1. Introduction
Blount disease is a developmental condition characterized by disordered endochondral ossification of the medial part of the proximal tibial physis resulting in multiplanar deformities of the lower limb.1 Since Blount's first description of this disease in 1937, understanding of the deformities in the disease has advanced.
Blount disease was once termed tibia vara, implying the deformity occurred solely in the frontal plane.1 It is now believed that many other deformities accompanied tibial varus in this disease.2, 3 Proximal tibial procurvatum and internal torsion are among the other common deformities found in Blount disease.2 Compensatory valgus deformity of the femur, once considered common in Blount disease, has been proven vice versa.3 Adding to the contradiction, distal femoral varus takes portion in causing genu varum in late onset-disease.3
In line with the understanding of the deformities, managements of those deformities have also advanced. If the deformities are overlooked in the management of the disease, they will lead to residual and iatrogenic translational deformities, increase the incidence of “recurrence”, and complicate the revision surgery.2
In the present study we systematically reviewed the evolving osteotomies in the correction of deformities in Blount disease. The aim of our study is to reviewed current methods of osteotomy for Blount disease.
2. Methods
We sought for relevant articles across databases of MEDLINE and CINAHL. We also searched Cochrane library for any relevant reviews or trial registers. The search strategy involves the following: 1) tibia vara.mp, 2) blount*.mp, 3) 1 OR 2, 4) explode Osteotomy, and 5) 3 AND 4. Handsearching was conducted from the reference lists of retrieved articles and from major search engines across the web. Studies or reviews about osteotomy in Blount disease were considered. The exclusion criteria were study not reported in English, reported prior to 2009, or conducted not in human. All articles relevant to the study criteria were reviewed. We did not perform validity assessment or quantitative data synthesis for the included studies.
3. Results
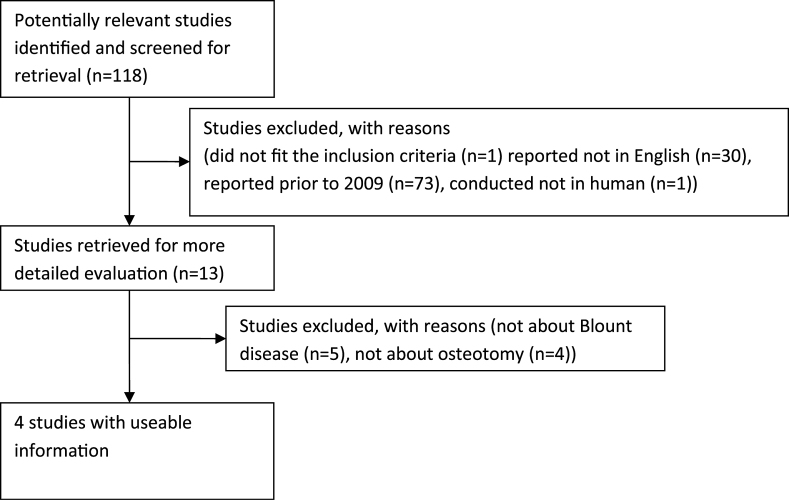
Searching across the databases initially resulted 115 articles. No relevant review or trial was found from the Cochrane library. Handsearching revealed three articles, totaling 118 articles. One study did not fit the inclusion criteria while 105 articles were excluded. The flow of included studies is shown in Fig. 1. Thirteen articles were retrieved for further evaluation.4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 Of these articles, only four articles fitted the study criteria.4, 5, 6, 7 They were summarized in Table 1.
Fig. 1.
Flow of the included study.
Table 1.
Study characteristics.
| Author | Year | Publication type | Sample size | Type of correction | Methods of osteotomy | Fixation device |
|---|---|---|---|---|---|---|
| Siregar6 | 2010 | Case report | 1 tibia in 1 patient | Acute | Bamboo osteotomy | Internal fixator |
| McCarthy5 | 2009 | Retrospective case series | 22 tibiae in 16 patients | Acute and gradual | Double osteotomy | Multiplanar external fixator |
| Ogbemudia7 | 2011 | Prospective case series | 47 tibiae in 31 patients | Acute | Anterior posterior interved-‘U’ osteotomy | Not required |
| Amer4 | 2010 | Retrospective case series | 22 tibiae in 20 patients | Acute and Gradual | angulation translatation high tibial osteotomy | Multiplanar external fixator |
Bamboo osteotomy was first reported by Siregar from Indonesia in 2010.6 It is claimed to be more stable and the healing is more rapid. Another advantage of this method is the evitable need for prophylaxis fasciotomy. Bamboo osteotomy involves creating multiple longitudinal incomplete fractures that allow plastic deformation at the site of correction. Skin is incised above 0.5 cm lateral to the tibial crest and 1.5 cm below tibial tuberosity. The incision is then deepened to the periosteum. The periosteum is stripped circumferentially by blunt dissection. Several longitudinal osteotomies are made using oscillating saw with the cuts 4 mm apart. The site of osteotomies is at the proximal tibia that enables the placement of 2 screw fixations with a locking compression plate. The osteotomies are then encased by suturing the periosteum. A short segment of fibula is then resected using different approach. Forceful manipulation is applied to correct the tiba vara, procurvatum, and internal rotation to obtain normal femoral tibial angle. The correction is maintained using locking compression plate with 2 screws on each fragment or with fixed-angled plate. The patient can be discharged within 2 days and allowed for non-weight bearing ambulation.
Anterior posterior inverted-‘U’ osteotomy was introduced by Ogbemudia from Niger in 2002.7 The basic of this osteotomy is the dome osteotomy, but instead of performing the dome in the coronal plane, sagittal plane is used.7, 17 Incision is made over the junction between the distal and middle third to remove 1 cm fibula. Another longitunal incision about 10 cm in length is made about a thumb's breadth lateral to anterior border of tibia and developed to the periosteum. The periosteum is incised longitudinally midway between the anterior and interosseus borders and stripped away. With a 2.7 mm drill, a uni-cortical arc of perforation was made over the lateral to the anterior border with the drill points 0.5 mm apart. These perforations are connected using 0.5 mm osteotome. Gauze soaked in adrenaline (1:200 000) is used to pack the wound. Another longitudinal incision is made over the medial border of tibia a little finger's breadth posterior to medial border of tibia and developed to the periosteum. A lane's bone lever is inserted to protect the neurovascular structure behind the level of osteotomy. A uni-cortical arc similar to lateral surface was made over the medial surface. The lowest parts of the two arcs are connected across the anterior and posterior surface with anterior limb osteotomy a quarter longer than the posterior limb. The apex of the osteotomy is at the level of the fibular neck. To correct internal torsion, a crescent-shaped wedge was removed from the superoposterior aspect of the lateral surface of the proximal fragment. One mm of wedge is needed to correct 10° of internal torsion. The deformities are then corrected by applying gentle traction and application of external rotation and valgus force. To prevent compartment syndrome, prophylactic fasciotomy is done. Postoperative, an above-knee cast with wide anterior window extending form the patella to the distal third of the leg is used for immobilization at the point of normal dorsalis pedis arterial pulsation. The lower extremity is elevated during the first five days, and on the 14th day, the cast is removed. The limb is manipulated to obtain the desired over-correction. An above knee scotch cast-brace is utilized afterward on the 18th day, the patient is allowed for partial weight bearing ambulation with axillary crutch.
From an initial study involving 31 subjects and 47 knees (4 Langenskiold's stage III, 43 stage IV–VI) with a follow up of 24 months, this osteotomy resulted in 17 fair and 30 good outcome according to Schoenecker's grading.7 All osteotomies went on to unite within 16 weeks. At 24 months after operation, the thigh foot angle, angle of Drennan, degree of varus, tibiofemoral angles, and degree of procurvatum improved from −25° to 4°, 25° to 11°, 39° to 5°, 35° to 5°, and 18° to 2° respectively.
Amer reported the use of single high tibial osteotomy in combination with Ilizarov apparatus.4 Only the internal rotation is corrected during surgery. Correction of varus deformity is conducted using gradual angulation and translation with the Ilizarov apparatus using “juxta-articular hinge assembly” until 10° of valgus. The correction is started one week postoperatively and usually takes 3–5 weeks. After desired correction is achieved, the apparatus is maintained for 10–12 weeks to allow consolidation. The advantage of this method is that it allows correction of associated deformities. However, high recurrence rate (45.5%) was reported after follow up of 2.9 years.
McCarthy retrospectively reviewed osteotomy combined with plateau elevation for severe Blount's disease in 16 patients (22 limbs) and found that this method significantly improved the tibiofemoral angle, anatomic medial proximal tibial angle, and the plateau angle.5 However, failures were observed in the 5 patients after 4.14 years of follow up although they were believed to be the result of under-correction and subsequent recurrence of the tibial osteotomy. This method involves 1 cm resection of fibula at the midshaft to slightly proximal, anterior and lateral compartment fasciotomy, epiphysiodeses of the proximal lateral tibia and proximal fibula, tibial plateu elevation, tibial osteotomy at the level of metaphyseal-diaphyseal junction, and placement of Ilizarov apparatus with the hinges at the right angle to the plane of maximum deformity and the primary hinge over the center of rotation angulation of the proximal tibia. Lengthening procedure is started after one week and angular correction after 1–2 weeks of lengthening procedure until satisfactory correction is achieved. The fixator device is maintained until the radiological consolidation of at least 3 of 4 cortices of the osteotomy. Thereafter, the patient is placed in long leg cast for 6 weeks of nonweight-bearing.
4. Discussion
Only little relevant articles about osteotomy for Blount disease are available. Most of them are limited to case report,6 or retrospective studies.4, 5 None of these studies is prospective randomized controlled trial. However, this is understandable given the incidence of Blount disease is rare so it will take years to obtained adequate sample size.12 This is also the reason that these studies are limited to small sample size.
Another particular important aspect that should be taken in interpreting the results of these studies is the duration of follow up. Chotigavanichaya found that the recurrence of deformity occurs over time.18 In the present review, study of McCarthy has the longest duration of follow up, followed by that of Amer.4, 5
Ideal osteotomy of tibia should completely correct or over-correct the deformity near the site of deformity in cancellous bone, allow early motion of the knee and weight bearing, provide convenience for exploration of the knee during osteotomy, and present no undue technical difficulties or potential hazards.19
All of the methods reviewed in our study were able to completely correct the deformity in the cancellous bone. With the use of Ilizarov apparatus, limb lengthening can be obtained in the method of McCarthy and Amer.4, 5 Although lengthening procedure is not available for Bamboo and inverted-U osteotomy, they do not further shorten the bone similar to that observed in osteotomy involving removal of laterally based wedge of bone.6, 20
Mobilization is early after bamboo osteotomy and late for double correction of McCarthy, while not reported in the study of Amer.4, 5, 6 Ogbemudia incorporated a hinge after 14 days.7 Early mobilization is required to prevent knee stiffness.
No potential hazards of compartment syndrome were observed in these methods although some require prophylaxis fasciotomy. Bamboo osteotomy can be performed in minimal invasive manner thus minimal surrounding soft tissue is manipulate.6 Peroneal nerve palsy as one of the complication in tibia osteotomy was not encountered.21
Recurrence rate to as high as 94% was observed following osteotomy in Blount disease.18 In our review, highest recurrence rate was reported in the study of Amer.4 We were however unable to determine whether the high recurrence was due to the limitation of their techniques since different duration of follow up was encountered among studies. Chotigavanichaya reported the recurrence rate as a function of time although the use of external fixator was one of the determinant for higher recurrence rate.18 Another predicting factor for higher recurrency was the age of the initiation of the osteotomy. The recurrence rate increased if the treatment is initiated after 4 years old.
5. Conclusions
Since many limitations were present in each study, we were unable to determine the best osteotomy for Blount disease. Each method shows its own advantages and disadvantages. Further well prepared study comparing methods of treatment is required. Meanwhile, we suggest the choice of osteotomy to be tailored to the need of the patient and the skill of the operator.
Conflicts of interest
All authors have none to declare.
References
- 1.Sabharwal S. Blount disease. J Bone Jt Surg Am. 2009;91:1758–1776. doi: 10.2106/JBJS.H.01348. [DOI] [PubMed] [Google Scholar]
- 2.Sabharwal S., Lee J., Zhao C. Multiplanar deformity analysis of untreated Blount disease. J Pediatr Orthop. 2007;27:260–265. doi: 10.1097/BPO.0b013e31803433c3. [DOI] [PubMed] [Google Scholar]
- 3.Gordon J.E., King D.J., Luhmann S.J., Dobbs M.B., Schoenecker P.L. Femoral deformity in tibia vara. J Bone Jt Surg Am. 2006;88:380–386. doi: 10.2106/JBJS.C.01518. [DOI] [PubMed] [Google Scholar]
- 4.Amer A.R., Khanfour A.A. Evaluation of treatment of late-onset tibia vara using gradual angulation translation high tibial osteotomy. Acta Orthop Belg. 2010;76:360–366. [PubMed] [Google Scholar]
- 5.McCarthy J.J., MacIntyre N.R., 3rd, Hooks B., Davidson R.S. Double osteotomy for the treatment of severe Blount disease. J Pediatr Orthop. 2009;29:115–119. doi: 10.1097/BPO.0b013e3181982512. [DOI] [PubMed] [Google Scholar]
- 6.Siregar P.U. Bamboo osteotomy for Blount's disease. Malaysian Orthop J. 2010;4:56–59. [Google Scholar]
- 7.Ogbemudia A.O., Bafor A., Ogbemudia P.E. Anterior posterior inverted-'U' osteotomy for tibia vara: technique and early results. Arch Orthop Trauma Surg. 2011;131:437–442. doi: 10.1007/s00402-010-1139-7. [DOI] [PubMed] [Google Scholar]
- 8.Aird J.J., Hogg A., Rollinson P. Femoral torsion in patients with Blount's disease: a previously unrecognised component. J Bone Jt Surg Br. 2009;91:1388–1393. doi: 10.1302/0301-620X.91B10.22554. [DOI] [PubMed] [Google Scholar]
- 9.Bito H., Takeuchi R., Kumagai K. A predictive factor for acquiring an ideal lower limb realignment after opening-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2009;17:382–389. doi: 10.1007/s00167-008-0706-8. [DOI] [PubMed] [Google Scholar]
- 10.Bushnell B.D., May R., Campion E.R., Schmale G.A., Henderson R.C. Hemiepiphyseodesis for late-onset tibia vara. J Pediatr Orthop. 2009;29:285–289. doi: 10.1097/BPO.0b013e31819a85c6. [DOI] [PubMed] [Google Scholar]
- 11.Clarke S.E., McCarthy J.J., Davidson R.S. Treatment of Blount disease: a comparison between the multiaxial correction system and other external fixators. J Pediatr Orthop. 2009;29:103–109. doi: 10.1097/BPO.0b013e3181982a62. [DOI] [PubMed] [Google Scholar]
- 12.Gilbody J., Thomas G., Ho K. Acute versus gradual correction of idiopathic tibia vara in children: a systematic review. J Pediatr Orthop. 2009;29:110–114. doi: 10.1097/BPO.0b013e31819849aa. [DOI] [PubMed] [Google Scholar]
- 13.Masrouha K.Z., Sraj S., Lakkis S., Saghieh S. High tibial osteotomy in young adults with constitutional tibia vara. Knee Surg Sports Traumatol Arthrosc. 2011;19:89–93. doi: 10.1007/s00167-010-1148-7. [DOI] [PubMed] [Google Scholar]
- 14.McIntosh A.L., Hanson C.M., Rathjen K.E. Treatment of adolescent tibia vara with hemiepiphysiodesis: risk factors for failure. J Bone Jt Surg Am. 2009;91:2873–2879. doi: 10.2106/JBJS.H.01245. [DOI] [PubMed] [Google Scholar]
- 15.Sabharwal S., Green S., McCarthy J., Hamdy R. What's new in limb lengthening and deformity correction. J Bone Jt Surg Am. 2011;93:213–221. doi: 10.2106/JBJS.J.01420. [DOI] [PubMed] [Google Scholar]
- 16.Saragaglia D., Mercier N., Colle P.-E. Computer-assisted osteotomies for genu varum deformity: which osteotomy for which varus? Int Orthop. 2010;34:185–190. doi: 10.1007/s00264-009-0757-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miller S., Radomisli T., Ulin R. Inverted arcuate osteotomy and external fixation for adolescent tibia vara. J Pediatr Orthop. 2000;20:450–454. [PubMed] [Google Scholar]
- 18.Chotigavanichaya C., Salinas G., Green T., Moseley C.F., Otsuka N.Y. Recurrence of varus deformity after proximal tibial osteotomy in Blount disease: long-term follow-up. J Pediatr Orthop. 2002;22:638–641. [PubMed] [Google Scholar]
- 19.Coventry M.B. Osteotomy of the upper portion of the tibia for degenerative arthritis of the Knee. J Bone Jt Surg Am. 1965;47-A:984–990. [PubMed] [Google Scholar]
- 20.Umrani S.P., Aroojis A.J. Infantile tibia vara: treatmetn fof Langenskiold stage IV. Indian J Orthop. 2008;42:351–354. doi: 10.4103/0019-5413.41861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Payman K., Patenall V., Borden P., Green T., Otsuka N. Complications of tibial osteotomies in children with comorbidities. J Pediatr Orthop. 2002;22:642–644. [PubMed] [Google Scholar]