Abstract
106 cases of intracranial tumours were evaluated, out of which 42 cases (39.6%) were histologically confirmed as gliomas. Computerised tomography (CT) imaging characteristics of glioma were studied with respect to morphology and contrast enhancement to find a possible correlation between CT appearance and the grade of malignancy. It was found that there is a range of patterns both before and after intravenous contrast, which allows an assessment of grading of the tumour with a fair degree of reliability.
Key Words: Gliomas, Intracranial tumours
Introduction
Primary cerebral gliomas are the largest single group (40-45%) of all intracranial tumours [1]. They are derived from glial cells which are of three basic types : astrocytic, ependymal, and oligodendrocytic. In addition epithelial lining of choroid plexus which is derived from the ependyma may be considered a fourth type of glial cell. Among these, astrocytic neoplasms are the commonest.
Gliomas can occur at any site in both children and adults, but gliomas of the optic chiasma and the brainstem are particularly common in children, where they have a peak incidence at one to six years and one to four years of age respectively. Cerebellar astrocytoma is also common in children, with a peak incidence at five to ten years. In adults, the age group commonly affected is 30-65 years and supratentorial gliomas outnumber posterior fossa gliomas by a ratio of 7:3 [2]. CT plays an important role in the diagnosis of these tumours and differentiating them from other intracranial space occupying lesions. CT remains the initial modality of choice for assessment of intracranial space occupying lesions. The aim of this study was to find a possible correlation between CT appearances and the grade of malignancy of gliomas.
Material and Methods
Patients attending (he service hospital, suspected of having intracranial space occupying lesions clinically were subjected to both plain and contrast CT. Each case was examined in detail with particular reference to history and symptoms followed by plain and contrast CT of head which were analysed systematically for : a) normal anatomical landmarks, b) size and shape of ventricular system, c) pre-contrast morphology of the lesion with reference to site, size, number, satellite lesions, density, mass effect, surrounding edema and intratumoral calcifications, d) postcontrast morphology and pattern of enhancement and e) associated bony changes.
Results
Out of 106 cases of intracranial tumours studied, 42 cases (39.6%) were histologically confirmed to be gliomas. 34 (32%) cases were other primary tumours and 30 (28.3%) cases were metastatic tumours (Fig 1). Peak incidence of 33.3% cases was found in 31-40 years age group. Second peak (23.8%) was found in 51-60 years age group (Table-1). The commonest histological type was low grade astrocytoma in 31% cases, followed by glioblastoma multiforme in 28.6% cases (Table-1). Majority (81%) of the lesions were hypodense (Table-2). 42.8% of cases showed rim enhancement, 26.2% of cases revealed no enhancement following contrast administration (Table-3). Intratumoral calcification was found in 16.6% of cases (Table-4). Majority of cases (81%) showed perilesional edema and 19% of cases had no surrounding edema (Table 5). 88% of cases were associated with evidence of mass effect and 12% of cases had no obvious mass effect (Table-6).
Fig. 1.
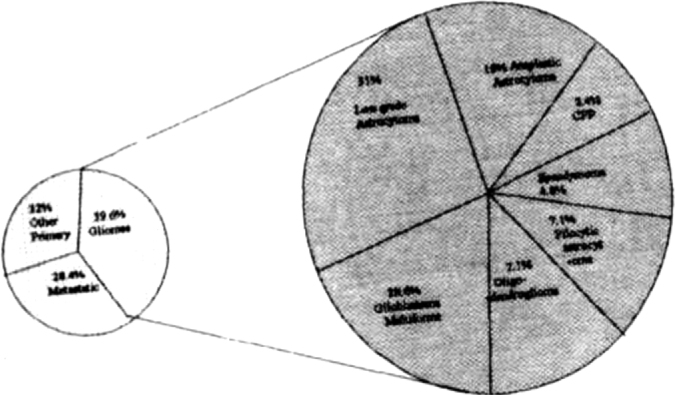
Incidence of intracranial tumours
TABLE 1.
Age and grade wise Incidence
| Age (in years) | Pilocytic astrocytoma | Low grade astrocytoma | Anaplastic-astrocytoma | Glioblastoma multiforme | Oligodendroglioma | Ependymoma | Choroid plexus papilloma | Total (% in parenthesis) |
|---|---|---|---|---|---|---|---|---|
| 0-10 | 02 | 00 | 00 | 00 | 00 | 01 | 01 | 04 (9.53) |
| 11-20 | 01 | 00 | 00 | 00 | 00 | 01 | 00 | 02 (4.77) |
| 21-30 | 00 | 02 | 01 | 01 | 00 | 00 | 00 | 04 (9.53) |
| 31-40 | 00 | 08 | 03 | 02 | 01 | 00 | 00 | 14 (33.3) |
| 41-50 | 00 | 00 | 02 | 02 | 01 | 00 | 00 | 05 (11.9) |
| 51-60 | 00 | 02 | 02 | 05 | 01 | 00 | 00 | 10 (23.8) |
| 61-70 | 00 | 01 | 00 | 02 | 00 | 00 | 00 | 03 (7.14) |
| Total | 03 | 13 | 08 | 12 | 03 | 02 | 01 | 42 |
| % | 7.1 | 31 | 19 | 28.6 | 7.1 | 4.8 | 2.4 | 100 |
TABLE 2.
CT densities of intracranial gliomas
| Type | Decreased | Increased | Isodense |
|---|---|---|---|
| Grade I gliomas | 03 | 00 | 00 |
| Grade It astrocytoma | 11 | 02 | 00 |
| Grade III anaplastic astrocytoma | 07 | 01 | 00 |
| Grade IV glioblastoma multiforme | 10 | 02 | 00 |
| Oligodendroglioma | 03 | 00 | 00 |
| Ependyrnoma | 00 | 01 | 01 |
| Choroid plexus papilloma | 00 | 01 | 00 |
| Total | 34 | 07 | 01 |
TABLE 3.
Contrast enhancement
| Type | Rim enhancement | Non homogeneous | Homogeneous | None |
|---|---|---|---|---|
| Grade I gliomas | 02 | 00 | 00 | 01 |
| Grade II astrocytoma | 01 | 03 | 00 | 09 |
| Grade III anaplastic astrocytoma | 02 | 04 | 01 | 01 |
| Grade IV | 10 | 02 | 00 | 00 |
| glioblastoma multiforme Oligodendroglioma | 03 | 00 | 00 | 00 |
| Ependymoma | 00 | 01 | 01 | 00 |
| Choroid plexus papilloma | 00 | 00 | 01 | 00 |
| Total | 18 | 10 | 03 | 11 |
TABLE 4.
Intratumoral calcification
| Type | Present | Absent |
|---|---|---|
| Grade I gliomas | 00 | 03 |
| Grade II astrocytoma | 02 | 11 |
| Grade III anaplastic astrocytoma | 01 | 07 |
| Grade IV glioblastoma multiforme | 00 | 12 |
| Oligodendroglioma | 03 | 00 |
| Ependymoma | 01 | 01 |
| Choroid plexus papilloma | 00 | 01 |
| Total | 07 | 35 |
TABLE 5.
Vasogenic edema
| Type | Mild | Moderate | Marked | None |
|---|---|---|---|---|
| Grade I gliomas | 03 | 00 | 00 | 00 |
| Grade II astrocytoma | 05 | 01 | 00 | 07 |
| Grade III anaplastic astrocytoma | 02 | 05 | 01 | 00 |
| Grade IV glioblastoma multiforme | 20 | 4 | 06 | 00 |
| Oligodendroglioma | 02 | 01 | 00 | 00 |
| Ependymoma | 02 | 00 | 00 | 00 |
| Choroid plexus papilloma | 00 | 00 | 00 | 01 |
| Total | 16 | 11 | 07 | 08 |
| % | 38.1 | 26.2 | 16.7 | 19.0 |
TABLE 6.
Mass effect
| Type | Marked | Moderate | Slight | None |
|---|---|---|---|---|
| Grade 1 gliomas | 00 | 01 | 02 | 00 |
| Grade II astrocytoma | 00 | 01 | 07 | 05 |
| Grade III anaplastic astrocytoma | 02 | 04 | 02 | 00 |
| Grade IV glioblastoma multiforme | 07 | 05 | 00 | 00 |
| Oligodendroglioma | 00 | 01 | 02 | 00 |
| Ependymoma | 00 | 01 | 01 | 00 |
| Choroid plexus papilloma | 00 | 01 | 00 | 00 |
| Total | 09 | 14 | 14 | 05 |
| % | 21.4 | 33.3 | 33.3 | 12 |
Discussion
Incidence of gliomas in this study was 39.6% whereas Russell [1] found the incidence of cerebral gliomas to be 40-45%. In adults, commonest histological type was low grade astrocytoma (31%) followed by glioblastoma multiforme (28.6%), whereas in children, pilocytic astrocytoma, ependymoma and choroid plexus papilloma were found to be more common (Table-1). According to a study by Rees [3] in 1996, glioblastoma was the commonest tumour in adults. These differences could well be explained by the fact that the service hospitals attend to a clientele which is generally young and the stringent policy of routine medical examination of all service personnel leads to early detection of any disease process.
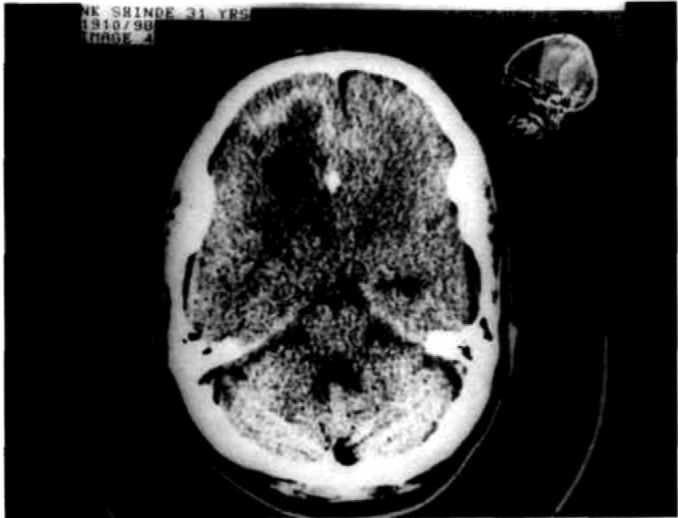
The majority of the gliomas presented as low attenuating lesions with exception of ependymoma and choroid plexus papilloma, and two cases each of grade II and grade IV and one case of grade III astrocytoma which showed increased density either due to haemorrhage or calcification. The well defined, rounded, low density lesion of the pilocytic astrocytoma (Fig-2) was distinctly different in appearance from the poorly defined low density lesion seen in low grade and anaplastic astrocytoma (Fig-3). Though the low density of low grade glioma can be confused with infarct, clinical presentation and careful examination can help in arriving at an accurate diagnosis.
Fig. 2.
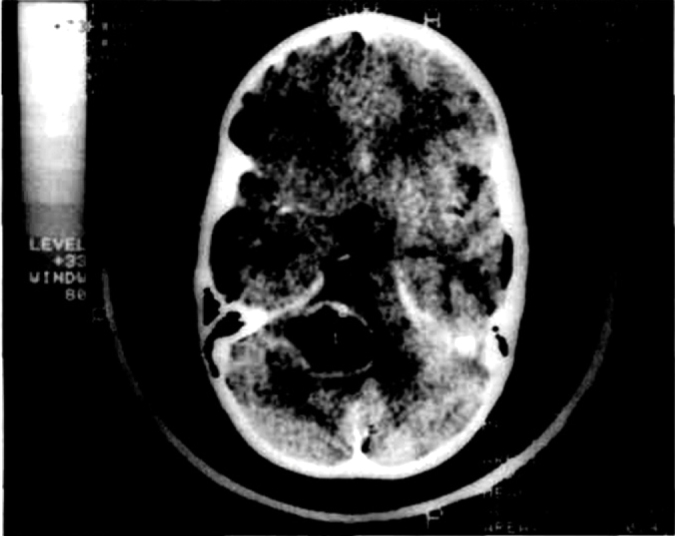
Axial contrast enhanced CT showing well defined low density lesion with rim enhancement in a case of pilocytic
Fig. 3.
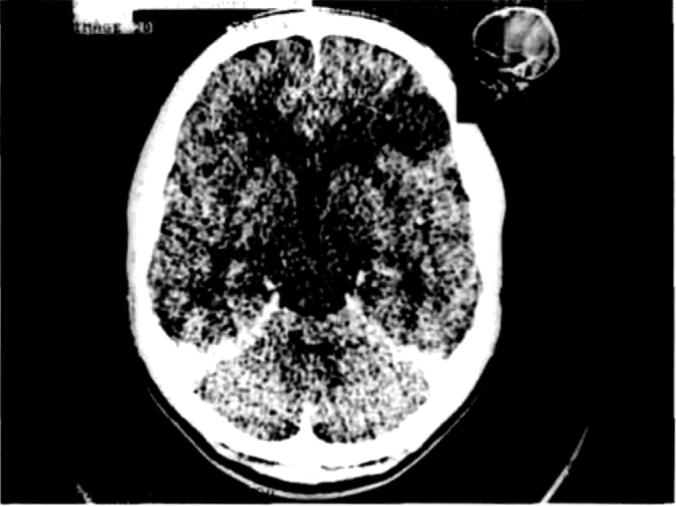
Axial CECT reveals a non enhancing low attenuating area (arrow) in the left frontal lobe with no mass effect in a case of low grade astrocytoma
The enhancement in the neoplasm in CT scan after intravenous contrast administration is thought to be due to increased tumour vascularity and disruption of the blood-brain barrier [4]. Post contrast CT scan is required for better visualisation of the tumour itself and to demarcate it from the surrounding edema. The appearance of the enhancement pattern may be highly characteristic and enable us to predict the grade of malignancy of the glioma with confidence.
Enhancement in a ring like fashion with thick irregular margins surrounding a central area of low density was never present in low grade and anaplastic astrocytoma and is virtually diagnostic of glioblastoma multiforme (Fig-4). Homogenous enhancement of the lesion may occur in any group and is a non-specific finding. The enhanced mural nodule in the wall of a cystic lesion with decreased density [5] is quite suggestive of pilocytic astrocytoma. Complete absence of enhancement may occur in any group, particularly in very cellular and avascular lesions.
Fig. 4.
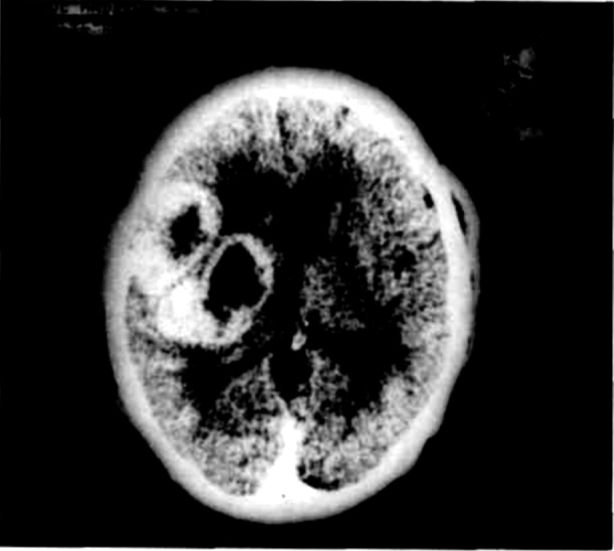
Axial CECT showing thick irregular peripherally enhancing lesion with central necrosis, surrounding edema and mass effect in a case of glioblastoma multiforme
In the present day scenario of aggressive approach for arriving at an early diagnosis, the presence of calcification should always raise the suspicion of oligodendroglioma. All cases of oligodendroglioma in this study showed evidence of intratumoral calcification (Table-4). Vonofakos et al found intratumoral calcification in 90% of cases [6]. The pattern commonly seen in oligodendroglioma was of nodular calcification (Fig-5) which can be mimicked by low grade glioma. The calcification in a lesion arising in the fourth ventricle especially in children should raise the possibility of ependymoma or choroid plexus papilloma. Choroid plexus papilloma occurs primarily within the first two years of age. The lateral and third ventricles are affected more frequently in children under two years (Fig-6), while the fourth ventricle is more often affected in adolescents [7, 8].
Fig. 5.
Axial non contrast CT showing hypodense area in the right frontal lobe with eccentric nodular calcification in oligodendroglioma
Fig. 6a & b.
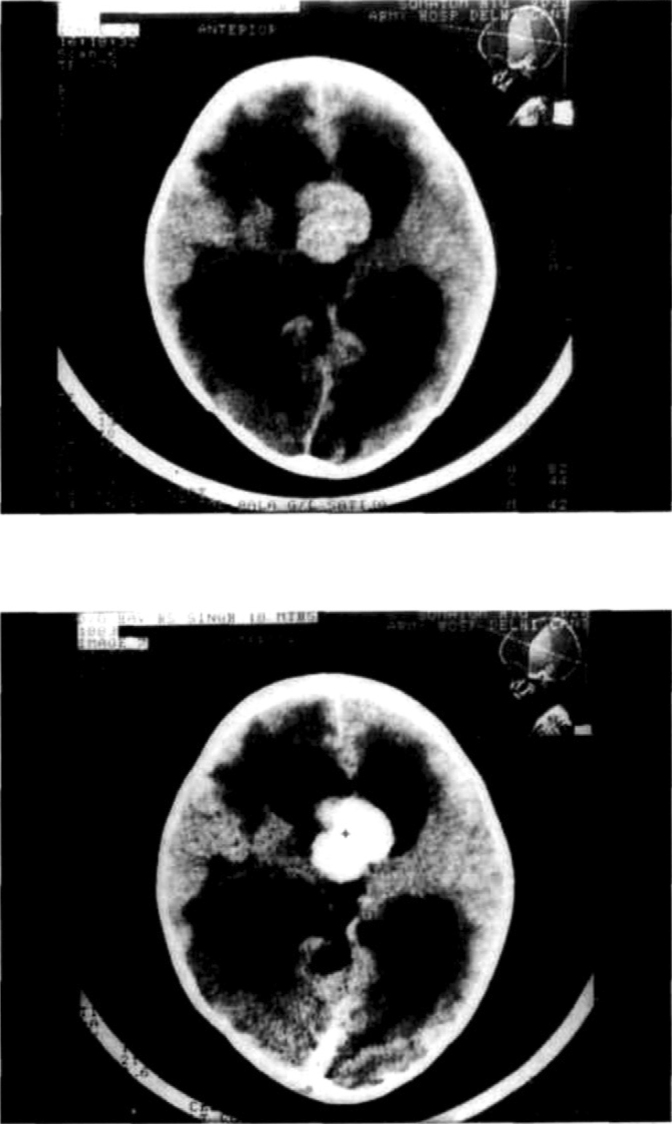
Axial NCCT & CECT in a child reveals a large lobulated densely enhancing mass arising from the roof of the third ventricle with resultant hydrocephalus
Posterior fossa tumours generally caused obstructive hydrocephalus and supratentorial lesions generally resulted in effacement of ipsilateral lateral ventricles with shift of midline structures.
Vasogenic edema was a feature of all the grades of gliomas except the low grade glioma, which can present without any perilesional edema (Table-5) and lead to confusion with infarct (Fig-2). But the useful clinical sign described by Scally [9] in diagnosing low grade glioma can be helpful in arriving at a diagnosis. It consists simply of observing whether the patient moves on to the CT table of his own accord. This indicates the diagnosis of a low grade astrocytoma rather than infarction, cerebritis or oedema of another cause.
Mass effect is produced by all grades except the low grade gliomas, which can sometimes present without any appreciable mass effect (Table-6). Mass effect was commonest and more pronounced in cases of glioblastoma (Fig-3). Oligodendroglioma and low grade astrocytomas had minimal mass effect compared to other grades. Mass effect has no relation with the grade of malignancy as the large cystic astrocytoma can also produce an appreciable mass effect.
In most cases, diagnosis of glioma can be made on the CT imaging in conjunction with the clinical history. Increasing experience and expertise indicates that there is a range of patterns on CT both before and after intravenous enhancement, which allows an assessment of the grading of the tumour with fair degree of reliability. Presently magnetic resonance imaging (MRI) is considered superior to CT in detecting and localizing tumours due to its multiplanar capability and better characterization of lesion in various sequences. But it lags behind CT in detection of calcification, which is of diagnostic importance in the differential diagnosis of brain tumours. In detecting acute intratumoral bleed CT is again considered superior to MRI.
References
- 1.Russell DS, Rubinstein LJ. Pathology of tumours of the nervous system. 4th ed. Edward Arnold; 1977. pp. 150–152. [Google Scholar]
- 2.Sutton D, Kendall B, Stevens J. Intracranial lesions. Sutton's Textbook of Radiology and Imaging. 6th ed. Churchill Livingstone; New York: 1998. pp. 1596–1602. [Google Scholar]
- 3.Rees JH, Smiriniotopoulos JG. Oligodendroglioma, clinical and imaging features in 87 patients. Presented at 34th Annual Meeting of the American Society of Neuroradiology; at Seattle. Washington on June 23; 1996. [Google Scholar]
- 4.Gado MH, Phelps ME, Coleman RE. An extravascular component of contrast enhancement in cranial computed tomography. Radiology. 1975;177:589–593. doi: 10.1148/117.3.589. [DOI] [PubMed] [Google Scholar]; Gado MH, Phelps ME, Coleman RE. An extravascular component of contrast enhancement in cranial computed tomography. Radiology. 1975;177:595–597. doi: 10.1148/117.3.595. [DOI] [PubMed] [Google Scholar]
- 5.Gol A, Mckissack W. The cerebellar astrocytomas. A report on 98 verified cases. J Neurosurg. 1959;16:287–296. doi: 10.3171/jns.1959.16.3.0287. [DOI] [PubMed] [Google Scholar]
- 6.Vonofakos D, Marcu H, Hacker H. Oligodendrogliomas. CT patterns with emphasis on features indicating malignancy. J Comput Assist Tomogr. 1979;3:783–788. [PubMed] [Google Scholar]
- 7.Laurence KM. The biology of choroid plexus papilloma in infancy and childhood. Acta Neurchir (Wien) 1979;50:79–90. doi: 10.1007/BF01813553. [DOI] [PubMed] [Google Scholar]
- 8.Tonami H, Kamehiro M, Oguchi M, Higashi K, Yamamoto I, Njima T. Chordoid glioma of the third ventricle: CT and MR findings. J Comput Assist Tomogr. 2000;24:336–338. doi: 10.1097/00004728-200003000-00029. [DOI] [PubMed] [Google Scholar]
- 9.Scally PM, Close PJ. A clinical sign of low grade astrocytoma. Australas Radiol. 1993;37:128–129. doi: 10.1111/j.1440-1673.1993.tb00034.x. [DOI] [PubMed] [Google Scholar]


