Introduction
The emergence of endoscopic surgery has revolutionized the management of endometriosis, infertility, ovarian cyst and ectopic pregnancy. Similarly, Assisted Reproductive Techniques (ART) have provided hope for those infertile couples where other therapies have failed. Notwithstanding the cost factor these options appear attractive. However, no method can replace Lower Segment Caesarean Section (LSCS) as a means of abdominal delivery of the foetus, when indicated. Therefore, any modifications in the technique which reduces the operative time, blood loss and post operative complications would be welcome. Misgav Ladach Technique [1], which involves certain modifications in the routine method of LSCS using Pfannensteil incision, achieves these objectives satisfactorily and is gaining popularity gradually. This method was first practiced in Misgav Ladach Hospital in Jerusalem from where it derives its name.
Steps of the Method
-
1.
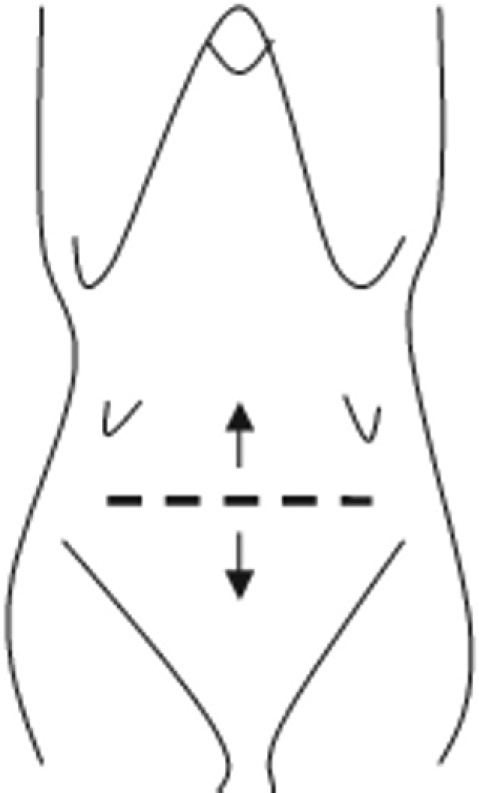
Skin incision is 3 cm below the line joining the anterior superior iliac spines and is about 15 – 17 cm long (Fig 1). It should be extremely superficial cutting only the cutis giving an almost bloodless field.
-
2.
It is deepened in the mid 3 – 4 cm upto the anterior rectus sheath which is cut transversely with the scalpel for that much length.
-
3.
It is then extended transversely by pulling the upper and lower edges of the cut rectus sheath in the cranio-caudal direction (Fig 2).
-
4.
Rectus abdominis muscles come into view now. The belly of these muscles is held by the surgeon and the assistant and pulled away from the midline to the respective side (Fig 3).
-
5.
Parietal peritoneum comes into view which is opened bluntly, as high as possible, by nibbling at it with the index finger. Peritoneal opening is extended transversely by pulling its upper and the lower edges in the cranio-caudal direction (Fig 4). This avoids inadvertent extension of the incision into the urinary bladder.
-
6.
Uterovesical pouch is opened with scissors and bladder pushed down by blunt dissection. Lower uterine segment is opened transversely with scalpel and extended laterally on each side applying traction with fingers. Delivery of the foetus is accomplished with the help of fundal pressure applied by the assistant. Injection Methergin (Methyl ergometrine) 0.2 mg IV is given soon after the delivery of the foetus which reduces blood loss. Placenta is removed manually which again contributes to reduced blood loss. Uterus is exteriorised, massaged and the uterine cavity is cleaned with an abdominal swab to make it contract faster. Uterine incision is closed with a single layer of absorbable suture (Chromic Catgut No. 1). The visceral peritoneum is left unsutured. Large clots are removed. However, no attempt is made to mop out the fluid blood mixed with amniotic fluid. After verifying the count from the scrub nurse, the abdomen is closed by suturing the anterior rectus sheath with Vicryl no.1 or Chromic catgut no. 1. Parietal peritoneum is not sutured. Skin is closed with 3 – 4 mattress silk sutures.
Fig. 1.

Position of Joel Cohen Incision
Fig. 2.
Extending the incision by pulling the cut ends of the sheath upwards and downwards as shown by arrows
Fig. 3.
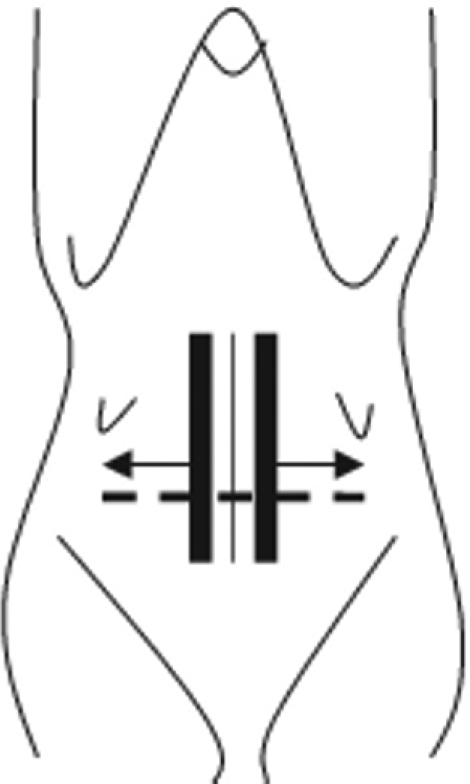
The bellies of the rectus abdominis muscles are held with fingers and pulled laterally away from the midline on each side
Fig. 4.
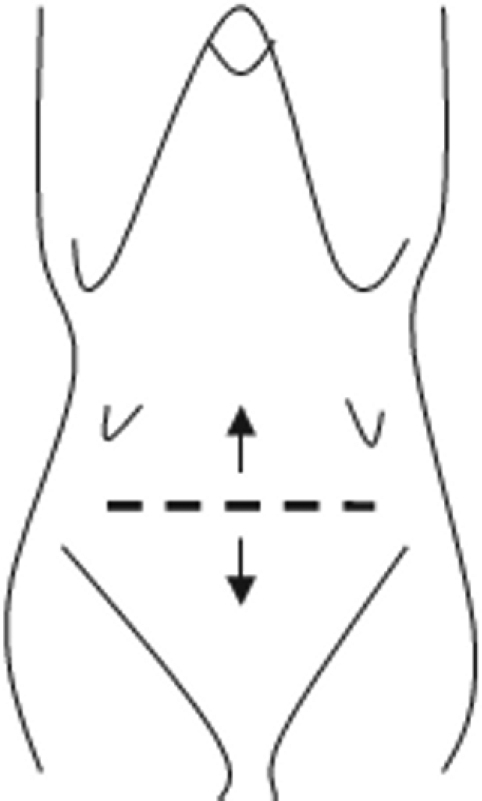
Peritoneal opening is extended transversely by applying traction in cranio-caudal direction
Advantages of the Technique
-
1.
Bleeding is less while giving the skin incision since it is superficial and blood vessels which run at right angles across the incision get retracted laterally when the incision is being extended transversely by pulling the anterior rectus sheath in the cranio-caudal direction.
-
2.
Rectus muscles need not be separated from the overlying anterior sheath in the midline by sharp dissection as in the Pfannensteil method. Since the incision is at a higher level than the Pfannensteil incision, dissection is not required in the region of the Pyramidalis muscles and this saves time.
-
3.
Since the peritoneum is opened bluntly chances of causing any injury to the intestines by use of sharp instruments is eliminated. Since, the peritoneal incision is extended transversely by applying force in cranio-caudal direction, chances of injury to the urinary bladder are reduced.
-
4.
Intestines are not packed off by roller gauge or abdominal swabs ensuring minimal handling of the gut during surgery. This results in an early return of bowel movements.
-
5.
Placenta is removed manually which shortens the third stage and reduces blood loss. However, this has not been accepted universally.
-
6.
Uterus is exteriorized which makes suturing easier. Uterine incision is closed in a single layer to give greater strength to the scar [2]. The 2 layer traditional method tends to give rise to tissue ischaemia impairing healing.
-
7.
The amniotic fluid which is left behind curb local infection by its bacteriostatic property.
-
8.
Suturing the peritoneum is superfluous, since it heals rapidly without suturing [3, 4]. Leaving visceral and parietal peritoneum unsutured reduces post operative adhesion formation [5]. This is probably due to use of less suture material and therefore less tissue reaction.
-
9.
Giving less number of sutures for the skin is associated with a lesser incidence of keloid formation.
-
10.
It is faster because several steps like suturing the uterus in more than one layer and suturing of visceral and parietal peritoneum are omitted.
-
11.
It offers marginal advantage in terms of cost because less suture material is required.
References
- 1.Darj E, Nordstrom ML. The Misgav Ladach method for cesarean section compared to the Pfannensteil method. Acta Obstet Gynecol Scand. 1999;78:37–41. [PubMed] [Google Scholar]
- 2.Tucker JM, Hauth JC, Hodgkins P. Trial of labour after a one or two layer closure of a low transverse uterine incision. Am J Obstet Gynecol. 1993;168:545–546. doi: 10.1016/0002-9378(93)90490-a. [DOI] [PubMed] [Google Scholar]
- 3.Chamberlain G. Caesarean Section. In: Chamberlain G, Steer P, editors. Turnbull's Obstetrics. 3rd. Harcourt Publishers; London: 2001. p. 612. [Google Scholar]
- 4.Heys SD, Goughd RJ, Steele . The Gastrointestinnal system: The peritoneum. In: Eremin O, editor. The scientific and clinical basis of surgical practice. 1st. Oxford University Press; Nottingham: 2001. p. 246. [Google Scholar]
- 5.Stark M. Adhesion — free cesarean section. World J Surg. 1993;17:419. doi: 10.1007/BF01658718. [DOI] [PubMed] [Google Scholar]


