Abstract
Invasive aspergillosis infection (IF) in patients with hematologic malignancies is common. Prognosis of IF in patients with acute myeloid leukemia (AML) not responsive to chemotherapy is very poor, especially when neutropenia is duration. Fractional HLA haplo-identical mobilized neutropenia peripheral blood stem cell (PBSC) transfusion, which was defined as micro-transplantation, was recently adopted in treatment of elder patients with AML and shown to be effective in fasting hemopoiesis recovery. Here we report the outcome of an elderly patient with AML accompanying IF treated with microtransplantation and voriconazole. The patient (female, age 62) was diagnosed relapsed AML accompaning suspected invasive fungal infection. She refused to accept further chemotherapy. PBSC from her daughter were collected and transfused fractionally. Voriconazole was used for anti- aspergillosis treatment. After stem cell infusions, the patient’s neutrophil count increased, and platelet transfusion interval extended from 3–4 to 10–14 days. Lung CT indicated that the lesions were significantly absorbed. The patient survived for 257 days. We concluded that for elderly patients with AML and accompanying IF who are not eligible for chemotherapy, microtransplant may be beneficial for improving the efficacy of anti-fungal treatment.
Keywords: Microtransplantation, Invasive aspergillosis infection, Leukemia
Introduction
The probability of invasive aspergillosis infection (IF) in patients with hematologic malignancies is 3.1 %, and the 90-day mortality rate is as high as 42 % [1]. Prognoses mainly depend on the state of the disease and the duration of neutropenia. For those patients with acute myeloid leukemia (AML), non-responsive to chemotherapy and with long durations of neutropenia, IF-related mortality is even higher and may reach 90 %, even if sufficient anti-fungal treatment were prescribed [2]. In recent years, there have been reports that infusion of allogeneic hematopoietic stem cells (microtransplantation) post chemotherapy could promote recovery of bone marrow suppression, shorten the neutropenic period and decrease the incidence of infection in elderly patients with AML [3]. Here we report the outcome after treating an elderly patient with AML and accompanying invasive aspergillosis infection with microtransplantation and voriconazole.
Case Report
The patient (female, age 62) was enrolled in the hospital in January 2014. Previously, in January 2013, she was diagnosed with myelodysplastic syndrome (MDS) at another hospital. This condition progressed to AML in April 2013. The patient reached complete response to the chemotherapy with decitabine and CAG (including G-CSF, aclarubicin and Ara-C). However, she relapsed in December 2013. A second course of decitabine together with CAG was recommended. In January 2014, the patient presented a fever and cough and at this time was transferred to our hospital. A physical examination at admission revealed a body temperature of 38.0 °C, severe anemia, scattered petechiae and ecchymosis. A routine blood analysis showed pancytopenia, with a white blood cell (WBC) count of 0.77 × 109/l, neutrophilic granulocyte cell count of 0.4 × 109/l, Hb 5.2 g/dl, and platelet cell count of 5 × 109/l. Bone marrow morphology revealed hyperplasia, myeloid dysplasia, and still 12 % of leukemia cells remained. Nodular focus was observed on the left upper lung. Aspergillus antigen (galactomannan) assay was positive (5.8 unit, reference range <0.5). According to the literature [4], the patient was diagnosed suspected invasive fungal infection and was given voriconazole antifungal therapy. After receiving voriconazole therapy, the patient’s body temperature returned to normal, and her cough was significantly relieved.
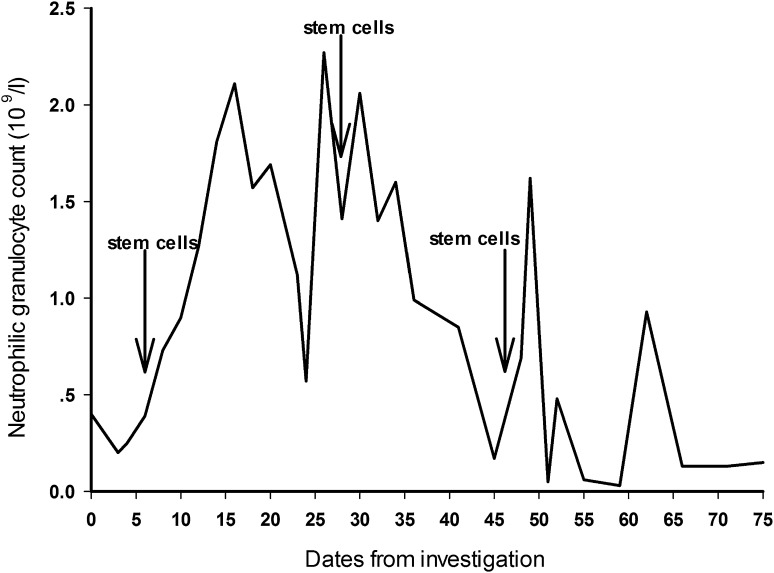
Due to the patient’s age, poor physical state and the complication of invasive pulmonary aspergillosis infection, further chemotherapy was denied by the patient and her relatives. Therefore, microtransplantation without chemotherapy was recommended. The patient’s HLA haplo-identical daughter was selected as the donor. Peripheral blood stem cells (PBSC) after G-CSF mobilization were collected in January 20, 2014. Donor PBSC, including mononuclear cells [2.8 × 108/donor body weight (kg)], and CD34+ cells [1.6 × 106/donor body weight (kg)], were divided into three packages. One package was infused into the patient on the day of collection. The remaining two packages were infused on February 11, 2014 and March 4, 2014, respectively. Prior to infusion, dexamethasone was given as an immunosuppressive treatment. No other immunosuppressants were administered. No fever, rash, diarrhea or other discomfort appeared during the transfusion. After stem cell infusions, the patient’s neutrophil count increased (shown in Fig. 1), and platelet transfusion interval extended from 3–4 to 10–14 days. Voriconazole was continued during the micro-transplant procedure. As reviewed in April 2014, the lung CT indicated that the lesions were significantly absorbed. To facilitate follow-up treatment, voriconazole was changed to an oral route without changing the dose until June 2014. Since that time, the patient continued to experience intermittent fevers that were alleviated by giving antibiotics. The patient died of leukemia cell systemic infiltration in October 4, 2014. From the time of the initial microtransplant, the patient survived for 257 days.
Fig. 1.
Changes in the patient’s neutrophil count before and after allogeneic hematopoietic stem cell micro-transplant. The patient was infused with daughter-source G-CSF mobilized peripheral hematopoietic stem cells on the 6th, 28th and 48th day of investigation. Transient increases in neutrophil number were observed after each infusion
Discussion
For patients with hematologic malignancies accompany with IF, it is crucial to increase granulocyte counts. Granulocyte transfusion is the most intuitive way and has been proven effective in some patients with hematologic malignancies [5]. However, granulocyte transfusion only transiently increases granulocyte counts, quite a few healthy donors are needed to collect a sufficient number of granulocytes, and repeated infusions with granulocytes from different donors in a short time are required to achieve a therapeutic aim. Microtransplantation was shown to be effective in accelerating granulocyte and platelets recovery in elderly patient with AML after chemotherapy [3]. We noticed that microtransplantation alone seems to be effective in restoring normal hematopoietic function. This was confirmed by the increased granulocyte count and elongation of platelet half-life following transfusion. We concluded that for elderly patients with AML and accompanying IF who are not eligible for chemotherapy, microtransplant may be beneficial for improving the efficacy of anti-fungal treatment.
Acknowledgments
This study was supported by Grants from self-financed projects from the bureau of health of Guangxi Province (Z2014357) and Guangxi Science and Technology Plan (1355005- 2-1).
Compliance with Ethical Standards
Author’s Contribution
Weiye Nie performed the research; Yongsheng Chen wrote the paper; Xiaolin Yin designed the research.
Conflict of interest
The authors declare no competing financial interests.
References
- 1.Nicolle MC, Benet T, Thiebaut A, Bienvenu AL, Voirin N, Duclos A, et al. Invasive aspergillosis in patients with hematologic malignancies: incidence and description of 127 cases enrolled in a single institution prospective survey from 2004 to 2009. Haematologica. 2011;96:1685–1691. doi: 10.3324/haematol.2011.044636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pagano L, Caira M, Candoni A, Offidani M, Martino B, Specchia G, et al. Invasive aspergillosis in patients with acute myeloid leukemia: a SEIFEM-2008 registry study. Haematologica. 2010;95:644–650. doi: 10.3324/haematol.2009.012054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo M, Hu KX, YU CL, Sun QY, Qiao JH, Wang DH, et al. Infusion of HLA-mismatched peripheral blood stem cells improves the outcome of chemotherapy for acute myeloid leukemia in elderly patients. Blood. 2011;117:936–941. doi: 10.1182/blood-2010-06-288506. [DOI] [PubMed] [Google Scholar]
- 4.Ascioglu S, Rex JH, de Pauw B, Bennett JE, Bille J, Crokaert F, et al. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis. 2002;34:7–14. doi: 10.1086/323335. [DOI] [PubMed] [Google Scholar]
- 5.Dinser R, Grgic A, Kim YJ, Pfreundschuh M, Schubert J. Successful treatment of disseminated aspergillosis with the combination of voriconazole, caspofungin, granulocyte transfusions, and surgery followed by allogeneic blood stem cell transplantation in a patient with primary failure of an autologous stem cell graft. Eur J Haematol. 2005;74:438–441. doi: 10.1111/j.1600-0609.2004.00384.x. [DOI] [PubMed] [Google Scholar]