Abstract
Purpose
This study was performed to compare the condylar position in patients with temporomandibular joint disorders (TMDs) and a normal group by using cone-beam computed tomography (CBCT).
Materials and Methods
In the TMD group, 25 patients (5 men and 20 women) were randomly selected among the ones suffering from TMD according to the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD). The control group consisted of 25 patients (8 men and 17 women) with normal temporomandibular joints (TMJs) who were referred to the radiology department in order to undergo CBCT scanning for implant treatment in the posterior maxilla. Linear measurements from the superior, anterior, and posterior joint spaces between the condyle and glenoid fossa were made through defined landmarks in the sagittal view. The inclination of articular eminence was also determined.
Results
The mean anterior joint space was 2.3 mm in the normal group and 2.8 mm in the TMD group, respectively. The results showed that there was a significant correlation between the superior and posterior joint spaces in both the normal and TMD groups, but it was only in the TMD group that the correlation coefficient among the dimensions of anterior and superior spaces was significant. There was a significant correlation between the inclination of articular eminence and the size of the superior and posterior spaces in the normal group.
Conclusion
The average dimension of the anterior joint space was different between the two groups. CBCT could be considered a useful diagnostic imaging modality for TMD patients.
Keywords: Cone-Beam Computed Tomography, Temporomandibular Joint Disorders, Mandibular Condyle
Introduction
Condylar position is the spatial relationship of mandibular condyle with the glenoid fossa in maximum intercuspation. It is influenced by many dynamic variables such as growing and remodeling, functional matrix activities, occlusion changes, and physiological adaptations.1 The optimum condylar position (centric relationship) is the uppermost and middlemost location facing the articular eminence which coincides with the maximum intercuspation of the teeth in the ideal state.2
The importance of diagnosing mild or moderate eccentricity of condyle is not clear. A low level of condylar eccentricity is seen in one-third to half of normal people, and is not a trustworthy index for assessing the joint soft tissue compartment. Furthermore, the form of the condylar head is not usually harmonious and concentric with the glenoid fossa. A considerably eccentric position of the condyle often reveals a disorder.3 Previous studies have reported that age-related morphological changes such as the flattening of joint compartments can alter the condylar position.4 The relationship between the condyle and glenoid fossa has already been studied by different methods.5
Temporomandibular joint disorder (TMD) is a significant public health problem affecting approximately 5% to 12% of the population.6 TMD is the second most common reason for facial pain after dental pain, and its clinical manifestations include muscular pain, arthralgia, limitation in mandibular movement, and joint sounds. TMD symptoms have a broad prevalence range between 20 and 40 years of age, with a lower prevalence in patients younger and older patients than that range.7 Although the relevance of condylar position and TMD is a controversial issue in temporomandibular joint (TMJ) studies, the prevailing opinion is that the condyle position could be a valuable diagnostic aid in TMDs. It appears that joints with internal derangement tend to have a posterior condyle position.8
Condylar position is clearly associated with disk displacement, especially in joints with reducible disk displacement. The condyle is dislocated posteriorly in these joints compared with those with no disk displacement. In other words, there is a positive correlation between a displaced disk and the condylar position.3,9,10
Functional forces applied to the TMJ may affect its morphology. Most morphological and asymmetric changes in condylar position are related to mandibular deviation during function and dentoskeletal disharmonies.11,12 Usually, clinical examinations cannot diagnose TMJ-related disorders exactly. In most cases, determination of etiologic factors and the right course of treatment are based on imaging.8 Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) is a standardized diagnostic system for TMD that has a dual-axis assessment protocol. Axis I (clinical and radiographic evaluation) is designed to differentiate myofascial pain, disc displacement, and arthralgia, arthritis, and arthrosis. Axis II assesses psychological conditions and pain-related disability.6,13 The purpose of this study was to evaluate the condylar position in patients with TMD and a normal group using cone-beam computed tomography (CBCT).
Materials and Methods
A total of 50 patients were evaluated in this cross-sectional study. Twenty-five patients (5 men and 20 women with the average age of 28.84±9.84 years) were enrolled as the TMD group. According to the RDC/TMD criteria, these patients were suffering from TMD (TMJ pain, limited opening, reciprocal clicking, and crepitus). The normal (control) group consisted of patients (8 men and 17 women with the average age of 28.43±3.24 years) with normal TMJs and Class I occlusion who were referred to the Oral and Maxillofacial Radiology Department of Mashhad Dental School in order to undergo CBCT scanning for implant planning in the posterior maxilla. Both groups were matched in terms of age and the gender. The patients who had previous orthodontic/TMJ treatment, trauma, or congenital craniofacial anomalies were excluded from the survey. IRB approval was obtained and all participants signed the informed consent form.
CBCT scans were obtained from the left and right TMJs with the ProMax 3D (Planmeca, Helsinki, Finland) in closed-mouth and maximum intercuspation position (standard view protocol; field of view=80 mm×80 mm×80 mm; voxel size 0.32 mm; exposure time 12 s). A maxillofacial radiologist and a prosthodontist precisely measured the joint spaces with Romexis® digital imaging software, version 2.9.2 (Planmeca, Helsinki, Finland) on the sagittal slices (slice thickness=0.16 mm). In accordance with the condyle longitudinal axis, the panoramic line was drawn in axial slices, connecting the condylar medial pole to its lateral one. Subsequently, the sagittal slices were obtained perpendicularly to the longitudinal axis of the mandibular condyle. The central sagittal slice, crossing the condylar midpoint, was considered to be the reference slice.14 The investigators were kept blind to the patients' status.
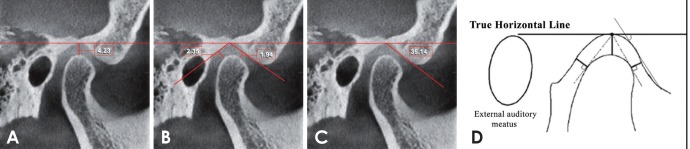
The distance between the uppermost point of the condylar head and the superior site of the glenoid fossa on the true horizontal line was measured as the superior joint space (Fig. 1A).14 In order to measure the anterior and posterior joint spaces, two tangent lines were drawn from the most superior point of the articular cavity on the most prominent part of the anterior and posterior condylar surfaces. The shortest distances between these points to the opposite glenoid fossa wall were measured as anterior and posterior condylar spaces (Fig. 1B).14 To measure the articular eminence inclination, a tangent line was drawn from the uppermost point of the glenoid fossa to the anterior inclination of articular eminence. The angle between this line and a true horizontal line was defined as the articular eminence inclination (Fig. 1C).14
Fig. 1. A. Measurement of the superior joint space. B. The anterior and posterior joint spaces. C. The articular eminence inclination. D. A schematic view.
All variables were distributed normally (one-sample Kolmogorov-Smirnov test). The independent t-test was used to compare mean joint spaces in the two groups. The significance level was set to p<0.05. Data were analyzed with SPSS ver.18 (SPSS Inc., Chicago, IL, USA).
Results
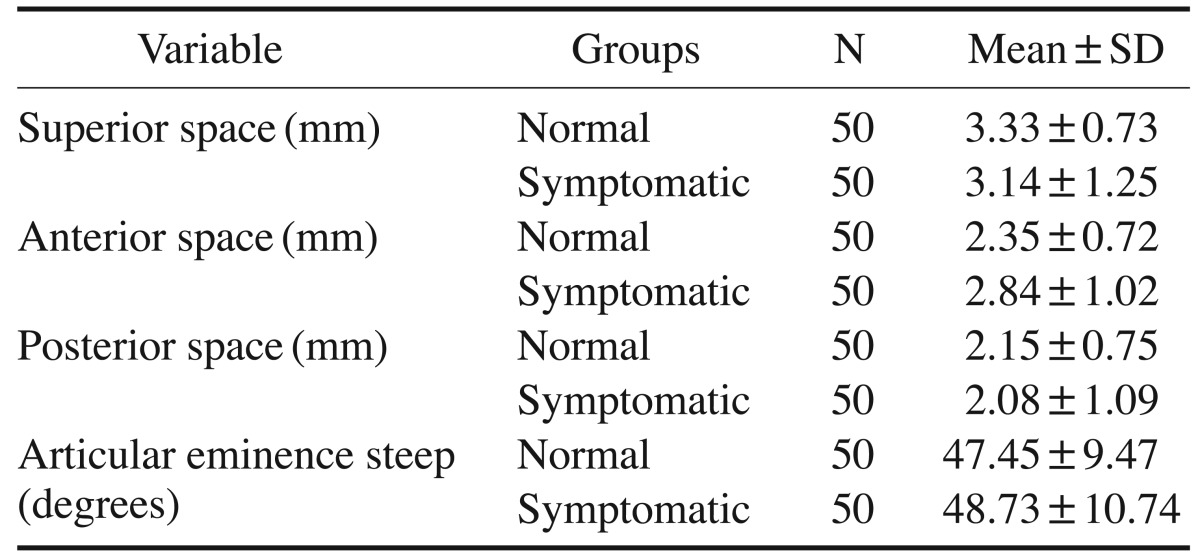
the superior and posterior joint spaces was not significantly different between the normal and TMD groups (p=0.36 and p=0.7, respectively), whereas the mean dimensions of the anterior joint space was larger in the TMD group (p<0.05). The articular eminence inclination did not differ between the normal and TMD patients (p=0.55) (Table 1). Correlation indices were not significant between the age and other quantitative variables in the TMD group.
Table 1. The quantitative variables in normal and temporomandibular disorder groups.
SD: standard deviation
A significant correlation was found between the dimensions of the superior and posterior joint spaces in both normal (p<0.05; r=0.61) and TMD (p<0.05; r=0.51) groups. Furthermore, in the TMD group, the correlation coefficient was significant between the size of superior and anterior joint spaces (p<0.05; r=0.45). There was a significant correlation between the articular eminence inclination and the size of superior and posterior joint spaces in the normal group (r=0.33 and r=0.42, respectively).
Discussion
This study compares the condylar position in normal subjects and patients with TMD. TMD is a heterogeneous category of pathologies affecting the TMJ, jaw muscles, or both.15 It is necessary to understand the anatomy and morphology of the TMJ in order not to misinterpret a normal situation as an abnormality. Various imaging modalities are used in TMJ-related studies. Although magnetic resonance imaging (MRI) is the gold-standard technique for depicting TMJ soft-tissue compartments, CBCT has obvious advantages over it. Greater availability, lower cost and higher accuracy in demonstrating hard-tissue components have made CBCT an acceptable imaging modality for TMJ evaluation.13
The mandibular condyle position is a fundamental factor in diagnosing TMD. Many researchers have proposed that the eccentric condyle position in the glenoid fossa is associated with TMD, whereas others have questioned its clinical significance because of the wide variations in condyle position.8,16,17 Ikeda et al.18 evaluated the CBCT scans of 22 individuals (with the average age of 18 years) in order to review the condylar position in asymptomatic patients. Their reported measures of superior, anterior, and posterior joint spaces were 2.5 mm, 1.3 mm, and 1.6 mm, respectively. Racial diversity and variations in measurement accuracy can justify the difference between other studies' dimensions and our measurements in the normal group (3.3 mm, 2.3 mm, and 2.1 mm for the superior, anterior, and posterior joint spaces). The dimensions of TMJ spaces could be considered diagnostic criteria for TMD.
For the most part, patients with TMD or internal derangement have diverse alterations in the condyle position when compared with the normal group. There is a high association between a retropositioned condyle and higher incidence of TMD. Decreased superior joint space has also been reported in some studies.3,8,19 In our study, the condyle was located slightly more posterior in the patients suffering from TMD. This was in agreement with previous studies. However, the superior joint space did not show a significant difference between the two groups in our survey.
The condylar position was measured in a study carried out on 25 patients (41 joints) with CT scans. It was found that in the TMJs with internal derangement, the anterior and superior joint spaces are wider than normal.20 It is assumed that there is not a meaningful difference between the two genders in the size of the superior, anterior, and posterior joint spaces. Moreover, there was no clear difference between these spaces on the right and left sides. The superior joint space has the greatest size in both genders.21,22,23
In an MRI study, 122 TMJs of 61 patients with TMD were examined. The posterior condyle position was found to be the main feature of TMJs with slight and moderate anterior disc displacement.24 In a similar study, 26 MR images of TMJs with anterior disk displacement (ADD) were evaluated and compared with 14 normal joints. They found that condyles of patients with ADD were situated more posteriorly and superiorly in the glenoid fossa than those in the control group. Furthermore, in the ADD group, the posterior condylar displacement was noted to be 2.4 times greater than the superior condylar displacement. These results indicate that in TMD patients, increased anterior joint space is a more prominent finding than reduced superior joint space. This was consistent with our expectations.25
The correlation between the joint spaces has not been studied previously. In our survey, the superior and posterior joint spaces were correlated significantly in both study groups. Furthermore, the superior and anterior joint space was also correlated in the TMD group. Articular eminence morphology affects articular disk movement, and its inclination is influenced by disc dislocation.4,22,23,26 In the present study, there was only a significant correlation between the articular eminence inclination and the size of superior and posterior joint spaces in the normal group. In addition, the current investigation showed no correlation between the patients' age and the articular eminence inclination.
In conclusion, the anterior joint space is larger in patients with TMD. CBCT imaging can offer useful information about the condylar position and morphology, which can be helpful in diagnosing patients with TMD and people susceptible to TMD.
Footnotes
This study was supported by the Vice Chancellor for Research of Mashhad University of Medical Sciences, in the form of grant No 900211.
References
- 1.Abdel-Fattah RA. Optimum temporomandibular joint (TMJ) condylar position. Todays FDA. 1989;1:1C–3C. [PubMed] [Google Scholar]
- 2.Weffort SY, de Fantini SM. Condylar displacement between centric relation and maximum intercuspation in symptomatic and asymptomatic individuals. Angle Orthod. 2010;80:835–842. doi: 10.2319/090909-510.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonilla-Aragon H, Tallents RH, Katzberg RW, Kyrkanides S, Moss ME. Condyle position as a predictor of temporomandibular joint internal derangement. J Prosthet Dent. 1999;82:205–208. doi: 10.1016/s0022-3913(99)70157-5. [DOI] [PubMed] [Google Scholar]
- 4.Ilguy D, Ilguy M, Fisekcioglu E, Dolekoglu S, Ersan N. Articular eminence inclination, height, and condyle morphology on cone beam computed tomography. ScientificWorldJournal. 2014;2014:761714. doi: 10.1155/2014/761714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arieta-Miranda JM, Silva-Valencia M, Flores-Mir C, Paredes-Sampen NA, Arriola-Guillen LE. Spatial analysis of condyle position according to sagittal skeletal relationship, assessed by cone beam computed tomography. Prog Orthod. 2013;14:36. doi: 10.1186/2196-1042-14-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014;28:6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:453–462. doi: 10.1016/j.tripleo.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 8.Ren YF, Isberg A, Westesson PL. Condyle position in the temporomandibular joint. Comparison between asymptomatic volunteers with normal disk position and patients with disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:101–107. doi: 10.1016/s1079-2104(95)80025-5. [DOI] [PubMed] [Google Scholar]
- 9.Ronquillo HI, Guay J, Tallents RH, Katzberg RW, Murphy W. Tomographic analysis of mandibular condyle position as compared to arthrographic findings of the temporomandibular joint. J Craniomandib Disord. 1988;2:59–64. [PubMed] [Google Scholar]
- 10.Kurita H, Ohtsuka A, Kobayashi H, Kurashina K. A study of the relationship between the position of the condylar head and displacement of the temporomandibular joint disk. Dentomaxillofac Radiol. 2001;30:162–165. doi: 10.1038/sj/dmfr/4600603. [DOI] [PubMed] [Google Scholar]
- 11.Rodrigues AF, Fraga MR, Vitral RW. Computed tomography evaluation of the temporomandibular joint in Class I malocclusion patients: condylar symmetry and condyle-fossa relationship. Am J Orthod Dentofacial Orthop. 2009;136:192–198. doi: 10.1016/j.ajodo.2007.07.032. [DOI] [PubMed] [Google Scholar]
- 12.Vitral RW, Telles Cde, S, Fraga MR, de Oliveira, RS, Tanaka OM. Computed tomography evaluation of temporomandibular joint alterations in patients with class II division 1 subdivision malocclusions: condyle-fossa relationship. Am J Orthod Dentofacial Orthop. 2004;126:48–52. doi: 10.1016/j.ajodo.2003.06.012. [DOI] [PubMed] [Google Scholar]
- 13.Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:844–860. doi: 10.1016/j.tripleo.2009.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol. 2004;33:196–201. doi: 10.1259/dmfr/27403192. [DOI] [PubMed] [Google Scholar]
- 15.McNeill C. Management of temporomandibular disorders: concepts and controversies. J Prosthet Dent. 1997;77:510–522. doi: 10.1016/s0022-3913(97)70145-8. [DOI] [PubMed] [Google Scholar]
- 16.Martin D, Rozencweig S, Maté A, Valenzuela J. The importance of condyle position in the diagnosis, treatment and prevention of TMD. Orthod Fr. 2015;86:125–149. doi: 10.1051/orthodfr/2015018. [DOI] [PubMed] [Google Scholar]
- 17.Dalili Z, Khaki N, Kia SJ, Salamat F. Assessing joint space and condylar position in the people with normal function of temporomandibular joint with cone-beam computed tomography. . Dent Res J (Isfahan) 2012;9:607–612. doi: 10.4103/1735-3327.104881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ikeda K, Kawamura A. Assessment of optimal condylar position with limited cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;135:495–501. doi: 10.1016/j.ajodo.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 19.Fernández Sanromán J, Gómez González JM, del Hoyo JA. Relationship between condylar position, dentofacial deformity and temporomandibular joint dysfunction: an MRI and CT prospective study. J Craniomaxillofac Surg. 1998;26:35–42. doi: 10.1016/s1010-5182(98)80033-4. [DOI] [PubMed] [Google Scholar]
- 20.Christiansen EL, Thompson JR, Zimmerman G. Computed tomography of condylar and articular disk positions within the temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1987;64:757–767. doi: 10.1016/0030-4220(87)90182-4. [DOI] [PubMed] [Google Scholar]
- 21.Al-koshab M, Nambiar P, John J. Assessment of condyle and glenoid fossa morphology using CBCT in South-East Asians. PLoS One. 2015;10:e0121682. doi: 10.1371/journal.pone.0121682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sulun T, Cemgil T, Duc JM, Rammelsberg P, Jager L, Gernet W. Morphology of the mandibular fossa and inclination of the articular eminence in patients with internal derangement and in symptom-free volunteers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:98–107. doi: 10.1067/moe.2001.114621. [DOI] [PubMed] [Google Scholar]
- 23.Kurita H, Ohtsuka A, Kobayashi H, Kurashina K. Flattening of the articular eminence correlates with progressive internal derangement of the temporomandibular joint. Dentomaxillofac Radiol. 2000;29:277–279. doi: 10.1038/sj/dmfr/4600542. [DOI] [PubMed] [Google Scholar]
- 24.Incesu L, Taşkaya-Yılmaz N, Öğütcen-Toller M, Uzun E. Relationship of condylar position to disc position and morphology. Eur J Radiol. 2004;51:269–273. doi: 10.1016/S0720-048X(03)00218-3. [DOI] [PubMed] [Google Scholar]
- 25.Gateno J, Anderson PB, Xia JJ, Horng JC, Teichgraeber JF, Liebschner MA. A comparative assessment of mandibular condylar position in patients with anterior disc displacement of the temporomandibular joint. J Oral Maxillofac Surg. 2004;62:39–43. doi: 10.1016/j.joms.2003.05.006. [DOI] [PubMed] [Google Scholar]
- 26.Kinniburgh RD, Major PW, Nebbe B, West K, Glover KE. Osseous morphology and spatial relationships of the temporomandibular joint: comparisons of normal and anterior disc positions. Angle Orthod. 2000;70:70–78. doi: 10.1043/0003-3219(2000)070<0070:OMASRO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]