Highlights
-
•
Breast reconstruction in anticoagulated patients is not well described.
-
•
They are at high risk for intra-operative and post-operative bleeding complications.
-
•
They often require abbreviated operative times because of other risk factors.
-
•
Here we make use of a recently described autologous technique to address these issues.
-
•
Extirpation & reconstruction took 2.5 h while minimizing perioperative bleeding risk.
Keywords: Breast reconstruction, Breast cancer, Breast surgery anticoagulation
Abstract
Introduction
The available options for post-mastectomy reconstruction in a patient requiring abbreviated operative times and immediate and sustained post-operative anticoagulation are limited.
Presentation of case
A 50 year old woman with a history of multiple deep venous thromboses (DVTs) and pulmonary embolisms (PEs) requested a bilateral prophylactic mastectomy and immediate reconstruction. She had a history of multiple breast biopsies demonstrating atypia and two sisters with premenopausal breast cancer. Her hematologist requested that her anticoagulation be held for the minimal amount of time and that her theater times be kept as short as possible. As such, we felt that she was not a candidate for traditional implant-based reconstruction nor autologous flap surgery. Instead, we made use of a recently described single-stage autologous modified Goldilocks procedure to complete her bilateral mastectomy and reconstruction in 150 min. She was anticoagulated in the operating room and was restarted on her preoperative regimen twelve hours after surgery. She suffered no post-operative complications.
Discussion
There is minimal published literature discussing immediate post-mastectomy reconstruction in the anticoagulated patient. Most reconstructive surgeons find these patients unsuitable for traditional reconstructive techniques. In the current case, we utilized a recently described single-stage autologous technique which allowed us to avoid the bleeding complications associated with the muscular dissection required with implant and flap-based reconstructive surgery. The extirpation and reconstruction was completed in 150 min which is significantly quicker than traditional reconstructions.
Conclusion
The modified Goldilocks procedure is an excellent option in the patient who requires immediate postoperative anticoagulation and abbreviated operative times.
1. Introduction
The use of anticoagulation is becoming more ubiquitous in the practice of modern medicine. It is not uncommon that the reconstructive breast surgeon is faced with a patient who has a strict requirement for anticoagulation in the perioperative period who desires post-mastectomy reconstruction. This could put the patient at significant bleeding risk in the postoperative setting where a sizable open raw space surrounds an implant or a large vascular muscle flap has been mobilized to reconstruct a breast mound. A large postoperative hematoma could result in severe consequences to a delicate microvascular anastomosis, thin mastectomy flap or general flap perfusion. In addition, expander-based reconstruction, by far the most common reconstructive technique utilized in the United States, requires multiple, regular “blind” needle sticks through the mastectomy flap and pectoralis muscle to reach final implant volume. In the fully anticoagulated patient, this provides ample opportunity for significant complications which could include an expanding hematoma and an increased risk of capsular contracture (secondary to repeated exposure of the prosthetic to blood). Expander-based reconstruction can result in regular, repeated muscle tears that could result in significant bleeding in fully anticoagulated patients. None of these conventional reconstructive options are without appreciable bleeding risk and many surgeons would consider these patients unacceptable candidates for any standard type of reconstruction. We recently described a single-stage definitive autologous post-mastectomy reconstructive technique most suitable to obese patients with macromastia and ptosis that does not rely on implants or traditional flap surgery [1]. Here, we extend the use of this technique to a smaller breasted patient requiring immediate postoperative anticoagulation and reduced operative time after bilateral mastectomy. Her extirpation and reconstructive surgery was completed in two and a half hours and intraoperative heparin was used without complication. We believe this reconstructive approach should be strongly considered in this growing patient population.
2. Case report
AA is a 50 year old female with a family history of premenopausal breast cancer in two sisters. She has a history of multiple surgical breast biopsies and atypical ductal hyperplasia. Based on Gail and Tyrer-Cuzick models, her calculated lifetime risk of breast cancer was over 50%. In addition, her breast size was smaller (Fig. 1) making repeated surgical breast biopsies deforming. She desired bilateral prophylactic mastectomy and immediate reconstruction. Notably, she also had a history of multiple deep venous thrombosis (DVT) and pulmonary embolism (PE) requiring inferior vena cava filter placement and lifelong anticoagulation. This also made chemoprevention with tamoxifen impossible as this further predisposes to thrombosis and is contraindicated in these patients. We discussed possible reconstructive options from implant to flap-based surgery. Given the requirement to restart her anticoagulation as soon as possible after surgery and to minimize anesthetic time, we felt traditional reconstructive techniques were inappropriate or limited because of their inherent bleeding risk and that the longer operative times would put her at increased risk for de novo intraoperative venous thromboembolism (VTE). We therefore proceeded with a technique we recently described- a definitive single-stage autologous reconstruction with free nipple grafts which uses local dermis and subcutaneous fat to reconstruct a breast mound, thus avoiding a muscular dissection or additional donor site surgery. Wise mammoplasty markings were designed with plans to narrow the width of the breast in order to maximize the amount of involuted tissue made available to reconstruct a breast mound (Fig. 2). The patient was given 7500 units of intravenous heparin before induction. The nipple areola complexes (NACs) were resized to 42 millimeters and preserved as free nipple grafts. Mastectomies were performed in standard fashion through incisions made through the medial and lateral extensions of the vertical limbs to the inframammary fold. All skin within the mammoplasty marking was preserved and deepithelialized, saving the underlying subcutaneous tissue as well. Inferior dermal tissue and fat was reshaped into a breast mound as previously described. Vertical limbs were closed over the reconstructed breast mound at the trifurcation in the inframammary fold providing additional projection. NACs were grafted into position to complete definitive reconstruction. Resection and reconstruction were completed in 2.5 h. The patient restarted anticoagulation 12 h after surgery. There was no evidence of postoperative bleeding or complication. Her final result one month after surgery is demonstrated in Fig. 3.
Fig. 1.
50 year old female with two sisters deceased from breast cancer and history of multiple breast biopsies demonstrating atypia. She has smaller breasts and requires lifelong anticoagulation secondary to a history of multiple DVT and PE.
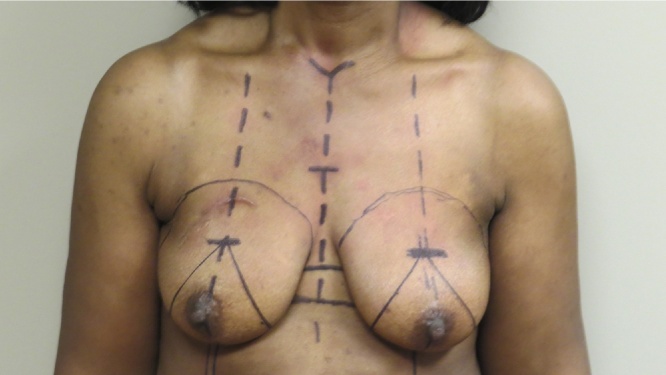
Fig. 2.
Preoperative Wise mammoplasty marking designed to safely maximize the distance between the vertical limbs to increase the amount of deepithelialized skin and underlying subcutaneous tissue that will be involuted and used to create a breast mound after a bilateral mastectomy is performed.
Fig. 3.
Seven month post-operative result after bilateral mastectomy and single stage autologous reconstruction with free nipple grafts performed in 2.5 h (both resection and reconstruction). Her final breast volume can be safely augmented in the future with lipotransfer.
3. Discussion
There is minimal published literature on experience with immediate post-mastectomy reconstruction in the patient requiring postoperative anticoagulation. One recent study described the implications of anticoagulation for port thrombosis in 7 patients and its impact on post-mastectomy reconstruction with most patients successfully undergoing reconstruction with some delays and modifications in the reconstructive strategy without bleeding complication [2]. Other studies, however, have clearly demonstrated an increased risk of postoperative hematoma after breast surgery and reconstruction in patients receiving both VTE prophylaxis and therapeutic anticoagulation [3], [4], [5], [6]. The implications of such a complication have far greater consequences and sequelae on an implant-based, pedicled or free flap reconstruction than the reconstructive approach used here. The duration of the surgical procedure may also place a patient with a history of recurrent DVT and PE at increased risk for a life threatening intraoperative event. The technique we recently described allowed us to complete our patient’s bilateral mastectomy and reconstruction in 2.5 h, significantly faster than traditional reconstructive options. Furthermore, this technique does not require creation of large open potential spaces around an implant, donor site surgery or a muscle flap. Exposure of implants to blood is known to increase risk of capsular contracture and is likely best avoided in this patient population. This technique is simple, cost-effective, quickly performed and definitive with an aesthetic result comparable to the more standard reconstructions. Initially described for patients with significant macromastia and ptosis allowing for a single stage reconstruction, we demonstrate the versatility and safety of this technique by extended the indication here to a smaller breasted woman who requires a short operative time and reduced risk of postoperative bleeding. It allows for a second stage surgery without a defined time frame to increase volume and improve shape that could involve fat grafting, definitive implant placement or skin retailoring procedures. In the event of a postoperative hematoma, this reconstruction can still be safely explored and evacuated which would be significantly more challenging with implants or flaps. The technique obviated any postoperative concerns of the implications of hematoma formation surrounding an implant, flap or microvascular anastomosis. It also avoids the requirement for regular invasive expansions of a temporary implant that puts these patients at continued bleeding risk for an extended period after their initial surgery. We believe this technique is a safer reconstructive option in patients requiring reduced operative times and a requirement to immediately restart postoperative anticoagulation.
4. Conclusions
There is minimal experience with post-mastectomy reconstruction in the high risk anticoagulated patient requiring abbreviated theater times and immediate postoperative anticoagulation. Traditional reconstructive techniques require prolonged operative times and provide multiple opportunities for bleeding complications both intraoperatively and post-operatively. The modified Goldilocks procedure offers reconstructive breast surgeons an opportunity to perform a single-stage autologous reconstruction with shorter operative times and less opportunity for bleeding complications than in the more common breast reconstructions available.
Conflict of interest
There are no conflicts of interest related to the contents of the submitted case report.
Funding
There are no sources of funding.
Ethics approval
The case report involves one patient under the care of both authors. She has provided written consent for publication of this report and all images. A copy of the written consent is available to the Editor-In-Chief of the journal upon request.
References
- 1.Schwartz J.C., Skowronski P. Total single-stage autologous breast reconstruction with free nipple grafts. Plast. Reconstr. Surg. Glob. Open. 2015;3(12):e587. doi: 10.1097/GOX.0000000000000563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Richards K., Forouhi P., Johnston A. Pre-operative thrombotic complications of neoadjuvant chemotherapy for breast cancer: implications for immediate breast reconstruction. Ann. Med. Surg. (Lond.) 2014;4(1):80–84. doi: 10.1016/j.amsu.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patiar S., Kirwan C., McDowell G. Prevention of venous thromboembolism in surgical patients with breast cancer. Br. J. Surg. 2007;94:412–420. doi: 10.1002/bjs.5782. [DOI] [PubMed] [Google Scholar]
- 4.Friis E., Hørby J., Sørensen L. Thromboembolic prophylaxis as a risk factor for postoperative complications after breast cancer surgery. World J. Surg. 2004;28:540–543. doi: 10.1007/s00268-004-7223-9. [DOI] [PubMed] [Google Scholar]
- 5.Lee K.T., Mun G.H. The efficacy of postoperative antithrombotics in free flap surgery: a systematic review and meta-analysis. Plast. Reconstr. Surg. 2015;135(4):1124–1139. doi: 10.1097/PRS.0000000000001100. [DOI] [PubMed] [Google Scholar]
- 6.Senchenkov A., Lemaine C., Tran N.V. Management of perioperative microvascular thrombotic complications- the use of multiagent anticoagulation algorithm in 395 consecutive free flaps. J. Plast Reconstr. Aesthet. Surg. 2015;68(9):1293–1303. doi: 10.1016/j.bjps.2015.05.011. [DOI] [PubMed] [Google Scholar]