists; and (B) frequency with which dentists prescribed an opioid to a patient with pre-existing concurrent opioid prescriptions, a potential patient-level indicator of increased risk for abuse, diversion, and unintentional overdose.
Methods
South Carolina’s PDMP (SCRIPTS) is an online service accessible to all registered prescribers and dispensers of controlled substances. All dispensers (e.g., pharmacies and dispensing prescribers) of Schedule II, III, and IV controlled substances are required to collect and report the following information to the data repository: (A) dispenser Drug Enforcement Agency (DEA) number; (B) date dispensed; (C) prescription number; (D) status (refill versus new); (E) National Drug Code; (F) quantity dispensed; (G) approximate number of days supplied; (H) patient name, address, and date of birth; (I) prescriber’s DEA number; and, (J) date of issue of prescription. Once entered, data is made available online to registered prescribers and pharmacists regarding specific patients’ history of dispensed controlled substances.
Following the approval of a Memorandum of Understanding (MOU) between the South Carolina Department of Health and Environmental Control, Health Information Designs (HID) LLC, and the Medical University of South Carolina, a segment of the South Carolina Prescription Drug Monitoring Program data, representing prescriptions dispensed between January 1, 2012 and December 31, 2013 was provided to the research team. The data timeframe reflects the most recent two years of data at the time of the MOU approval and is consistent with the most recent, publicly available, administrative prescribing data. (28) The dataset was produced as follows: (A) HID identified any patient receiving an opioid prescription from at least one dentist as indicated by the DEA controlled substance prescriber identification number; (B) The delivered database included any additional prescriptions in the PDMP for each patient, regardless of prescribing physician; (C) Patients were matched using a cluster ID created by using algorithms established by HID allowing them to return ID matches on similar names, birth dates and addresses and produce unique, HIPPA (Health Insurance Portability and Accountability Act, passed by Congress in 1996) compliant identifiers for each patient.
The delivered dataset contained the following information: de-identified unique prescriber number, prescriber type (dentist or other), de-identified unique patient number, year of birth, gender, zip code (first three digits only), prescription number, National Drug Code, drug name and strength (as listed in HID’s NDC table), quantity of drug dispensed, number of days’ supplied, refill status, date prescription was written, and date dispensed. Upon the research team’s receipt of the delivered dataset, all NDC identifiers in the resultant database were matched to the corresponding prescription type using the PDMP Assist Conversion table created by the Centers for Disease Control National Center for Injury Prevention and Control in September 2014. Identifiers not matched in the PDMP Assist resource, were queried in Find-A-Code (www.findacode.com/ndc/search.php). Matched identifiers were categorized by drug type (immediate release opioid, extended release opioid, opioid unspecified, other). Given the de-identified nature of all variables, the Institutional Review Board deemed this study “not human subjects research.”
Data Analysis Plan
The delivered dataset contained a total of 2,333,431 prescription records. Prescription records with missing data for drug type, fill status (new or refill), prescriber type, or age of patient recipient were excluded. In total, 4,155 records (0.2%) were excluded leaving the final analyzed data set with a total of 2,329,276 prescription records. Descriptive statistics were computed on the final data set to determine total number of prescribers as well as total number and demographics of patients and their prescriptions. Incidents of concurrent opioid prescriptions were assessed. To do so, the number of pre-existing dispensed opioids for that given patient were counted within the specified timeframe (i.e., 30 days prior to dental opioid prescription, 90 days prior to dental opioid prescription, and 180 days prior to dental opioid prescription) for each dental opioid prescription in the database.
Results
Dental Opioid Prescriptions
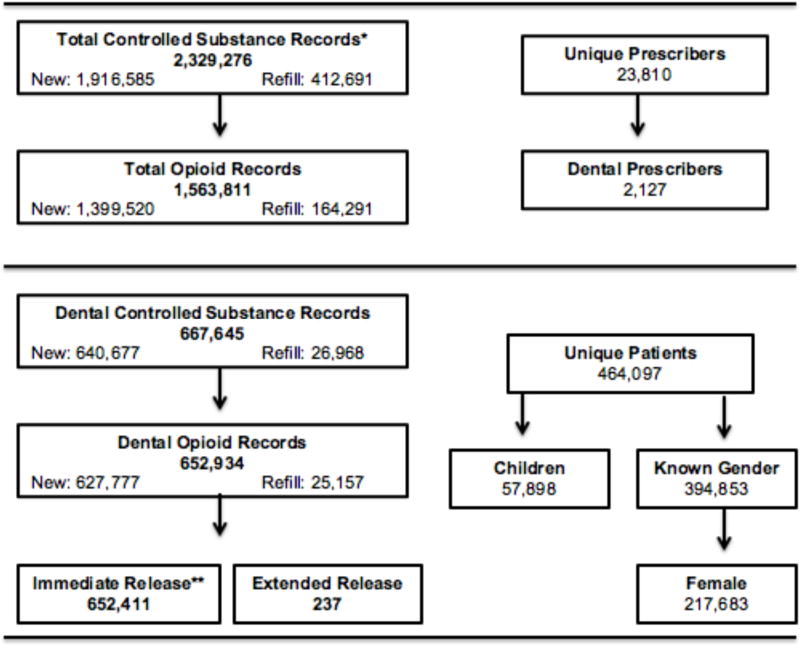
Dentists represented a minority of unique prescribers (8.9%), yet prescribed a substantial proportion (44.9%) of initial fill opioids dispensed to their patients (see Figure 1). The vast majority (97.8%) of controlled substances prescribed by dentists were opioid analgesics, and of these dentist prescribed opioids, nearly all were for immediate release formulations (99.9%; see Table 1). The average number of dispensed opioid prescriptions issued per dentist was 310.3 (SD=565.9; median = 132; mode = 1 [count 71]). The mean number of refills dispended for dentist prescribed opioids was 1.1 (SD=0.3). Children (individuals under the age of 21 years old at the time of opioid dispensation) accounted for 12.5% of all patients receiving dispensed opioids from dental prescriptions and 11.2% (n=73,401) of the total volume of dentist prescribed opioids dispensed.
Figure 1.
Opioid prescribing volumes, provider type, and patient characteristics of the delivered PDMP dataset (2012–2013). Footnote: * A total of 4,155 records (0.18%) were excluded from analysis due to missing at least one field of critical data. ** A total of 286 dental opioid prescriptions did not have a formulation (immediate or extended) indicated. 165x140mm (72 x 72 DPI)
Table 1.
Top five dentist prescribed opioid analgesic prescriptions filled most frequently in South Carolina between January 1, 2012 and December 31, 2013.
| Opioid Type | Total Prescriptions | % Opioids Prescribed* |
|---|---|---|
| Hydrocodone/Acetaminophen# | 497,547 | 76.1% |
| Oxycodone/Acetaminophen# | 79,682 | 12.2% |
| Codeine/Acetaminophen# | 44,333 | 6.8% |
| Hydrocodone/Ibuprofen# | 19,795 | 3.0% |
| Meperidine (Demerol) # | 7,772 | 1.2% |
Percentages do not sum to 100% as opioids listed only represent the top five opioid types most frequently prescribed by South Carolina dentists.
Immediate release formulation
Patients with Multiple Pre-Existing Dispensed Opioid Prescriptions
Table 2 presents data regarding the frequency with which dentists prescribed an opioid analgesic to patients who had additional opioid prescriptions (from any provider) dispensed within the previous 30-days, 90-days, and 180-days. In the majority of dental prescribing incidents, patients had no concurrently dispensed opioids within the prior 30-day, 90-day, and 180-day timeframe. However, patients had at least one pre-existing opioid prescription dispensed within the past 30-days in 136,141 incidents (20.9%) of dental opioid prescribing. Patients had at least one pre-existing opioid prescription dispensed within the past 90-days in 187,855 incidents (28.8%) of dental opioid prescribing. Patients had at least one pre-existing opioid prescription dispensed within the past 180-days in 226,258 incidents (34.7%) of dental opioid prescribing. Of concern, on 324 occasions dentists prescribed an opioid to a patient who had 10 or more opioid analgesic prescriptions dispensed within the 30-days prior to their encounter with the dentist.
Table 2.
Frequencies of pre-existing multiple concurrent opioid prescription volumes at the time of dental opioid prescribing incidents.
| No. Prior Opioid Prescriptions | No. Of Incidents | % Of Incidents Involving Female Patients* | % Of Incidents Involving Children (<21)** | No. Of Patients Represented | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30d | 90d | 180d | 30d | 90d | 180d | 30d | 90d | 180d | 30d | 90d | 180d | |
| 0 | 491,636 | 439,922 | 401,519 | 54.5 | 53.9 | 53.5 | 12.5 | 13.3 | 14.0 | 424,203 | 401,142 | 380,131 |
| 1 | 94,414 | 105,634 | 113,934 | 56.9 | 56.5 | 56.1 | 7.6 | 8.1 | 8.6 | 81,410 | 96,360 | 106,763 |
| 2 | 25,875 | 36,067 | 42,918 | 59.4 | 58.8 | 58.2 | 4.9 | 5.5 | 6.0 | 20,906 | 31,996 | 39,483 |
| 3 | 8,861 | 17,793 | 20,477 | 61.7 | 60.1 | 59.5 | 3.5 | 3.5 | 4.0 | 6,800 | 15,335 | 18,578 |
| 4 | 3,636 | 9,873 | 12,209 | 62.5 | 61.9 | 61.4 | 2.9 | 2.9 | 3.3 | 2,588 | 8,263 | 10,943 |
| 5 | 1,565 | 5,746 | 8,343 | 67.2 | 64.9 | 61.7 | 3.5 | 2.5 | 2.7 | 1,096 | 4,722 | 7,384 |
| 6 | 784 | 4,134 | 6,620 | 69.5 | 64.0 | 62.3 | 2.2 | 1.9 | 2.2 | 487 | 3,361 | 5,819 |
| 7 | 373 | 2,594 | 4,740 | 69.0 | 64.6 | 62.9 | 2.7 | 2.1 | 1.9 | 236 | 2,036 | 4,126 |
| 8 | 183 | 1,681 | 3,556 | 67.7 | 65.5 | 64.1 | 2.2 | 2.1 | 1.7 | 119 | 1,289 | 2,994 |
| 9 | 126 | 1,179 | 2,567 | 67.9 | 67.8 | 63.8 | 0.8 | 1.6 | 1.8 | 70 | 900 | 2,172 |
| 10 | 112 | 770 | 2,045 | 60.4 | 65.7 | 64.7 | 0 | 1.7 | 1.7 | 48 | 579 | 1,721 |
| 11 | 51 | 551 | 1,578 | 47.6 | 67.5 | 64.5 | 0 | 1.8 | 1.5 | 23 | 386 | 1,313 |
| 12 | 34 | 418 | 1,443 | 33.3 | 68.5 | 64.9 | 0 | 2.6 | 1.3 | 16 | 302 | 1,204 |
| 13 | 19 | 307 | 1,118 | 29.4 | 64.7 | 64.5 | 0 | 1.6 | 1.2 | 6 | 207 | 915 |
| 14 | 16 | 221 | 907 | 50.0 | 64.8 | 67.6 | 0 | 0.9 | 1.1 | 4 | 151 | 729 |
| 15 | 10 | 170 | 685 | 50.0 | 74.5 | 67.3 | 0 | 0.6 | 1.6 | 4 | 103 | 553 |
| >15 | 82 | 717 | 3,118 | 66.2 | 60.7 | 66.8 | 0 | 0 | 0.8 | 5 | 134 | 879 |
| Total >0 | 136,141 | 187,855 | 226,258 | 113,818 | 166,124 | 205,576 | ||||||
Female patients accounted for 55.1% of total patients with known gender in the full sample.
Children under 21 years of age accounted for 12.5% of total patients in the full sample.
Table 2 also presents data regarding the percent of incidents in which a dentist prescribed an opioid to a patient with pre-existing dispensed opioid prescriptions that involved female patients (Percent Incidents Involving Female Patients) and that involved children under 21 years of age (Percent of Incidents Involving Children < 21). A total of 8,905 incidents of dental opioid prescribing involved a child with at least one pre-existing opioid dispensed in the past 30-days. A total of 11,821 incidents of dental opioid prescribing involved a child with at least one pre-existing opioid dispensed in the past 90-days. A total of 14,253 incidents of dental opioid prescribing involved a child with at least one pre-existing opioid dispensed in the past 180-days. Finally, unique patients represented by these multiple concurrent opioid prescribing incidents are presented. Of note, some patients experienced more than one occurrence of multiple concurrent opioid prescribing during the two-year span of data collected.
Discussion
Results of the current study indicate that between January 1, 2012 and December 31, 2013, South Carolina dentists prescribed an average of more than 150 opioid prescriptions per year, per dentist. Consistent with self-reported prescribing practices (18), the vast majority of dental opioid prescriptions dispensed in the current study were for immediate release opioids. Hydrocodone and oxycodone combination products accounted for 76% and 12% of dental opioid prescriptions, respectively. Best practice recommendations, as well as preclinical and clinical research, support nonsteroidal anti-inflammatory drugs (NSAIDs) as the first-choice analgesic in the vast majority of postoperative dental situations. (14,29) Optimal doses of NSAIDs have demonstrated pain management outcomes superior to single-entity opioids, and at least as effective as optimal doses of peripheral/opioid combination drugs. (14) Further, pharmacogenetics data suggest that opioids including hydrocodone, oxycodone, and codeine may be ineffective in up to 10% of the Caucasian population. (30,31,32) As a result, best practice recommendations note that opioid analgesics should be reserved for the minority of situations in which optimal doses of NSAIDs and/or acetaminophen/aspirin provide insufficient pain management. (14,29)
The majority of dental patients in the current study did not have recent additional opioid prescriptions at the time their dentist prescribed an opioid. These patients likely represented low to no risk for opioid misuse and/or diversion. However, it was remarkably common for dental patients to have received additional opioid prescriptions from other physicians. Non-dental providers accounted for more than half of all opioids dispensed to dental patients over the two-year period. In fact, in one-fifth (20.9%) of all dental opioid prescribing incidents, dentists prescribed an opioid analgesic to a patient having at least one prior opioid dispensed within the previous 30-days. Dentists prescribed opioids to patients with pre-existing opioids dispensed within the past 90-days and 180-days in 28.8% and 34.7% of all dental opioid prescription incidents, respectively.
In each of these instances, information regarding the presence of concurrent opioid prescriptions was available to the prescribing dentist via PDMP query. When a PDMP query reveals pre-existing, concurrent opioid prescriptions, coordination of care with other prescribers is warranted to determine whether the patient is at-risk for misuse, diversion, or unintentional overdose. For example, individuals undergoing chronic opioid therapy or medication-assisted treatment for opioid addiction (e.g., methadone, buprenorphine) often have existing treatment agreements (or contracts) with their primary prescriber that prohibits receipt of opioid prescriptions from other sources. (29,33) In addition, dentists should also attend to patients’ daily morphine milligram equivalent dose (MMEs) resulting from concomitant opioid prescriptions. Increasing evidence suggests regimens involving greater than 100 MMEs, as well as concurrent use/access to benzodiazepines, confer increased risk for overdose. (11,34–36)
Although no gold standard exists for identifying ‘doctor shoppers’ or diverters, dentists should be cautious in prescribing to patients with a history of: overlapping opioid prescriptions from multiple unique providers, use of multiple pharmacies for dispensing of their prescriptions, and pre-existing combined daily opioid dosages in excess of potential therapeutic value. When present, these conditions should raise caution and trigger further evaluation of the patient. (36–38) Use of opioids for management of acute post-operative dental pain should be avoided if possible in all of the aforementioned situations. In the rare circumstance that all non-opioid options for pain management have been exhausted, immediate release opioids should be prescribed only for the anticipated duration of moderate-to-severe pain, and dentists should take extra precaution to educate the patient regarding the risks and relative benefits. (29)
Children under the age of 21 received 11% of dentist prescribed opioids dispensed, though they accounted for less than 1% of incidents in which dentists prescribed to a patient with pre-existing opioid prescriptions. Patients, particularly adolescents, are often unaware of what behaviors constitute opioid misuse and the risks associated with these behaviors. (39) Therefore, once the decision to prescribe an opioid has been made, dentists should consistently provide patients with standardized education regarding the importance of using the medication only as prescribed, potential consequences of sharing their medication, and how to securely store and dispose of any unused medication. Patient education is particularly important for adolescent patients and their families due to the heightened risk for onset of opioid misuse among this demographic. (40,41)
The current study had limitations worth noting. The delivered dataset only reflected dispensed prescriptions and may not have captured opioids prescribed by dentists that were not dispensed by a South Carolina pharmacy. As noted, 4,155 prescription records were excluded due to missing data; however, missing data accounted for a small proportion of all prescription records (0.2%) and did not substantially impact findings. Multiple prescriptions written by the same provider for the same medication were not identified as refills; only subsequent fills of a pre-existing prescription were coded as refills in the current dataset. Therefore, the current study cannot definitively disentangle multiple prescription episodes from scenarios in which the patient was extending an existing prescription. This study was limited to the de-identified information standardly collected by the PDMP. Patient age at time of dispensing was calculated by subtracting “Year of Birth” from “Year Dispensed” and therefore conservatively estimates the number of children represented. Information regarding specific procedures and/or diagnoses eliciting opioid prescriptions was not available. Given the finite start and end points of the dataset timeframe, counts of multiple pre-existing opioid prescriptions were likely underestimated for individuals receiving their first (or final) dental opioid prescription inside the selected 30-day, 90-day, and 180-day timeframes. Finally, data represent prescriptions dispensed in 2012 and 2013 and do not necessarily reflect current dental prescribing. Although the delayed release and analysis of administrative monitoring data is a common concern (28, 38,42,43), one major policy change is not reflected in the results of this study. In October 2014, the DEA, recognizing the high abuse potential of hydrocodone, rescheduled this product to schedule II of the Controlled Substances Act. (44, 45) Data from the current study cannot speak to potential changes in dental opioid prescribing as a result of this policy change.
Conclusions
Consistent with best practice recommendations, opioids should be reserved for only a minority of cases of moderate to severe postoperative pain in which all other management options have been exhausted. Additionally, the increased regulation of hydrocodone products means that these prescriptions can no longer be phoned into the pharmacy, which may viewed as a deterrent to prescribing these medications as frequently. In these rare instances, query of a PDMP by a dentist is a useful tool in helping the dentist identify patients who may be at increased risk for opioid abuse, misuse, or addiction as demonstrated by the patients’ record and pattern of filling previous opioid prescriptions. All states - except Missouri - currently have operational PDMPs in place. As of July 2015, a PDMP use was mandatory for prescribers in 26 states (see www.pdmpassist.org). Although initial evidence suggests that mandatory use policies decrease dental opioid prescribing, in the absence of mandated use, rates of registration and use of PDMP are strikingly low among dentists. (22, 46) The proactive use of a PDMP offers a clinical care coordination tool and affords dentists the opportunity to identify patients with pre-existing, recently dispensed opioids and engage these patients in clinically oriented discussions regarding the pros and cons of their acute post-operative dental pain management options. For practitioners interested in learning more about their state’s PDMP, information may be found in Table 3.
Table 3.
PDMP website links for each U.S. state with a program operable as of October 2015.
Acknowledgments
This research was supported by the National Institute on Drug Abuse grants K12-DA031794 and K23-DA036566 and by the South Carolina Clinical & Translation Research (SCTR) Institute, with an academic home at the Medical University of South Carolina, through NIH Grant Number UL1-TR000062.
Footnotes
Disclosure. None of the authors reported any disclosures.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Manchikanti L, Helm S, 2nd, Fellows B, et al. Opioid epidemic in the United States. Pain Physician. 2012;15:ES9–38. [PubMed] [Google Scholar]
- 2.Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockille, Md: Substance Abuse and Mental Health Services Administration; 2014. NSDUH Series H-48, HHS Publicaiton No. (SMA) 14–4863. [Google Scholar]
- 3.Volkow ND, McLellan TA. Curtailing diversion and abuse of opioid analgesics without jeopardizing pain treatment. JAMA. 2011;305:1346–1347. doi: 10.1001/jama.2011.369. [DOI] [PubMed] [Google Scholar]
- 4.Inciardi JA, Surratt HL, Cicero TJ, et al. The “black box” of prescription drug diversion. J Addict Dis. 2009;28:332–347. doi: 10.1080/10550880903182986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reinke T. Providers need to boost efforts to prevent abuse of narcotics. Manag Care. 2014;23(4):11–12. [PubMed] [Google Scholar]
- 6.Shei A, Rice JB, Kirson NY, et al. Sources of prescription opioids among diagnosed opioid abusers. Curr Med Res Opin. 2015;31:779–784. doi: 10.1185/03007995.2015.1016607. [DOI] [PubMed] [Google Scholar]
- 7.Voepel-Lewis T, Wagner D, Tait AR. Leftover prescription opioids after minor procedures: an unwitting source for accidental overdose in children. JAMA Pediatr. 2015;169:497–498. doi: 10.1001/jamapediatrics.2014.3583. [DOI] [PubMed] [Google Scholar]
- 8.McCabe SE, West BT, Boyd CJ. Leftover prescription opioids and nonmedical use among high school seniors: a multi-cohort national study. J Adolesc Health. 2013;52:480–485. doi: 10.1016/j.jadohealth.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305:1315–1321. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 10.Meyer R, Patel AM, Rattana SK, et al. Prescription opioid abuse: A literature review of the clinical and economic burden in the United States. Popul Health Manag. 2014;17(6):372–387. doi: 10.1089/pop.2013.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yokell MA, Delgado MK, Zaller ND, et al. Presentation of prescription and nonprescription opioid overdoses to US emergency departments. JAMA Intern Med. 2014;174(12):2034–2037. doi: 10.1001/jamainternmed.2014.5413. [DOI] [PubMed] [Google Scholar]
- 12.Hasegawa K, Espinola JA, Brown DF, et al. Trends in U.S. emergency department visits for opioid overdose, 1993–2010. Pain Med. 2014;15:1765–1770. doi: 10.1111/pme.12461. [DOI] [PubMed] [Google Scholar]
- 13.Imtiaz S, Shield KD, Fischer B, et al. Harms of prescription opioid use in the United States. Subst Abuse Treat Prev Policy. 2014;9:43. doi: 10.1186/1747-597X-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hersh EV, Kane WT, O'Neil MG, et al. Prescribing recommendations for the treatment of acute pain in dentistry. Compend Contin Educ Dent Suppl. 2011;32:22, 24–30. [PubMed] [Google Scholar]
- 15.Moore PA, Hersh EV. Combining ibuprofen and acetaminophen for acute pain management after third-molar extractions: translating clinical research to dental practice. JADA. 2013;144:898–908. doi: 10.14219/jada.archive.2013.0207. [DOI] [PubMed] [Google Scholar]
- 16.Denisco RC, Kenna GA, O'Neil MG, et al. Prevention of prescription opioid abuse: the role of the dentist. JADA. 2011;142:800–810. doi: 10.14219/jada.archive.2011.0268. [DOI] [PubMed] [Google Scholar]
- 17.Oakley M, O'Donnell J, Moore PA, et al. The rise in prescription drug abuse: raising awareness in the dental community. Compend Contin Educ Dent Suppl. 2011;32:14–16. 18–22. [PubMed] [Google Scholar]
- 18.Moore PA, Nahouraii HS, Zovko JG, et al. Dental therapeutic practice patterns in the U.S. part II: Analgesics, cortico-steroids, and anitbiotics. Gen Dent. 2006;54:201–207. [PubMed] [Google Scholar]
- 19.Ashrafioun L, Edwards PC, Bohnert AS, et al. Nonmedical use of pain medications in dental patients. Am J Drug Alcohol Abuse. 2014;40:312–316. doi: 10.3109/00952990.2014.930152. [DOI] [PubMed] [Google Scholar]
- 20.Haegerich TM, Paulozzi LJ, Manns BJ, et al. What we know, and don't know, about the impact of state policy and systems-level interventions on prescription drug overdose. Drug Alcohol Depend. 2014;145:34–47. doi: 10.1016/j.drugalcdep.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nuckols TK, Anderson L, Popescu I, et al. Opioid prescribing: a systematic review and critical appraisal of guidelines for chronic pain. Ann Intern Med. 2014;160:38–47. doi: 10.7326/0003-4819-160-1-201401070-00732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deyo RA, Irvine JM, Hallvik SE, et al. Leading a horse to water: Facilitating registration and use of a prescription drug monitoring program. Clin J Pain. 2014 doi: 10.1097/AJP.0000000000000180. e-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herman C. The Minnesota prescription monitoring program. Northwest Dent. 2011;90:33–35. [PubMed] [Google Scholar]
- 24.Hansen M. Using prescription drug monitoring programs to address drug abuse. NCSL Legisbrief. 2015;23(12):1–2. [PubMed] [Google Scholar]
- 25.Green TC, Mann MR, Bowman SE, et al. How does use of a prescription monitoring program change pharmacy practice? J Am Pharm Assoc. 2013;53:273–281. doi: 10.1331/JAPhA.2013.12094. [DOI] [PubMed] [Google Scholar]
- 26.Jena AB, Goldman D, Weaver L, et al. Opioid prescribing by multiple providers in Medicare: retrospective observational study of insurance claims. BMJ. 2014;348:g1393. doi: 10.1136/bmj.g1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paulozzi LJ. Prescription drug overdoses: a review. J Safety Res. 2012;43:283–289. doi: 10.1016/j.jsr.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 28.Dart RC, Surratt HL, Cicero TJ, et al. Trends in opioid analgesic abuse and mortality in the United States. NEJM. 2015;372:241–248. doi: 10.1056/NEJMsa1406143. [DOI] [PubMed] [Google Scholar]
- 29.Becker DE. Pain management: Part 1: Managing acute and postoperative dental pain. Anseth Prog. 2010;57:67–79. doi: 10.2344/0003-3006-57.2.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Linares OA, Daly D, Linares AD, et al. Personalized oxycodone dosing: using pharmacogenetic testing and clinical pharmacokinetics to reduce toxicity risk and increase effectiveness. Pain Med. 2014;15(5):791–806. doi: 10.1111/pme.12380. [DOI] [PubMed] [Google Scholar]
- 31.Crews KR, Gaedigk A, Dunnenberger HM, et al. Clinical Pharmacogenetics Implementation Consortium. Clinical Pharmacogenetics Implementation Consortium guidelines for cytochrome P450 2D6 genotype and codeine therapy: 2014 update. Clin Pharmacol Ther. 2014;95(4):376–82. doi: 10.1038/clpt.2013.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Linares OA, Fudin J, Daly-Linares A, et al. Individualized Hydrocodone Therapy Based on Phenotype, Pharmacogenetics, and Pharmacokinetic Dosing. Clin J Pain. 2015 doi: 10.1097/AJP.0000000000000214. e-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 33.Chou R, Fanciullo GJ, Fine PG, et al. Opioid treatment guidelines: clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10:113–130. doi: 10.1016/j.jpain.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hirsch A, Proescholdbell SK, Bronson W, et al. Prescription histories and dose strengths associated with overdose deaths. Pain Med. 2014;15(7):1187–95. doi: 10.1111/pme.12391. [DOI] [PubMed] [Google Scholar]
- 35.Baumblatt AG, Wiedman C, Dunn JR, et al. High risk use by patients prescribed opioids for pain and its role in overdose deaths. JAMA Inern Med. 2014;174:796–801. doi: 10.1001/jamainternmed.2013.12711. [DOI] [PubMed] [Google Scholar]
- 36.Ringwalt C, Schiro S, Shanahan M, et al. The use of a prescription drug monitoring program to develop algorithms to identify providers with unusual prescribing practices for controlled substances. J Primary Prevent. 2015;36(5):287–299. doi: 10.1007/s10935-015-0397-0. [DOI] [PubMed] [Google Scholar]
- 37.McDonald DC, Carlson KE. Estimating the prevalence of opioid diversion by “doctor shoppers” in the United States. PLoS One. 2013;8:e69241. doi: 10.1371/journal.pone.0069241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liang Y, Turner BJ. Assessing risk for drug overdose in a national cohort: role for both daily and total opioid dose? J Pain. 2015;16:318–325. doi: 10.1016/j.jpain.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McCauley JL, Back SE, Brady KT. Pilot of a brief, web-based educational intervention targeting safe storage and disposal of prescription opioids. Addict Behav. 2013;38:2230–2235. doi: 10.1016/j.addbeh.2013.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCabe SE, Schulenberg JE, O'Malley PM, et al. Non-medical use of prescription opioids during the transition to adulthood: a multi-cohort national longitudinal study. Addiction. 2014;109:102–110. doi: 10.1111/add.12347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Murphy SM, Friesner DL, Rosenman R. Opioid misuse among adolescents: new evidence from a misclassification analysis. Appl Health Econ Health Policy. 2015;13:181–192. doi: 10.1007/s40258-015-0151-z. [DOI] [PubMed] [Google Scholar]
- 42.Yang Z, Wilsey B, Bohm M, et al. Defining risk for prescription opioid overdose: pharmacy shopping and overlapping prescriptions among long-term opioid users in Medicaid. J Pain. 2015;16(5):445–453. doi: 10.1016/j.jpain.2015.01.475. [DOI] [PubMed] [Google Scholar]
- 43.Mack KA, Zhang K, Paulozzi L, et al. Prescription practices involving opioid analgesics among Americans with Medicaid, 2010. J Health Care Poor Underserved. 2015;26:182–198. doi: 10.1353/hpu.2015.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cicero TJ, Ellis MS, Surratt HL, et al. Factors influencing the selection of hydrocodone and oxycodone as primary opioids in substance abusers seeking treatment in the United States. Pain. 2013;154:2639–2648. doi: 10.1016/j.pain.2013.07.025. [DOI] [PubMed] [Google Scholar]
- 45.Hydrocodone Combination Products Fact Sheet. Springfield, VA: Drug Enforcement Agency, U.S. Department of Justice; 2014. Drug Fact Sheet Series. [Google Scholar]
- 46.Rasubala L, Pernapati L, Velasquez X, et al. Impact of a mandatory prescription drug monitoring program on prescription of opioid analgesics by dentists. PLoS One. 2015;10:e0135957. doi: 10.1371/journal.pone.0135957. [DOI] [PMC free article] [PubMed] [Google Scholar]