Abstract
Tonsillar lymphoma usually presents as unilateral or bilateral enlargement or as an ulcerative or fungating lesions. Most lymphomas that involve the tonsils are diffuse large B-cell lymphomas and primary low grade lymphomas are exceptional. We report a case of primary B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) affecting tonsils with interfollicular pattern of infiltration in a 54-year-old female who clinically presented with bilateral tonsillar enlargement, sore throat, dysphagia and respiratory difficulty, unresponsive to the conservative treatment. To the best of our knowledge, till date only six cases of CLL/SLL infiltrating tonsils have been reported in the English literature, three of these were known cases of CLL/SLL prior to tonsillectomy. In the present case diagnosis of CLL/SLL was first time established on tonsillar histomorphology and that too with an unusual interfollicular pattern of infiltration.
Keywords: Chronic lymphocytic leukemia, Tonsils, Interfollicular
Introduction
Routine tonsillectomy is performed for various non-neoplastic conditions for instance obstructive sleep apnea, snoring, and recurrent infection, and those responding to conservative treatment [1]. Non-Hodgkin lymphoma of the tonsils accounts for less than 1 % of malignant head and neck tumors as a whole, and commonest histologic type is diffuse large B cell lymphoma(DLBCL) [2]. Tonsillar involvement in chronic lymphocytic leukemia (CLL) is rare and has only been reported 6 times previously in the English literature (Table 1) [3–8]. We describe a case of an elderly female presenting with bilateral tonsillar enlargement as a first clinical manifestation of CLL/SLL and to best of our knowledge this is the third such description of tonsillar CLL with predominant interfollicular pattern of infiltration.
Table 1.
Reported cases of tonsillar CLL/SLL in English literature
| Reference; Year | Age/sex | Clinical presentation | Known case of CLL | Histopathology diagnosis | Pattern of infiltration |
|---|---|---|---|---|---|
| Nolan [3]; 1996 | 69/M | Obstructive sleep apnea | Yes | CLL | NA |
| Chehal et al. [4]; 2002 | 66/M | Obstructive sleep apnea | Yes | CLL | NA |
| Tsou et al. [5]; 2004 | 41/M | Obstructive sleep apnea | Yes | SLL | Diffuse infiltrate |
| Kaur et al. [6]; 2004 | 56/M | Incidental | No | SLL | Interfollicular infiltrate |
| Soria-Céspedes et al. [7]; 2010 | 54/M | Obstructive sleep apnea | No | SLL | Interfollicular infiltrate |
| Minca et al. [8]; 2012 | 52/M | Incidental in a known case of squamous cell carcinoma tonsils | No | SLL | Diffuse infiltrate |
| Present case | 54/F | Recurrent sore throat, dysphagia and respiratory difficulty | No | CLL | Interfollicular infiltrate |
Case Presentation
Case History
A previously healthy 54-year-old female complained of persistent sore throat, dysphagia and respiratory difficulty for last 6 months. On evaluation both the tonsils were enlarged, for which tonsillectomy was performed as the patient was unresponsive to conservative treatment. There were no palpable cervical lymph nodes or B symptoms (fever, weight loss and cold sweats).
Pathologic Findings
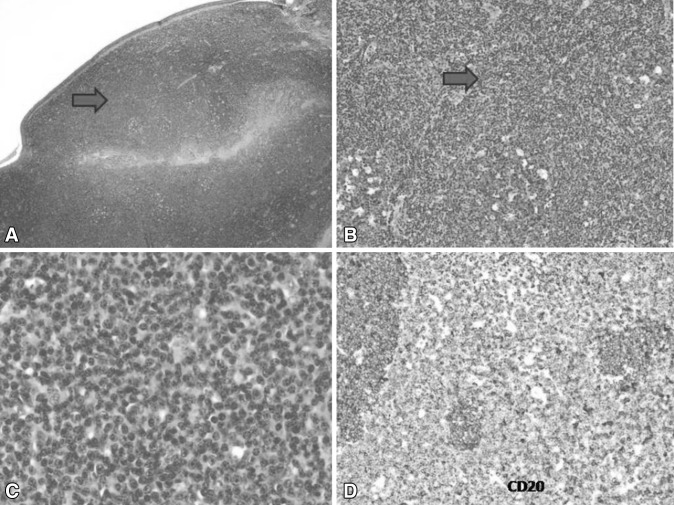
Gross examination revealed bilateral tonsillar enlargement (right > left). Right and left tonsillar tissue measuring 52 and 34 mm in maximum dimensions respectively. On histologic evaluation, many well preserved lymphoid follicles with reactive germinal centres were seen. At places there was marked interfollicular expansion by monomorphic appearing atypical lymphoid infiltrate. Individual cells were small in size with scant cytoplasm, round nuclei with clumped nuclear chromatin and inconspicuous nucleoli (Fig. 1). No proliferation centres (pseudofollicles) were seen. Morphological possibility of CLL/SLL and mantle cell lymphoma were considered. On immunohistochemistry, the interfollicular atypical lymphoid infiltrate showed dim CD20 positivity, strong CD5 and strong CD23 positivity consistent with a diagnosis of CLL/SLL (Figs. 1, 2). Ki-67 proliferative index in these interfollicular areas was 12–15 %. Bcl-2 and cyclin-D1 were negative in the atypical lymphoid infiltrate. Diagnosis of CLL/SLL was first established on tonsillar histomorphology and subsequent haematological work-up revealed absolute lymphocytosis(Total leukocyte count-10.8 × 109/L; Absolute lymphocyte count 4.2 × 109/L) without anemia (Hb-133 mmol/L) and thrombocytopenia (Platelet count 378 × 109/L). A complete staging workup showed mild bilateral cervical lymphadenopathy of size 0.5–1.0 cm, however no significant lymphadenopathy or hepatosplenomegaly was noted. Flow cytometry of peripheral blood was held back as diagnosis was already established on histopathology.
Fig. 1.
a Tonsil with interfollicular expansion as highlighted by arrow head (H&E, ×20); b interfollicular pattern of infiltrate is highlighted by arrow head. In addition, reactive follicles are also noted(H&E, ×100); c atypical lymphoid infiltrate is composed of small lymphoid cells with clumped chromatin(H&E, ×400); d CD20 immunohistochemistry: Note “dim” reactivity in interfollicular CLL/SLL in comparison to the reactive germinal center with strong CD20 reactivity (Original magnification, ×200)
Fig. 2.
a, b Atypical lymphoid infiltrate is positive for both CD5 and CD23(Original magnification, ×200)
Discussion
B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) is one of the most common lymphoproliferative disorders in western countries [9]. Although most patients with CLL/SLL will ultimately demonstrate peripheral blood and bone marrow involvement (CLL), some cases exhibit exclusively nodal disease (SLL) at time of diagnosis [10]. Both bone marrow or peripheral blood CLL and nodal-based SLL have identical morphologic and immunophenotypic characteristics. Thus, the International Lymphoma Study Group proposed the designation CLL/SLL to acknowledge that both CLL and SLL are currently considered to be different manifestations of the same disease entity [11].
Bilateral tonsillar enlargement secondary to CLL infiltration is rare with only 6 cases reported in the English literature (Table 1) [3–8]. Three of the reported cases had a working diagnosis of CLL/SLL prior to tonsillectomy, however in the present case diagnosis was made primarily on tonsillar tissue and was later correlated with peripheral blood findings which revealed isolated absolute lymphocytosis with few smudge cells. In addition, this case highlights interfollicular pattern of infiltration which is described previously only twice.
Chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) typically involves nodal or extranodal tissues as a diffuse proliferation with pseudofollicular growth centers obliterating normal architecture. The explanation for the predominantly interfollicular pattern of CLL/SLL in tonsils is unclear. This microanatomic predilection may be explained, in part, by the putative origin of CLL/SLL from a CD5+ve CD23+ve B-cell that is a recirculating pregerminal center B-cell, which resides or homes to the follicular mantle zone [12]. Perhaps these cases represent partial or early involvement by neoplasm. However, the retention of these patterns in extranodal sites, and the presence of disseminated disease in most cases argue against this explanation. Alternatively, the neoplastic cells may secrete cytokines that induce germinal center formation, at least in extranodal sites [13].
From a diagnostic standpoint, the recognition of this unusual pattern of CLL/SLL infiltration along with demonstration of the characteristic immunophenotypic profile is important to arrive at the correct diagnosis.
Conclusion
The present case clearly highlights that bilateral asymmetrical tonsillar enlargement unresponsive to conservative treatment in an elderly is unusual and should alert the clinician and histopathologist to look for the possibility of an indolent lymphoma. In addition, the present case also clearly highlights unusual interfollicular pattern of involvement in CLL/SLL that can be difficult to recognize histologically, and it should be further supported with immunophenotypic profile to give lead to a correct diagnosis.
References
- 1.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Rep. 2009;11:1–25. [PubMed] [Google Scholar]
- 2.Mohammadianpanah M, Omidvai S, Mosalei A, et al. Treatment results of tonsillar lymphoma: 10 years experience. Ann Hematol. 2005;83:223–226. doi: 10.1007/s00277-004-0860-0. [DOI] [PubMed] [Google Scholar]
- 3.Nolan P. Chronic lymphocytic leukaemia presenting as severe obstructive sleep apnoea. Respirology. 1996;1:299–301. doi: 10.1111/j.1440-1843.1996.tb00046.x. [DOI] [PubMed] [Google Scholar]
- 4.Chehal A, Haidar JH, Jabbour R, Yammout B, Bazarbachi A. Obstructive sleep apnea secondary to chronic lymphocytic leukemia. Ann Oncol. 2002;13:1833–1834. doi: 10.1093/annonc/mdf277. [DOI] [PubMed] [Google Scholar]
- 5.Tsou YA, Cheng YK, Lin CD, Chang WC, Tsai MH. Small B cell lymphocytic lymphoma presenting as obstructive sleep apnea. World J Surg Oncol. 2004;2:26. doi: 10.1186/1477-7819-2-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaur P, Nazeer T. B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma presenting in the tonsil: a case report and review of literature. Am J Otolaryngol. 2004;25(2):121–125. doi: 10.1016/j.amjoto.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 7.Soria-Céspedes D, Baquera-Heredia J, Pardo A, Ortiz-Hidalgo C. Bilateral tonsillar hypertrophy as the first manifestation of B cell-small lymphocytic lymphoma with interfollicular pattern. Rev Med Inst Mex Seguro Soc. 2010;48(1):75–78. [PubMed] [Google Scholar]
- 8.Minca EC, Popat SR, Chadha MK, Merzianu M. Small lymphocytic lymphoma obscuring microscopic tonsillar squamous cell carcinoma: an unknown occurrence with a known primary. Head Neck Pathol. 2012;6(1):125–129. doi: 10.1007/s12105-010-0228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Redaelli A, Laskin BL, Stephens JM, et al. The clinical and epidemiological burden of chronic lymphocytic leukaemia. Eur J Cancer Care (Engl) 2004;13:279–287. doi: 10.1111/j.1365-2354.2004.00489.x. [DOI] [PubMed] [Google Scholar]
- 10.Armitage JO, Weisenburger DD. New approach to classifying non-Hodgkin’s lymphomas: clinical features of the major histologic subtypes. Non-Hodgkin’s Lymphoma Classification Project. J Clin Oncol. 1998;16:2780–2795. doi: 10.1200/JCO.1998.16.8.2780. [DOI] [PubMed] [Google Scholar]
- 11.Harris N, Jaffe E, Stein H, Banks P, Chan J, Cleary M, et al. A revised European-American classification of lymphoid neoplasms:a proposal from the International Lymphoma Study Group. Blood. 1994;84:1361–1392. [PubMed] [Google Scholar]
- 12.Kipps TJ. The CD5 B cell. Adv Immunol. 1989;47:117–185. doi: 10.1016/S0065-2776(08)60663-X. [DOI] [PubMed] [Google Scholar]
- 13.Gupta D, Lim MS, Medeiros LJ, Elenitoba-Johnson KSJ. Small lymphocytic lymphoma with perifollicular, marginal zone, or interfollicular distribution. Mod Pathol. 2000;13(11):1161–1166. doi: 10.1038/modpathol.3880214. [DOI] [PubMed] [Google Scholar]