Introduction
Deposition of calcium in the skin has been categorised into a group of disorders referred to as calcinosis cutis, which was described by Virchow in 1855. It is a rare and poorly understood autosomal dominant disorder with variable expressivity and is frequently seen in children of Afro-caribbean descent [1]. The aetiology remains uncertain and patients present in the first to second decade of life with large progressively enlarging juxta-articular calcification with tendency to ulcerate the skin and encase adjacent structures [2]. We report a case of primary normo-phosphataemic tumoral calcinosis in a young child and its features as seen on plain radiographs.
Case Report
A two year old boy was brought with the history of multiple, patchy, hard, nodular swellings over right lower limb and right side of chest for the past one year. The lesions were progressively increasing in size and the child had developed difficulty in walking and bending his right knee. There was no history of previous illness or trauma in the past. No family history of similar illness was elicited. General examination revealed a well-nourished, healthy child with restriction of movement at the hip, knee and ankle joints on the right side. Rest of the general and systemic examination was essentially normal. Local examination revealed patches of hard, nodular, mobile and non-tender masses within the soft tissues around the hip and knee joint on right side. Similar nodular lesions were also felt on the right chest wall. These lesions ranged from 3 - 15 cm in size, without ulceration or sinuses.
Haematological and biochemical parameters including blood urea, serum creatinine, calcium, phosphorus and alkaline phosphatase were within normal limits. Radiographic examination of the pelvis revealed extensive, ribbon like juxta-articular calcification in the soft tissues around the hip joint on the right side (Fig. 1). A similar, small cluster of calcifications was also seen on right side of chest. Radiograph of the thighs and knee joints showed lace like soft tissue calcification around the knee joint on the right side (Fig. 2).
Fig. 1.

Radiograph of the pelvis including thigh (Antero-posterior view) showing extensive, ribbon-like juxta-articular calcification in the soft tissues around the hip joint on the right side. The contralateral side appears uninvolved.
Fig. 2.

Radiograph of knee joint (antero-posterior view) showing lace like soft tissue calcification around the knee joint.
Biopsy from a lesion over the skin at the right hip showed normal appearance of the epidermis with deposits of calcium and ossification in the deeper dermis (Fig. 3). No foreign body giant cells or inflammatory exudates were seen. Based on the above findings a diagnosis of primary normo-phosphataemic tumoral calcinosis was made.
Fig. 3.
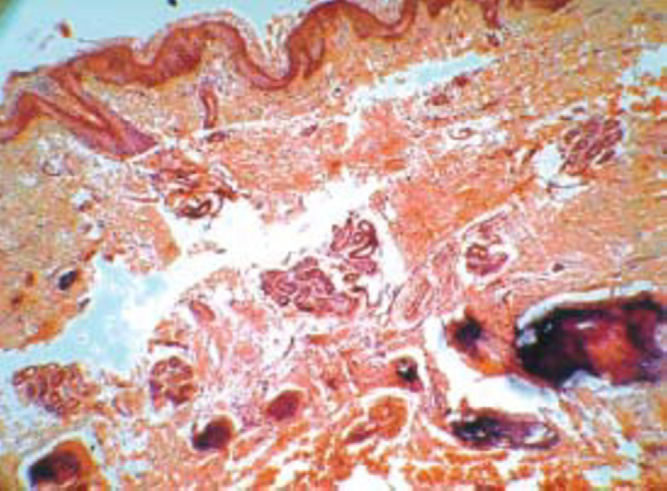
Low power photomicrograph of the skin showing normal epidermis and dermis with unremarkable adnexa. Deeper dermis shows spicules of bone, with areas of calcification.
Discussion
Tumoral calcinosis is a rare, benign condition, characterised by calcific deposits of hydroxyapatite or amorphous calcium phosphate crystals in soft tissues near large joints [3]. It is commonly seen in the first two decades of life. Deposition of calcium in the skin is categorised into a group of disorders referred to as calcinosis cutis which is further subdivided according to the underlying pathological process of calcification into dystrophic, metastatic, idiopathic and iatrogenic. Tumoral calcinosis falls under the idiopathic variety of calcinosis cutis. However some authors have postulated that an inborn error of phosphorus metabolism relating to abnormal phosphate reabsorption and 1,25-dihydroxyvitamin D formation in the proximal renal tubule may be the likely aetiology [4].
There are two distinct subtypes of idiopathic tumoral calcinosis [5], namely primary normophosphataemic tumoral calcinosis in which the patient has normal serum phosphate and calcium levels and primary hypophosphataemic tumoral calcinosis in which the patient has elevated serum phosphate levels with normal serum calcium. Patients with tumoral calcinosis typically present with painless masses in juxta-articular locations, at hip, knee and elbow joints although the shoulder, hands and feet can be involved. Constitutional signs and symptoms are characteristically absent.
Plain radiographs in tumoral calcinosis are often diagnostic showing multiple areas of well-circumscribed, nodular masses with fibrous septae giving a “cobblestone” or “chicken-wire” appearance. Films exposed with a horizontal beam may show the “sedimentation sign” due to mineral portion pooling dependently, creating a fluid calcium level [6]. Symmetrical and bilateral involvement is seen commonly. Bone scintigraphy with radio labelled phosphate compounds (Technetium 99m methylene diphosphonate), demonstrates increased uptake in the soft-tissue masses. On magnetic resonance imaging (MRI), the lesion is hypointense on all sequences with presence of areas of high signal on T2 and inversion recovery sequences, corresponding to oedema due to an inflammatory response to pathologic calcification [6]. The lesions are cystic and multilocular with a capsule and prominent fibrous septae on gross pathology. Histopathology reveals calcium deposits in the dermis, with or without a surrounding giant cell reaction [7].
Spontaneous regression does not occur and the management is unsatisfactory. In patients with defective phosphate metabolism, calcium and phosphate restricted diet and phosphate binder with meal is helpful. Acetazolamide has been tried to increase the urinary phosphate excretion [8]. Indications for surgical removal of skin lesions are pain, recurrent infection, ulceration and functional impairment. The results are not encouraging and recurrences are common.
Conflicts of Interest
None identified
References
- 1.Kluger G, Kochs A, Holthausen H. Heterotopic ossification in childhood and adolescence. J Child Neurol. 2000;15:406–413. doi: 10.1177/088307380001500610. [DOI] [PubMed] [Google Scholar]
- 2.Fitz-Henley M. Image and diagnosis: Calcinosis cutis. West Indian Med J. 2002;51:246–272. [PubMed] [Google Scholar]
- 3.Emery KH, Fletcher BD. The Soft Tissues. In: Kuhn Jerald P, Slovis Thomas L., editors. Caffey's Pediatric Diagnostic Imaging. 10th ed. Mosby; Philadelphia: 2004. pp. 2009–2011. [Google Scholar]
- 4.Murray Ronald O, Jacobson Harold G, Stoker Dennis J. Radiology of Skeletal disorders. 3rd ed. Churchill Livingstone; New York: 1990. pp. 822–823. [Google Scholar]
- 5.Smack D, Norton SA, Fitzpatrick JE. Proposal for a pathogenesis-based classification of tumoral calcinosis. Int J Dermatol. 1996;35:265–271. doi: 10.1111/j.1365-4362.1996.tb02999.x. [DOI] [PubMed] [Google Scholar]
- 6.Martinez Salutario, Vogler JB, III, Harrelson JM, Lyles KW. Imaging of Tumoral Calcinosis: New Observations. Radiology. 1990;174:215–222. doi: 10.1148/radiology.174.1.2294551. [DOI] [PubMed] [Google Scholar]
- 7.Puvabanditsin S, Garrow E, Titapiwatanakun R. Severe calcinosis cutis in an infant. Pediatr Radiol. 2004;11:23–26. doi: 10.1007/s00247-004-1363-9. [DOI] [PubMed] [Google Scholar]
- 8.Kumaran MS, Bhadada S, Bhansali A, Shriram M, Kumar B. Young boy with multiple periarticular swellings and discharging sinuses: Tumoral calcinosis. Indian Journal of Paediatrics. 2004;71:1144. [PubMed] [Google Scholar]


