Abstract
Objectives
Suicide is unfortunately common in psychiatric practice, but difficult to predict. This study sought to assess which clinical symptoms increase in the months before suicidal behavior in a sample of psychiatric outpatients with bipolar disorder.
Methods
Data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) trial were used. A total pf 103 participants who attempted suicide or died by suicide during the trial were included; a 15% random sample of the remaining participants (n = 427) was used as a comparison sample. Linear mixed models in the six months before suicidal behavior were conducted for each of five proposed acute risk factors for suicidal behavior. Participants were assessed using the Clinical Monitoring Form (CMF) at each visit for the following potential acute risk factors for suicidal behavior: suicidal ideation, loss of interest, anxiety, psychomotor agitation, and high-risk behavior.
Results
Each of the five symptoms was elevated overall in individuals who engaged in suicidal behavior (p < 0.05). The severity of both suicidal ideation and loss of interest significantly increased in the months before suicidal behavior (p < 0.001). Anxiety demonstrated comparable effect sizes across multiple models. Psychomotor agitation and high-risk behavior were not significantly elevated before suicidal behavior.
Conclusions
Suicidal ideation, loss of interest and, to a lesser extent, anxiety may represent acute suicide risk factors up to four months before suicidal behavior in outpatients with bipolar disorder. Further investigation of these potential acute risk factors in prospective analyses is warranted.
Keywords: anhedonia, anxiety, bipolar disorder, suicidal ideation, suicide
In 2012, over 40,000 Americans died by suicide (1). With over eight million adults thinking about suicide, and one million attempting suicide each year in the United States (2), suicide risk assessment is an essential skill for all mental health clinicians. However, suicidal behavior remains very difficult to predict (3), as it is a low base rate phenomenon that occurs across psychiatric diagnoses, ethnicities, and most age groups (4). Death by suicide is even more difficult to predict, as few studies are sufficiently powered to detect its relatively low base rate (5). Careful suicide assessment is essential for psychiatric diagnoses such as bipolar disorder (BD), which has been associated with particularly high rates of suicidal behavior and death (6–8).
Predicting suicidal behavior often relies on identifying and monitoring both long-term and acute risk factors. Risk assessments include factors that may lead to a suicide death sometime in the patient’s lifetime (long-term) and those variables that signal a more transient, dynamic state indicating near-term risk (acute). In short, when completing a comprehensive risk assessment, a clinician may collect data on a number of factors that indicate elevated lifetime risk; history of suicide attempts is a commonly cited example (9). However, these static variables do not tell the clinician whether the patient in her office will kill himself in the next week to month. Such a distinction has implications for treatment, including psychiatric hospitalizations and watch status.
While research on acute suicide risk factors are critical and a focus of the Suicide Research Prioritization Task Force (10), empirical data on acute risk factors in particular are limited. Techniques that have been used to recreate the time before a suicide attempt or death include follow-back interviews (11) and psychological autopsies (12). Another potential method is examining large naturalistic studies and clinical trials where the suicidal behavior occurs prospectively in the context of clinical assessment. For example, data regarding suicide attempts and deaths over the course of the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) study have been previously reported, and baseline predictors of future suicidal behavior (long-term risk factors) have already been published (13–17). Those studies suggested that lifetime history of suicidal behavior is a significant predictor of future suicidal behavior. In addition to long-term risk factors, the STEP-BD dataset also provides an opportunity to evaluate acute risk factors for suicidal behavior in patients with BD.
This analysis sought to evaluate potential acute risk factors in the six months before a suicide attempt or death in the STEP-BD sample. Acute risk factors in this context are described as symptoms that significantly increased in the months before suicidal behavior, as these variables would be most helpful to clinicians in determining whether a patient is experiencing a suicidal crisis. The time period differs from the framework around suicide warning signs proposed by Rudd and colleagues (18), in which specific symptoms such as increased ideation or giving away belongings are thought to signal imminent suicide risk in the following minutes, hours, or days. It should be noted, however, that more recent critical reviews of the literature have stated that there are little to no data on the specific symptoms or time frames associated with imminent risk of suicidal behavior (19, 20).
Available data in the STEP-BD study included information about overall mood states (depression, mania, or irritability), substance abuse, and headaches/migraine in addition to DSM-IV symptoms of depression and mania. From these options, we were interested in specific symptoms that might signal an acute suicidal crisis (18). Consequently, we concentrated on suicidal thoughts and symptoms such as anxiety/agitation rather than overall mood effects (i.e. whether the patient was in a depressed, manic, or mixed episode), although such analyses of mood were completed post-hoc due to the relationship between BD mood states and suicide attempts (7, 21). In total, the five symptoms included in the analysis were: 1) suicidal thoughts, due to the relationship to later suicide attempts and death (22, 23); 2) loss of interest as a measure of anhedonia, which has been linked to acute suicide risk (24); 3) anxiety, due to its relationship to the transition from suicidal thoughts to suicidal behavior (25); 4) psychomotor agitation, because of its relationship to death by suicide in psychiatric inpatient samples (26); and 5) high-risk behavior, as a proxy for impulsivity or recklessness, both of which have also been associated with suicidal behavior (27).
Patients and methods
Participants
All data were drawn from the STEP-BD study (28), which followed 4,360 patients with BD across 22 academic psychiatry centers over seven years. The prospective study used comparable assessments over the course of both naturalistic treatment and randomized clinical trials. All clinicians were trained and certified in assessment and evidence-based treatments. The study was reviewed and approved by the institutional review board (IRB) of each participating institution.
Suicidal behavior outcome
Over the course of the STEP-BD study, data on prospective suicidal behavior were collected via the serious adverse events report [(SAE) reviewed by an independent safety officer and committee for serious adverse events], which recorded deaths by suicide and suicide attempts, and the Care Utilization form (CU) in which all participants were asked whether they had attempted suicide in the last three months. In the sample of 4,360 patients participating in the STEP-BD study, eight suicide deaths and 44 attempts were reported on SAE forms, and 244 attempts were reported on CU forms. Previous analyses of suicidal behavior in the STEP-BD trial calculated a suicide rate of 0.014 per 100 person years (15). Additional data regarding suicide attempts and deaths in this sample have been reported using similar methods of determining suicidal behavior (13, 15). In the present study, data from the CU and SAE forms were collapsed, as detailed in the Statistical analysis section and in Supplementary Figure S1.
Affective Disorder Evaluation (ADE)
Upon baseline entry into the original STEP-BD study, all patients were assessed using the Affective Disorder Evaluation (ADE) for clinical assessment (28, 29). This assessment evaluated the intensity of suicidal ideation, loss of interest, abnormal anxiety, psychomotor agitation, and high-risk behavior. Each of these symptoms, with the exception of anxiety, was rated on a scale from +2 to −2, with +2/−2 signifying ‘much more’ or ‘much less’ than usual, +1/−1 signifying ‘clearly present and fulfills SCID criteria’, and 0 signifying ‘none or usual’ for the past week. These symptoms were assessed in the same manner on every clinic visit using the Clinical Monitoring Form (CMF). Specifically, suicidal ideation was assessed using the questions: “Were there times when you were feeling so bad that you felt your life was not worth living? What about actually thinking about suicide or harming yourself?”. Loss of interest was assessed using the question: “Have you been able to enjoy pleasant things that happened?”, and then reverse-coded to facilitate comparison to other variables. Psychomotor agitation was assessed using the question: “Were there times you were so fidgety or agitated it was hard for you to stay still?”. High-risk behavior was assessed using the questions: “Did you do anything that was unusual for you or that other people might think was excessive, foolish, or risky? Did you do anything which would have caused a problem if you were caught?”.
Anxiety was assessed differently; patients were asked how many days they had experienced abnormal anxiety over the past two weeks on the ADE and then what percentage of the last 10 days they experienced abnormal anxiety on the Clinical Monitoring Form (CMF) (resulting in a scale from 0 to 100). Data from the ADE were used to analyze baseline data, and results from the CMF were used to analyze symptom trajectories during the study.
Statistical analysis
Patients with suicidal behavior
Data on suicidal behavior were collected from the SAE and CU forms, including the date of suicidal behavior compared to the date of consent (resulting in a days from consent variable). One hundred and eighty-six patients with prospective suicidal behavior were included in baseline univariate analyses.
In order to track clinical symptoms across time and reduce overall missing data, the analysis was limited to patients who had at least two clinic visits, in two different months, before the suicidal behavior. The resulting sample comprised 103 participants (Supplementary Fig. S1 describes this process). This group will hereafter be referred to as the prospective suicidal behavior group.
Comparison sample
For comparison, a 15% random sample was selected from the patients with BD who did not attempt suicide during the study in order to obtain a sample roughly three to four times greater than the sample with prospective suicidal behavior. The full sample was not used in order to avoid problems with heterogeneous variances that can occur with substantial differences in group sample sizes. No attempt was made to match the samples. The random selection procedure from SPSS provided a pseudo-random sample using no replacement in a Mersenne Twister algorithm. Five hundred and sixty-four individuals were selected for this group and all were included in the baseline univariate analysis. In order to assess trajectory of symptoms, the comparison group was limited to the first six months of participation in STEP-BD. These patients were limited to those who had at least two clinic visits in this timeframe, resulting in 427 patients for analysis. This group will be referred to as the no prospective suicidal behavior group.
Univariate analysis
Demographic and baseline characteristics of individuals who did and did not engage in suicidal behavior over the course of the STEP-BD study were evaluated using t-tests and chi-squares. Age, suicide attempt history, and scores on the Personality Disorders Questionnaire (PDQ) (30) were included in these models, as these variables were shown to predict prospective suicide attempts in previous multivariate analyses of the dataset (13). In addition, Spearman correlations were used to evaluate the relationship between the five symptoms of interest in the month before suicidal behavior. Significance was considered at p < 0.05, two-tailed. Supplemental analyses were conducted to compare participants included in linear mixed model analysis and those who did not have at least two clinic visits before exhibiting suicidal behavior.
Time analysis
The six months before suicidal behavior (or the first six months of participation in the comparison sample) was coded in relation to the time of attempt (Month −1 is the latest month and occurred closest to the time of suicidal behavior). If a patient had multiple visits within the same 30-day period, their scores were aggregated using median score. Therefore, each patient had up to six time points recorded for each clinical variable.
Linear mixed models
Separate linear mixed models were run using each clinical symptom as the dependent variable. Suicidal behavior (whether or not the patient engaged in prospective suicidal behavior) was a fixed between-subjects factor, and time (months before suicide attempt) was included as a fixed within-subjects factor. The interaction between time and suicidal behavior was also included in the model, as was a fixed intercept. According to Schwarz’s Bayesian criteria, a compound symmetry covariance structure had the best fit for the data. Models were run with quadratic codings for time, with similar fit for the results; the linear models are thus reported. Missing data were accounted for using restricted maximum likelihood estimation. Due to the five clinical symptoms of interest, all linear mixed models were run using a Bonferroni correction for multiple analyses, p < 0.01, two-tailed. Effect sizes were calculated using Cohen’s d. Due to the use of linear mixed models, all figures include estimated marginal means and standard errors of these mean estimates.
Global functioning and mood effects
Because many other potential suicide risk factors were not included in the initial analysis, supplemental models were run assessing global functioning, mood effects, substance abuse, and headaches in the six months before suicidal behavior to describe general clinical functioning. Clinical functioning was assessed using the Clinical Global Impression (CGI) and Global Assessment of Functioning (GAF) rating scales. Mood effects were measured by items assessing mood elevation and abnormal irritability (which was assessed similarly to abnormal anxiety, on a scale from 0 to 100) as well as depressed mood (which was assessed similarly to the other potential acute risk factors, on a scale from −2 to +2). Substance use, alcohol use, headaches and migraine headaches were assessed using a dichotomous variable. Results across these analyses were compared using effect sizes.
Supplemental analyses
Because of the high rate of missing data in the overall model (36%), secondary analyses were run that collapsed clinical ratings using medians across two-month intervals. Thus, linear mixed models were run across three, instead of six, time points. While this approach did not allow for fine-grain analysis of the month before suicidal behavior, missing data were reduced to 3%. This approach also limited the analysis to patients with visits throughout the six month timeframe (i.e., patients who only had visits in the two months before the suicidal behavior were excluded).
Due to concerns about differences in reporting methods between the SAE report and CU form, the models were also run using only suicidal behavior reported on the SAE form. Models were also run excluding suicide deaths. Similarly, in order to adjust for baseline levels of symptoms, all models were run for the five months before suicidal behavior, adjusting for symptoms reported in the sixth month. In addition, due to the importance of age, history of suicide attempt, and PDQ score noted in previous analyses by Antypa (13), models were run adjusting for these variables.
All statistics were conducted with IBM SPSS 21.
Results
Baseline demographic and clinical characteristics of the sample are presented in Table 1. Prospective suicidal behavior was associated with past history of suicide attempts; younger age; higher PDQ and CGI scores; lower GAF score; increased suicidal ideation, loss of interest, abnormal anxiety, psychomotor agitation, high-risk behavior, and irritability; and a more prevalent history of migraine headaches at baseline (p < 0.05). In comparing participants with (n = 103) and without (n = 83) two clinic visits before suicidal behavior, no significant differences were found for baseline clinical symptoms, age, or gender. Individuals who were excluded from the linear mixed model analysis due to number of clinic visits were more likely to report a past history of suicide attempts (X2= 6.87, p = 0.009).
Table 1.
Baseline demographic and clinical characteristics of suicide attempters compared to random sample of non-attempters
| No prospective suicidal behavior | Prospective suicidal behavior | χ2 or t | p-value | |
|---|---|---|---|---|
| Demographics and clinical characteristics | ||||
|
| ||||
| Gender, male, n (%) | 232 (45) | 59 (36) | 3.53a | 0.06 |
| Past suicide attempt, n (%) | 171 (31) | 131 (73) | 96.82a | <0.01 |
| Age, years, mean (SD) | 39.00 (12.90) | 35.46 (12.05) | −3.08 | <0.01 |
| PDQ score-, mean (SD) | 36.86 (18.40) | 48.07 (16.92) | 6.57 | <0.001 |
|
| ||||
| Proposed acute suicide risk factors, mean (SD | ||||
|
| ||||
| Suicidal ideation | 0.16 (0.34) | 0.34 (0.48) | 5.61 | <0.01 |
| Loss of interest | 0.45 (0.64) | 0.71 (0.78) | 4.49 | <0.01 |
| Abnormal anxiety | 4.74 (5.49) | 5.89 (5.54) | 2.47 | 0.01 |
| Psychomotor agitation | 0.24 (0.40) | 0.38 (0.54) | 3.63 | <0.01 |
| High-risk behavior | 0.08 (0.27) | 0.13 (0.35) | 2.32 | <0.01 |
|
| ||||
| Global functioning, mean (SD) | ||||
|
| ||||
| CGI overall | 2.92 (1.26) | 3.61 (1.17) | 6.58 | <0.001 |
| GAF in last month | 61.07 (12.09) | 55.99 (12.03) | −4.95 | <0.001 |
|
| ||||
| Mood effects, mean (SD) | ||||
|
| ||||
| Elevated mood | 1.76 (3.37) | 2.00 (3.54) | 0.82 | 0.41 |
| Abnormal irritability | 3.87 (4.87) | 5.98 (5.75) | 4.89 | <0.001 |
| Depressed mood | 0.43 (0.70) | 0.52 (0.84) | 1.07 | 0.29 |
|
| ||||
| Alcohol/substance abuse and headaches/migraines | ||||
|
| ||||
| Alcohol use (drinks per day), mean (SD) | 0.74 (1.92) | 0.82 (2.90) | 0.44 | 0.66 |
| History of substance use, n (%) | 93 (16) | 40 (22) | 2.56a | 0.11 |
| History of migraines, n (%) | 149 (26) | 66 (35) | 6.17a | 0.01 |
Suicidal ideation, loss of interest, psychomotor agitation, high-risk behavior, and depressed mood are rated on a scale from −2 to +2. Abnormal anxiety, elevated mood, and abnormal irritability were rated as days in the last two weeks.
PDQ = Personality Disorders Questionnaire; CGI = Clinical Global Impression rating scale; GAF = Global Assessment of Functioning rating scale.
Chi-square.
A correlation matrix of selected CMF variables at Month −1 is presented in Table 2. Each prospective suicide risk factor was significantly correlated with the others (p < 0.05) with the exception of high-risk behavior with suicidal ideation and loss of interest. Significant correlations ranged from r = 0.13 to 0.48. With regard to mood effects variables, each was significantly correlated with the prospective suicide risk factors with the exception of high-risk behavior with depressed mood, and elevated mood with suicidal ideation and loss of interest.
Table 2.
Spearman correlations of Clinical Monitoring Form (CMF) outcome variables at Month -1
| Suicidal ideation | Loss of interest | Abnormal anxiety | Psychomotor agitation | High-risk behavior | |
|---|---|---|---|---|---|
| Proposed acute suicide risk factors | |||||
|
| |||||
| Suicidal ideation | – | 0.48a | 0.32a | 0.27a | 0.11 |
| Loss of interest | – | 0.36a | 0.21a | 0.01 | |
| Abnormal anxiety | – | 0.21a | 0.13b | ||
| Psychomotor agitation | – | 0.22a | |||
| High-risk behavior | – | ||||
|
| |||||
| Mood effects | |||||
|
| |||||
| Elevated mood | 0.05 | 0.02 | 0.16a | 0.26a | 0.34a |
| Abnormal irritability | 0.20a | 0.25a | 0.46a | 0.28a | 0.23a |
| Depressed mood | 0.50a | 0.58a | 0.37a | 0.21a | 0.06 |
p < 0.01;
p < 0.05.
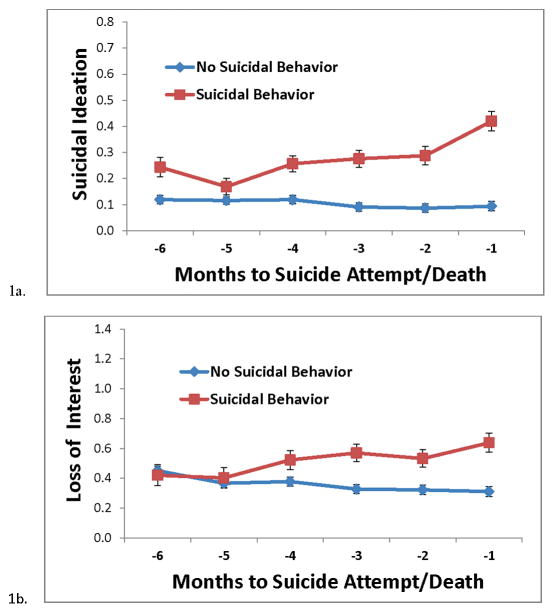
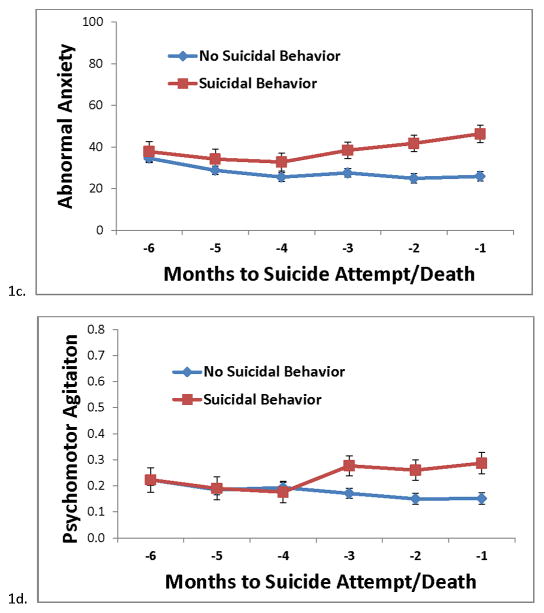
Proposed acute suicide risk factors
From the linear mixed models, a main effect for prospective suicidal behavior was found for suicidal ideation, loss of interest, and abnormal anxiety (p < 0.001), with values higher in the group with prospective suicidal behavior (Table 3). A significant time by suicidal behavior interaction was observed for suicidal ideation and loss of interest (p < 0.001). For suicidal ideation, a significant difference was noted between the groups at all time points with the exception of Month -5 (the fifth month before suicidal behavior). For loss of interest, a significant difference was observed from Months -4 to −1. The main effect or time by suicidal behavior interaction for abnormal anxiety and psychomotor agitation were not significant after adjusting for multiple comparisons. The time by behavior interaction for suicidal ideation was still significant when adjusting for depressed mood (p < 0.001).
Table 3.
Fixed effects for clinical symptoms in time before suicide attempt/death
| Main effect for suicidal behavior | Time by suicidal behavior interaction | Overall effect size between groups | Effect size at Month -1 | |||
|---|---|---|---|---|---|---|
|
|
||||||
| F | p-value | F | p-value | Cohen’s d | Cohen’s d | |
| Proposed acute suicide risk factors | ||||||
|
| ||||||
| Suicidal ideation | 58.57 | <0.001f | 7.31 | <0.001f | 0.67 | 0.41 |
| Loss of interest | 13.28 | <0.001f | 4.00 | 0.001f | 0.31 | 0.22 |
| Abnormal anxiety | 12.91 | <0.001f | 2.39 | 0.04 | 0.31 | 0.20 |
| Psychomotor agitation | 4.22 | 0.04 | 2.64 | 0.02 | 0.18 | 0.14 |
| High-risk behavior | 6.20 | 0.013 | 0.86 | 0.51 | 0.22 | 0.06 |
|
| ||||||
| Global functioning | ||||||
|
| ||||||
| CGIa | 53.28 | <0.001 | 5.84 | <0.001 | 0.63 | 0.38 |
| GAFb | 30.51 | <0.001 | 4.84 | <0.001 | 0.48 | 0.33 |
|
| ||||||
| Mood effects | ||||||
|
| ||||||
| Elevated moodc | 9.89 | 0.002 | 0.51 | 0.12 | 0.28 | 0.08 |
| Abnormal irritabilityc | 13.01 | <0.001 | 0.72 | 0.61 | 0.31 | 0.11 |
| Depressed moodd | 13.62 | <0.001 | 1.99 | 0.08 | 0.38 | 0.24 |
|
| ||||||
| Alcohol/substance abuse and headaches/migrainese | ||||||
|
| ||||||
| Alcohol abuse | 4.46 | 0.035 | 1.66 | 0.14 | 0.19 | 0.05 |
| Substance abuse | 12.31 | <0.001 | 1.49 | 0.19 | 0.30 | 0.06 |
| Headaches | 4.30 | 0.039 | 1.01 | 0.41 | 0.18 | 0.09 |
| Migraine headaches | 0.61 | 0.44 | 1.17 | 0.32 | 0.07 | 0.00 |
CGI = Clinical Global Impression rating scale. Higher scores represent more severe illness. Average CGI in the last month before suicidal behavior was 3.7 [standard error (SE) = 0.1]. Average CGI in last month for controls was 2.58 (SE = 0.07).
GAF = Global Assessment of Functioning. Higher scores represent higher levels of functioning. Average GAF in the last month before suicidal behavior was 56.3 (SE = 1.2). Average GAF in last month for controls was 65.1 (SE = 0.7).
Elevated mood and Abnormal irritability were assessed on a similar scale as Abnormal Anxiety, that is, a percentage (from 0 to 100) of time in the last 10 days was that the symptom was experienced.
Depressed mood was assessed on the same scale as suicidal thoughts, loss of interest, psychomotor agitation, and high-risk behavior, that is, on a scale from −2 to +2.
Alcohol/substance abuse and Headaches/migraines were measured on a dichotomous scale of ‘Yes/No’.
Significant after correcting for multiple comparisons, Bonferroni, p = 0.01, two-tailed.
Trajectories of clinical symptoms in the six months before suicide attempt are presented in Figures 1A–1E. Overall effect sizes between groups ranged from 0.18 (high-risk behavior) to 0.66 (suicidal ideation). In order to compare the symptom trajectories across the same scale, the effect sizes for all symptoms by month before suicidal behavior are presented in Figure 2.
Figure 1.
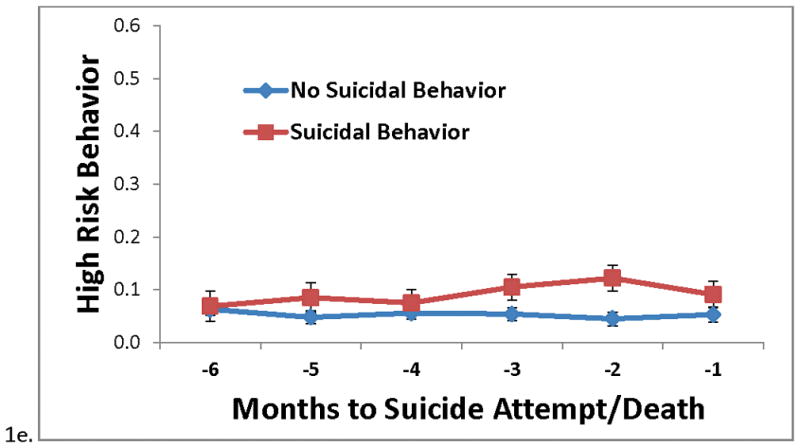
1A–1E. Median clinical symptoms in the six months before suicide attempt/death, compared to random sample of non-attempters. All assessments were taken from the Clinical Monitoring Form (CMF). Due to the use of linear mixed models, all figures include estimated marginal means and standard errors of these mean estimates.
Fig. 2.
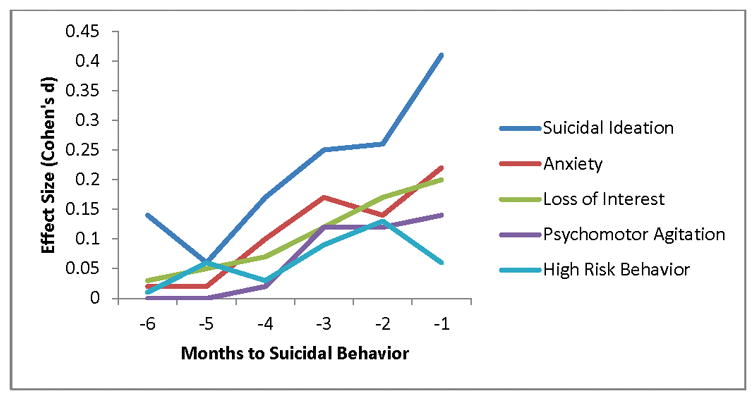
Differences in symptom trajectories in the six months before suicidal behavior in patients with versus without prospective suicidal behavior.
Global functioning and mood effects
For a general picture of clinical functioning and mood effects, additional models were run with the CGI scale, the GAF scale, elevated mood, irritability, depressed mood, substance/alcohol use, as well as headaches and migraine headaches, not adjusting for multiple comparisons. Both CGI and GAF scores demonstrated a significant main effect and time by suicidal behavior interaction (p < 0.001). Elevated mood, abnormal irritability, alcohol use, substance use and headache demonstrated a significant main effect, but there was no time by behavior interaction. For depressed mood, the main effect was significant, but the interaction did not reach significance (p = 0.08) although effect sizes were comparable to those for loss of interest and anxiety. Additional data regarding potential acute suicide risk factors adjusted for mood effects, as well as age, history of suicide attempts, and PDQ score are presented in the Supporting Information.
Supplemental analyses
As noted previously, ratings were collapsed over two-month, instead of one-month, intervals in a post-hoc model due to concerns about missing data. Using linear mixed models with these intervals, similar effect sizes were noted for suicidal ideation, loss of interest, and anxiety. Models also found similar effect sizes when only SAE form-reported suicidal behaviors were included and when models were run excluding suicide deaths (see Supplementary Tables S1A and S1B).
Symptoms in the five months before suicidal behavior were run, adjusting for symptoms in the sixth month (see Supplementary Table 1C). Across the supplemental analyses, similar effect sizes were found for the loss of interest and anxiety variables.
To ensure that these findings were not due to variables in the comparison sample, the same models were run with a new, distinct 15% random sample of non-attempters. Overall effect sizes for main effects and interactions were comparable.
Discussion
In this sample of patients drawn from the STEP-BD study, suicidal thoughts were elevated for up to four months before suicide attempt or death. Loss of interest was also moderately elevated before suicidal behavior, while anxiety was not significantly elevated before suicidal behavior after adjusting for multiple comparisons. Psychomotor agitation and high-risk behavior were associated with prospective suicidal behavior overall, but did not demonstrate a similar trajectory in the months just before suicidal behavior. Taken together, our findings suggest that suicidal ideation and loss of interest may represent acute risk factors for suicidal behavior in patients with BD in outpatient settings.
These results reinforce the role of suicidal ideation as an acute risk factor for suicidal behavior (22, 23). The post-hoc finding that suicidal ideation was elevated in the months before suicidal behavior independent of changes in depressed mood further underscores the importance of regular direct assessment of suicidal thoughts in order to observe possible fluctuations. Measures such as the Columbia Suicide Severity Rating Scale (C-SSRS) (31), the Scale for Suicide Ideation (SSI) (32), and the Suicide Status Form (SSF) (33) were developed for this purpose. In addition, it is possible that suicidal thoughts increased in intensity during the time before suicidal behavior, although this is difficult to interpret from the CMF item. Further investigations of factors that lead to increased severity of suicidal thoughts may have important implications for the treatment of suicidal patients.
Loss of interest (often referred to as anhedonia) and, to a lesser extent, anxiety, also emerged as acute risk factors for suicide; nevertheless, inconsistent results on supplemental analyses underscore the need for additional replication. Fawcett and colleagues previously identified anhedonia as a clinical warning sign for suicide (24) and, more recently, changes in anhedonia were shown to correlate with suicidal thoughts independent of depression in a sample of psychiatric inpatients (34). Anxiety has commonly been assessed as an acute risk factor for suicide and has been associated with the transition from suicidal thoughts to suicidal behavior (25). In addition, anxiety sensitivity has been the focus of cognitive behavioral treatment to reduce suicidal thoughts and behavior (35). Because these symptoms are closely related to depressed mood, further work is needed to examine whether each symptom independently predicts acute risk or whether it represents an underlying suicidal ‘process’ or ‘mode’ comprising multiple related symptoms as part of a suicidal crisis (36).
In the present study, psychomotor agitation and high-risk behavior showed no statistically significant increase in symptoms right before suicide attempt/death. Non-significant findings may reflect the inadequacy of a single item to capture a phenomenon as complex as agitation or impulsivity, which may also depend on clinical context such as mood state or substance abuse. Nevertheless, the results suggest that these symptoms may be useful as long-term, but not acute, risk factors in the months before suicidal behavior. For example, aggressive impulsivity is a proposed suicide endophenotype (37), but whether it functions as an underlying risk factor for suicide for an individual across the lifespan or as a symptom whose exacerbation leads to a suicidal crisis or “impulsive attempt” remains to be seen (38). Such a discussion highlights the difficulties inherent in suicide research and the need for innovative approaches to better categorize the time period before suicidal behavior.
Despite the importance of these preliminary findings, this study is also associated with several limitations that reinforce the need for further investigation and replication. First, participants in a research trial may not generalize to assessment and care received in the community. As noted in a previous STEP-BD analysis (15), the suicide rate in the STEP-BD trial may be lower than what would be seen in the community due to the regular clinical visits, standardized assessments, and evidence-based treatments associated with the trial. In addition, we excluded potentially high-risk participants with less than two visits during the time frame of interest from analysis, which may have led to an incomplete picture of acute suicide risk in this sample. As follow-up with suicidal patients is often difficult, new technologies such as text messaging and smartphone applications could be beneficial in future studies of symptom monitoring in suicidal patients.
Second, the use of single items from the CMF, which often used a ‘none or usual’ score, may not have captured the complexity of symptoms. Future analyses will need to use assessments comprising multiple items, such as the C-SSRS, SSI, or SSF—all of which can independently capture both symptom intensity and change from baseline—for a more comprehensive suicide risk assessment.
Third, it is possible that these symptom trajectories, or the impact of mood state, would differ if weekly or daily data were available. Fourth, many other possible clinical symptoms could have been evaluated as acute risk factors, such as sleep disturbance, more in-depth assessments of the symptoms of borderline personality disorder, or other types of physical pain. Fifth, the time period for the comparison sample may not have been comparable to the time frame used in the participants with suicidal behavior. Lastly, data presented here were reported by the patient to a clinician. Multimodal investigation of these acute risk factors, including implicit measures, biomarkers, and behavioral paradigms (39), is indicated.
Conclusions
This study found that increased suicidal ideation, loss of interest and, to a lesser extent, anxiety, may represent acute risk factors for later suicidal behavior in patients with BD. High-risk behavior and increased psychomotor agitation were confirmed as longer-term risk factors; however, patients may not report increased intensity of these symptoms in the months before suicide attempt or death.
Supplementary Material
Acknowledgments
Data used in the preparation of this article were obtained from the limited access datasets distributed from the National Institute of Health-supported Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) study. This multi-site clinical trial studies current treatments for bipolar disorder, including medications and psychosocial therapies. The study was supported by National Institute of Mental Health (NIMH) Contract #N01MH80001 to Massachusetts General Hospital and the University of Pittsburgh. The ClinicalTrials.gov identifier is NCT00012558. The opinions, interpretations, conclusions, and recommendations reported here are those of the authors and are not necessarily endorsed by the STEP-BD study investigators or the federal government.
Funding for this work was supported by the Intramural Research Program at the NIMH, National Institutes of Health (IRP-NIMH-NIH; ZIA MH002927) by a NARSAD Independent Investigator Award to CAZ, and by a Brain and Behavior Mood Disorders Research Award to CAZ.
EDB had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Ioline Henter (NIMH) provided invaluable editorial assistance.
Footnotes
Trial Registration: NCT00012558 (original STEP-BD trial); NCT00088699 (present study)
Portions of this analysis were presented at the annual meeting of the American Association of Suicidology, April 15-18, 2015, Atlanta, GA, USA
Disclosures
CAZ is listed as a co-inventor on a patent for the use of ketamine and its metabolites in major depression and has assigned his rights in the patent to the U.S. government but will share a percentage of any royalties that may be received by the government. EDB, JLVV, DAL, RM-V, and MT report no conflicts of interest, financial or otherwise.
References
- 1.Centers for Disease Control and Prevention. National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) 2013. [Google Scholar]
- 2.Crosby AE, Han B, Ortega LA, Parks SE, Gfroerer J. Suicidal thoughts and behaviors among adults aged >/=18 years--United States, 2008–2009. MMWR Surveill Summ. 2011;60:1–22. [PubMed] [Google Scholar]
- 3.O'Connor E, Gaynes BN, Burda BU, Soh C, Whitlock EP. Screening for and treatment of suicide risk relevant to primary care: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;158:741–54. doi: 10.7326/0003-4819-158-10-201305210-00642. [DOI] [PubMed] [Google Scholar]
- 4.Borges G, Nock MK, Haro Abad JM, Hwang I, Sampson NA, Alonso J, et al. Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. J Clin Psychiatry. 2010;71:1617–28. doi: 10.4088/JCP.08m04967blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldney RD, Spence ND. Is suicide predictable? Aust N Z J Psychiatry. 1987;21:3–4. doi: 10.1080/00048678709160893. [DOI] [PubMed] [Google Scholar]
- 6.Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J Consult Clin Psychol. 2000;68:371–7. [PubMed] [Google Scholar]
- 7.Schaffer A, Isometsä ET, Tondo L, et al. International Society for Bipolar Disorders Task Force on Suicide: meta-analyses and meta-regression of correlates of suicide attempts and suicide deaths in bipolar disorder. Bipolar Disord. 2015;17:1–16. doi: 10.1111/bdi.12271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nordentoft M, Mortensen PB, Pedersen CB. Absolute risk of suicide after first hospital contact in mental disorder. Arch Gen Psychiatry. 2011;68:1058–64. doi: 10.1001/archgenpsychiatry.2011.113. [DOI] [PubMed] [Google Scholar]
- 9.Suominen K, Isometsa E, Suokas J, Haukka J, Achte K, Lonnqvist J. Completed suicide after a suicide attempt: a 37-year follow-up study. Am J Psychiatry. 2004;161:562–3. doi: 10.1176/appi.ajp.161.3.562. [DOI] [PubMed] [Google Scholar]
- 10.National Action Alliance for Suicide Prevention: Research Prioritization Task Force. A prioritized research agenda for suicide prevention: An action plan to save lives. Rockville, MD: National Institute of Mental Health and the Research Prioritization Task Force; 2014. [Google Scholar]
- 11.Bagge CL, Glenn CR, Lee HJ. Quantifying the impact of recent negative life events on suicide attempts. J Abnorm Psychol. 2013;122:359–68. doi: 10.1037/a0030371. [DOI] [PubMed] [Google Scholar]
- 12.Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33:395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- 13.Antypa N, Antonioli M, Serretti A. Clinical, psychological and environmental predictors of prospective suicide events in patients with bipolar disorder. J Psychiatr Res. 2013;47:1800–8. doi: 10.1016/j.jpsychires.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Bauer MS, Wisniewski SR, Marangell LB, Chessick CA, Allen MH, Dennehy EB, et al. Are antidepressants associated with new-onset suicidality in bipolar disorder? A prospective study of participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) J Clin Psychiatry. 2006;67:48–55. doi: 10.4088/jcp.v67n0108. [DOI] [PubMed] [Google Scholar]
- 15.Dennehy EB, Marangell LB, Allen MH, Chessick C, Wisniewski SR, Thase ME. Suicide and suicide attempts in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) J Affect Disord. 2011;133:423–7. doi: 10.1016/j.jad.2011.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marangell LB, Dennehy EB, Wisniewski SR, Bauer MS, Miyahara S, Allen MH, et al. Case-control analyses of the impact of pharmacotherapy on prospectively observed suicide attempts and completed suicides in bipolar disorder: findings from STEP-BD. J Clin Psychiatry. 2008;69:916–22. doi: 10.4088/jcp.v69n0605. [DOI] [PubMed] [Google Scholar]
- 17.Simon NM, Zalta AK, Otto MW, Ostacher MJ, Fischmann D, Chow CW, et al. The association of comorbid anxiety disorders with suicide attempts and suicidal ideation in outpatients with bipolar disorder. J Psychiatr Res. 2007;41:255–64. doi: 10.1016/j.jpsychires.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 18.Rudd MD, Berman AL, Joiner TE, Jr, Nock MK, Silverman MM, Mandrusiak M, et al. Warning signs for suicide: theory, research, and clinical applications. Suicide Life Threat Behav. 2006;36:255–62. doi: 10.1521/suli.2006.36.3.255. [DOI] [PubMed] [Google Scholar]
- 19.Glenn CR, Nock MK. Improving the short-term prediction of suicidal behavior. Am J Prev Med. 2014;47(3 Suppl 2):S176–S80. doi: 10.1016/j.amepre.2014.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Claasen CA, Harvilchuck-Laurenson JD, Fawcett J. Prognostic models to detect and monitor the near-term risk of suicide: state of the science. Am J Prev Med. 2014;47(Suppl 2):S181–S5. doi: 10.1016/j.amepre.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Holma KM, Haukka J, Suominen K, et al. Differences in incidence of suicide attempts between bipolar I and II disorders and major depressive disorder. Bipolar Disord. 2014;16:652–61. doi: 10.1111/bdi.12195. [DOI] [PubMed] [Google Scholar]
- 22.Britton PC, Ilgen MA, Rudd MD, Conner KR. Warning signs for suicide within a week of healthcare contact in Veteran decedents. Psychiatry Res. 2012;200:395–9. doi: 10.1016/j.psychres.2012.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuo WH, Gallo JJ, Tien AY. Incidence of suicide ideation and attempts in adults: the 13-year follow-up of a community sample in Baltimore, Maryland. Psychol Med. 2001;31:1181–91. doi: 10.1017/s0033291701004482. [DOI] [PubMed] [Google Scholar]
- 24.Fawcett J, Scheftner WA, Fogg L, Clark DC, Young MA, Hedeker D, et al. Time-related predictors of suicide in major affective disorder. Am J Psychiatry. 1990;147:1189–94. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- 25.Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15:868–76. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sani G, Tondo L, Koukopoulos A, Reginaldi D, Kotzalidis GD, Koukopoulos AE, et al. Suicide in a large population of former psychiatric inpatients. Psychiatry Clin Neurosci. 2011;65:286–95. doi: 10.1111/j.1440-1819.2011.02205.x. [DOI] [PubMed] [Google Scholar]
- 27.Dumais A, Lesage AD, Alda M, Rouleau G, Dumont M, Chawky N, et al. Risk factors for suicide completion in major depression: a case-control study of impulsive and aggressive behaviors in men. Am J Psychiatry. 2005;162:2116–24. doi: 10.1176/appi.ajp.162.11.2116. [DOI] [PubMed] [Google Scholar]
- 28.Sachs GS, Thase ME, Otto MW, Bauer M, Miklowitz D, Wisniewski SR, et al. Rationale, design, and methods of the systematic treatment enhancement program for bipolar disorder (STEP-BD) Biol Psychiatry. 2003;53:1028–42. doi: 10.1016/s0006-3223(03)00165-3. [DOI] [PubMed] [Google Scholar]
- 29.Sachs GS. Strategies for improving treatment of bipolar disorder: integration of measurement and management. Acta Psychiatr Scand Suppl. 2004:7–17. doi: 10.1111/j.1600-0447.2004.00409.x. [DOI] [PubMed] [Google Scholar]
- 30.Fossati A, Maffei C, Bagnato M, Donati D, Donini M, Fiorilli M, et al. Brief communication: criterion validity of the Personality Diagnostic Questionnaire-4+ (PDQ-4+) in a mixed psychiatric sample. J Pers Disord. 1998;12:172–8. doi: 10.1521/pedi.1998.12.2.172. [DOI] [PubMed] [Google Scholar]
- 31.Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266–77. doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343–52. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 33.Jobes DA, Nelson KN, Peterson EM, Pentiuc D, Downing V, Francini K, et al. Describing suicidality: an investigation of qualitative SSF responses. Suicide Life Threat Behav. 2004;34:99–112. doi: 10.1521/suli.34.2.99.32788. [DOI] [PubMed] [Google Scholar]
- 34.Winer ES, Nadorff MR, Ellis TE, Allen JG, Herrera S, Salem T. Anhedonia predicts suicidal ideation in a large psychiatric inpatient sample. Psychiatry Res. 2014;218:124–8. doi: 10.1016/j.psychres.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 35.Capron DW, Norr AM, Zvolensky MJ, Schmidt NB. Prospective evaluation of the effect of an anxiety sensitivity intervention on suicidality among smokers. Cogn Behav Ther. 2014;43:72–82. doi: 10.1080/16506073.2013.777466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wenzel A, Brown GK, Beck AT. Cognitive therapy for suicidal patients : scientific and clinical applications. 1. Washington, DC: American Psychological Association; 2009. [Google Scholar]
- 37.Mann JJ, Arango VA, Avenevoli S, Brent DA, Champagne FA, Clayton P, et al. Candidate endophenotypes for genetic studies of suicidal behavior. Biol Psychiatry. 2009;65:556–63. doi: 10.1016/j.biopsych.2008.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Watkins HB, Meyer TD. Is there an empirical link between impulsivity and suicidality in bipolar disorders? A review of the current literature and the potential psychological implications of the relationship. Bipolar Disord. 2013;15:542–558. doi: 10.1111/bdi.12090. [DOI] [PubMed] [Google Scholar]
- 39.Nock MK, Park JM, Finn CT, Deliberto TL, Dour HJ, Banaji MR. Measuring the suicidal mind: implicit cognition predicts suicidal behavior. Psychol Sci. 2010;21:511–7. doi: 10.1177/0956797610364762. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.