Abstract
Aim of the study
Aim of the study was to investigate the demographics of Ewing sarcoma family of tumours (ESTF) patients, treatment alternatives, clinical outcomes, and prognostic factors for survival.
Material and methods
We retrospectively reviewed 39 patients with ESFT who were admitted to our institute between September 2008 and September 2012.
Results
The patients included 32 (82.1%) males and seven (17.9%) females of median age 24 (range, 18–66) years. Among the 27 patients with a primary osseous localization, 17 (43.5%) had a central axis localization. Fifteen patients (38.5%) had metastases at the time of diagnosis. Patients were followed up for a median period of 18 (range, 2–134) months. The median event-free survival (EFS) was 23 (range, 1–64) months, and the 1- and 4-year EFS were 60% and 48%, respectively. The median overall survival (OS) was 91 (range, 1–188) months, and the 1- and 4-year OS were 78% and 54%, respectively. Gender, age, primary tumor site, and local treatment modalities, either alone or in combination, did not have a significant effect on OS (p = 0.210, p = 0.617, p = 0.644, and p = 0.417, respectively). In contrast, osseous site of peripheral localization, limited stage, and metastasis to the bone significantly affected OS (p = 0.015, p < 0.001, and p = 0.042, respectively).
Conclusions
ESFTs are aggressive tumors with a high rate of relapse and metastatic potential. Patients with peripheral bone involvement and limited stage had a good prognosis. Appropriate surgical resection, radiotherapy, and aggressive chemotherapy regimens are recommended.
Keywords: Ewing's sarcoma family of tumors, adult, treatment
Introduction
Ewing's sarcoma (ES), primitive neuroectodermal tumor (PNET), Askin's tumor, PNET of the bone, and extraosseous ES together form the Ewing sarcoma family of tumors (ESFT) [1–4]. These tumors originate from the neuroectoderm and are composed of undifferentiated neuroepithelial cells that have the capacity to differentiate into neuronal, neuroglial, or other mesenchymal cell types. ESFTs derive from small, round blue cells and are periodic acid-Schiff (PAS)- and CD99 (MIC2)-positive [5]. The annual incidence and mortality rates are 0.1/100,000 and 0.05/100,000, respectively [6]. ESFT exhibits an irregular geographic pattern of incidence. Caucasians are affected much more often, whereas the rates are much lower in East Asian and African populations [7]. ESFT is considered to be a pediatric malignancy, with ∼80% of cases occurring before the age of 18 years [8]. Diagnosis is often determined during the second decade of life. Approximately 20–30% of patients are younger than 10 years of age, and the frequency declines with increasing age [4, 6, 9].
Diagnosis is made by biopsy followed by histology, immunohistochemical staining, molecular pathology, and biobanking. Molecular pathology studies have revealed a common gene rearrangement involving the ES gene on chromosome 22 [10]. Certain translocations of the ES gene have been identified, the most frequent of which is t(11;22)(q24;q12), although t(21;22)(q22;q12) also occurs [6]. Most lesions in children arise from the bone, whereas ≥ 50% of lesions in adults occur in the soft tissue [10]. Before to the use of multi-drug chemotherapy, long-term survival was < 10% with surgery or radiotherapy alone [11]. Systemic chemotherapy is effective for microscopic and macroscopic metastasis, in addition to its effects on tumor volume depletion. Chemotherapy combined with surgery and/or radiotherapy is used to achieve local control of this disease. Survival is 60–70% in patients with localized disease, compared with 20–40% in those with metastatic disease [4, 9, 12, 13]. The aim of this retrospective study was to investigate the demographics of ESTF patients, treatment alternatives, clinical outcomes, and prognostic factors for survival.
Material and methods
We retrospectively evaluated ESFT patients aged ≥ 18 years who were admitted to the medical oncology outpatient clinic of the Ankara Oncology Education and Research Hospital between September 2008 and September 2012. Age, gender, primary tumor location, stage, site of metastasis, the presence of surgical operation, radiotherapy, chemotherapy, and the treatments administered were recorded. The tumor was considered to be central or peripheral when its primary localization was confined to the trunk and pelvis or to the limbs, respectively. Event-free survival (EFS) was defined as the time from diagnosis to disease recurrence, progression, disease-related death, or toxicity-related chemotherapy. Overall survival (OS) was defined as the time from the date of diagnosis to death or last contact.
Statistical analyses
Data were analyzed using SPSS software (ver. 16 for Windows; SPSS Inc., Chicago, IL, USA). Continuous variables are presented as medians (ranges) and categorical variables as numbers (percentages). A p-value ≤ 0.05 was considered to indicate statistical significance. Kaplan-Meier survival analyses followed by log-rank tests were used to identify significant relationships among EFS, categorical variables, and OS. The median EFS and OS values, 95% confidence intervals (95% CI), and standard deviations were calculated for all variables. The significance of the effects of categorical variables on survival was assessed using multivariate Cox's proportional hazard regression analysis. The relative risk and 95% CI were calculated for all variables.
Results
A total of 39 patients with ESFT were followed up and treated at our clinic. The median age of the patients was 24 (range, 18–66) years. Thirty-two patients (82.1%) were male, and seven (17.9%) were female. Nine patients (23%) were < 19 years of age, whereas 30 (77%) were ≥ 20 years. Tumors arose from an osseous site in 27 patients (69.2%) and an extraosseous site in 12 (30.8%). In patients with a primary osseous tumor, 10 (25.7%) were located in the extremities and 17 (43.5%) in the axial skeleton. The extraosseous primary tumor location sites included the lymph node (five cases, 12.8%), lungs (three cases, 7.7%), brain (three cases, 7.7%), and uterus (one case, 2.6%). Twenty-four patients (61.5%) who did not have any metastasis at the time of diagnosis were considered to be in the “limited stage”. Fifteen patients (38.5%) had metastases at the time of diagnosis. The most common sites of metastasis were bone in nine cases (23.1%) and bone plus lung in three (7.7%). Regarding treatment, two (5.2%) patients did not agree to undergo chemotherapy: one underwent surgery only and the other radiotherapy only. Eight patients (20.5%) received chemotherapy alone, one died of febrile neutropenia due to the toxic effects of chemotherapy, and one developed recurrence while on chemotherapy prior to local treatment. In addition, six patients who were at the metastatic stage at the time of diagnosis received chemotherapy alone, rather than alternating chemotherapy with local treatment of surgery and/or radiotherapy. For local treatment in addition to chemotherapy, 14 (35.9%) patients underwent surgery, eight (20.5%) radiotherapy, and seven (17.9%) both radiotherapy and surgery (Table 1).
Table 1.
Clinical characteristics of patients
| Parameter | n | % |
|---|---|---|
| Gender | ||
| male | 32 | 82.1 |
| female | 7 | 17.9 |
| Age of diagnosis | ||
| ≤ 19 | 9 | 23 |
| ≥ 20 | 30 | 77 |
| Primary tumor site | ||
| osseous | 27 | 69.2 |
| extraosseous | 12 | 30.8 |
| Extraosseous site | ||
| lymph node | 5 | 12.8 |
| lung | 3 | 7.7 |
| brain | 3 | 7.7 |
| uterus | 1 | 2.6 |
| Osseous site | ||
| extremity | 10 | 25.7 |
| axial skeleton | 17 | 43.5 |
| Stage | ||
| limited | 24 | 61.5 |
| metastatic | 15 | 38.5 |
| Site of metastasis | ||
| osseous | 10 | 66.7 |
| extraosseous | 5 | 33.3 |
| Treatment modalities | ||
| surgery alone | 1 | 2.6 |
| radiotherapy alone | 1 | 2.6 |
| chemotherapy alone | 8 | 20.5 |
| surgery/chemotherapy | 14 | 35.9 |
| radiotherapy/chemotherapy | 8 | 20.5 |
| radiotherapy/surgery/chemotherapy | 7 | 17.9 |
Apart from the two patients who chose not to receive chemotherapy, 31 (79.5%), including nine of the 15 patients with metastasis at the time of diagnosis, were administered an alternating chemotherapy regimen every 3 weeks for a total of 17 cycles, consisting of cyclophosphamide (1,200 mg/m2/day on day 1) / adriamycin (75 mg/m2/day on day 1) / vincristine (maximum 2 mg/day on day 1) (CAV) or ifosfamide (1.8 g/m2/day, days 1–5) / etoposide (100 mg/m2/day, days 1–5) (IE) as the first-line chemotherapy. Local treatment, which was planned for week 12, included radiation therapy, surgery, or both [12]. Of the six remaining patients who had metastasis at the time of diagnosis, three (7.7%) underwent CAV chemotherapy, one (2.6%) IE chemotherapy (2.5 g/m2/day ifosfamide, days 1–3; 120 mg/m2/day etoposide, days 1–3), one (2.6%) VCE chemotherapy, and one (2.6%) cisplatin (60 mg/m2/day on day 1) plus adriamycin (60 mg/m2/day on day 1) chemotherapy.
The median follow-up period of the patients was 18 (range, 2–134) months. At the end of this period, 16 patients (41%) had died, one due to the toxic effects of chemotherapy and 15 due to disease progression. The median EFS was 23 months (95% CI: 1–64), the 1-year general EFS was 60%, and the 4-year general EFS was 48%. Gender, age, site of the primary tumor, surgery, radiotherapy, or local treatment with chemotherapy (surgery and radiotherapy, alone or in combination) did not have a significant effect on EFS (p = 0.547, p = 0.922, p = 0.708, p = 0.111, p = 0.673, and p = 0.534, respectively). However, an osseous site of peripheral localization, limited stage, or bone metastasis correlated significantly with EFS (p = 0.005, p < 0.001, and p = 0.07, respectively).
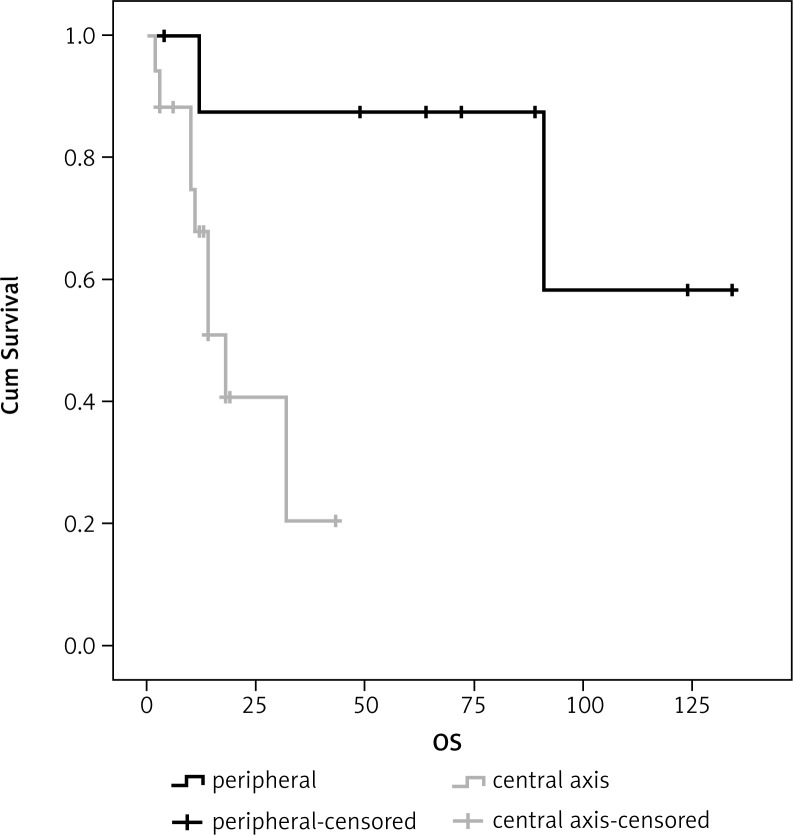
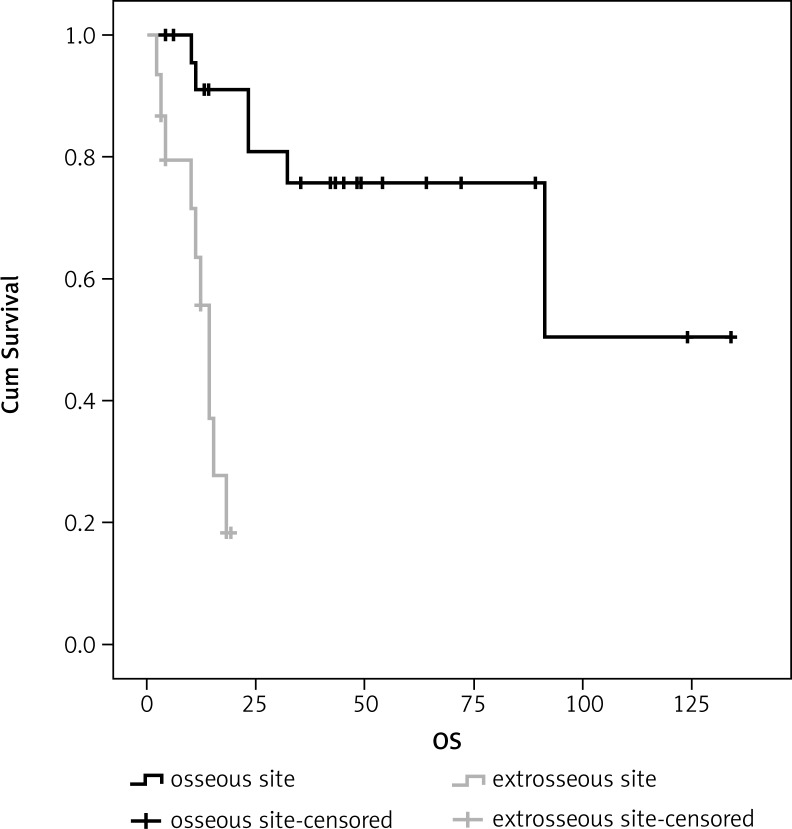
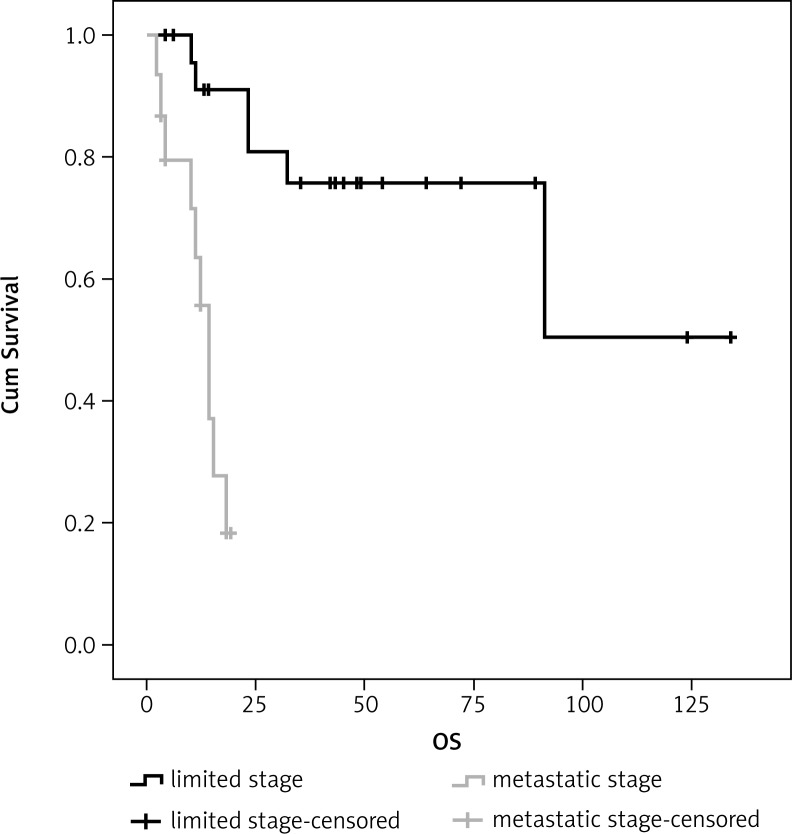
The median OS, 1-year general OS, and 4-year general OS were 91 months (95% CI: 1–188), 78%, and 54%, respectively. Gender, age, primary site of the tumor, or the treatment used for local control in addition to chemotherapy (surgery and radiotherapy, alone or in combination) did not have a significant effect on OS (p = 0.210, p = 0.617, p = 0.644, and p = 0.417, respectively). However, peripheral localization, limited stage, and bone metastasis did have a significant effect (p = 0.015, p < 0.001, and p = 0.042, respectively) (Table 2; Figs. 1–3).
Table 2.
Statistical analysis of patients one year event free survival and overall survival according to demographic characteristic
| Parameter | EFS | p | OS | p |
|---|---|---|---|---|
| Gender | 0.547 | 0.210 | ||
| male | 59% | 77% | ||
| female | 67% | 83% | ||
| Diagnosis of age | 0.922 | 0.617 | ||
| ≤ 19 | 62% | 85% | ||
| ≥ 20 | 60% | 75% | ||
| Primary tumor site | 0.708 | 0.644 | ||
| osseous | 53% | 75% | ||
| extraosseous | 75% | 83% | ||
| Osseous site | 0.005 | 0.015 | ||
| peripheral | 87% | 87% | ||
| central axis | 34% | 68% | ||
| Stage | < 0.001 | < 0.001 | ||
| limited | 86% | 90% | ||
| metastatic | 16% | 56% | ||
| Site of metastasis | 0.07 | 0.042 | ||
| osseous | 0% | 80% | ||
| extraosseous | 40% | 39% | ||
| Local treatments with chemothearpy | 0.534 | 0.417 | ||
| surgery/chemotherapy | 69% | 92% | ||
| radiotherapy/chemotherapy | 50% | 75% | ||
| radiotherapy/surgery/chemotherapy | 71% | 86% |
EFS – event free survival; OS – overall survival
Fig. 1.
Patient survival curves according to the osseous site
Fig. 3.
Patient survival curves according to the metastasis site of the tumor
Fig. 2.
Patient survival curves according to the stage of the tumor
Univariate analysis revealed that central axis osseous localization had a greater effect on EFS than did a peripheral osseous localization (p < 0.025). The most important prognostic factors for OS were central axis localization and surgical treatment in primary osseous tumors (p = 0.041 and p = 0.058, respectively; Tables 3 and 4).
Table 3.
Analysis of combined effects of all risk factors believed to predict event free survival
| Parameter | RR | 95% CI (lower limit–upper limit) |
p |
|---|---|---|---|
| Gender (male) | 1.457 | 0.41–5.06 | 0.554 |
| Age (≤ 19) | 1.052 | 0.37–2.92 | 0.923 |
| Localization (osseous) | 1.204 | 0.45–3.21 | 0.711 |
| Osseous site (peripheral) | 0.093 | 0.01–0.74 | 0.025 |
| Surgery (positive) | 0.489 | 0.19–1.21 | 0.123 |
| Radiotherapy (positive) | 1.200 | 0.49–2.91 | 0.677 |
RR – relative risk; CI – confidence interval
Table 4.
Analysis of combined effects of all risk factors believed to predict overall
| Parameter | RR | 95% CI (lower limit–upper limit) | p |
|---|---|---|---|
| Gender (male) | 3.363 | 0.44–5.64 | 0.242 |
| Age (≤ 19) | 1.059 | 0.36–3.05 | 0.916 |
| Localization (osseous) | 1.285 | 0.43–3.79 | 0.649 |
| Osseous site (peripheral) | 0.111 | 0.01–0.91 | 0.041 |
| Surgery (positive) | 0.366 | 0.13–1.03 | 0.058 |
| Radiotherapy (positive) | 1.149 | 0.42–8.64 | 0.783 |
RR – relative risk; CI – confidence interval
Discussion
The ESFT generally involves the bones, particularly the long bones of the lower limbs, followed by the pelvis and thoracic bones. The lower extremities are the most common primary sites for ES, accounting for 40–45% of newly diagnosed patients, with ∼50% of these occurring in the femur [9]. In a study performed in 98 ESFT patients aged ≤ 18 years, 52 presented with a primary lesion confined to the limbs [14]. In another study in adults, the primary tumors were localized to the trunk in 53.8% of cases or to peripheral sites in 41.7% of cases [15]. Consistent with this, in the current study, the number of patients with centrally localized tumors was higher than those with peripheral tumors.
ESFT has a strong potential to metastasize. Metastases occur most commonly in the lungs and bone [16]. More than 10% of patients present with multiple bone metastases at initial diagnosis. Although metastases to the lungs, bone, bone marrow, or a combination thereof are detectable in ∼25% of patients, metastases to the lymph nodes are rare [11]. A study by Grier et al. in EFST patients reported that 23.1% of patients had metastasis, and that the most common metastatic sites were the lungs, bones, and bone marrow [12]. Kutluk et al. reported that the rate of metastasis was 34% at the time of diagnosis [17]. An additional study in adult extraskeletal ES patients showed that 31% of the patients were metastatic at the time of diagnosis [18]. Another study in adult and adolescent extraskeletal ES patients demonstrated that 43% of patients admitted to the hospital were in the metastatic stage [8]. Smorenburg et al. demonstrated the most common sites of metastasis to be the lungs and bone [19]. In the current study, a higher percentage of patients had metastasis at the time of diagnosis. The most common metastatic sites were the lungs and bones, consistent with previous studies.
Modern day ESFT treatment consists of 3–6 cycles of initial combination chemotherapy after diagnosis by biopsy, followed by surgery and/or local therapy and then 6–10 cycles of chemotherapy [20, 21]. The 5-year survival rate among patients with ESFT, particularly those with localized disease, has increased from 10 to 60% with the use of combination chemotherapies. The most commonly used chemotherapeutic drugs are adriamycin, vincristine, ifosfamide, etoposide, dactinomycin, and cyclophosphamide [6, 7, 9, 12, 13, 22–24].
As part of the local control method, preoperative radiotherapy can be combined with surgery to avoid intralesional resection and to obtain negative surgical margins. If surgery is impossible, then radiotherapy can be performed alone. Postoperative radiotherapy should be administered in patients with inadequate surgical margins and considered if there is a poor histological response of the surgical specimen to chemotherapy [8, 25, 26]. When surgery is considered, effort should be made to perform limb-sparing surgery [9]. In another study, the authors found that better local control was achieved in patients who underwent surgery [27]. In addition, Hauesler et al. reported that local treatment was a poor prognostic factor for survival [28].
Systemic chemotherapy is effective for microscopic and macroscopic metastases due to its tumor volume-depleting effects. In an INT-0091 study performed by the Pediatric Oncology Group Children's Cancer Group, non-metastatic ESTF patients received cyclophosphamide-adriamycin-vincristine-dactinomycin (CAVD) chemotherapy, or alternating CAVD and IE chemotherapies. In the metastatic group, the 5-year disease-free survival (DFS) and OS were not altered by the chemotherapy. However, in the non-metastatic group, intensive chemotherapy extended the rates of both DFS and OS [29]. The ESMO guidelines state that chemotherapy should be used in patients with metastatic disease, such as those with localized disease. In patients with lung metastasis, the combination of total lung irradiation with thoracotomy is essential for achieving complete remission and controlling localized residual microscopic disease. For patients with bone metastasis, palliative radiotherapy should be performed in addition to chemotherapy [6].
Extraskeletal ES is an aggressive type of tumor with a high incidence of local recurrence and distant metastasis. El Weshi et al. demonstrated that the outcome of adult extraskeletal ES is similar to that of skeletal ES in terms of the response to multi-modality treatment and the prognostic factors that influence treatment outcomes. Adequate surgical resection, aggressive chemotherapy, and adjuvant local radiation therapy, when indicated, comprise the optimal treatment for best results with this rare disease [30]. In the Euro-EWING 99 R3 study, treatment consisted of six cycles of vincristine, ifosfamide, doxorubicin, and etoposide (VIDE), one cycle of vincristine, dactinomycin, and ifosfamide (VAI), local treatment (surgery and/or radiotherapy), and high-dose busulfan-melphalan followed by autologous stem-cell transplantation. Age, tumor volume, and the extent of metastatic spread are relevant risk factors [31]. In advanced stage ES, the combination of temozolomide and irinotecan was a well-tolerated and reliable palliative treatment regimen [32, 33]. Racibborka et al. demonstrated that the combination of temozolomide, irinotecan, and vincristine was effective and well tolerated in patients with relapsed or refractory ES [34]. In the current study, we used a chemotherapy protocol in which local control methods were administered to most patients, despite their metastatic status at the time of diagnosis. Metastatic disease status at the time of diagnosis, tumors arising from extra-osseous rather than osseous tissue, and age ≥ 26 years at the time of diagnosis were reported to be poor prognostic factors for survival [13, 35]. The current study also revealed unfavorable effects on survival caused by centrally localized tumors in osseous primary sites, metastasis at the time of diagnosis, and non-bone metastasis.
We were unable to demonstrate that surgery and/or radiotherapy performed for local control yielded a significant improvement in survival. The results suggested that palliative but less toxic treatments might be preferable over more aggressive treatments, particularly in patients with metastatic disease.
The authors declare no conflict of interest.
References
- 1.Delattre O, Zucman J, Melot T, et al. The Ewing family of tumors – a subgroup of small-round-cell tumors defined by specific chimeric transcripts. N Engl J Med. 1994;331:294–9. doi: 10.1056/NEJM199408043310503. [DOI] [PubMed] [Google Scholar]
- 2.Murphey MD, Senchak LT, Mambalam PK, Logie CI, Klassen-Fischer MK, Kransdorf MJ. From the radiologic pathology archives: ewing sarcoma family of tumors: radiologic-pathologic correlation. Radiographics. 2013;33:803–31. doi: 10.1148/rg.333135005. [DOI] [PubMed] [Google Scholar]
- 3.Subbiah V, Anderson P, Lazar AJ, et al. Ewing's sarcoma: standard and experimental treatment options. Curr Treat Options Oncol. 2009;10:126–40. doi: 10.1007/s11864-009-0104-6. [DOI] [PubMed] [Google Scholar]
- 4.Ross KA, Smyth NA, Murawski CD, Kennedy JG. The biology of ewing sarcoma. ISRN Oncol. 2013;2013:759725. doi: 10.1155/2013/759725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zagar TM, Triche TJ, Kinsella TJ. Extraosseous Ewing's sarcoma: 25 years later. J Clin Oncol. 2008;26:4230–2. doi: 10.1200/JCO.2008.16.5308. [DOI] [PubMed] [Google Scholar]
- 6.Saeter G. Ewing's sarcoma of bone: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol. 2007;18(Suppl 2):ii79–80. doi: 10.1093/annonc/mdm048. [DOI] [PubMed] [Google Scholar]
- 7.Ferrari S, Sundby Hall K, Luksch R, et al. Nonmetastatic Ewing family tumors: high-dose chemotherapy with stem cell rescue in poor responder patients. Results of the Italian Sarcoma Group/Scandinavian Sarcoma Group III protocol. Ann Oncol. 2011;22:1221–7. doi: 10.1093/annonc/mdq573. [DOI] [PubMed] [Google Scholar]
- 8.Cotterill SJ, Ahrens S, Paulussen M, Jürgens HF, Voûte PA, Gadner H, Craft AW. Prognostic factors in Ewing's tumor of bone: analysis of 975 patients from the European Intergroup Cooperative Ewing's Sarcoma Study Group. J Clin Oncol. 2000;18:3108–14. doi: 10.1200/JCO.2000.18.17.3108. [DOI] [PubMed] [Google Scholar]
- 9.Bernstein M, Kovar H, Paulussen M, Randall RL, Schuck A, Teot LA, Juergens H. Ewing's sarcoma family of tumors: current management. Oncologist. 2006;11:503–19. doi: 10.1634/theoncologist.11-5-503. [DOI] [PubMed] [Google Scholar]
- 10.Maki RG. Pediatric sarcomas occurring in adults. J Surg Oncol. 2008;97:360–8. doi: 10.1002/jso.20969. [DOI] [PubMed] [Google Scholar]
- 11.Iwamoto Y. Diagnosis and treatment of Ewing's sarcoma. Jpn J Clin Oncol. 2007;37:79–89. doi: 10.1093/jjco/hyl142. [DOI] [PubMed] [Google Scholar]
- 12.Grier HE, Krailo MD, Tarbell NJ, et al. Addition of ifosfamide and etoposide to standard chemotherapy for Ewing's sarcoma and primitive neuroectodermal tumor of bone. N Engl J Med. 2003;348:694–701. doi: 10.1056/NEJMoa020890. [DOI] [PubMed] [Google Scholar]
- 13.Nesbit ME, Jr, Gehan EA, Burgert EO, Jr, et al. Multimodal therapy for the management of primary, nonmetastatic Ewing's sarcoma of bone: a long-term follow-up of the First Intergroup study. J Clin Oncol. 1990;8:1664–74. doi: 10.1200/JCO.1990.8.10.1664. [DOI] [PubMed] [Google Scholar]
- 14.Sari N, Toğral G, Cetindağ MF, Güngör BS, Ilhan IE. Treatment results of the Ewing sarcoma of bone and prognostic factors. Pediatr Blood Cancer. 2010;54:19–24. doi: 10.1002/pbc.22278. [DOI] [PubMed] [Google Scholar]
- 15.Huang KL, Chen CF, Wu PK, Chen PC, Chen WM, Liu CL, Chen TH. Clinical outcomes and prognostic factors of Ewing sarcoma: a clinical analysis of 12 patients in Taiwan. J Chin Med Assoc. 2012;75:16–20. doi: 10.1016/j.jcma.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 16.Ahmed SK, Robinson SI, Okuno SH, Rose PS, Issa Laack NN. Adult Ewing sarcoma: survival and local control outcomes in 36 patients with metastatic disease. Am J Clin Oncol. 2014;37:423–9. doi: 10.1097/COC.0b013e31827de65e. [DOI] [PubMed] [Google Scholar]
- 17.Kutluk MT, Yalçin B, Akyüz C, Varan A, Ruacan S, Büyükpamukçu M. Treatment results and prognostic factors in Ewing sarcoma. Pediatr Hematol Oncol. 2004;21:597–610. doi: 10.1080/08880010490501006. [DOI] [PubMed] [Google Scholar]
- 18.Arpaci E, Yetisyigit T, Seker M, et al. Prognostic factors and clinical outcome of patients with Ewing's sarcoma family of tumors in adults: multicentric study of the Anatolian Society of Medical Oncology. Med Oncol. 2013;30:469. doi: 10.1007/s12032-013-0469-z. [DOI] [PubMed] [Google Scholar]
- 19.Smorenburg CH, van Groeningen CJ, Meijer OW, Visser M, Boven E. Ewing's sarcoma and primitive neuroectodermal tumour in adults: single-centre experience in The Netherlands. Neth J Med. 2007;65:132–6. [PubMed] [Google Scholar]
- 20.Womer RB, West DC, Krailo MD, et al. Randomized controlled trial of interval-compressed chemotherapy for the treatment of localized Ewing sarcoma: a report from the Children's Oncology Group. J Clin Oncol. 2012;30:4148–54. doi: 10.1200/JCO.2011.41.5703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ferrari S, Palmerini E, Alberghini M, et al. Vincristine, doxorubicin, cyclophosfamide, actinomycin D, ifosfamide, and etoposide in adult and pediatric patients with nonmetastatic Ewing sarcoma. Final results of a monoinstitutional study. Tumori. 2010;96:213–8. doi: 10.1177/030089161009600205. [DOI] [PubMed] [Google Scholar]
- 22.Schuck A, Ahrens S, von Schorlemer I, et al. Radiotherapy in Ewing tumors of the vertebrae: treatment results and local relapse analysis of the CESS 81/86 and EICESS 92 trials. Int J Radiat Oncol Biol Phys. 2005;63:1562–7. doi: 10.1016/j.ijrobp.2005.05.036. [DOI] [PubMed] [Google Scholar]
- 23.Le Deley MC, Paulussen M, Lewis I, et al. Cyclophosphamide compared with ifosfamide in consolidation treatment of standard-risk Ewing sarcoma: results of the randomized noninferiority Euro-EWING99-R1 trial. J Clin Oncol. 2014;32:2440–8. doi: 10.1200/JCO.2013.54.4833. [DOI] [PubMed] [Google Scholar]
- 24.Luksch R, Tienghi A, Hall KS, et al. Primary metastatic Ewing's family tumors: results of the Italian Sarcoma Group and Scandinavian Sarcoma Group ISG/SSG IV Study including myeloablative chemotherapy and total-lung irradiation. Ann Oncol. 2012;23:2970–6. doi: 10.1093/annonc/mds117. [DOI] [PubMed] [Google Scholar]
- 25.Vogin G, Helfre S, Glorion C, Mosseri V, Mascard E, Oberlin O, Gaspar N. Local control and sequelae in localised Ewing tumours of the spine: a French retrospective study. Eur J Cancer. 2013;49:1314–23. doi: 10.1016/j.ejca.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 26.Pérez-Muñoz I, Grimer RJ, Spooner D, Carter S, Tillman R, Abudu A, Jeys L. Use of tissue expander in pelvic Ewing's sarcoma treated with radiotherapy. Eur J Surg Oncol. 2014;40:197–201. doi: 10.1016/j.ejso.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 27.Puri A, Gulia A, Jambhekar NA, Laskar S. Results of surgical resection in pelvic Ewing's sarcoma. J Surg Oncol. 2012;106:417–22. doi: 10.1002/jso.23107. [DOI] [PubMed] [Google Scholar]
- 28.Haeusler J, Ranft A, Boelling T, et al. The value of local treatment in patients with primary, disseminated, multifocal Ewing sarcoma (PDMES) Cancer. 2010;116:443–50. doi: 10.1002/cncr.24740. [DOI] [PubMed] [Google Scholar]
- 29.Yock TI, Krailo M, Fryer CJ, et al. Local control in pelvic Ewing sarcoma: analysis from INT-0091 – a report from the Children's Oncology Group. J Clin Oncol. 2006;24:3838–43. doi: 10.1200/JCO.2006.05.9188. [DOI] [PubMed] [Google Scholar]
- 30.El Weshi A, Allam A, Ajarim D, Al Dayel F, Pant R, Bazarbashi S, Memon M. Extraskeletal Ewing's sarcoma family of tumours in adults: analysis of 57 patients from a single institution. Clin Oncol (R Coll Radiol) 2010;22:374–81. doi: 10.1016/j.clon.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 31.Ladenstein R, Pötschger U, Le Deley MC, et al. Primary disseminated multifocal Ewing sarcoma: results of the Euro-EWING 99 trial. J Clin Oncol. 2010;28:3284–91. doi: 10.1200/JCO.2009.22.9864. [DOI] [PubMed] [Google Scholar]
- 32.Wagner LM, McAllister N, Goldsby RE, Rausen AR, McNall-Knapp RY, McCarville MB, Albritton K. Temozolomide and intravenous irinotecan for treatment of advanced Ewing sarcoma. Pediatr Blood Cancer. 2007;48:132–9. doi: 10.1002/pbc.20697. [DOI] [PubMed] [Google Scholar]
- 33.Casey DA, Wexler LH, Merchant MS, Chou AJ, Merola PR, Price AP, Meyers PA. Irinotecan and temozolomide for Ewing sarcoma: the Memorial Sloan-Kettering experience. Pediatr Blood Cancer. 2009;53:1029–34. doi: 10.1002/pbc.22206. [DOI] [PubMed] [Google Scholar]
- 34.Raciborska A, Bilska K, Drabko K, et al. Vincristine, irinotecan, and temozolomide in patients with relapsed and refractory Ewing sarcoma. Pediatr Blood Cancer. 2013;60:1621–5. doi: 10.1002/pbc.24621. [DOI] [PubMed] [Google Scholar]
- 35.Baldini EH, Demetri GD, Fletcher CD, Foran J, Marcus KC, Singer S. Adults with Ewing's sarcoma/primitive neuroectodermal tumor: adverse effect of older age and primary extraosseous disease on outcome. Ann Surg. 1999;230:79–86. doi: 10.1097/00000658-199907000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]