Abstract
Purpose
The aim of this study was to assess and compare the diagnostic performance of panoramic and occlusal radiographs in detecting submandibular sialoliths.
Materials and Methods
A total of 40 patients (20 cases and 20 controls) were included in this retrospective study. Cases were defined as subjects with a submandibular sialolith confirmed by computed tomography (CT), whereas controls did not have any submandibular calcifications. Three observers with different expertise levels assessed panoramic and occlusal radiographs of all subjects for the presence of sialoliths. Intraobserver and interobserver agreement were assessed using the kappa test. Sensitivity, specificity, accuracy, positive and negative predictive values, and the diagnostic odds ratio of panoramic and occlusal radiographs in screening for submandibular sialoliths were calculated for each observer.
Results
The sensitivity and specificity values for occlusal and panoramic radiographs all ranged from 80% to 100%. The lowest values of sensitivity and specificity observed among the observers were 82.6% and 80%, respectively (P=0.001). Intraobserver and interobserver agreement were higher for occlusal radiographs than for panoramic radiographs, although panoramic radiographs demonstrated a higher overall accuracy.
Conclusion
Both panoramic and occlusal radiographic techniques displayed satisfactory diagnostic performance and should be considered before using a CT scan to detect submandibular sialoliths.
Keywords: Radiography, Panoramic; Radiography, Dental; Salivary Gland Calculi; Multidetector Computed Tomography
Introduction
Sialolithiasis is one of the most prevalent large obstructive disorders of the major salivary glands, and originates from the deposition of calcium salts around accumulations of organic debris consisting of mucous substances,1 ductal epithelial cells, bacteria, or even foreign bodies, thereby forming so-called sialoliths.2 The submandibular gland is the most commonly affected gland (80%-92% of cases).3,4 The severity of symptoms depends on the extent of salivary duct obstruction, as well as the presence of a secondary infection. The main clinical features are pain and swelling associated with eating - an activity involving increased salivary flow - and subsequent sialadenitis.5,6
Conventional radiographs have been used for diagnosing submandibular sialoliths.7 However, approximately 20% of sialoliths are poorly calcified and thus are not visible in two-dimensional radiographic images.8,9 Furthermore, radiopaque calcifications may be superimposed on the mandible. Non-contrast computed tomography (CT) has emerged as a standard method of diagnosing salivary stones in the United States.7,10 This is mainly because CT allows the assessment of soft-tissue details such as the glandular parenchyma, which may demonstrate associated sialadenitis. Moreover, in cases of abscesses associated with sialadenitis or a suspected malignant lesion, CT may be recommended to assess soft tissue conditions and the possibility of infiltration of the bone or deep structures. 11,12 Nevertheless, CT has disadvantages, such as a high cost and the fact that it involves administering large doses of radiation to the patient.13
For surgical planning, the choice of an imaging method for diagnosing sialoliths depends on the complexity of the case.7 In a recent clinical study, most surgical procedures to remove submandibular sialoliths only required conventional plain-film radiographs (i.e., occlusal and panoramic radiographs), whereas 14% of the cases additionally required CT scans in order to determine the three-dimensional location of the sialolith precisely.14 Therefore, it can be hypothesized that conventional radiography, including occlusal and panoramic radiographs, may have comparable levels of precision and accuracy for the detection of sialoliths. Furthermore, since the diagnostic requirements depend on the complexity of the case, we also hypothesized that the degree of experience and expertise of the observer could affect the results.
Thus, the aim of this study was to assess and compare the diagnostic performance of panoramic and occlusal radiographs in screening for submandibular sialoliths.
Materials and Methods
Subjects
This diagnostic study was conducted using radiographic images from the archives of the Department of Oral and Maxillofacial Radiology, Field of Tumor Biology of the Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences. All patients who participated in this study signed an informed consent form. The approval for conducting this retrospective analysis was obtained from the Ethics Committee of the University of São Paulo (protocol No. 569.107). The Standards for the Reporting of Diagnostic Accuracy15 and the guidelines of the Helsinki Declaration were followed in this investigation.
Inclusion and exclusion criteria
All radiographic images included in this study were obtained and analyzed consecutively between July 2013 and September 2014. All subjects underwent occlusal and panoramic radiography. In addition, all subjects had a CT scan (taken during dental treatment) that was analyzed to confirm the presence or absence of any sialolith, as previously described in the literature.16,17 Subjects were then classified into cases and controls. Cases were defined as subjects with a submandibular sialolith, as confirmed in CT scans analyzed by two experienced radiologists, whereas controls did not present any detectable submandibular calcification.
Patients with recent mandibular tooth extractions (less than 6 months of follow-up) were excluded in order to avoid the socket-remodeling period. Patients with metabolic disorders, such as diabetes and vitamin D deficiency, were excluded, as well as patients with other oral pathologies, bone disorders, or pathologic calcifications.
Radiographic methods
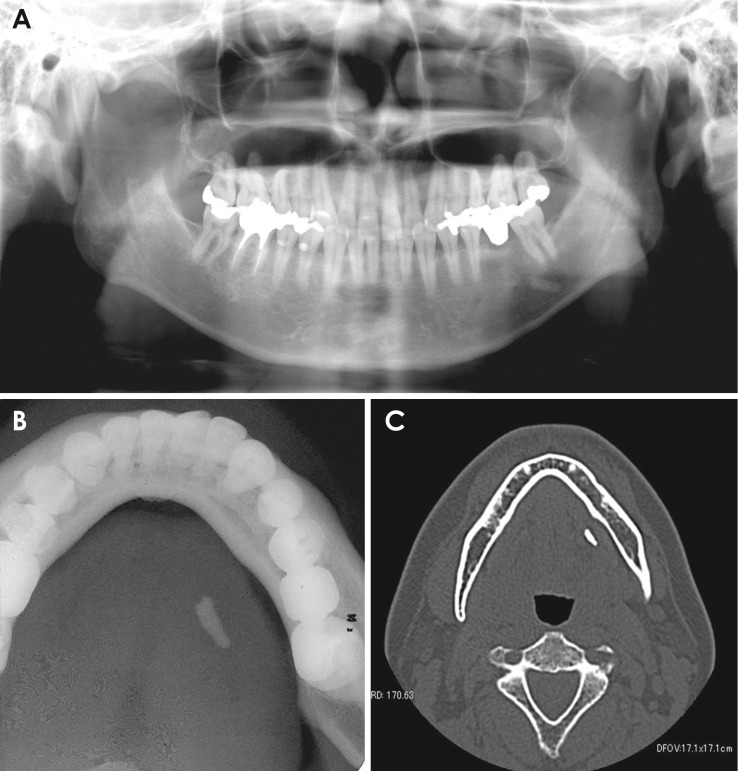
Digital panoramic radiographs were taken using a Veraviewepocs 2D apparatus (Morita, Tokyo, Japan; exposure conditions: 60 kV, 4 mA, 0.5 mm copper filter). Images were analyzed using the ImageJ® software (National Institute of Health, Bethesda, MD, USA). Briefly, images were corrected using a magnification factor of 1.3. Spatial calibration was set at a scale of 1 pixel per 96 µm (Fig. 1A).
Fig. 1. Radiographic images of submandibular sialoliths. A. Panoramic radiography, B. Occlusal radiography, C. Computed tomographic axial image.
Occlusal mandibular radiographs were obtained using an intraoral X-ray device (Veraview iX; J Morita Corporation, Kyoto, Japan) operating at 70 kV and with an exposure time of 0.12 s. For the occlusal radiographs, 6×8 cm F Speed film (Kodak Insight dental film; Eastman Kodak Company, Rochester, NY, USA) was used. The central beam was positioned through the median sagittal plane, corresponding to an angle of 70° in relation to the film (Fig. 1B). All images were digitized on a flatbed image scanner (Epson expression 10000XL, Long Beach, CA, USA) with a spatial resolution of 600 dots per inch and 8-bit depth contrast resolution.
Multislice CT datasets were obtained using a GE Light Speed Pro32 (GE Healthcare, Milwaukee, WI, USA) spiral CT scanner with a slice thickness of 1 mm and field of view of 36-38 mm, Digital Imaging Communication in Medicine (DICOM) images were assessed using a DICOM viewer (OsiriX® 6.0 version, Pixmeo, Geneva, Switzerland) (Fig. 1C).
Data analysis
Images were analyzed using the ImageJ® software. All observations were performed using the computer monitors. The images from the occlusal and panoramic radiographs were viewed on a single liquid crystal display monitor (Dell Ultrasharp 2408WFP-24'' Widescreen Flat Panel Monitors, Round Rock, TX, USA), which was set at its optimal resolution (1920×1200). The color quality was set at 16 bit, which was the highest depth supported by the hardware of the CBCT device.
Since occlusal and panoramic radiography are commonly available in clinical and academic environments, all observations of images obtained using these methods were made in a random order by 3 trained observers with different expertise levels. Observer 1 was an undergraduate student, Observer 2 was an oral maxillofacial radiologist, and Observer 3 was an oral surgeon and PhD student in oral radiology.
Intraobserver reliability was assessed based on two sets of observations performed 2 weeks apart to eliminate memory bias. All images were assessed in a quiet, dimly lit room in three sessions (n=20 exams in each session). The examiners were asked to diagnose the presence or absence of radiopaque bodies in the area of the submandibular gland in both cases and controls in order to calculate sensitivity and specificity.
Statistical analysis
The sample size was determined with the goal of detecting a minimum diagnostic odds ratio of 5 and to give the study a power of 80% at a level of significance of 5%. Intraobserver and interobserver agreement were assessed using the kappa test. Furthermore, the mean sensitivity and specificity of occlusal and panoramic radiographs for screening sialoliths were also calculated for each observer. The overall accuracy, positive and negative predictive values, and diagnostic odds ratio were also calculated for both radiographic examinations. The significance of the results was assessed with Fisher's exact test. P-values <.05 were considered to indicate statistical significance.
All statistical analyses were performed using SPSS version 17 (SPSS Inc., Chicago, IL, USA).
Results
A total of 40 patients (20 cases and 20 controls) were included in the study. The case group (Fig. 1) had a mean age of 60.6±9.8 years, whereas the control group had a mean age of 56.2±7.7 years. In the case group, a higher prevalence of sialoliths was noted in women (70%) than in men (30%), and all sialoliths analyzed were unilateral. However, sialoliths were more prevalent on the right side (65%) than on the left side (35%).
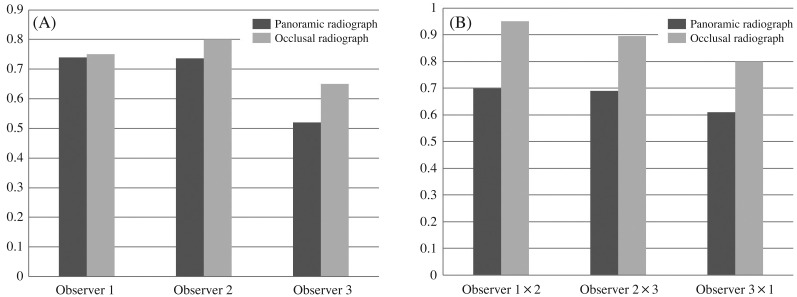
Significant levels of intraobserver and interobserver agreement (Fig. 2A, Fig. 2B, respectively) were confirmed for both techniques analyzed herein (P<0.05). The kappa values for the occlusal radiographs were higher than those for panoramic radiographs. For intraobserver agreement, the lowest kappa value was 0.52 (P=0.03) for panoramic radiographs and 0.64 (P=0.01) for occlusal radiographs, indicating a minimum of moderate to substantial agreement. For interobserver agreement, the lowest kappa value was 0.61 (P=0.01) for panoramic radiographs and 0.80 (P=0.001) for occlusal radiographs, indicating at least substantial agreement.
Fig. 2. Diagnostic performance results with 95% confidence intervals. A. Kappa values for intraobserver agreement. B. Kappa values for interobserver agreement.
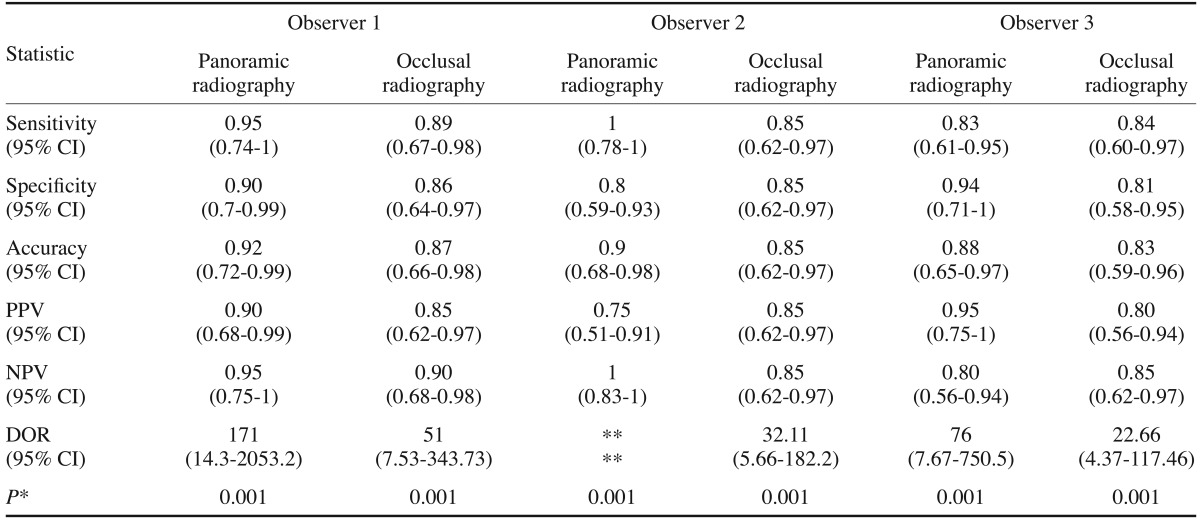
The mean sensitivity and specificity for both the occlusal and panoramic techniques ranged from 80% to 100%, indicating good performance in diagnosing sialoliths (Table 1). A minimum sensitivity of 82.6% and a minimum specificity of 80% were found among the observers. The panoramic radiographs exhibited greater overall accuracy than the occlusal radiographs, and this held true for all observers. All results indicative of diagnostic performance were statistically significant for all observers (P=0.001).
Table 1. Diagnostic performance of occlusal and panoramic radiographs for screening submandibular sialoliths.
CI: confidence interval, PPV: positive predictive value, NPV: negative predictive value, DOR: diagnostic odds ratio, *: Significance according to the Fisher's exact test (P<0.05 indicates statistical significance), **: Odds ratio infinity
Discussion
In the present study, all submandibular sialoliths were unilateral, and were observed more frequently on the right side (65%) and in women (70%), corresponding to findings from other studies.3,18 According to our results, panoramic and occlusal radiographs demonstrated satisfactory precision and accuracy for the detection of sialoliths (P=0.001), as confirmed by the observation of high positive predictive values (i.e., the probability that a sialolith is present when the test is positive) and high negative predictive values (i.e., the probability that a sialolith is not present when the test is negative). This finding is in contrast with those of another study that concluded that plain radiographs are not suitable for the diagnosis of calcified inflammatory diseases.19 However, while panoramic radiographs demonstrated greater overall accuracy, occlusal radiographs exhibited greater precision, as reflected by intraobserver and interobserver agreement. To our knowledge, this is the first study to address this question using clinically available radiographic methods. The lower precision of panoramic radiographs may have been caused by the overlapping image of the mandibular bone where the sialolith was located, which is a type of distortion that occurs frequently in panoramic radiographic images. Furthermore, overlapping images in the body of the mandible could additionally lead to misdiagnoses including sclerosis, logs, bone dysplasia, and other bone lesions.
Sialoliths remaining in the salivary glands may lead to the occurrence of secondary infections and cause purulent drainage through the duct; the tissues overlying the gland appear edematous, hyperemic, and sensible to palpation.6 Surgical removal is recommended when the salivary gland is permanently damaged by infection, obstruction,20 or in cases where the sialolith is located inside the gland parenchyma.16,21 In these cases, CT scans are useful for accurately assessing the three-dimensional position of the sialolith, which could minimize the extent and morbidity of the procedure performed to treat the sialolith.
This study also attempted to assess differences in precision among observers with different levels of expertise. Contrary to our expectations, the experience of each observer in the field of radiology did not significantly influence the results of this study. However, Observer 2, who had more extensive expertise in clinical oral radiology, exhibited 100% sensitivity in detecting sialoliths with panoramic radiography, which may indicate the potentially high level of accuracy of this method. However, one limitation of this study is that the present results apply only to sialoliths that have become calcified enough to be visualized using radiographic methods. Smaller and radiolucent sialoliths are usually diagnosed and treated using sialendoscopy,14 and therefore were not considered in this study.
In conclusion, unless determining the three-dimensional location of a sialolith is absolutely required for surgical planning, panoramic and occlusal radiographic techniques can be considered viable diagnostic tools for screening for submandibular sialolithiasis, as they exhibited satisfactory diagnostic performance for this purpose.
Footnotes
A postdoctoral scholarship was granted to A.R.G.C. by the National Council for Scientific and Technological Development CNPq - Science Without Borders, Brazil, N°232643/2013-0.
References
- 1.Williams MF. Sialolithiasis. Otolaryngol Clin North Am. 1999;32:819–834. doi: 10.1016/s0030-6665(05)70175-4. [DOI] [PubMed] [Google Scholar]
- 2.Marchal F, Kurt AM, Dulguerov P, Lehmann W. Retrograde theory in sialolithiasis formation. Arch Otolaryngol Head Neck Surg. 2001;127:66–68. doi: 10.1001/archotol.127.1.66. [DOI] [PubMed] [Google Scholar]
- 3.Lustmann J, Regev E, Melamed Y. Sialolithiasis. A survey on 245 patients and a review of the literature. Int J Oral Maxillofac Surg. 1990;19:135–138. doi: 10.1016/s0901-5027(05)80127-4. [DOI] [PubMed] [Google Scholar]
- 4.Gritzmann N. Sonography of the salivary glands. AJR Am J Roentgenol. 1989;153:161–166. doi: 10.2214/ajr.153.1.161. [DOI] [PubMed] [Google Scholar]
- 5.Schwarz D, Kabbasch C, Scheer M, Mikolajczak S, Beutner D, Luers JC. Comparative analysis of sialendoscopy, sonography, and CBCT in the detection of sialolithiasis. Laryngoscope. 2015;125:1098–1101. doi: 10.1002/lary.24966. [DOI] [PubMed] [Google Scholar]
- 6.Markiewicz MR, Margarone JE, 3rd, Tapia JL, Aguirre A. Sialolithiasis in a residual Wharton's duct after excision of a submandibular salivary gland. J Laryngol Otol. 2007;121:182–185. doi: 10.1017/S0022215106003525. [DOI] [PubMed] [Google Scholar]
- 7.Sobrino-Guijarro B, Cascarini L, Lingam RK. Advances in imaging of obstructed salivary glands can improve diagnostic outcomes. Oral Maxillofac Surg. 2013;17:11–19. doi: 10.1007/s10006-012-0327-8. [DOI] [PubMed] [Google Scholar]
- 8.Becker M, Marchal F, Becker CD, Dulguerov P, Georgakopoulos G, Lehmann W, et al. Sialolithiasis and salivary ductal stenosis: diagnostic accuracy of MR sialography with a three-dimensional extended-phase conjugate-symmetry rapid spin-echo sequence. Radiology. 2000;217:347–358. doi: 10.1148/radiology.217.2.r00oc02347. [DOI] [PubMed] [Google Scholar]
- 9.Jager L, Menauer F, Holzknecht N, Scholz V, Grevers G, Reiser M. Sialolithiasis: MR sialography of the submandibular duct - an alternative to conventional sialography and US? Radiology. 2000;216:665–671. doi: 10.1148/radiology.216.3.r00se12665. [DOI] [PubMed] [Google Scholar]
- 10.Madani G, Beale T. Inflammatory conditions of the salivary glands. Semin Ultrasound CT MR. 2006;27:440–451. doi: 10.1053/j.sult.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Zenk J, Koch M, Klintworth N, König B, Konz K, Gillespie MB, et al. Sialendoscopy in the diagnosis and treatment of sialolithiasis: a study on more than 1000 patients. Otolaryngol Head Neck Surg. 2012;147:858–863. doi: 10.1177/0194599812452837. [DOI] [PubMed] [Google Scholar]
- 12.Bialek EJ, Jakubowski W, Zajkowski P, Szopinski KT, Osmolski A. US of the major salivary glands: anatomy and spatial relationships, pathologic conditions, and pitfalls. Radiographics. 2006;26:745–763. doi: 10.1148/rg.263055024. [DOI] [PubMed] [Google Scholar]
- 13.Bodner L. Giant salivary gland calculi: diagnostic imaging and surgical management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:320–323. [PubMed] [Google Scholar]
- 14.Vaiman M. Comparative analysis of methods of endoscopic surgery of the submandibular gland: 114 surgeries. Clin Otolaryngol. 2015;40:162–166. doi: 10.1111/coa.12357. [DOI] [PubMed] [Google Scholar]
- 15.Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, et al. Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. Standards for Reporting of Diagnostic Accuracy. Clin Chem. 2003;49:1–6. doi: 10.1373/49.1.1. [DOI] [PubMed] [Google Scholar]
- 16.Ardekian L, Klein HH, Araydy S, Marchal F. The use of sialendoscopy for the treatment of multiple salivary gland stones. J Oral Maxillofac Surg. 2014;72:89–95. doi: 10.1016/j.joms.2013.06.206. [DOI] [PubMed] [Google Scholar]
- 17.Yousem DM, Kraut MA, Chalian AA. Major salivary gland imaging. Radiology. 2000;216:19–29. doi: 10.1148/radiology.216.1.r00jl4519. [DOI] [PubMed] [Google Scholar]
- 18.Nahlieli O, Eliav E, Hasson O, Zagury A, Baruchin AM. Pediatric sialolithiasis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:709–712. doi: 10.1067/moe.2000.109075a. [DOI] [PubMed] [Google Scholar]
- 19.Zenk J, Iro H, Klintworth N, Lell M. Diagnostic imaging in sialadenitis. Oral Maxillofac Surg Clin North Am. 2009;21:275–292. doi: 10.1016/j.coms.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 20.McGurk M, Makdissi J, Brown JE. Intra-oral removal of stones from the hilum of the submandibular gland: report of technique and morbidity. Int J Oral Maxillofac Surg. 2004;33:683–686. doi: 10.1016/j.ijom.2004.01.024. [DOI] [PubMed] [Google Scholar]
- 21.Koch M, Zenk J, Iro H. Algorithms for treatment of salivary gland obstructions. Otolaryngol Clin North Am. 2009;42:1173–1192. doi: 10.1016/j.otc.2009.08.002. [DOI] [PubMed] [Google Scholar]