Abstract
The author describes paediatric case of relapsed acute lymphoblastic leukaemia (ALL) presented as aleukemic leukaemia cutis (ALC). A 2 year old child was admitted in tertiary oncology centre. He suffered from pre B cell ALL with absent Philadelphia chromosome. This patient received multiagent induction chemotherapy as per Berlin–Frankfurt–Munster (BFM) protocol for ALL. He achieved remission after 28 days of treatment. Subsequently he presented with multiple skin lesions in the form of multiple small erythematous violaceous macules, papules, plaques and nodules on face, chest and back regions. Histopathological examination of biopsy of skin revealed diffuse infiltration of tumor cells with prominent nucleoli, scant eosinophilic cytoplasm and numerous mitotic figures consistent with LC. Immunohistochemistry was positive for CD 10, CD 19, CD 22, CD 24, CD 79-a and TdT while negative for surface immunoglobulin. At the time of presentation his peripheral blood smear and bone marrow examination was negative for malignant cells. Sanctuary sites including central nervous system and testicles were not involved. So patient was diagnosed as ALC. He was managed as per BFM relapse protocol for ALL. Skin lesions disappeared completely after 2 weeks of treatment. Unfortunately patient developed bone marrow and testicular relapse after 2 months. He was given testicular radiotherapy and systemic chemotherapy for relapsed ALL. But his marrow was showing persistent activity and he expired after 4 months.
Keywords: Aleukemic leukaemia cutis, Leukaemia cutis, Relapsed acute lymphoblastic leukaemia, Pre B cell ALL, Paediatric case
Introduction
Leukemia cutis (LC) is a rare condition characterized by cutaneous lesion resulting from infiltration of the dermis, epidermis or subcutis by neoplastic leukemic cells. Aleukemic leukemia cutis (ALC) is LC in the absence of bone marrow involvement.
Global incidence of LC is between 2 and 4 % for acute myeloid leukaemia (AML). Out of these, 7 % of cases present as ALC. LC usually occurs in patients with AML-M5. LC occurs at presentation with systemic leukaemia (23–44 %) or in the setting of an established leukaemia (44–77 %). LC can rarely precede development of detectable leukaemia in bone marrow [1, 2] LC in acute lymphoblastic leukaemia (ALL) is very uncommon, occurs in 1–3 % of patients [1, 3, 4]. ALC is very rare in ALL and extremely uncommon in pre B cell ALL.
The intension of this case report is to depict a very rare manifestation of relapsed B cell ALL in the form of ALC in paediatric patient.
Case Vignette
A 2 year old child was admitted in our tertiary oncology centre. He suffered from pre B cell ALL with absent Philadelphia chromosome. This patient received induction chemotherapy with 4 drugs: daunorubicin, vincristine, prednisolone and L asparaginase as per Berlin–Frankfurt–Munster (BFM) protocol for ALL. He achieved remission after 28 days of treatment. Subsequently he presented with multiple skin lesions in the form of multiple small erythematous violaceous macules, papules, plaques and nodules on face, chest and back region (Fig. 1). On physical examination his oral cavity was normal and there was no hepatospleenomegaly or lymphadenopathy.
Fig. 1.
Skin lesions of ALC. a Papulo-nodular skin lesions over face, b and c nodular skin lesions over back
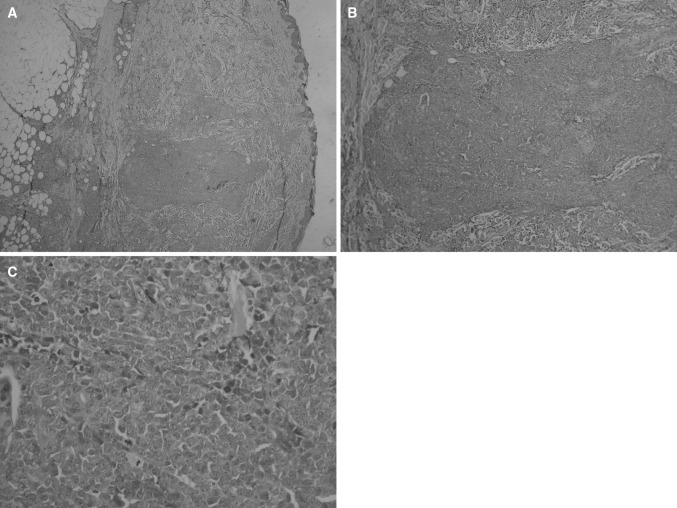
Histopathological examination of biopsy of skin lesions revealed diffuse infiltration of tumor cells with prominent nucleoli, scant eosinophilic cytoplasm and numerous mitotic figures consistent with leukemia cutis (LC) (Fig. 2). Immunohistochemistry suggestive of presence of B cell markers like CD 10, 19, 22, 24, 79-a, TdT and absence of sIg.
Fig. 2.
HPE of ALC
His Laboratory tests at the time of presentation showed, hemoglobin—12.9 g/dL; WBC—31.9 × 109/L with 68.5 % polymorphonuclear cells; 16.5 % lymphocytes; 11.5 % monocytes; 3.4 % eosinophils; 1 % basophils and platelets 5.28 × 109/L. His peripheral blood smear was normal, with no evidence of blasts. Bone marrow aspiration did not reveal blast cells. CSF cytology was also negative for malignant cells and bilateral testicular sonography was normal. So he was diagnosed as acute leukemia cutis (ALC).
He was treated with BFM relapse protocol for ALL including 4 drug chemotherapy in the form of cyclophosphamide, vincristine, prednisolone, L asparaginase. Skin lesions disappeared completely after 2 weeks of treatment.
Subsequently patient developed relapse of bone marrow and testicular relapse after 2 months. He was given testicular radiotherapy and chemotherapy for relapsed ALL. But his marrow was showing persistent activity and he expired after 4 months.
Discussion
The common cause of treatment failure in childhood ALL is relapse. It occurs in 15–20 % of ALL patients. Most ALL relapses occur during treatment or within the first 2 years after completion of treatment. Although there are reports of relapses occurring even after 10 years from the diagnosis [5, 6]. The majority of relapses occur in the bone marrow, either in an isolated form or combined with involvement of another site mainly CNS or testes. Isolated skin relapse is extremely uncommon.
Leukemia cutis (LC) is a rare condition characterized by cutaneous lesion resulting from infiltration of the dermis, epidermis or subcutis by neoplastic leukemic cells.
Majority of cases of LC occur with established systemic leukemia, but it may precede rarely with bone marrow involvement [1, 2]. LC occurs in 2–4 % of patients with AML. LC is very rarely found in ALL about 1–3 % of these patients and extremely rare in pre B cell ALL [1, 3, 4].
Aleukemic leukemia cutis (ALC) is defined as skin involvement by leukemic cells in the absence of marrow involvement. ALC is extremely rare and commonly misdiagnosed. ALC is associated with AML as per certain reports but it is extremely rare with ALL, in particular pre B-ALL.
The reported evidence may be overestimated without biopsy because skin lesions similar to LC have a wide range of inflammatory, neoplastic and infectious etiologies. Certain cutaneous syndromes associated with leukemia such as Sweet’s syndrome, erythema multiforme, erythema nodosum, and pyoderma gangrenosum [7–9]. LC is different from theses cutaneous syndromes. LC is presented as violaceous or erythematous nodules, papules, and plaques of different sizes. The lower extremities are involved most commonly, followed by the upper extremities, back, chest, scalp, and face.
The mechanisms for skin involvement are not fully understood. It has been suggested that certain chemokine receptors and adhesion molecules in leukemic cells like CD56 are responsible for invasion of leukemic cells into skin. It has been suggested that endothelial intercellular adhesion molecule-1 interact with lymphocyte function-associated antigen-1 on blast cells are responsible for skin homing. Thus, this explain the spread of leukemias to skin [10]. But mechanism of ALC in absence of marrow involvement is not yet defined.
Literature review shows only 14 reported cases of ALC associated with ALL. When using the most stringent definition of ALC [11–16] (negative peripheral blood and negative bone marrow at time of diagnosis), only 3 cases of ALC with T-ALL [12, 13, 16], 1 case with nonspecified ALL [15], 1 with bilinear ALL [17], 1 with B-ALL [18] have been reported in adult patients.
As per literature review, characteristics of LC described by different authors are given in Table 1.
Table 1.
Aleukemic leukemia cutis (ALC) in pediatric patients with ALL cases—literature review
| Reference | No. of patients | Age (years) | Type of acute leukemia | Type of relapse |
|---|---|---|---|---|
| Kishimoto et al. [19] | 1 | 70 | B-ALL | LC |
| Lee et al. [11] | 1 | 20 | B-ALL | LC |
| Najem et al. [12] | 1 | 11 | T-ALL | ALC |
| Taniguchi et al. [13] | 1 | 62 | T-ALL | ALC |
| Cochrane et al. [15] | 1 | 63 | Non specific ALL | ALC |
| Ali et al. [16] | 1 | 13 | T-ALL | ALC |
| Leah et al. [18] | 1 | 27 | Pre B-ALL | ALC |
| Aneta et al. [17] | 1 | 13 | Bilinear ALL | ALC |
| Present case | 1 | 2 | Pre B-ALL | ALC |
Conclusion
Isolated cutaneous relapse is rare. This appears to be first reported case of pediatric B cell ALL presented as ALC, as sole sign of relapse. ALC must be considered as one of the differential diagnosis of cutaneous lesions in ALL.
References
- 1.Su WP. Clinical, histopathologic, and immunohistochemical correlations in leukemia cutis. Semin Dermatol. 1994;3:223–230. [PubMed] [Google Scholar]
- 2.Wagner G, Fenchel K, Back W, et al. Leukemia cutis: epidemiology, clinical presentation, and differential diagnosis. J Dtsch Dermatol Ges. 2012;10:27–36. doi: 10.1111/j.1610-0387.2011.07842.x. [DOI] [PubMed] [Google Scholar]
- 3.Cho-Vega JH, Medeiros J, Prieto VG, et al. Leukemia cutis. Am J Clin Pathol. 2008;129:130–142. doi: 10.1309/WYACYWF6NGM3WBRT. [DOI] [PubMed] [Google Scholar]
- 4.Sander CA, Medeiros LJ, Abruzzo LV, et al. Lymphoblastic lymphoma presenting in cutaneous sites: a clinicopathologic analysis of six cases. J Am Acad Dermatol. 1991;25:1023–1031. doi: 10.1016/0190-9622(91)70302-I. [DOI] [PubMed] [Google Scholar]
- 5.Gaynon PS. Childhood ALL and relapse. Br J Haematol. 2005;131(5):579–587. doi: 10.1111/j.1365-2141.2005.05773.x. [DOI] [PubMed] [Google Scholar]
- 6.Rizzani C, Valsecchi MG, et al. outcome of very late relapse in children with ALL. Haematologica. 2004;89(4):427–434. [PubMed] [Google Scholar]
- 7.Millot F, Robert A, Bertrand Y, et al. Cutaneous involvement in children with ALL or lymphoblastic lymphoma: the Children’s Leukemia Cooperative Group of the European Organization of Research and Treatment of Cancer (EORTC) Pediatrics. 1997;100:60–64. doi: 10.1542/peds.100.1.60. [DOI] [PubMed] [Google Scholar]
- 8.Stawiski MA. Skin manifestations of leukemias and lymphomas. Cutis. 1978;21:814–818. [PubMed] [Google Scholar]
- 9.Ratnam KV, Khor C, Su D. Leukemia cutis. Dermatol Clin. 1994;12:419–429. doi: 10.1016/0738-081X(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 10.Bakst RL, Tallman MS, et al. How I treat extramedullary acute myeloid leukemia. Blood. 2011;118(14):3785–3793. doi: 10.1182/blood-2011-04-347229. [DOI] [PubMed] [Google Scholar]
- 11.Lee JI, Park HJ, Oh ST, et al. A case of leukemia cutis at the site of a prior catheter insertion. Ann Dermatol. 2009;21:193–196. doi: 10.5021/ad.2009.21.2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Najem N, Zadeh V, Badawi M, et al. Aleukemic leukemia cutis in a child pre ceding T-cell acute lymphoblastic leukemia. Pediatr Dermatol. 2011;28:535–537. doi: 10.1111/j.1525-1470.2011.01578.x. [DOI] [PubMed] [Google Scholar]
- 13.Taniguchi S, Hamada T, Kutsuna H, et al. Lymphocytic aleukemic leukemia cutis. J Am Acad Dermatol. 1996;35:849–850. doi: 10.1016/S0190-9622(96)90101-2. [DOI] [PubMed] [Google Scholar]
- 14.Kishimoto H, Furui Y, Nishioka K. B-cell ALL with a leukemic leukemia cutis. Eur J Dermatol. 2001;11:151–152. [PubMed] [Google Scholar]
- 15.Cochrane T, Milne JA. A leukaemic acute lymphoblastic leukaemia presenting with cutaneous lesions. Br J Dermatol. 1974;91:587–589. doi: 10.1111/j.1365-2133.1974.tb12950.x. [DOI] [PubMed] [Google Scholar]
- 16.Ali R, Ozan U, Ozkalemkas F, et al. Leukaemia cutis in T-cell acute lymphoblastic leukaemia. Cytopathology. 2006;17:158–161. doi: 10.1111/j.1365-2303.2006.00289.x. [DOI] [PubMed] [Google Scholar]
- 17.Aneta S, Jakub L, Joanna Z et al (2014) Aleukemic leukemia cutis as a manifestation of acute lymphoblastic leukemia in a 13-year-old girl. Prog Med Sci 27(4):271–274
- 18.Leah H, Jayesh M, Jonathan C, et al. Recurrent aleukemic leukemia cutis in a patient with pre-B-cell acute lymphoblastic leukemia. J Clin Oncol. 2013;31:353–355. doi: 10.1200/JCO.2012.46.1939. [DOI] [PubMed] [Google Scholar]
- 19.Kishimoto H, Furui Y, Nishioka K. B-cell ALL with a leukemic leukemia cutis. Eur J Dermatol. 2001;11:151–152. [PubMed] [Google Scholar]