Abstract
Cervical thymic cysts are among the rarest cysts found in the neck. They usually occur during infancy and childhood, and they are extremely rare in adults. They may be found at any level of the pathway of normal thymic descent, from the angle of the mandible to the superior mediastinum. Being uncommon, they are rarely included in the clinical diagnosis of lateral neck masses and are commonly misdiagnosed as branchial cysts, lymphatic malformations, epidermoid cysts, dermoid cysts, lymphadenitis or neoplastic masses. The diagnosis of cervical thymic cyst is rarely made preoperatively and histopathological examination of the excised specimen is the only definitive means of diagnosis in a majority of the reported cases. We report the clinical presentation and therapeutic management of a rare case of multiloculated cervical thymic cyst in a 24-year-old adult which masqueraded as a tuberculous lympadenitis along with a review of literature.
Keywords: Multiloculated cervical thymic cyst, Tuberculous lympadenitis, Lateral neck masses, Thymectomy
Introduction
Cervical thymic cyst is a rare abnormality that is caused by arrest of the normal embryogenic migration of thymic primordium. Hsieh et al. [1] reported cervical thymic cysts to be 0.3 % of all congenital cervical cysts in children. In 1901, Polloson and Piery made the first attempt of surgical excision of this lesion in an infant; however a successful total removal was accomplished in 1944. We report the clinical presentation and therapeutic management of a rare case of multiloculated cervical thymic cyst in a 24-year-old lady which masqueraded as a tuberculous lympadenitis along with a review of literature.
Care Report
A 24-year-old lady presented to our centre with an insidious onset painless swelling over the right side of the neck since 2 months. There was no history of difficulty in swallowing, hoarseness or any other constitutional symptoms. Her family history and past medical history were unremarkable. Clinical examination revealed an isolated 4 cm firm and mobile matted lymph nodal swelling in right level III cervical region. General examination and examination of the rest of the organ systems were normal. Her chest skiagram, biochemical and hematological investigations were within normal limits. A CT of the neck revealed a 5.3 × 4.2 × 2 cm partly necrotic nodal mass in the right level 3 region (Fig. 1). Fine needle aspiration cytology from the swelling revealed a proteinaceus material with few neutrophils and histiocytes, no atypical cells were seen. Cytological examination of the fluid was suggestive of a granulomatous reaction. A provisional diagnosis of a tuberculous cervical adenitis was made and the patient was taken for an excision biopsy for confirmation of the same. Intra-operatively the matted swelling was carefully dissected off the internal jugular vein, carotid artery, vagus nerve and from the sternocleidomastoid muscle and removed in toto (Fig. 2). The final histopathology surprisingly revealed multiloculated cyst lined by stratified squamous epithelium and at places by cuboidal epithelium. Cyst wall showed thymic tissue. Cholesterol clefts and granulomatous reaction was also seen. The final impression was that of a cervical thymic cyst (Fig. 3). The postoperative period was uneventful and the patient has been locally controlled for more than 6 months.
Fig. 1.
a, b A CT of the neck revealed a 5.3 × 4.2 × 2 cm partly necrotic nodal mass in the right level 3 region
Fig. 2.

Intra-operatively the matted swelling was carefully dissected off the internal jugular vein, carotid artery, vagus nerve and from the sternocleidomastoid muscle and removed in toto
Fig. 3.
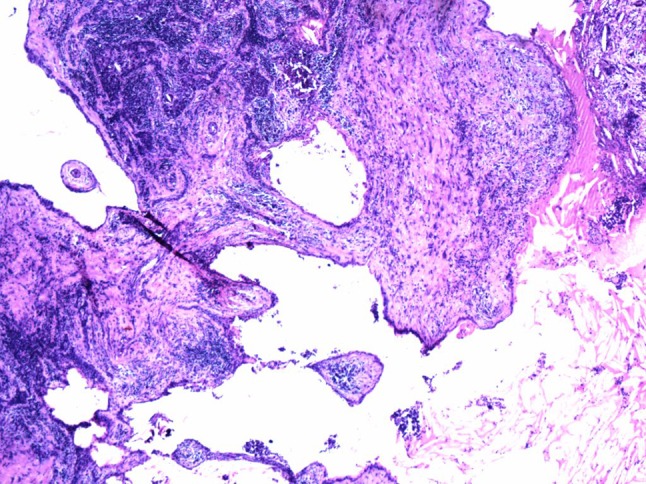
H&Ex20: Showing a multiloculated cyst lined by stratified squamous epithelium and at places by cuboidal epithelium. Cyst wall showed thymic tissue. Cholesterol clefts and granulomatous reaction was also seen, suggestive of a cervical thymic cyst
Discussion
Thymic cysts are very rare representing only about 1 % of cystic cervical masses [2]. The thymus is embryologically derived from the third pharyngeal pouch and descends into the mediastinum. It is initially connected to the pharynx by hollow structures named as “thymopharyngeal ducts”. It is believed that during its path of descent, remnants of thymic tissue may be left behind, leading to formation of a cervical thymic cyst. Speer [3] originally proposed five specific theories of origin for the development of cervical thymic cysts which included epithelial remnants, degenerating Hassall’s corpuscles, infectious/inflammatory product and neoplastic, hyperplastic and involutional changes of the epithelial, lymphoid/connective tissue and vascular elements of the thymus. The two more favoured theories include the persistence of thymopharyngeal ducts (congenital) and the degeneration of Hassall’s corpuscles within ectopic thymic remnants (acquired) [4, 5]. The former hypothesis is well accepted and most consistent with the developmental anatomy of the thymus.
Patients with cervical thymic cysts are more commonly males (males:females 3:2) and usually present in the first decade of life [4]. They usually occur during infancy and childhood, and they are extremely rare in adults [6]. The usual clinical presentation is as a slow growing painless mass in the lateral aspect of neck either deep or superficial to sternocleidomastoid muscle. Huge cervical thymic cysts compressing the neighbouring structures leading to dysphagia, dyspnoea, and hoarseness of voice have also been reported [4]. Being uncommon, they are rarely included in the clinical diagnosis of cervical masses and are commonly misdiagnosed as branchial cysts, lymphatic malformations, epidermoid cysts, dermoid cysts, thyroglossal cysts, lymphadenitis or neoplastic masses. [7].
Ultrasound and CT scans are both useful modalities to assess cervical thymic cysts [8]. On ultrasound, cervical thymic cysts appear as hypoechoic masses with few septae and internal echoes. Thymic cysts appear hypodense and well defined with minimal enhancement of the margins on contrast CT scans. A CT scan additionally helps in surgical planning and assessing the extent of the lesion.
The diagnosis of cervical thymic cysts rarely made preoperatively and histopathological examination of the excised specimen is the only definitive means of diagnosis in a majority of the reported cases [4, 9].
Thymic cysts can be histologically differentiated from the other neck cysts i.e. thyroglossal duct cysts, branchial cleft cysts, cystic hygromas, dermoid cysts, epidermoid cysts and bronchogenic cysts due to the presence of thymic tissue. Further, the frequent atrophic condition of the thymic remnants necessitates a rigorous sampling of the specimen prior to rendering a diagnosis of a cervical thymic cyst. The increasing number of cervical thymic cysts reported over the years probably reflects a greater awareness of this condition among clinicians and pathologists.
For both diagnostic and therapeutic reasons, surgery is the treatment of choice for most neck masses, including cervical thymic cyst [4, 9, 10]. In most cases, removal by a combination of blunt and sharp dissection is all that is required and complete excision is curative. Thymectomy during childhood has been documented to produce impairment of immune status in later life and hence, it is imperative to confirm the presence of mediastinal thymus prior to proceeding with the excision of the cervical thymic cyst and in the absence of which the definitive surgical procedure should be deferred. There has been no reported recurrence and long term prognosis of cervical thymic cysts are excellent.
In conclusion, our case highlights the need for considering cervical thymic cyst, although rare, as a differential diagnosis of lateral neck mass in adults.
Compliance with Ethical Standards
Conflicts of interest
None.
Ethical Issues
All procedures performed in this case report were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Appropriate informed consents have been obtained.
References
- 1.Hsieh YY, Hsueh S, Hsueh C, Lin JN, Luo CC, Lai JY, Huang CS. Pathological analysis of congenital cervical cysts in children: 20 years of experience at Chang Gung Memorial Hospital. Chang Gung Med J. 2003;26:107–113. [PubMed] [Google Scholar]
- 2.Betti M, Hoseini NH, Martin A, Buccoliero A, Messineo A, Ghionzoli M. Cervical thymic cyst in childhood: a case report. Fetal Pediatr Pathol. 2015;34:65–69. doi: 10.3109/15513815.2014.966181. [DOI] [PubMed] [Google Scholar]
- 3.Speer FD. Thymic cysts. Bull N Y Med Coll. 1938;1:142–150. [Google Scholar]
- 4.Nguyen Q, deTar M, Wells W, Crockett D. Cervical thymic cyst: case reports and review of the literature. Laryngoscope. 1996;106(3 Pt 1):247–252. doi: 10.1097/00005537-199603000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Shenoy V, Kamath MP, Hegde MC, Rao Aroor R, Maller VV. Cervical thymic cyst: a rare differential diagnosis in lateral neck swelling. Case Rep Otolaryngol. 2013;2013:350502. doi: 10.1155/2013/350502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alzahrani HA, Iqbal JM, Abu Shaheen AK, Al Harthi BN. Cervical thymic cyst in an adult. Case Rep Surg. 2014;2014:801745. doi: 10.1155/2014/801745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bothale KA, Mahore SD, Karmarkar P, Dongre T. IMAGES: ectopic thymic cyst: a rare case report. Indian J Pathol Microbiol. 2015;58:118–119. doi: 10.4103/0377-4929.151207. [DOI] [PubMed] [Google Scholar]
- 8.Gaddikeri S, Vattoth S, Gaddikeri RS, Stuart R, Harrison K, Young D, Bhargava P. Congenital cystic neck masses: embryology and imaging appearances, with clinicopathological correlation. Curr Probl Diagn Radiol. 2014;43(2):55–67. doi: 10.1067/j.cpradiol.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Jørgensen RL, Larsen SR, Bay M, Godballe C (2014) Cervical thymic cysts are a rare cause of neck masses in children and adolescents. Ugeskr Laeg 176(41) [PubMed]
- 10.Prosser JD, Myer CM., 3rd Branchial cleft anomalies and thymic cysts. Otolaryngol Clin North Am. 2015;48(1):1–14. doi: 10.1016/j.otc.2014.09.002. [DOI] [PubMed] [Google Scholar]



