Abstract
Objective
Non-union after intramedullary nail fixation of femur shaft fractures is although infrequent but a challenging condition to treat. The treatment options available to deal with such a situation include exchange nailing, removal of nail and re-osteosynthesis with plating, or Ilizarov fixation. We believe that rotational instability, in the presence of a nail, is one of the main reasons for most of the non-union. We present our experience of plate augmentation leaving the nail in situ for non-union of femoral shaft fracture.
Methods
In this retrospective study, we had operated 16 cases of the femoral shaft non-union, which were treated by plate augmentation and bone grafting (if needed) with retention of the intramedullary interlocking nail in situ. The cases of infected non-union and any fracture less than one-year duration were excluded from the study.
Results
Bone grafting was done only in 4 cases with atrophic non-union. We could achieve union in all the cases at an average time of 6.25 months. The average time of surgery between the primary surgery of interlocking nail fixation and the plate augmentation was 13 months. Mean surgical time for plate augmentation and bone grafting was 71 min. No major complication or implant failure was encountered. An average residual shortening of the limb was 0.9 cm and average range of motion of the knee was 115°.
Conclusion
Plate augmentation seems an effective, reliable, safe and an easy procedure for the treatment of femoral shaft non-union after an intramedullary nailing.
Keywords: Fracture, Non-union, Femur, Intramedullary nail, Plate
1. Introduction
The fracture of femoral shaft is a commonly seen injury in Orthopaedic practice and is often caused by high-energy trauma like road traffic accidents (RTA) or sometimes after low energy trauma.1 The treatment of choice for these fractures is closed intramedullary nailing as they have shown excellent union results.2 Non-union after intramedullary nail fixation of femur shaft fractures is although infrequent but quite challenging to treat.3 The treatment options available to deal with such situation include exchange nailing, removal of nail and re-osteosynthesis with plating, or Ilizarov fixation.4 An exchange nailing is considered as the most accepted method for the non-union of femur shaft fractures.5 However, the results with this technique are inconsistent.6 Also the removal of nail and re-osteosynthesis with the plate constitute a well-known method but requires extensive soft tissue and vascular compromise, which hampers union.7 The use of Ilizarov fixation is a cumbersome procedure and is not favoured routinely especially in the thigh, by most surgeons.
We believe that rotational instability, in the presence of a nail, is one of the main reasons for most of the non-union. We present our experience of plate augmentation leaving the nail in situ for non-union of femoral shaft fracture. It is an efficient technique, which provides additional rotational stability at the non-union site, and leaving the nail in situ protects the plate from bending forces. The additional advantages of this technique are that it can be done with minimally invasive technique, allows early rehabilitation of the patient and carries lesser morbidity.
2. Materials and methods
In this retrospective study, we had operated 16 cases of the femoral shaft non-union (Table 1), which were treated by plate augmentation and bone grafting (only in oligotrophic non union) with retention of the intramedullary interlocking nail in situ. Fourteen out of 16 patients were referred from other centres, whereas two patients were operated primarily in our centre. In 12 cases, a prior dynamisation was done, and in other 4 cases, no procedure was done after the primary surgery. All of these fractures progressed to non-union. We have not selected the patients for dynamization as it should be done in early stages (usually 10–24 weeks). Once the patient presented to us after almost a year we have directly gone for the plate augmentation process. The patients were assessed clinically and radiologically for the presence of infection, limb length, range of knee motion and status of the union. Only the cases of femoral shaft non-union with an intramedullary nail in situ and minimum duration of 1 year or more from the primary surgery were included in this study. Twelve out of sixteen patients had evidence of hypertrophic non-union (Fig. 1a) while four showed oligotrophic non-union (Fig. 2a). All the patients had blood investigations including complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). The cases of infected non-union and any fracture of less than one-year duration were excluded from the study. All the cases were operated by the senior author (RV), where an augmentation plating was done and retaining the existing intramedullary nail. Bone-grafting was performed in only four patients with atrophic non-union. Postoperatively active and passive range of knee exercises were started on the 2nd postoperative day, after removal of the drain from the surgical site. Early non-weight bearing mobilisation with a walking aid was allowed. The weight bearing was delayed for six weeks. All the patients were followed up clinically and radiologically at regular intervals.
Table 1.
Patient demographics.
| Cases | Age in years | Sex | Average blood loss (ml) | Type of non union | Time between 1st and 2nd surgery (months) | Duration of plate augmentation surgery (min) | Average duration of follow up post plate augmentation surgery (months) | Average union time (months) | Complications |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 30 | F | 150 | Hypertrophic | 14 | 60 | 9 | 6 | Nil |
| 2 | 28 | F | 200 | Hypertrophic | 13 | 75 | 9 | 5 | Nil |
| 3 | 31 | M | 150 | Hypertrophic | 12 | 60 | 9 | 6 | Nil |
| 4 | 26 | F | 120 | Hypertrophic | 12 | 55 | 7 | 4 | Nil |
| 5 | 47 | F | 200 | Oligotrophic | 15 | 80 | 10 | 8 | Nil |
| 6 | 30 | F | 150 | Hypertrophic | 14 | 65 | 10 | 6 | Nil |
| 7 | 32 | F | 180 | Hypertrophic | 13 | 65 | 9 | 6 | Nil |
| 8 | 40 | M | 300 | Hypertrophic | 12 | 95 | 9 | 6 | Nil |
| 9 | 55 | F | 180 | Oligotrophic | 13 | 70 | 12 | 8 | Nil |
| 10 | 32 | M | 120 | Hypertrophic | 12 | 60 | 9 | 6 | Nil |
| 11 | 42 | F | 220 | Hypertrophic | 13 | 90 | 10 | 6 | Nil |
| 12 | 34 | F | 250 | Hypertrophic | 13 | 80 | 9 | 6 | Nil |
| 13 | 28 | M | 150 | Oligotrophic | 14 | 70 | 8 | 4 | Nil |
| 14 | 50 | F | 250 | Oligotrophic | 12 | 65 | 15 | 9 | Infection |
| 15 | 41 | M | 120 | Hypertrophic | 14 | 60 | 10 | 7 | Nil |
| 16 | 30 | F | 150 | Hypertrophic | 12 | 70 | 9 | 6 | Nil |
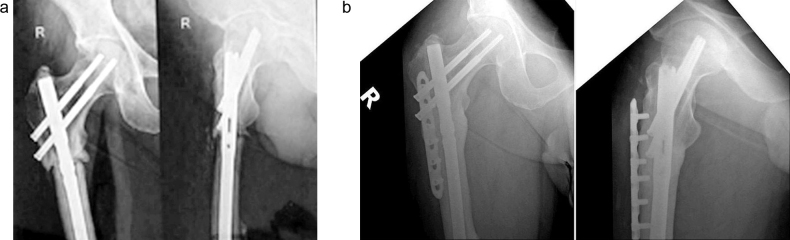
Fig. 1.
(a) Radiographs showing anteroposterior (AP) and lateral view of proximal femur hypertrophic non-union with intramedullary nail in situ. (b) Post-operative radiographs AP and lateral view of proximal femur fracture showing solid union of the fracture with augmentation of the plate.
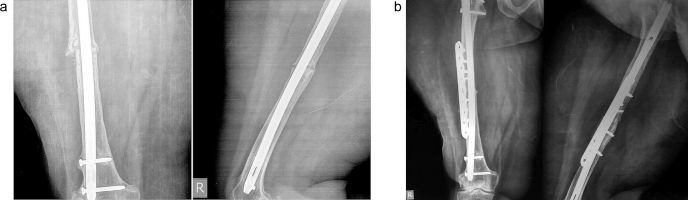
Fig. 2.
(a) Radiographs showing AP and lateral view of femur shaft oligotrophic non-union with intramedullary nail in situ. (b) Post-operative radiographs AP and lateral view of femur shaft showing solid union of the fracture with augmentation of the plate and bone grafting.
3. Surgical technique
Surgery was performed in lateral decubitus, using a direct lateral approach by splitting the tensor fascia lata and vastus lateralis muscles to reach the non-union site.8 Intraoperatively, we noticed rotational instability at the fracture site in all cases. The periosteum was not stripped from the bone to preserve the periosteal blood supply. The fixation of fracture was done with a 6–10 holes, 4.5 mm titanium (locking) low contact dynamic compression plate (LCDCP, Synthes™), using mostly unicortical screws and wherever possible bicortical screws. Cortico-cancellous bone grafts from ipsilateral iliac crest were harvested simultaneously by another surgical team and used around the fracture site in 4 cases of atrophic non-union. The knee was mobilised immediately in post operative period and no splintage was used.
4. Results
There were 11 females and five males in the present study with the average age of 36 years (range 26–55 years). The average time of surgery between the primary surgery of interlocking nail fixation and the plate augmentation was 13 months (range 12–15 months). Mean surgical time for plate augmentation and bone grafting was 71 min (range 55–95 min). The average blood loss during the surgery was around 180 ml (range 120–300 ml). No neurovascular complications were noticed after the surgical procedure; one patient developed surgical site infection which required the additional procedure of debridement. In this patient wound healed completely in three weeks. The average duration of follow-up was 9.62 months (range 7–15 months). We could achieve union in all cases (Fig. 1, Fig. 2) with an average time to radiographic union of 6.25 months (range 4–9 months). An average residual shortening of the limb was 0.9 cm (range 0.5–2.0 cm) and average range of motion of the knee was 115° (range 100–135°). None of the implants showed a failure on follow-up radiographs.
5. Discussion
The use of intramedullary interlocking nail for the femoral shaft fractures has shown excellent results in the literature. However, the critical situation arises, when these fractures fail to unite with intramedullary nails. The known causes of failure include comminuted fracture pattern or significant displacement of fragments and mechanical factors (like small diameter of the nail, insufficient locking) and malalignment of fragments.9 In the present study, we found that rotational instability at the fracture site and comminution of fracture were the leading causes of non-union.
Various methods of surgical treatment have been advocated for the treatment of femoral non-union. They are associated with various advantages and disadvantages (Table 2). Exchange nailing is known to be the most acceptable method of treatment for femoral non-union.10 The thicker nail provides better bending and rotational stability and also the reaming of the canal promotes osteogenesis.11 However the results of the union after exchange nailing vary significantly in the literature, and high failure rate has been reported.12 Also, the exchange nailing in comminuted and distal femur fractures is not advised as the nail does not provide adequate stability in the wide distal fragment.13 Ilizarov's ring fixation after nail removal is also described for non-union of femur shaft fractures with good results.14 However it is a troublesome and time-consuming procedure for the patient and is associated with several complications namely pin tract infection, malrotation, etc. Thus, Ilizarov fixation is not a routinely performed surgery in aseptic femur fracture non-union. Dynamisation is more routinely done as it is a simple procedure. However, the results are unreliable. Also, it may lead to further instability of the fragment.15 Removal of nail and reduction of the fragments followed by fixation by conventional plate requires a long incision, extensive approach with significant soft tissue and vascular compromise; also, it delays the rehabilitation of the patient as the removal of nail causes increased bending force on the plate which may lead to failure of plate, thus the weight bearing has to be protected. Plate augmentation is equally effective for proximal, middle and distal third femoral fractures. We have used locking plate, as it gives good purchase even with unicortical screws.
Table 2.
Comparison of pros and cons between different surgical techniques of fracture shaft femur non-union.
| Technique | Pros | Cons |
|---|---|---|
| Exchange nailing | • Stable fixation • Reaming promotes osteogenesis • Early rehabilitation • Less blood loss |
• Inconsistent results • Do not provide adequate stability in distal femur non unions. • Radiation exposure |
| Plate reosteosynthesis | • Proper reduction of fragments • Allow rigid fixation • Bicortical purchase of all the screws |
• Longer incision • Extensive approach • Significant soft tissue and vascular compromise • Delayed rehabilitation |
| Dynamisation | • Easy day care procedure. • Low cost. |
• Poor, unreliable results • Predispose to shortening |
| Illizarov fixation | • Provides stable fixation • Allow early weight bearing |
• Complications such as pin tract infection and malrotation are commonly seen. • Long learning curve • Cumbersome for the patient |
| Plate augmentation | • Provides additional rotational stability especially in distal femoral non union • Nail in situ prevents bending load on the plate • Minimal incision • Does not require extensive approach • Lesser blood loss • Early rehabilitation |
• Very few screws with bicortical purchase • Does not allow correction of deformity with presence of intact nail |
We agree with Choi and Kim16 that plate augmentation allows additional rotational stability at the fracture site, where the plate holds the fragments in place thus preventing their macro motion. The advantage of leaving the nail in situ is that it helps in neutralising the bending forces on the plate and maintaining alignment of the fracture fragments. Furthermore, plate augmentation can be performed with a minimal incision and it does not require an extensive surgical approach to the bone, as does the conventional plate technique. The blood loss during the surgery is also less. We believe that the post-operative rehabilitation time is significantly reduced in plate augmentation because of the additional support of the nail in situ.
In the present study, we could achieve bony union in all the 16 cases with no significant complication and no implant failure. Very few studies have been done on plate augmentation with a nail in situ, and they have shown results comparable to the present study.17, 18, 19, 20, 21 We believe that plate augmentation in the non-union femoral shaft fractures leaving the nail in situ is a useful and easy technique to adopt with good results and is associated with only minimal complications. Bone grafting is only required, in addition, in fractures with atrophic type of non-union.
Conflicts of interest
The authors have none to declare.
Contributor Information
Raju Vaishya, Email: raju.vaishya@gmail.com.
Amit Kumar Agarwal, Email: amitorthopgi@yahoo.co.in.
Nishint Gupta, Email: nishintgupta@gmail.com.
Vipul Vijay, Email: dr_vipulvijay@yahoo.com.
References
- 1.Neumann M.V., Südkamp N.P., Strohm P.C. Management of femoral shaft fractures. Acta Chir Orthop Traumatol Cech. 2015;82(1):22–32. [PubMed] [Google Scholar]
- 2.Winquist R.A., Hansen S.T., Jr., Clawson D.K. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am. 1984;66(4):529–539. [PubMed] [Google Scholar]
- 3.Lambiris E., Panagopoulos A., Zouboulis P. Current concepts: aseptic nonunion of femoral shaft diaphysis. Eur J Trauma Emerg Surg. 2007;33(2):120–134. doi: 10.1007/s00068-007-6195-5. [DOI] [PubMed] [Google Scholar]
- 4.Crowley D.J., Kanakaris N.K., Giannoudis P.V. Femoral diaphyseal aseptic non-unions: is there an ideal method of treatment? Injury. 2007;38(2):S55–S63. doi: 10.1016/s0020-1383(07)80010-6. [DOI] [PubMed] [Google Scholar]
- 5.Hierholzer C., Glowalla C., Herrler M. Reamed intramedullary exchange nailing: treatment of choice of aseptic femoral shaft nonunion. J Orthop Surg Res. 2014;9:88. doi: 10.1186/s13018-014-0088-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Furlong A.J., Giannoudis P.V., DeBoer P. Exchange nailing for femoral shaft aseptic nonunion. Injury. 1999;30(4):245–249. doi: 10.1016/s0020-1383(99)00073-x. [DOI] [PubMed] [Google Scholar]
- 7.Wu C.C., Shih C.H. Treatment of 84 cases of femoral nonunion. Acta Orthop Scand. 1992;63(1):57–60. doi: 10.3109/17453679209154851. [DOI] [PubMed] [Google Scholar]
- 8.Hoppenfeld S., De Boer P. 4th ed. JB Lippincott Company; 2009. Surgical Exposures in Orthopaedics; pp. 464–467. [Google Scholar]
- 9.Pihlajamaki H.K., Salminen S.T., Bostman O.M. The treatment of nonunions following intramedullary nailing of femoral shaft fractures. J Orthop Trauma. 2002;16(6):394–402. doi: 10.1097/00005131-200207000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Hak D.J., Lee S.S., Goulet J.A. Success of exchange reamed intramedullary nailing for femoral shaft nonunion or delayed union. J Orthop Trauma. 2000;14(3):178–182. doi: 10.1097/00005131-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Somford M.P., Bekerom M.P., Kloen P. Operative treatment for femoral shaft nonunions, a systematic review of the literature. Strateg Limb Reconstr. 2013;8(2):77–88. doi: 10.1007/s11751-013-0168-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weresh M.J., Hakanson R., Stover M.D. Failure of exchange reamed intramedullary nails for ununited femoral shaft fractures. J Orthop Trauma. 2000;14(5):335–338. doi: 10.1097/00005131-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Brinker M.R., O’Connor D.P. Exchange nailing of ununited fractures. J Bone Joint Surg Am. 2007;89(1):177–188. doi: 10.2106/JBJS.F.00742. [DOI] [PubMed] [Google Scholar]
- 14.Menon D.K., Dougall T.W., Pool R.D. Augmentative Ilizarov external fixation after failure of diaphyseal union with intramedullary nailing. J Orthop Trauma. 2002;16(7):491–497. doi: 10.1097/00005131-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Jung H.G., Kim D.J., Kim B.H. Treatment of the femoral shaft nonunion occurred after intramedullary nailing. J Korean Orthop Assoc. 2007;42(5):653–658. [Google Scholar]
- 16.Choi Y.S., Kim K.S. Plate augmentation leaving the nail in situ and bone grafting for non-union of femoral shaft fractures. Int Orthop. 2005;29(5):287–290. doi: 10.1007/s00264-005-0668-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ueng S.W., Chao E.K., Lee S.S. Augmentative plate fixation for the management of femoral nonunion after intramedullary nailing. J Trauma. 1997;43(4):640–644. doi: 10.1097/00005373-199710000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Wang F.D., Gao Y.Z., Yuan W. Augmentative locking compression plate (LCP) combined with bone graft for the treatment of aseptic femoral shaft nonunion after intramedullary nailing. Zhongguo GU Shang. 2014;27(10):815–818. [PubMed] [Google Scholar]
- 19.Said G.Z., Said H.G., el-Sharkawi M.M. Failed intramedullary nailing of femur: open reduction and plate augmentation with the nail in situ. Int Orthop. 2011;35(7):1089–1092. doi: 10.1007/s00264-010-1192-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin C.J., Chiang C.C., Wu P.K. Effectiveness of plate augmentation for femoral shaft nonunion after nailing. J Chin Med Assoc. 2012;75(8):396–401. doi: 10.1016/j.jcma.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 21.Jhunjhunwala H.R., Dhawale A.A. Is augmentation plating an effective treatment for non-union of femoral shaft fractures with nail in situ? Eur J Trauma Emerg Surg. 2016;42(June (3)):339–343. doi: 10.1007/s00068-015-0534-8. [DOI] [PubMed] [Google Scholar]