Abstract
Objectives
Anesthesia can alter gastric and small intestinal motility, but its effect on gastroesophageal reflux (GER) is unclear. We set out to evaluate the effect of anesthesia on pH-multichannel intraluminal Impedance (pH Impedance) evaluation of GER.
Methods
Retrospective single center analysis of 95 pH Impedance probe studies performed in patients both with anesthesia exposure and esophagogastroduodenoscopy (n=50) and without (n=45).
Results
Increased acid reflux per hour, non-acid reflux per hour and total reflux per hour was observed in the first 4 hours, both overall and in ≥1 year olds and in both sedation groups. This difference remained for the older children without sedation by multiple regression analysis for non-acid reflux per hour and total reflux per hour. Patients using PPI had more non-acid reflux events per hour and total reflux events per hour regardless of sedation.
Conclusions
Based on the results of this study, there is no need to eliminate the data collected immediately after placement of the probe in children under 1 year old, but in those ≥1 without sedation, there may be a greater number of reflux events in the first 4 hours. The first 4 hours, therefore, should be carefully evaluated in patients older than 1 year of age. Further study is needed to provide normative data for the first 4 hours versus the later time period, both for those undergoing sedation as well as unsedated patients, in order to validate the findings from this study and to better understand the mechanism of GER.
Keywords: pH Impedance, Anesthesia, Gastroesophageal Reflux
Introduction
The pH-multichannel intraluminal impedance (pH impedance) monitor is a sensitive tool that is used to detect liquid reflux, independent of pH, and gas reflux episodes.1–3 PH impedance monitoring has been used in pediatrics since 2002 and is becoming the gold standard for the evaluation of reflux. The utility of pH impedance studies, however, is limited by the lack of robust reference range data on the quantity of reflux in healthy children and a shortage of evidence-based studies validating results to clinical outcomes. Despite these limitations, it is increasingly used in the evaluation of gastroesophageal reflux disease (GERD). The pH impedance monitor can be placed while a child is awake or under anesthesia and is frequently coordinated with esophagogastroduodenoscopy (EGD). There is currently very little data regarding the effects of anesthesia on pH impedance results.
It is well established that anesthesia decreases gastric emptying.1, 2, 4–7 This effect appears to be independent of the type of anesthesia, with decreased emptying documented with both inhaled and epidural anesthetics as well as with propofol.7, 8 Lombardo et al. used electrogastrography to show abnormal motility in the stomach following anesthesia exposure.6 Motility of the small intestine is also decreased by anesthesia.9 Several studies suggest motility returns to normal about two hours following anesthesia exposure.4, 7, 8 It is unknown how delayed gastric emptying and decreased gastric and intestinal motility affects gastroesophageal reflux, but it could be postulated that decreased motility will result in increased reflux events.
There is scant literature regarding the influence of anesthesia on pH impedance monitoring. Because adults typically have the pH impedance monitor placed while they are awake, there is no adult literature on this subject. Research in animals has shown that anesthesia increases reflux. In cats, propofol increases reflux during anesthesia.10 Anesthesia with acepromazine, propofol, and isoflurane caused decreased pH and an increased number of reflux episodes in anesthetized dogs compared to awake dogs.11 These studies, however, do not address the question of what happens to gastroesophageal reflux after anesthesia ends or how long the effects last.
There is one pediatric study that has looked at this question, comparing the pH tracings of 88 children during the six hours after anesthesia to the six-hour period 24 hours later using a Bravo capsule attached to the wall of the esophagus during EGD.12 This study found increased reflux episodes in the period following anesthesia, but evaluated only pH and not impedance. In this study, the attachment of the capsule itself may alter reflux patterns.
Given that anesthesia decreases gastric emptying and affects both gastric and small intestinal motility, it is important to evaluate if anesthesia exposure changes the results of the pH impedance study. A better understanding of how anesthesia affects pH impedance monitoring could greatly change how studies are interpreted and the conclusions made from them. We hypothesized that anesthesia would increase the amount of both acid and non-acid reflux in the four hours immediately following anesthesia in children.
Methods
Participants
We performed a retrospective, single-center study evaluating patients that had undergone pH impedance studies at Children's Hospital Colorado during the years 2009 – 2012 (1322 studies completed during this time frame). The study was approved by our institutional review board (COMIRB Protocol number 12-1442) and was exempted from patient/parent consent. Each researcher was assigned a year of patients from which to identify subjects. Patients were randomly selected from our existing database based on age and stratified into 2 different groups: less than 1 year of age and greater than 1 year of age. Children younger than 2 months and older than 18 years were not included. Matching cases for each age group were found both with and without anesthesia exposure, and all cases were reviewed individually to ensure the pH impedance study was at least 24 hours long and of sufficient quality. From there, each patient’s individual pH impedance data was reviewed. Demographic information was collected for each subject including age, gender, body mass index (BMI), endoscopy data available for those undergoing EGD (presence or absence of esophagitis), use of proton pump inhibitor (PPI) medication, and exposure to medications at the time of pH impedance placement including ondansetron and the type of anesthesia used (if applicable). Seven patients were removed from the study due to incomplete (< 24 hours) or poor quality data (probe failure) following data collection during a quality review by one of the researchers.
Measures
Each patient’s pH impedance study data was analyzed using software from Sandhill Scientific and this analysis was used without manual modification. Three specific time intervals were chosen to evaluate separately. To characterize the potential effect of anesthesia, the initial 4 hours of the study were analyzed as these were postulated to show the most affect from anesthesia. The “abridged” study was the remainder of the study excluding the first 4 hours. Lastly, the total study was re-analyzed including both the initial 4 hours and the remainder of the recorded study time (full study). For each discrete time interval, the same data was collected including the percentage of the time with pH less than 4, the number of both acid reflux events and non-acid reflux events per hour, the number of reflux events lasting longer than 5 minutes, the length of time of the longest reflux event, and the percent time recumbent (by parental report).
Statistical Analysis
All original pH impedance data was analyzed with Sandhill Scientific software (version 5.5.5.1). Reports were verified and data was collected in Microsoft Excel. Patient demographics were compared by t-tests for continuous variables and an exact chi-square test for categorical variables. The outcomes including % time pH <4, number of acid reflux episodes/hour, number of non-acid reflux episodes/hour and total number of reflux episodes/hour were not normally distributed (the data were skewed) so geometric means with 95% confidence intervals were calculated for the univariate analyses. General linear models were used to compare the outcomes between sedation and no sedation groups, taking into account use of opioids, ondansetron, patient BMI, PPI, esophagitis and age group (<1 vs. ≥1), using log transformed outcome data. Similar models were used to test the difference in the outcomes between the first 4 hours and the abridged data, using untransformed data since the differences in the outcomes were normally distributed. The effect of sedation was tested within the general linear model for the dataset. Comparisons were also made within each age subgroup, and also between PPI groups, using similar methods. All statistical analyses were conducted using SAS Version 9.4 (SAS Inc., Cary, NC)
Results
The patient characteristics (age, BMI and sex) were similar for the two groups (Table 1). Ninety-five patients were analyzed, 22 aged <1 and 73 aged ≥1 year of age. In those <1 year of age, 11 received anesthesia and 11 received no sedation. In those ≥1 year of age, 39 received anesthesia and 34 received no sedation. Six subjects were excluded due to incomplete studies (less than 24 hours) and one was removed due to concern for probe failure. The anesthesia group consists primarily of patients who received both inhalant and propofol anesthesia, although 8 patients (16%) received only inhalant or only propofol for anesthesia. Twenty-eight of the patients (56%) also received opioids during the procedure. The mean anesthesia time was 34 minutes.
TABLE 1.
Demographics on all 95 patients
| Variable | Covariate Group |
Anesthesia (n=50) |
No Sedation (n=45) |
p-value |
|---|---|---|---|---|
| Age | Mean(SD) | 5.78 (5.48) | 5.12 (5.16) | 0.550 |
| BMI | Mean(SD) | 18.65 (4.75) | 17.06 (3.87) | 0.080 |
| Sex | Male | 32 (64.0) | 22 (48.9) | 0.152 |
| Opioids | Yes | 28 (56.0) | 0 (0.0) | <.001 |
| Ondansetron | Yes | 36 (72.0) | 1 (2.2) | <0.001 |
| PPI | Yes | 34 (68.0) | 26 (57.8) | 0.395 |
| Esophagitis | Unknown | 3 (6.0) | 27 (60.0) | <0.001 |
| Yes | 11 (22.0) | 8 (17.8) |
| Patients aged <1 year: | ||||
|---|---|---|---|---|
| Variable | Covariate Group |
Anesthesia (n=11) |
No Sedation (n=11) |
p-value |
| Age | Mean(SD) | 0.61 (0.23) | 0.41 (0.23) | 0.062 |
| BMI | Mean(SD) | 16.68 (1.44) | 15.73 (1.95) | 0.205 |
| Sex | Male | 10 (90.9) | 7 (63.6) | 0.311 |
| Opioids | Yes | 4 (36.4) | 0 (0.0) | 0.090 |
| Ondansetron | Yes | 3 (27.3) | 0 (0.0) | 0.214 |
| PPI | Yes | 8 (72.7) | 9 (81.8) | 1.000 |
| Esophagitis | Unknown | 3 (27.3) | 10 (90.9) | 0.008 |
| Yes | 1 (9.1) | 0 (0.0) | ||
| Patients aged ≥1 year: | ||||
|---|---|---|---|---|
| Variable | Covariate Group |
Anesthesia (n=39) |
No Sedation (n=34) |
p-value |
| Age | Mean(SD) | 7.23 (5.37) | 6.64 (5.06) | 0.631 |
| BMI | Mean(SD) | 19.20 (5.21) | 17.49 (4.25) | 0.133 |
| Sex | Male | 22 (56.4) | 15 (44.1) | 0.352 |
| Opioids | Yes | 24 (61.5) | 0 (0.0) | <0.001 |
| Ondansetron | Yes | 33 (84.6) | 1 (2.9) | <0.001 |
| PPI | Yes | 26 (66.7) | 17 (50.0) | 0.162 |
| Esophagitis | Unknown | 0 (0.0) | 17 (50.0) | <0.001 |
| Yes | 10 ( 25.6) | 8 ( 23.5) | ||
The pH-multichannel intraluminal Impedance monitor measures both acidic and non-acidic reflux. Non-acidic reflux is defined as a refluxate with a pH greater than 4, while acidic reflux is defined by a pH less than 4. Univariate analysis of the full data set showed a significant difference (p=0.042) over the full study time, 0.58 versus 0.91 acid reflux events per hour for anesthesia versus no sedation, respectively (See Table 2). A significant difference was also found in the first 4 hours (p=0.002) for the comparison between acid reflux per hour with anesthesia (0.96 acidic reflux events per hour) versus no sedation (1.80 acidic reflux events per hour). In patients ≥ 1 year old, univariate analysis showed a significant difference (p=0.008) in first 4 hours, anesthesia versus no sedation, for acid reflux per hour. Over the entire period of observation there were fewer acid reflux events per hour in the anesthesia group (0.59) compared with the no sedation group (0.96) in those aged ≥ 1, but this did not reach statistical significance (p=0.056). A significant difference was observed in the older age group for total number of reflux episodes per hour in the first 4 hours (2.09 versus 3.11 for anesthesia versus no sedation, respectively, p=0.030). No differences were identified in the <1 year old group with univariate analysis or for any comparisons with multiple regression for the effect of sedation on outcome, allowing for opioids, ondansetron, BMI, PPI and esophagitis (see supplementary Table 1, http://links.lww.com/MPG/A588). There was no statistically significant difference when comparing % time in which pH was <4 for any of the comparisons.
TABLE 2.
Univariate analysis for each outcome (geometric mean and 95% confidence intervals), overall and for patients aged ≥1. Multiple regression analyses are presented in the Supplemental Digital Content.
| All patients: | ||||
|---|---|---|---|---|
| Outcome | Dataset | Sedation | No Sedation | p-value |
| % Time pH < 4 | Full data | 1.23 (0.82, 1.84) | 1.51 (0.93, 2.44) | 0.513 |
| Abridged data | 1.07 (0.68, 1.69) | 1.63 (0.97, 2.73) | 0.222 | |
| First 4 hours | 1.88 (1.24, 2.85) | 2.48 (1.56, 3.94) | 0.368 | |
| Number of acid reflux episodes/hour |
Full data | 0.58 (0.43, 0.78) | 0.91 (0.66, 1.26) | 0.042 |
| Abridged data | 0.51 (0.36, 0.71) | 0.66 (0.44, 0.98) | 0.317 | |
| First 4 hours | 0.96 (0.73, 1.27) | 1.80 (1.37, 2.36) | 0.002 | |
| Number of non-acid reflux episodes/hour |
Full data | 0.92 (0.68, 1.23) | 0.90 (0.67, 1.19) | 0.911 |
| Abridged data | 0.90 (0.66, 1.21) | 0.90 (0.68, 1.20) | 0.967 | |
| First 4 hours | 1.28 (0.97, 1.69) | 1.45 (1.10, 1.91) | 0.533 | |
| Total number of reflux episodes/hour |
Full data | 1.82 (1.49, 2.22) | 2.19 (1.83, 2.62) | 0.173 |
| Abridged data | 1.74 (1.41, 2.16) | 2.03 (1.67, 2.47) | 0.290 | |
| First 4 hours | 2.14 (1.66, 2.75) | 2.72 (2.08, 3.57) | 0.188 | |
| Patients aged ≥1: | ||||
|---|---|---|---|---|
| Outcome | Dataset | Sedation | No Sedation | p-value |
| % Time pH < 4 | Full data | 1.47 (0.96, 2.27) | 1.44 (0.86, 2.41) | 0.942 |
| Abridged data | 1.24 (0.75, 2.05) | 1.53 (0.87, 2.70) | 0.572 | |
| First 4 hours | 1.87 (1.28, 2.74) | 2.53 (1.54, 4.17) | 0.325 | |
| Number of acid reflux episodes/hour |
Full data | 0.59 (0.41, 0.85) | 0.96 (0.67, 1.37) | 0.056 |
| Abridged data | 0.54 (0.37, 0.80) | 0.77 (0.51, 1.16) | 0.221 | |
| First 4 hours | 1.02 (0.75, 1.39) | 1.84 (1.36, 2.50) | 0.008 | |
| Number of non-acid reflux episodes/hour |
Full data | 0.74 (0.54, 1.01) | 0.76 (0.56, 1.04) | 0.868 |
| Abridged data | 0.72 (0.52, 0.98) | 0.74 (0.55, 1.00) | 0.876 | |
| First 4 hours | 1.22 (0.90, 1.64) | 1.48 (1.11, 1.98) | 0.335 | |
| Total number of reflux episodes per hour |
Full data | 1.64 (1.32, 2.05) | 2.17 (1.81, 2.59) | 0.054 |
| Abridged data | 1.56 (1.23, 1.97) | 1.88 (1.51, 2.35) | 0.238 | |
| First 4 hours | 2.09 (1.59, 2.73) | 3.11 (2.43, 4.00) | 0.030 | |
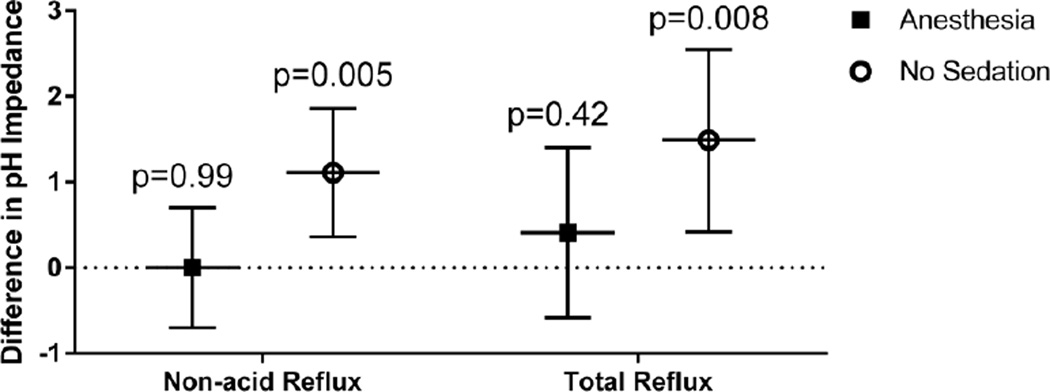
Significant differences were seen when evaluating change between the time periods, comparing the first 4 hours data to the abridged data (See Table 3). In the no sedation group, there were more acid, non-acid and total reflux episodes per hour in the first 4 hours compared to the abridged study. This effect was statistically significant in patients aged ≥1 (p<0.001, p=0.006 and p<0.001 for acid, non-acid and total reflux, respectively), and remained significant in patients aged ≥1 even when allowing for other covariates (p=0.005 and p=0.008 for non-acid and total reflux, respectively, Figure 1; supplementary Table 2, http://links.lww.com/MPG/A589). Therefore, there were significantly more non-acid reflux events per hour in the first 4 hours compared with the later time period in older children. However, this difference was not statistically greater in the no sedation group than the anesthesia group (p=0.082), although the effect was larger in the no sedation group.
TABLE 3.
Univariate analysis for the mean change (and 95% confidence intervals) from the 1st 4 hours to the abridged dataset for each outcome, overall and for patients aged ≥1, and by sedation. Multiple regression analyses are presented in the Supplemental Digital Content.
| All patients: | ||
|---|---|---|
| Outcome | Mean difference | p-value |
| % Time pH < 4 | 0.47 (−0.62, 1.56) | 0.402 |
| Number of acid reflux episodes/hour | 0.44 ( 0.18, 0.70) | 0.001 |
| Number of non-acid reflux episodes/hour | 0.45 ( 0.13, 0.77) | 0.007 |
| Total number of reflux episodes/hour | 0.90 ( 0.51, 1.29) | <.001 |
| Patients aged ≥1: | ||
|---|---|---|
| Outcome | Mean difference | p-value |
| % Time pH < 4 | 0.58 (−0.79, 1.96) | 0.408 |
| Number of acid reflux episodes/hour | 0.50 ( 0.18, 0.82) | 0.003 |
| Number of non-acid reflux episodes/hour | 0.62 ( 0.31, 0.93) | <0.001 |
| Total number of reflux episodes/hour | 1.14 ( 0.69, 1.58) | <0.001 |
| All patients: | |||
|---|---|---|---|
| Outcome | Sedation Group | Mean difference | p-value |
| % Time pH < 4 | Sedation | −0.23 (−1.72, 1.27) | 0.768 |
| No Sedation | 1.24 (−0.34, 2.82) | 0.127 | |
| Number of acid reflux episodes/hour | Sedation | 0.22 (−0.14, 0.57) | 0.232 |
| No Sedation | 0.68 ( 0.31, 1.05) | <0.001 | |
| Number of non-acid reflux episodes/hour | Sedation | 0.45 ( 0.00, 0.89) | 0.052 |
| No Sedation | 0.46 (−0.01, 0.93) | 0.057 | |
| Total number of reflux episodes/hour | Sedation | 0.69 ( 0.15, 1.23) | 0.014 |
| No Sedation | 1.14 ( 0.57, 1.71) | <0.001 | |
| Patients aged ≥1: | |||
|---|---|---|---|
| Outcome | Sedation Group | Mean difference | p-value |
| % Time pH < 4 | Sedation | −0.56 (−2.42, 1.29) | 0.554 |
| No Sedation | 1.90 (−0.09, 3.89) | 0.065 | |
| Number of acid reflux episodes/hour | Sedation | 0.19 (−0.23, 0.62) | 0.376 |
| No Sedation | 0.85 ( 0.40, 1.30) | <0.001 | |
| Number of non-acid reflux episodes/hour | Sedation | 0.58 ( 0.15, 1.01) | 0.011 |
| No Sedation | 0.67 ( 0.21, 1.13) | 0.006 | |
| Total number of reflux episodes/hour | Sedation | 0.80 ( 0.20, 1.40) | 0.011 |
| No Sedation | 1.52 ( 0.87, 2.16) | <0.001 | |
Figure 1.
Mean difference (±95% CI) in pH Impedance between the 1st 4 hours and the abridged data (for number of non-acid reflux episodes/hour and total number of reflux episodes per hour), in patients aged ≥1 year, controlling for opioids, ondansetron, BMI, PPI and esophagitis. p-values are for the comparison of the difference versus a null hypothesis of no difference.
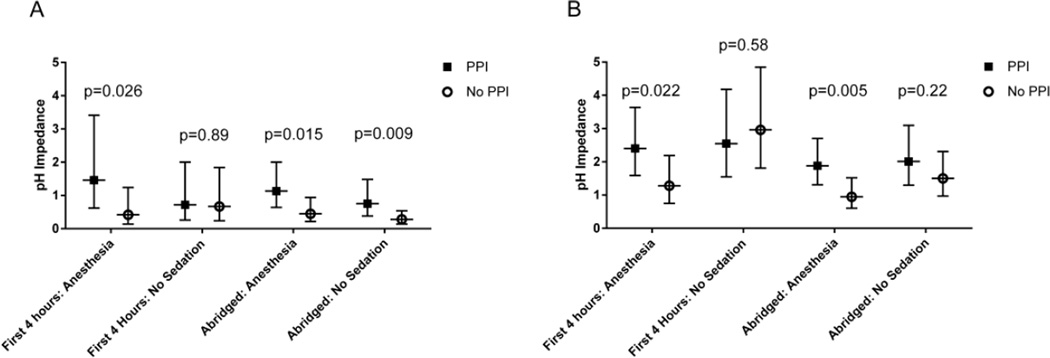
Proton pump inhibitor (PPI) use was present in all groups varying between 50% in the no sedation and ≥1 year olds to 82% in the no sedation <1 year olds (Table 1). There were significant differences between PPI and no PPI use within all 3 datasets (full, first 4 hours and abridged) for non-acid reflux per hour in one or both sedation groups, and for total reflux per hour in the anesthesia group, both overall and in patients aged ≥1. These differences remained significant after allowing for the other covariates (Figure 2). Generally outcomes (non-acidic reflux per hour and total reflux) were higher with PPI (supplementary Table 3, http://links.lww.com/MPG/A590).
Figure 2.
Geometric mean pH Impedance (±95% CI) in patients aged ≥1 year, with and without PPI by sedation group, controlling for opioids, ondansetron, BMI, and esophagitis, (A) number of non-acid reflux episodes/hours and (B) total number of reflux episodes/hour. P-values are for comparisons between PPI and no PPI groups.
Families were asked to document the position of the children with position buttons on the monitor. While there were no significant differences when the full studies were compared between anesthesia and the no sedation group, there was increased time in the recumbent position in the first 4 hours for the anesthesia group, with 49% of the time spent recumbent compared to 18% in the no sedation group (p<0.001).
Discussion
To our knowledge, this is the first study analyzing the effects of anesthesia on gastroesophageal reflux as measured by the pH-multichannel intraluminal impedance (pH impedance) monitoring device. Our study shows: 1) Differences in acid reflux per hour exist between patients receiving anesthesia and those without sedation in univariate evaluation for both age groups. However when controlling for opioids, ondansetron, BMI, PPI, esophagitis and age, these differences were no longer statistically significant overall or within each age group. 2) Univariate analysis for the difference between the first 4 hours and the abridged time period showed increased acid reflux per hour, non-acid reflux per hour and total reflux per hour both overall and in ≥1 year olds. This difference remained statistically significant for the ≥ 1 year old group without sedation in multiple regression analysis for non-acid reflux per hour and total reflux per hour. The first 4 hour dataset had significantly more reflux events than in the abridged dataset for these outcomes in the no sedation group. 3) Patients using PPI had more non-acid reflux events per hour and total reflux events per hour, notably in patients aged ≥1 and undergoing anesthesia. Percent time in which pH was <4 did not appear to be significantly different between sedation groups or with and without PPI.
The study by Chawla on the Bravo pH monitoring system identified an increase in acidic reflux in the first six hours following anesthesia.12 The authors questioned the role that propofol, NPO status, endoscopy with air insufflation, decreased oral intake and decreased activity played in these differences. There is some literature on the effects of propofol on LES pressures;13 however, no correlation to reflux has been made. Previous studies on the effects of anesthesia on GER are very limited and are mainly in the veterinary literature.
Similar to the Bravo probe study,12 our study found increased acid refluxes per hour and total reflux per hour following placement of the probe. However, we also found a significant change over time in the non-acid refluxes per hour in the no sedation group which was not statistically significant in the anesthesia group, contrary to what we had hypothesized. The no sedation group had higher non-acid reflux per hour and total reflux per hour between the first 4 hours and the abridged study in patients aged ≥1 year, controlling for opioids, ondansetron, BMI, PPI and esophagitis. We hypothesize this difference is due to shorter NPO times, increased activity, earlier oral intake after pH probe placement, and decreased recumbent time. We question the role of the placement of the pH probe itself in the increased reflux events. We also question the role of anesthesia, prolonged NPO times, decreased oral intake and decreased activity during recovery on dampening reflux in those in which the probe was placed during anesthesia.
Our study also showed increase in reflux in children taking PPI, regardless of sedation. In the <1 year old group no differences were found by multiple regression, but there were significant differences between PPI and no PPI use within the full dataset, the first 4 hour dataset and the abridged dataset for non-acid reflux per hour in one or both sedation groups, and for total reflux per hour in the sedation group, in patients aged ≥1. Subjects taking PPI had more non-acid reflux per hour and total reflux per hour. This group of patients likely had more reflux causing symptoms resulting in their PPI prescription. It is also possible that the children on PPI did not take their medication prior to the placement of the probe resulting in acid hypersecretion that is later controlled following PPI dosing.
A larger prospective study may be able to better control for some of these factors and better isolate the role of anesthesia on GER. This study was limited by its retrospective nature and by the multiple anesthetics used during the anesthesia exposures. It is possible that each medication affects reflux and gastric motility differently, although previous studies have not shown this. We were also limited by our data on patient positioning, which we found to be poorly reported. Position and activity, to include sleep, clearly impact reflux and our study cannot fully evaluate this. Specific type of meal composition may also greatly impact reflux which was not available in our data that simply identified a meal. Future prospective studies could better capture this data on position, activity and dietary intake during the study. An additional limitation was the small number of patients (n=22) in the subgroup analyses of patients aged <1 and there may have been insufficient power to detect differences. The <1 year old group appears to have different physiology which warrants independent study.
Conclusion
When comparing the anesthesia and no sedation groups directly there was no difference in outcome when taking covariates into account. However, the no sedation group did have higher non-acid reflux measured by intraluminal pH in the first four hours compared to the remainder of the study, which remained statistically significant when controlling for opioids, ondansetron, PPI use, BMI, age and presence of esophagitis. Limited differences were seen in the <1 year old group with no differences between sedation group or outcome over time by multiple regression. Based on the results of this study, there may be no need to eliminate the data collected immediately after placement of the probe in children <1 year of age, but in those ≥1, there may be a greater number of reflux events in the first 4 hours compared to the later time period in probes placed without sedation. The first 4 hours should be carefully evaluated in patients ≥1 year of age. The finding of increased reflux in the early portion of impedance probe testing in the no sedation group suggests that there may be additional factors that impact the interpretation of these studies. Further study is therefore needed to provide normative data for the first 4 hours versus the abridged data, separately for those undergoing sedation versus unsedated patients, in order to validate the findings from this study and to better understand the mechanism of gastroesophageal reflux. Future studies may help to identify the appropriate time to start data collection in both populations.
Supplementary Material
What is known
Lower esophageal sphincter pressure is decreased by anesthesia
Gastroesophageal reflux increases following endoscopy as measured by BRAVO pH measuring device
Veterinary studies show increases in gastroesophageal reflux following anesthesia
New findings
Increased non-acid and total reflux in the first 4 hours following pH probe placement in non-sedated children older than 1 year of age.
No significant difference in reflux parameters between anesthesia and non-sedated patients when controlling for age, BMI, presence of esophagitis, and exposure to opioids, Ondansetron, and Proton Pump Inhibitors (PPI).
Acknowledgments
Financial support: No funding was required for this research.
Abbreviations
- pH Impedance
PH-multichannel intraluminal Impedance
- GER
Gastroesophageal reflux
- GERD
gastroesophageal reflux disease
- EGD
esophagogastroduodenoscopy
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jpgn.org).
Conflicts of Interest: None
References
- 1.Mousa MM, Rosen R, Woodley FW, et al. Esophageal Impedance monitoring for gastroesophageal reflux. J Pediatr Gastroenterol Nutr. 2011;52:129–139. doi: 10.1097/MPG.0b013e3181ffde67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wenzl TG, Benninga MA, Loots CM, et al. Indications, methodology, and interpretation of combined esophageal Impedance-pH monitoring in children: ESPGHAN EURO-PIG standard protocol. J PediatrGastroenterol Nutr. 2012;55:230–234. doi: 10.1097/MPG.0b013e3182592b65. [DOI] [PubMed] [Google Scholar]
- 3.Sullivan JS, Sundaram SS. Gastroesophageal reflux. Pediatr Rev. 2012;33:243–253. doi: 10.1542/pir.33-6-243. [DOI] [PubMed] [Google Scholar]
- 4.Schurizek BA. The effects of general anaesthesia on antroduodenal motility, gastric pH and gastric emptying in man. Dan Med Bull. 1991;38:347–365. [PubMed] [Google Scholar]
- 5.Mushambi MC, Rowbotham DJ, Bailey SM. Gastric emptying after minor gynaecological surgery. The effect of anesthetic technique. Anaesthesia. 1992;47:297–299. doi: 10.1111/j.1365-2044.1992.tb02167.x. [DOI] [PubMed] [Google Scholar]
- 6.Lombardo L, Ruggia O, Crocella L, et al. Epidural plus general anesthesia vs general anesthesia alone for elective aortic surgery: effects on gastric electrical activity and serum gastrin secretion. Minerva Anestesiol. 2009;75:109–115. [PubMed] [Google Scholar]
- 7.Waldén J, Thörn SE, Lövqvist A, et al. The effect of anesthestic technique on early postoperative gastric emptying: comparison of propofol-remifentanil and opiod-free sevofluorane anesthesia. J Anesth. 2006;20:261–267. doi: 10.1007/s00540-006-0436-3. [DOI] [PubMed] [Google Scholar]
- 8.Hammas B, Thörn SE, Wattwil M. Propofol and gastric effects of morphine. Acta Anaesthesiol Scand. 2001;45:1023–1027. doi: 10.1034/j.1399-6576.2001.450816.x. [DOI] [PubMed] [Google Scholar]
- 9.Resnick J, Greenwald DA, Brandt LJ. Delayed gastric emptying and postoperative ileus after nongastric abdominal surgery: part I. Am J Gastroenterol. 1997;92:751–762. [PubMed] [Google Scholar]
- 10.Galatos AD, Savas I, Prassinos NN, et al. Gastro-oesophageal reflux during thiopentone or propofol anaesthesia in the cat. J Vet Med A Physiol Pathol Clin Med. 2001;48:287–294. doi: 10.1046/j.1439-0442.2001.00357.x. [DOI] [PubMed] [Google Scholar]
- 11.Favarato ES, de Souza MV, Costa PR, et al. Ambulatory esophageal pHmetry in healthy dogs with and without the influence of general anesthesia. Vet Res Commun. 2011;35:271–282. doi: 10.1007/s11259-011-9471-0. [DOI] [PubMed] [Google Scholar]
- 12.Chawla A, Girda E, Walker G, et al. Effect of propofol on acid reflux measured with the Bravo pH monitoring system. ISRN Gastroenterol. 2013;2013:605931. doi: 10.1155/2013/605931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kohjitani A, Shirakawa J, Satoh E, et al. Effects of sevoflurane and enflurane on lower esophageal sphincter pressure and gastroesophageal reflux pressure gradient in children. J Anesth. 1999;13:1–7. doi: 10.1007/s005400050013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.