Abstract
Background
A TKA is the most effective and cost-effective surgical option for moderate to severe osteoarthritis (OA) of the knee. Yet, black patients are less willing to undergo knee replacement surgery than white patients. Decision aids help people understand treatment options and consider the personal importance of possible benefits and harms of treatments, including TKA.
Questions/purposes
We asked: (1) Does a patient-centered intervention consisting of a decision aid for knee OA and motivational interviewing improve the proportion of referrals of blacks with knee OA to orthopaedic surgery? (2) Does the intervention increase patients’ willingness to undergo TKA?
Methods
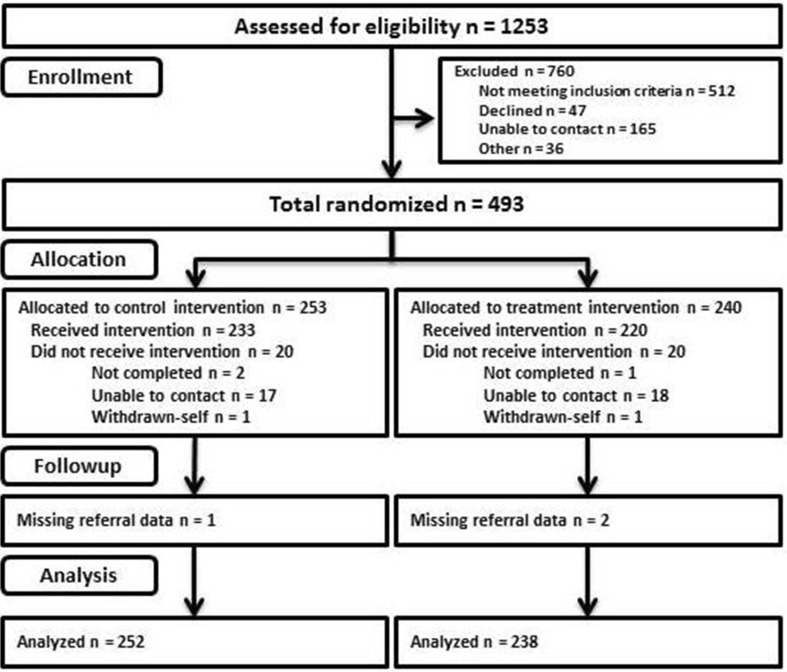
Adults who self-identified as black who were at least 50 years old with moderate to severe knee OA were enrolled from urban primary care clinics in a two-group randomized, controlled trial. A total of 1253 patients were screened for eligibility, and 760 were excluded for not meeting inclusion criteria, declining to participate, or other reasons. Four hundred ninety-three patients were randomized and completed the intervention; three had missing referral data at followup. The mean age of the patients was 61 years, and 51% were women. The majority had an annual household income less than USD 15,000. Participants in the treatment group were shown a decision-aid video and had a brief session with a trained counselor in motivational interviewing. Participants in the control group received an educational booklet about OA that did not mention joint replacement. The two groups had comparable demographic and socioeconomic characteristics. The primary outcome was referral to orthopaedic surgery 12 months after treatment exposure. Receipt of referral was defined as the receipt of a recommendation or prescription from a primary care provider for orthopaedic evaluation. The secondary outcome was change in patient willingness to undergo TKA based on patient self-report.
Results
The odds of receiving a referral to orthopaedic surgery did not differ between the two study groups (36%, 90 of 253 of the control group; 32%, 76 of 240 of the treatment group; odds ratio [OR], 0.81; 95% CI, 0.56–1.18; p = 0.277). At 2 weeks followup, there was no difference between the treatment and the control groups in terms of increased willingness to consider TKA relative to baseline (34%, 67 of 200 patients in the treatment group; 33%, 68 of 208 patients in the control group; OR, 1.06; p = 0.779). At 12 months followup, the percent increase in willingness to undergo TKA still did not differ between patients in the treatment and control groups (29%, 49 of 174 in the treatment group; 27%, 51 of 191 in the control group; OR, 1.10; p = 0.679).
Conclusion
A combination decision aid and motivational interviewing strategy was no better than an educational pamphlet in improving patients’ preferences toward joint replacement surgery for knee OA. The type of intervention treatment also did not affect access to surgical evaluation. Other tools that target patient knowledge, beliefs, and attitudes regarding surgical treatments for OA may be further developed and tested in the future.
Level of Evidence
Level I, therapeutic study.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-016-4834-z) contains supplementary material, which is available to authorized users.
Introduction
Although a TKA is highly effective in treating advanced knee osteoarthritis (OA), it is underused by black patients compared with white patients [9, 21, 30, 39]. Racial disparities in patients’ surgical and medical management cannot be attributed to prevalence or severity of OA [2, 10]. The burden of OA also is greater in the black population than in the white population; black race has been associated with lower quality of life [16] and higher likelihood of disability [35] for those with OA. Access to care also might determine use of surgical services. However, racial differences in undergoing TKA persist even after controlling for health insurance status [20, 31].
An important factor that may help explain racial disparities in OA care involves patient preferences. The decision of a primary care physician to refer a patient to a specialist is influenced by a mix of patient, physician, and healthcare system structural characteristics [11]. However, patient characteristics are most likely to affect this referral decision [11]. Depending on the extent to which racial or ethnic minority patients convey reluctance to accept physicians’ recommendations, patients’ preferences can contribute to health disparities. Several studies have shown that black patients have a greater aversion toward joint replacement surgery than white patients [1, 7, 18, 19, 31].
Decision aids promote shared decision-making between providers and patients. They improve patients’ knowledge regarding treatment options, reduce decisional conflict, and stimulate patients to take an active role in decision-making [5, 23, 27]. They increase accurate perceptions of treatment risk and improve congruence between a patient’s values and the chosen option [27]. They are tools designed to prepare people to participate in making specific and deliberate choices among treatment options in ways that they prefer. They also have been shown to increase use of evidence-based treatments [27]. In a pilot study [37], a decision aid for knee OA and a personalized arthritis report immediately improved willingness for TKA among black veterans.
Similarly, motivational interviewing is a counseling technique that relies on identifying and mobilizing patients’ values and goals to stimulate behavior change [4, 28, 29]. This technique is designed to find a constructive way to overcome the challenges that arise when a health professional ventures into a patient’s motivation for change [26]. It is about arranging conversations so that patients talk themselves into change, based on their own values and interests [26]. Pairing the decision aid with motivational interviewing allows presentation of various OA treatment options, determination of patient’s current values and goals, and guidance of a decision congruent with these goals and values. In a previous study of black men who were veterans who had knee OA, a combination of a decision aid and motivational interviewing increased the patients’ willingness to undergo surgery, at 1 month followup, and the number of referrals to an orthopaedic clinic [17]. The generalizability of these results to other study populations (perhaps including women patients and nonveterans) is unknown.
In the current study, we asked: (1) Does a patient-targeted intervention consisting of a decision aid and motivational interviewing improve the proportion of referrals of black patients with knee OA to orthopaedic surgery? (2) Does the intervention increase patients’ willingness to undergo TKA? We hypothesized that a decision aid combined with a brief motivational interviewing intervention would increase the likelihood of patients receiving a referral to orthopaedic surgery and their willingness to consider TKA, after 12 months.
Patients and Methods
Design Overview
This randomized, controlled trial compared the effects of a knee OA decision aid and motivational interviewing (treatment) with receipt of an OA education booklet (control) in patients with moderate-to-severe knee OA (ClinicalTrials.gov#: NCT02413411). Participants were randomly assigned at baseline to either the intervention or the control group. The study protocols were approved by the institutional review boards of the University of Pennsylvania, Philadelphia VA Medical Center, and the University of Pittsburgh. All participants provided informed consent before participation.
Participants
Participants were recruited between April 2008 and May 2013. Potentially eligible participants were identified by screening medical records of patients in primary care clinics. They also were identified via existing research and clinic registries. Additional participants were sought via local advertisements. All were assessed for study eligibility by telephone interview. Those without a recent knee radiograph on file had radiographs ordered and done. Eligible participants were those who self-identified as black, were 50 years or older, had chronic and frequent knee pain, a WOMAC score of 39 or greater, and had radiographic evidence of knee OA. Only those who previously self-identified themselves as black/African-American and at least 50 years old based on medical records or registries were screened, along with those who responded to advertisements that asked for potentially eligible participants based on the study eligibility criteria.
Exclusion criteria were prior history of joint replacement, a diagnosis of terminal illness, diagnosis of inflammatory arthritis (eg, rheumatoid arthritis), contraindications to joint replacement surgery (eg, lower extremity paralysis), had a prosthetic leg, cognitive impairment, and did not have a telephone.
Randomization and Intervention
Participants were randomized to one of the two study arms using a computer-generated random assignment. The computer-generated randomization result was sent to the study coordinator via email before the scheduled intervention session. Owing to the nature of the intervention, participants could not have been blinded to the study arm they were assigned to. Primary care providers were blinded from the study arm participants were assigned to.
Participants randomly assigned to the treatment group received a two-phase series of a patient-centered educational intervention [17]. First, participants in the treatment group watched a 40-minute decision-aid video. Developed by the Foundation for Informed Medical Decision-Making (Boston, MA, USA), the video discussed the benefits and risks of various pharmacologic (eg, medications, injections, complementary therapy) and surgical treatment options for knee OA. It also covered clinical indications for joint replacement, anticipated clinical course during surgery, and postoperative expectations. It described the potential complications of undergoing joint replacement surgery and the anticipated lifespan of a prosthesis. Second, participants in the treatment group underwent counseling regarding TKA using a motivational interviewing strategy [25]. Participants were asked about their thoughts regarding TKA, and their goals and values regarding their arthritis (Appendix 1. Supplemental material is available with the online version of CORR®). Information regarding TKA and how to engage the patients’ primary care providers in discussing their knee pain also were provided. Trained, certified interventionists in motivational interviewing conducted each face-to-face counseling session which lasted approximately 30 minutes.
Participants randomly assigned to the control group received an educational booklet, developed by the NIH National Institute of Arthritis and Musculoskeletal and Skin Diseases (Bethesda, MD, USA), that summarized how to live with knee OA. It did not specifically mention joint replacement as a treatment option but provided examples of exercises one could do to improve knee pain and stiffness. Many physicians provide educational materials to patients when considering various treatments for OA; therefore, it would be appropriate to compare the intervention treatment with this clinically relevant alternative [12].
Outcome Measures
Participants completed a baseline questionnaire before beginning intervention. Followup questionnaires were conducted by telephone at 2 weeks, 3 months, and 12 months after the intervention. Assessors of outcomes were blinded to which study arm the patients were assigned.
The primary outcome measure was receipt of a referral to orthopaedic surgery based on a patient’s self-report at the 12-month postintervention followup. For study purposes, we defined a referral as a primary care provider’s recommendation or prescription for an orthopaedic evaluation (in this case) within 12 months of randomization. This outcome variable was confirmed by electronic chart review.
The secondary outcome measure was change in patient preference regarding TKA. At baseline and at the 2-week, 3-month, and 12-month followups, participants were asked: “If your knee pain were ever to get severe, would you be willing to have surgery to replace your knee if your doctor recommended it?” [15]. Response options ranged from “definitely not willing” to “definitely willing” in a five-category ordinal response scale. Willingness to undergo TKA has been shown to be the primary predictor of receiving a referral to an orthopaedic surgeon and actually receiving a TKA [13, 14].
Covariates
Age, sex, education, employment, income, marital status, and living situation were gathered at baseline. Severity of the knee OA was assessed using the WOMAC index [3]. Summary scores range from 0 to 100, where higher scores indicate increased pain, stiffness, and functional limitations. Both subscales of the Arthritis Self-Efficacy Scale also were measured [24]. The pain subscale measures patients’ confidence that they can manage arthritis-related pain (range, 5–50), and the function subscale measures patients’ confidence that they can perform specific daily activities (range, 9–90). Higher scores suggest greater self-efficacy. Medical comorbidity was assessed using an interviewer-based modification of the Charlson comorbidity index (range, 0–17) [8, 22]. Quality of life was assessed using the SF-12® survey, version 2, from which the physical and mental component scores were calculated (range, 0–100) [36]. Higher scores indicate better health.
Sample Size and Power
The power analysis for patient treatment preference was based on binary logistic regression. With a total of 400 participants to be randomized, there was 80% power to detect absolute differences of at least 15% in patient preference between patients in the two groups. This number of patients also allowed detection of a 10% difference in the proportion of referrals for surgery between the two study groups.
Study Population
A total of 1253 subjects were identified as potential candidates for the study (Fig. 1). In all, 493 black patients with chronic, frequent knee pain were randomly assigned to either the control (n = 253) or treatment (n = 240) group. Among the randomly assigned participants, 233 (92.1%) in the control group and 220 (91.7%) in the treatment group actually received the allocated intervention. No meaningful between-group differences were found for baseline age, sex, education, employment status, marital status, living situation, household income, OA disease severity by WOMAC, arthritis self-efficacy scores, comorbidities, and SF-12® quality-of-life scores (Table 1).
Fig. 1.
The flow diagram shows the steps that were used for patient selection and group analysis.
Table 1.
Baseline demographic and clinical characteristics of the study sample*
| Variable | Control (n = 253) |
Treatment (n = 240) |
p value† |
|---|---|---|---|
| Recruitment site, number (%) | 0.696 | ||
| University of Pennsylvania | 135 (53) | 131 (55) | |
| University of Pittsburgh | 16 (6) | 19 (8) | |
| Philadelphia Veterans Administration | 102 (40) | 90 (38) | |
| Demographic characteristics‡ | |||
| Age, years | 61.14 ± 7.86 | 62.02 ± 8.09 | 0.224 |
| Sex, number of (%) men | 124 (49) | 118 (49) | 0.973 |
| Number (%) with less than high school education | 53 (21) | 50 (21) | 0.975 |
| Number (%) currently working | 56 (22) | 48 (20) | 0.562 |
| Number (%) currently married | 61 (24) | 69 (29) | 0.242 |
| Number (%) living alone | 111 (44) | 112 (47) | 0.560 |
| Number (%) with annual household income less than USD 15,000 | 125 (54) | 109 (49) | 0.357 |
| Clinical characteristics | |||
| WOMAC | 59.51 ± 13.21 | 58.69 ± 14.16 | 0.510 |
| Arthritis Self-Efficacy pain | 25.31 ± 10.28 | 26.43 ± 10.19 | 0.231 |
| Arthritis Self-Efficacy function | 52.21 ± 18.25 | 55.28 ± 17.99 | 0.061 |
| Charlson comorbidity index | 3.33 ± 2.22 | 3.07 ± 2.05 | 0.182 |
| SF-12® Physical Component | 31.00 ± 9.79 | 32.58 ± 9.79 | 0.085 |
| SF-12® Mental Component | 45.96 ± 8.99 | 46.19 ± 8.47 | 0.775 |
| Number (%) willing to undergo TKA§ | 170 (67) | 164 (69) | 0.634 |
*Except where indicated otherwise, values are mean ± SD; †t-tests for continuous variables, chi-square tests for categorical variables; ‡there were slight variations in the number of patients who provided information for some of the demographic characteristics. Most had two or fewer patients missing data. The income variable had the highest number of patients with missing data (39 subjects did not provide responses); §willingness to undergo TKA = willing if participant response was “probably willing” or “definitely willing”.
Statistical Analysis
Demographic and clinical characteristics were compared by intervention group using t-tests for continuous variables and chi-square tests for categorical variables.
Change in willingness to undergo TKA since baseline for each followup (ie, 2-week, 3-month, and 12-month postintervention) was assessed by comparing the proportion of participants who had increased willingness versus no change or decreased willingness. Change in willingness was calculated by subtracting a participant’s coded score before the intervention from the postintervention score. It then was dichotomized as increased willingness versus no change or decreased willingness. Chi-square tests were performed using available data from patients who completed each followup assessment. To analyze the change in willingness of different patient groups (for descriptive purposes), chi-square tests were repeated after stratifying patients by recruitment site and sex.
Referral to orthopaedics within 12 months after the intervention was modeled using logistic regression. The initial model contained a treatment (vs control) group as the only predictor. The dichotomized baseline willingness and key covariates determined a priori then were added to the initial model: age, sex, education, and WOMAC index score. Arthritis Self-Efficacy scores, Charlson comorbidity index score, and SF-12® Physical and Mental Component scores subsequently were added. To further analyze the effect of the intervention by different patient groups, the proportion of patients who received a referral to orthopaedics by recruitment site and sex were compared using chi-square tests.
On analyzing the effect of the intervention on the proportion of referrals, we included only the 490 participants with nonmissing referral outcomes. This analysis assumes that outcome data are missing completely at random. Although a sensitivity analysis usually would be needed to explore the effect of departures from this assumption, with less than 1% missing data, this was not warranted since even the most biased imputation of referral outcomes would not alter our conclusions.
Results
Orthopaedic Referral
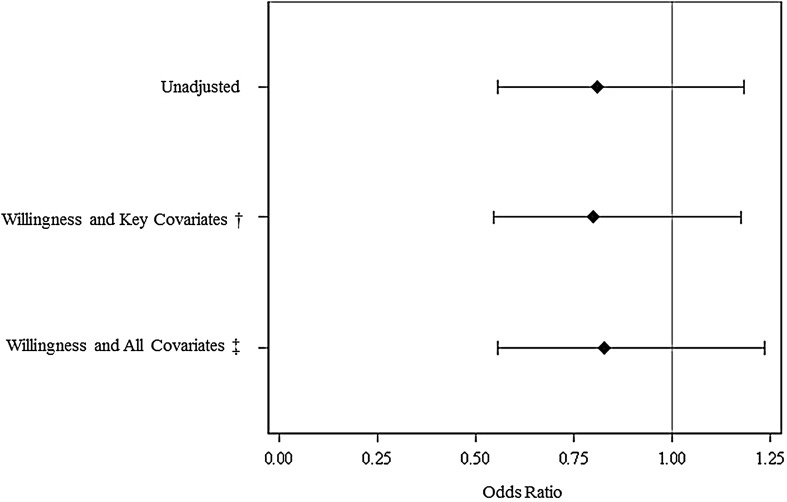
At 12 months, 90 (36%) patients in the control group and 76 (32%) in the treatment group were referred to an orthopaedic surgeon (odds ratio [OR], 0.81; 95% CI, 0.56–1.18; p = 0.277). The proportion of patients who received a referral did not differ by treatment group when stratified by recruitment site or sex (Table 2). When adjusted for baseline willingness to consider TKA, age, sex, education, and WOMAC total score, there was no difference in receiving a referral between the two groups of patients (OR, 0.80; 95% CI, 0.55–1.18; p = 0.257) (Fig. 2). When further adjusted for Arthritis Self-Efficacy score, Charlson comorbidity score, SF-12® physical health, and SF-12® mental health scores, difference in the proportion of referrals between the two groups still was not different (OR, 0.83; 95% CI, 0.56–1.24; p = 0.357).
Table 2.
Patients referred to an orthopaedic surgeon at 12 months
| Variable | Control group Number (%) |
Treatment group Number (%) |
p value* |
|---|---|---|---|
| Recruitment site | |||
| University Clinic | 48 (32) | 42 (28) | 0.496 |
| Veterans’Administration Clinic | 42 (41) | 34 (38) | 0.631 |
| Sex | |||
| Male | 51 (41) | 43 (37) | 0.455 |
| Female | 39 (30) | 33 (27) | 0.606 |
*chi-square tests.
Fig. 2.
The graph shows the odds ratios of referral to an orthopaedic surgeon at 12 months postintervention in unadjusted and adjusted models. *Unadjusted and adjusted odds ratios (95% CI) with the control group as the reference group; †key covariates: age, sex, education, WOMAC; ‡all covariates: key covariates plus Arthritis Self-Efficacy Function score, Charlson comorbidity score, and SF-12 Physical and Mental Component scores.
Willingness to Undergo Surgery
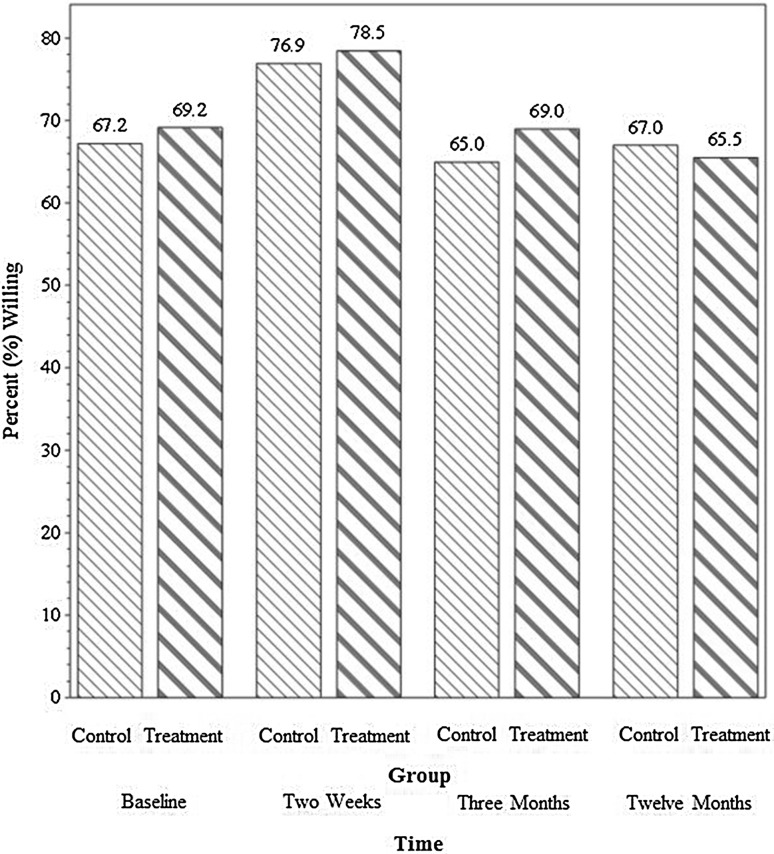
At 2 weeks followup, there was no difference between the treatment and the control groups in terms of increased willingness to consider TKA relative to baseline (34% [67 of 200] of patients in the treatment group and 33% in the control group [68 of 208], respectively [OR, 1.06; 95% CI, 0.70–1.60; p = 0.779]).
A higher proportion of patients also were willing to consider the procedure at the 2-week followup than at baseline in the control (77% [160 of 208] and 67% [170 of 253]; OR, 1.63; 95% CI, 1.07–2.47; p = 0.022) and treatment (79% [157 of 200] and 69% [164 of 237]; OR, 1.63; 95% CI, 1.05–2.51; p = 0.028) groups (Fig. 3). Increase in willingness to undergo TKA also did not differ between the two groups at 3 months or 12 months (Table 3).
Fig. 3.
The bar graph shows the observed proportions of patients willing to consider TKA across groups and times. The number of patients who completed the willingness question was different each time: at baseline, 490; at 2 weeks, 408; at 3 months, 400; and at 12 months, 365.
Table 3.
Change in willingness by treatment group*
| Variable | Control group | Treatment group | OR (95% CI) |
p value† |
|---|---|---|---|---|
| All patients | ||||
| Number (%) increased at 2 weeks | 68/208 (33) | 67/200 (34) | 1.06 (0.70–1.60) |
0.779 |
| Number (%) increased at 3 months | 52/203 (26) | 64/197 (33) | 1.43 (0.93–2.21) |
0.106 |
| Number (%) increased at 12 months | 51/191 (27) | 49/174 (29) | 1.10 (0.70–1.75) |
0.678 |
| University clinic patients | ||||
| Number (%) increased at 2 weeks | 34/114 (30) | 41/118 (35) | 1.29 (0.74–2.24) |
0.372 |
| Number (%) increased at 3 months | 27/109 (25) | 43/116 (37) | 1.84 (1.03–3.27) |
0.037 |
| Number (%) increased at 12 months | 31/108 (29) | 35/104 (34) | 1.30 (0.72–2.33) |
0.381 |
| Veterans Administration clinic patients | ||||
| Number (%) increased at 2 weeks | 34/94 (36) | 26/82 (32) | 0.83 (0.45–1.56) |
0.572 |
| Number (%) increased at 3 months | 25/94 (27) | 21/81 (26) | 0.98 (0.50–1.93) |
0.959 |
| Number (%) increased at 12 months | 20/83 (24) | 14/70 (20) | 0.80 (0.37–1.74) |
0.575 |
| Male patients | ||||
| Number (%) increased at 2 weeks | 36/109 (33) | 33/102 (33) | 0.98 (0.55–1.75) |
0.956 |
| Number (%) increased at 3 months | 27/107 (25) | 28/103 (27) | 1.12 (0.61–2.08) |
0.716 |
| Number (%) increased at 12 months | 23/99 (23) | 18/89 (20) | 0.85 (0.42–1.71) |
0.647 |
| Female patients | ||||
| Number (%) increased at 2 weeks | 32/99 (32) | 34/98 (35) | 1.15 (0.63–2.08) |
0.648 |
| Number (%) increased at 3 months | 25/96 (26) | 36/94 (38) | 1.83 (0.98–3.39) |
0.055 |
| Number (%) increased at 12 months | 28/92 (30) | 31/85 (37) | 1.36 (0.73–2.55) |
0.334 |
*Change in willingness was assessed relative to baseline; dichotomized as increased willingness versus no change or decreased willingness. The number of patients who completed followup was different at each time; OR = odds ration; †chi-square tests.
Among patients recruited at a university clinic, the increase in willingness at the 3-month followup was greater for patients in the treatment group than for patients in the control group (37% [43 of 116] vs 25% [27 of 109]; OR, 1.84; 95% CI, 1.03–3.27; p = 0.038). At the 12-month followup, there was no difference between the groups (34% [35 of 104] vs 29% [31 of 108]; OR, 1.30; 95% CI, 0.72–2.33; p = 0.383). Change in willingness among patients from the VA clinic also did not differ by treatment group at the 2-week, 3-month, and 12-month followups (Table 3). Among women, increase in willingness at the 3-month followup was not different among those in the treatment group or in the control group (38% [36 of 94] vs 26% [25 of 96]; OR, 1.83; 95% CI, 0.98–3.39; p = 0.056). In general, change in willingness did not differ by treatment group at all followup times when men and women were analyzed separately (Table 3).
Discussion
Several studies have documented racial variations in the use of TKA, with black patients having decreased likelihood of undergoing TKA than white patients [9, 21, 39]. Studies also have shown that racial differences in patient preference contribute to racial variations in the use of total joint replacement [13, 18, 19, 31]. How to best educate black patients about joint replacement as a viable treatment option, determine if undergoing the surgical procedure is consistent with their goals and values, and improve their access to surgical evaluation is unclear. This randomized, controlled study examined the effect of an educational intervention (decision aid with counseling using motivational interviewing) on black patients with knee OA receiving a referral to orthopaedic surgery. Although some study participants increased their willingness to undergo surgery, there were no differences between the treatment and control groups with respect to the number of referrals to orthopaedic surgery within 12 months.
There are a few limitations to consider in interpreting our results. Race was based on patient self-report, and there may be a discrepancy between self-identification and observer-reported race. Yet, some consider self-reported race/ethnicity a better measure [38]. We did not evaluate nonsurgical treatments our study participants may have received. Proportions of patients using these OA treatments might have differed by study group, potentially confounding the effects of the intervention on patient treatment preferences. Race-related demographic and socioeconomic characteristics of patients also might have differed by study group. Nonetheless, the randomization process helped ensure that characteristics that could confound our results were equally distributed. The study design also could be a potential threat to the study’s internal validity. As patients’ preferences were elicited at the 2-week and 3-month followups, these actions might have influenced receipt of referrals by patients in both study arms. As a result, the effect of the treatment might have been negated. However, there is no compelling reason to believe that merely asking people about their preferences would significantly change their preferences. We also followed patients for only 12 months. Given the long-term trajectory of knee OA, it is conceivable a longer followup might have resulted in a higher number of referrals among those who received the intervention. Finally, our intervention was brief and occurred only once. It is possible that a more-frequent intervention and better access to a decision aid for patients could result in greater improvement in patient preference toward joint replacement.
As the intervention treatment did not improve patients’ willingness to consider TKA among those who completed followup, it was not surprising to find that the intervention also did not lead to an increased number of referrals for orthopaedic surgery. In a study of patients with knee and hip OA at a VA orthopaedic clinic, patient preferences had the most substantial effect on receiving a recommendation for total joint replacement [13]. The decreased likelihood of black patients receiving a recommendation for joint replacement compared with white patients in that study was largely explained by the lower preference for joint replacement among blacks. Moreover, in a study of Canadian patients with OA, patient preference for joint replacement was the strongest predictor of time to first arthroplasty [14].
Regardless, receiving a referral to a surgical specialist is likely dependent on the patient’s treatment preferences, the primary care provider’s management style, and the characteristics of the healthcare system. Evidence suggests that race may affect providers’ conscious and unconscious beliefs about and expectations from patients [33, 34]. In turn, these beliefs might lead to biases in providers’ interpretation of symptoms and treatment decisions [6, 32, 33]. In many institutions, a primary care provider usually initiates the surgical referral for patients. Some patients could self-refer themselves to orthopaedic surgery. Moreover, limited access to healthcare (eg, limited medical insurance benefits) could discourage a patient from wanting a TKA or dissuade a primary care provider from giving a referral to a surgical specialist. In short, physician-level and healthcare-level factors might play a part regarding whether a surgical referral is made, and our proposed intervention targeted only patient attitudes.
The decision aid provided evidence-based information regarding knee OA and the different treatment options for the disease. The motivational interviewing strategy assessed patient values and goals to help determine if surgery is the most appropriate treatment option. It also helped patients tackle their views about TKA and taught them how to engage providers in addressing their arthritis symptoms. In a small study of veterans [37], the combination of the Foundation for Informed Medical Decision-Making decision aid for OA and personalized arthritis report immediately improved willingness by black veterans to consider TKA, but did not increase willingness among white veterans. The intervention also eliminated racial disparities in expectations regarding TKA outcomes. In a previous study of only patients from VA clinics [17], we found that an intervention consisting of a decision aid and motivational interviewing increased willingness to consider TKA.
There may be a few different reasons for the disparate outcomes related to treatment preferences between the current study and the VA studies. There were patients with missing willingness data at different times. Attrition bias could have affected our results. Differences in patient population groups studied also might explain the varied results. The previous investigations studied only veterans with knee OA [17, 37]. The current study sample consisted of mostly patients who received care in an academic center, along with veterans. When stratified by recruitment site, the intervention improved willingness of patients from university clinics, yet it did not last beyond 3 months. This improvement in willingness among university clinic patients at 3 months might have been a type 1 error, a spurious finding. Moreover, nearly all participants in the other studies were men, whereas 51% of randomized participants in the current study were women. However, in this study, change in willingness to undergo TKA did not change by treatment group regardless of the sex of the patient. Socioeconomic status profile, along with beliefs, knowledge, and attitudes regarding TKA and knee OA also might differ between our study population and the VA study populations. Such study group differences could contribute to varying responses to similar interventions. Finally, the other studies were conducted at earlier times. General attitudes and beliefs regarding TKA might have changed since then.
In this large study of black patients with knee OA who were potential candidates for TKA, an educational intervention consisting of a decision aid supplemented by brief motivational interviewing was no better than a control treatment in improving the proportion of referrals to orthopaedic surgery or patient willingness to undergo joint replacement if recommended. It is possible that these findings may be attributable to the performance of this particular intervention. A few studies have shown favorable benefits of implementing patient-targeted education tools, including decision aids, in patients with OA [17, 37]. Other tools that target patient knowledge, beliefs, and attitudes regarding surgical treatments for OA may be further developed and tested in the future. It also is worthwhile to assess other means that may improve access of blacks to orthopaedic evaluations. Enhancing the dynamics of the patient-provider relationship, advancing the knowledge of primary care providers on the benefits and risks of TKA, and increasing access to healthcare may help reduce disparities in the use of arthroplasty.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Footnotes
Funding was received from the NIH/National Institute of Arthritis and Musculoskeletal Skin Diseases Grant# 1-RO1-AR-054474-5 (SI) and K24AR055259 (SI).
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might post a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that signed consent was obtained from patients.
This study was performed at the University of Pennsylvania and the Philadelphia VA Medical Center, Philadelphia, PA, USA; and the University of Pittsburgh, Pittsburgh, PA, USA.
References
- 1.Allen KD, Golightly YM, Callahan LF, Helmick CG, Ibrahim SA, Kwoh CK, Renner JB, Jordan JM. Race and sex differences in willingness to undergo total joint replacement: the Johnston County Osteoarthritis Project. Arthritis Care Res (Hoboken). 2014;66:1193–1202. doi: 10.1002/acr.22295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first national Health and Nutrition Examination Survey (HANES I): evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol. 1988;128:179–189. doi: 10.1093/oxfordjournals.aje.a114939. [DOI] [PubMed] [Google Scholar]
- 3.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 4.Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction. 1993;88:315–335. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- 5.Bozic KJ, Belkora J, Chan V, Youm J, Zhou T, Dupaix J, Bye AN, Braddock CH, 3rd, Chenok KE, Huddleston JI., 3rd Shared decision making in patients with osteoarthritis of the hip and knee: results of a randomized controlled trial. J Bone Joint Surg Am. 2013;95:1633–1639. doi: 10.2106/JBJS.M.00004. [DOI] [PubMed] [Google Scholar]
- 6.Burgess DJ, van Ryn M, Crowley-Matoka M, Malat J. Understanding the provider contribution to race/ethnicity disparities in pain treatment: insights from dual process models of stereotyping. Pain Med. 2006;7:119–134. doi: 10.1111/j.1526-4637.2006.00105.x. [DOI] [PubMed] [Google Scholar]
- 7.Byrne MM, O’Malley KJ, Suarez-Almazor ME. Ethnic differences in health preferences: analysis using willingness-to-pay. J Rheumatol. 2004;31:1811–1818. [PubMed] [Google Scholar]
- 8.Chaudhry S, Jin L, Meltzer D. Use of a self-report-generated Charlson Comorbidity Index for predicting mortality. Med Care. 2005;43:607–615. doi: 10.1097/01.mlr.0000163658.65008.ec. [DOI] [PubMed] [Google Scholar]
- 9.Cisternas MG, MGC Data Svcs, Murphy L, Croft JB, Helmick CG. Racial disparities in total knee replacement among Medicare enrollees-United States, 2000-2006. MMWR. 2009;58:133–138. [PubMed]
- 10.Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly: The Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30:914–918. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 11.Forrest CB, Nutting PA, von Schrader S, Rohde C, Starfield B. Primary care physician specialty referral decision making: patient, physician, and health care system determinants. Med Decis Making. 2006;26:76–85. doi: 10.1177/0272989X05284110. [DOI] [PubMed] [Google Scholar]
- 12.Freedland KE. Demanding attention: reconsidering the role of attention control groups in behavioral intervention research. Psychosom Med. 2013;75:100–102. doi: 10.1097/PSY.0b013e3182851b75. [DOI] [PubMed] [Google Scholar]
- 13.Hausmann LR, Mor M, Hanusa BH, Zickmund S, Cohen PZ, Grant R, Kresevic DM, Gordon HS, Ling BS, Kwoh CK, Ibrahim SA. The effect of patient race on total joint replacement recommendations and utilization in the orthopedic setting. J Gen Intern Med. 2010;25:982–988. doi: 10.1007/s11606-010-1399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hawker GA, Guan J, Croxford R, Coyte PC, Glazier RH, Harvey BJ, Wright JG, Williams JI, Badley EM. A prospective population-based study of the predictors of undergoing total joint arthroplasty. Arthritis Rheum. 2006;54:3212–3220. doi: 10.1002/art.22146. [DOI] [PubMed] [Google Scholar]
- 15.Hawker GA, Wright JG, Coyte PC, Williams JI, Harvey B, Glazier R, Badley EM. Differences between men and women in the rate of use of hip and knee arthroplasty. N Engl J Med. 2000;342:1016–1022. doi: 10.1056/NEJM200004063421405. [DOI] [PubMed] [Google Scholar]
- 16.Ibrahim SA, Burant CJ, Siminoff LA, Stoller EP, Kwoh CK. Self-assessed global quality of life: a comparison between African-American and white older patients with arthritis. J Clin Epidemiol. 2002;55:512–517. doi: 10.1016/S0895-4356(01)00501-7. [DOI] [PubMed] [Google Scholar]
- 17.Ibrahim SA, Hanusa BH, Hannon MJ, Kresevic D, Long J, Kwoh CK. Willingness and access to joint replacement among African American patients with knee osteoarthritis: a randomized, controlled intervention. Arthritis Rheum. 2013;65:1253–1261. doi: 10.1002/art.37899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Differences in expectations of outcome mediate African American/white patient differences in “willingness” to consider joint replacement. Arthritis Rheum. 2002;46:2429–2435. doi: 10.1002/art.10494. [DOI] [PubMed] [Google Scholar]
- 19.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Understanding ethnic differences in the utilization of joint replacement for osteoarthritis: the role of patient-level factors. Med Care. 2002;40(1 suppl):144–151. doi: 10.1097/00005650-200201001-00006. [DOI] [PubMed] [Google Scholar]
- 20.Jones A, Kwoh CK, Kelley ME, Ibrahim SA. Racial disparity in knee arthroplasty utilization in the veterans health administration. Arthritis Rheum. 2005;53:979–981. doi: 10.1002/art.21596. [DOI] [PubMed] [Google Scholar]
- 21.Katz BP, Freund DA, Heck DA, Dittus RS, Paul JE, Wright J, Coyte P, Holleman E, Hawker G. Demographic variation in the rate of knee replacement: a multi-year analysis. Health Serv Res. 1996;31:125–140. [PMC free article] [PubMed] [Google Scholar]
- 22.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Legare F, Ratte S, Stacey D, Kryworuchko J, Gravel K, Graham ID, Turcotte S. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2010:CD006732. [DOI] [PubMed]
- 24.Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum. 1989;32:37–44. doi: 10.1002/anr.1780320107. [DOI] [PubMed] [Google Scholar]
- 25.Miller W. Motivational interviewing with problem drinkers. Behav Psychother. 1983;11:147–172. doi: 10.1017/S0141347300006583. [DOI] [Google Scholar]
- 26.Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. New York, NY: The Guilford Press; 2013. [Google Scholar]
- 27.O’Connor AM, Bennett CL, Stacey D, Barry M, Col NF, Eden KB, Entwistle VA, Fiset V, Holmes-Rovner M, Khangura S, Llewellyn-Thomas H, Rovner D. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2009:CD001431. [DOI] [PubMed]
- 28.Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55:305–312. [PMC free article] [PubMed] [Google Scholar]
- 29.Senft RA, Polen MR, Freeborn DK, Hollis JF. Brief intervention in a primary care setting for hazardous drinkers. Am J Prev Med. 1997;13:464–470. [PubMed] [Google Scholar]
- 30.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349:1350–1359. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 31.Suarez-Almazor ME, Souchek J, Kelly PA, O’Malley K, Byrne M, Richardson M, Pak C. Ethnic variation in knee replacement: patient preferences or uninformed disparity? Arch Intern Med. 2005;165:1117–1124. doi: 10.1001/archinte.165.10.1117. [DOI] [PubMed] [Google Scholar]
- 32.van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40(1 suppl):140–151. doi: 10.1097/00005650-200201001-00015. [DOI] [PubMed] [Google Scholar]
- 33.van Ryn M, Burgess D, Malat J, Griffin J. Physicians’ perceptions of patients’ social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. Am J Public Health. 2006;96:351–357. doi: 10.2105/AJPH.2004.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc. Sci. Med. 2000;50:813–828. doi: 10.1016/S0277-9536(99)00338-X. [DOI] [PubMed] [Google Scholar]
- 35.Verbrugge LM, Gates DM, Ike RW. Risk factors for disability among U.S. adults with arthritis. J Clin Epidemiol. 1991;44:167–182. doi: 10.1016/0895-4356(91)90264-A. [DOI] [PubMed] [Google Scholar]
- 36.Ware JE, Jr, Kosinski M, Bjorner JB, Turner-Bowker DM, Gandek B, Maruish ME. User’s Manual for the SF-36v2TM Health Survey. Lincoln, RI: Quality Metric Incorporated; 2007. [Google Scholar]
- 37.Weng HH, Kaplan RM, Boscardin WJ, Maclean CH, Lee IY, Chen W, Fitzgerald JD. Development of a decision aid to address racial disparities in utilization of knee replacement surgery. Arthritis Rheum. 2007;57:568–575. doi: 10.1002/art.22670. [DOI] [PubMed] [Google Scholar]
- 38.Williams DR. Race/ethnicity and socioeconomic status: measurement and methodological issues. Int J Health Serv. 1996;26:483–505. doi: 10.2190/U9QT-7B7Y-HQ15-JT14. [DOI] [PubMed] [Google Scholar]
- 39.Wilson MG, May DS, Kelly JJ. Racial differences in the use of total knee arthroplasty for osteoarthritis among older Americans. Ethn Dis. 1994;4:57–67. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.