Highlights
-
•
This was a case of hip osteonecrosis with onset during intravenous corticosteroid therapy for Vogt-Koyanagi-Harada syndrome.
-
•
After seven weeks, the patient was diagnosed at extremely early stage of osteonecrosis of the femoral head.
-
•
She was treated with joint-preserving regenerative therapy using growth factor.
Abbreviations: ONFH, osteonecrosis of the femoral head; MRI, magnetic resonance imaging; THA, total hip arthroplasty; VKH, Vogt-Koyanagi-Harad
Keywords: Osteonecrosis, Femoral head, Vogt-Koyanagi-Harada, Avascular necrosis, Regenerative therapy, Case report
Abstract
Introduction
Osteonecrosis of the femoral head (ONFH) is a corticosteroid-associated disease that mostly cause femoral head collapse and gait disturbance. At the final stage of ONFH, the most reliable treatment is total hip arthroplasty even in young patients. Although magnetic resonance imaging (MRI) is useful for early diagnosis, initial stages are asymptomatic, with pain intensifying after femoral head collapse.
Presentation of case
A 34-year-old female patient with rapid bilateral loss of vision was diagnosed Vogt-Koyanagi-Harada syndrome. She immediately received corticosteroid pulse therapy. While undergoing therapy, she complained of groin pain. The initial MRI of the hip did not show abnormal findings. As the right proximal thigh pain progressed, an MRI of the lumbar spine was performed. No compression of the spinal cord was observed, and right ONFH was suspected on the basis of a characteristic band image. The patient was diagnosed with Stage 1 ONFH 7 weeks after the initial symptoms. She was successfully treated by joint-preserving regenerative therapy using growth factor. After surgery, the patient completely recovered from pain.
Discussion
The occurrence of hip pain while receiving corticosteroid therapy was very rare. The present case was considered a result of reduction of the blood supply to the femoral head induced by hip pain that progressed to ONFH for unknown reasons.
Conclusion
It is difficult to identify cases of corticosteroid-associated ONFH even in patients with potential risk. In this case, we could identify the patient extremely early based on the ONFH image and could provide joint-preserving regenerative therapy.
1. Introduction
Osteonecrosis of the femoral head (ONFH) is an intractable disease that causes progressive femoral head collapse, severe pain, and gait disturbance [1], [2]. Although the etiology of ONFH has yet to be fully elucidated, background factors, such as corticosteroid use and alcohol abuse, have been indicated. The 30 s and 40 s are susceptible ages for disease onset. The most important factor affecting the fate of ONFH patients is the presence or absence of femoral head collapse. The final stage of ONFH comprises severe secondary osteoarthritis of the hip joint, and the optimal treatment is total hip arthroplasty (THA), even in young patients. In daily clinical practice, even if the diagnosis is established, 80% of untreated patients experience femoral head collapse and have to undergo THA [3]. Because the collapse rate of ONFH is high [4], a recent strategy of ONFH treatment has shifted the approach to early diagnosis and early intervention [1], [5]. Many joint-preserving therapies are being studied for the purpose of preventing femoral head collapse [6], [7], [8], [9], [10], [11], [12], [13]. Magnetic resonance imaging (MRI) can be useful for early diagnosis, but the symptoms corresponding to the initial stage are usually absent or present as slight pain, that intensifies after the femoral head collapses. Several months to several years can elapse from the occurrence of asymptomatic ONFH and the onset of symptomatic ONFH [4]. A limitation of this study is that it may only determine the reason for the difference in the occurrence and the onset of ONFH. Here we describe a rare ONFH case associated with groin pain during intravenous corticosteroid pulse therapy, which was diagnosed at an extremely early stage of ONFH, and could be treated with joint-preserving regenerative therapy.
2. Presentation of case
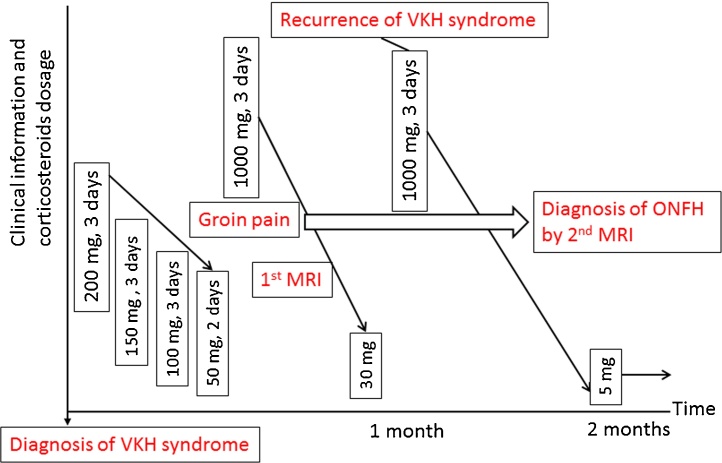
A 34-year-old woman was hospitalized in the emergency department with rapid bilateral loss of vision, at the end of 2012. At the prodromal stage, 10 days earlier, she presented with unexplained bilateral visual symptoms, headache, and deafness. On fundus observation, both bilateral uveitis and a sunset fundus were confirmed. After evaluating these clinical findings and symptoms, she was diagnosed with Vogt-Koyanagi-Harada (VKH) syndrome. She immediately received systemic steroid pulse therapy. The first course comprised 200 mg, 150 mg, and 100 mg of methylprednisolone administered intravenously for 3 days each, followed by a dose of 50 mg for 2 days. However, her symptoms did not improve. Thus, a second course of 1000 mg corticosteroid therapy was administered for 3 days starting on day 12 after initial diagnosis. Weak eyesight improved; administration of corticosteroid was gradually tapered to 30 mg/day. However, at 1 month after initial diagnosis, she developed panuveitis, alopecia, and extensive depigmentation of body hair. Clinical recurrence of VKH syndrome was observed. Next, she received third corticosteroid pulse therapy. After three courses of steroid pulse therapy, vision loss improved. Administration of corticosteroid was gradually tapered to 5 mg/day and switched to low-dose oral drugs (Fig. 1).
Fig. 1.
Progress information of the patient. Because of recurrence of Vogt-Koyanagi-Harada (VKH) syndrome, the patient received 3 courses of systemic steroid pulse therapy in 1 month. ONFH, osteonecrosis of the femoral head; MRI, magnetic resonance imaging.
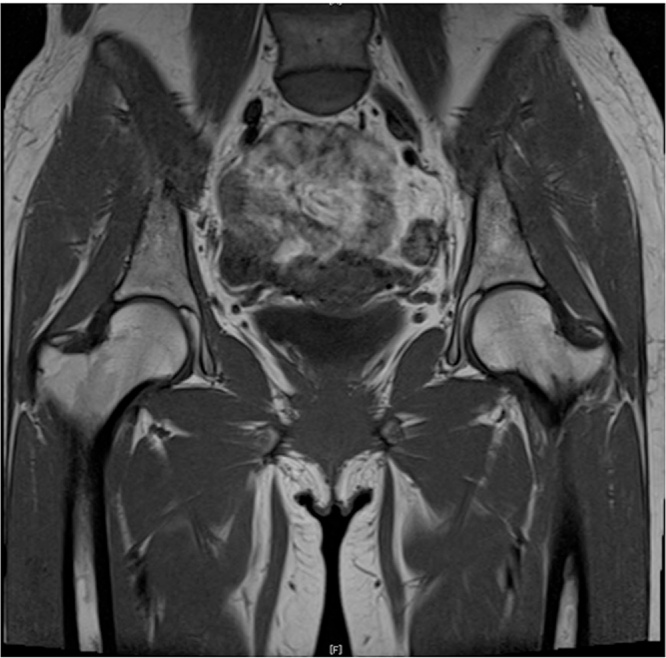
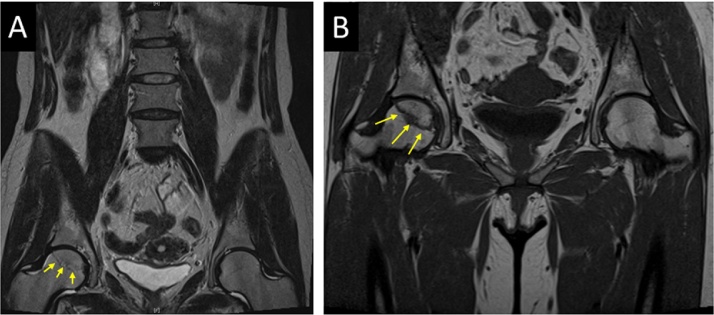
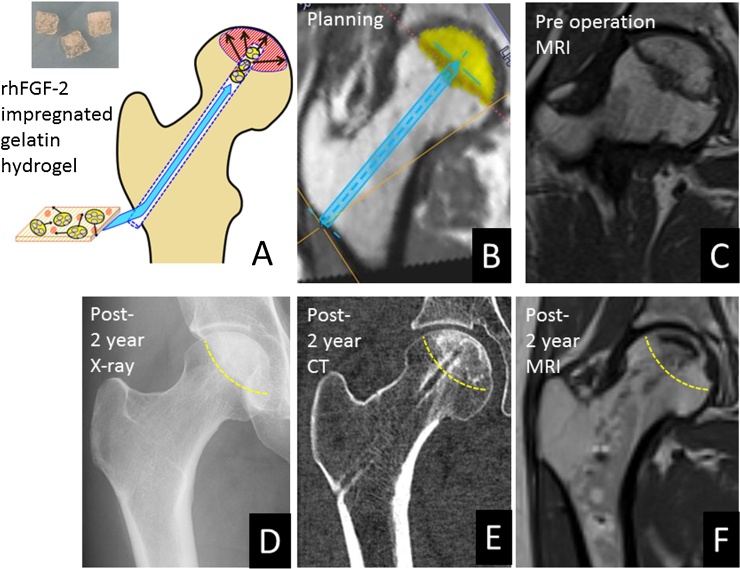
On the third day of the second course of systemic steroid pulse therapy, 2 h after receiving 1000 mg corticosteroids, she complained of acute bilateral groin pain when walking. This noticeable symptom was recorded, and she could still clearly remember the situation. Several days had been passed without any decrease in groin pain, and she was referred to our department. An orthopedic doctor suspected a case of steroid induced ONFH; however, there were no abnormal signs in the MRI scan of the hip joints and physical examination (Fig. 2). We observed the evolution of her condition and avoided the administration of analgesics. Subsequently, uncomfortable bilateral pain around the groin and proximal thigh continued for 1 month. She consulted the orthopedic department again. To exclude the possibility of neurological symptoms from the lumbar spine, radiographs and MRI of the lumbar spine was performed. Although, there was no compression of the spinal cord, the scout view of T2-weighted MRI showed a characteristic band image consistent with ONFH. Thus, she was diagnosed with stage 1 ONFH in the right hip (Fig. 3). After unilateral ONFH diagnosis, she complained of continuous and severe right hip joint pain. Immediately, we started a clinical trial of regenerative therapy using growth factor for patients with precollapse stage of ONFH. This consisted of the clinical application of recombinant human fibroblast growth factor-2-impregnated gelatin hydrogel. The patient agreed and provided written informed consent to participate in this clinical trial and was surgically treated on April 2013. Three months postoperatively, the severe pain disappeared completely with full marks in the Harris hip score. Three clinical scores improved 2 years postoperatively (visual analog scale for pain, 0 mm; University of California, Los Angeles [UCLA] activity score, 7; and Harris hip score, 100.0 points) compared with those preoperatively (visual analog scale for pain, 41.0 mm; UCLA activity score, 4; Harris hip Score, 57.0 points) (Table 1). Two years after the surgery, radiographic regeneration of ONFH was observed without femoral head collapse. Radiographs, computed tomography images, and MRI showed bone regeneration in the area of ONFH (Fig. 4).
Fig. 2.
Magnetic resonance imaging obtained after the onset of bilateral groin pain. There were no significant findings.
Fig. 3.
Right osteonecrosis of the femoral head could be diagnosed by magnetic resonance imaging (MRI). Characteristic band pattern was shown (yellow arrows). The scout view of T2-weighted MRI (A) and T1-weighted MRI (B).
Table 1.
Clinical outcomes.
| Score (range) | Preoperation | 3 months postoperatively | 6 months postoperatively | 12 months postoperatively | 24 months postoperatively |
|---|---|---|---|---|---|
| VAS (0–100) |
41.0 | 0 | 0 | 0 | 0 |
| UCLA (1–10) |
4 | 6 | 6 | 7 | 7 |
| HHS (0–100) |
57.0 | 100.0 | 100.0 | 100.0 | 100.0 |
Abbreviations: VAS, visual analog scale for pain; UCLA, UCLA activity rating; HHS, Harris hip Score.
Fig. 4.
A schema and radiological results of the regenerative therapy. Dashed yellow lines show the border of ONFH area. (A) A schema of the surgical procedure administering the rhFGF-2 gelatin hydrogel by the percutaneous technique. The actual hydrogel (small photograph). (B) A screenshot used for preoperative planning. The area of osteonecrosis of the femoral head (ONFH) is shown in yellow. The route of the drilling is shown by the blue screw. Pre-operative magnetic resonance imaging (MRI) (C) and 2-year postoperative radiographs show bone formation within the ONFH area: radiograph (D), computed tomography (CT) image (E), and T1-weighted MRI (F).
3. Discussion
ONFH and VKH syndrome are rare and intractable diseases in Europe. Conversely, in Asia, VKH syndrome is one of the most common causes of panuveitis [14]. Because of the high rate of clinical recurrence in patients with VKH syndrome, early high-dose corticosteroid therapy is essential for treatment [15]. First, we describe a rare case of VKH syndrome associated with groin pain and treated with systemic corticosteroid therapy, with ONFH onset 7 weeks later. In routine clinical practice, most of the ONFH cases are usually diagnosed after the femoral head collapses. There are several reports indicating that uveitis patients with systemic disorders, who require corticosteroid therapy, have a potential risk of developing ONFH. Peretz et al. reported that patients with uveitis and systemic diseases, including sarcoidosis, spondyloarthropathy, Behcet’s disease, Crohn’s disease, Cushing’s syndrome, osteoporosis, cataracts, and ONFH, required corticosteroids or immunosuppressive drugs and were at risk of presenting side effects [16]. To the best our knowledge, this is the second case of ONFH following VKH syndrome. Smith et al. reported that 6 uveitis patients with ONFH were identified including 1 patient with VKH syndrome, comprising a prevalence of 0.25% for VKH syndrome. They concluded that corticosteroid-associated ONFH is a rare but serious complication in uveitis; a higher level of suspicion for ONFH may be warranted in patients with systemic corticosteroid use [17]. It is difficult to predict the onset of corticosteroid-associated ONFH, even in the patients with potential risk. In this study, we showed that repeated clinical examinations and MRI evaluations were useful in diagnosing ONFH at an extremely early stage.
In this case, why the patient complained of groin pain while receiving corticosteroid therapy was unclear. Because ONFH is considered to be caused by the critical loss of the vascular supply to the femoral head, several causative factors may influence its development, including hypercoagulation, bone marrow fat embolisms, and elevation of intraosseous pressure in the femoral head [1], [2]. Some of these complex factors may induce groin pain immediately after receiving systemic corticosteroid therapy, but further study is needed to clarify the mechanism of pain.
The patient could be successfully treated by regenerative therapy using growth factor. This surgical treatment is based on translational clinical research in an experimental animal study by the authors [18]. We reported the first clinical application of recombinant human fibroblast growth factor-2-impregnated gelatin hydrogel for patients with precollapse stage of ONFH with good clinical results and safety [11]. Femoral head collapse progresses until severe secondary osteoarthritis develops, destroying both the femoral head and the acetabulum. End-stage ONFH patients usually require THA which involves risk of infection, dislocation, revision, and limitation of sports activities throughout the patient’s life. Considering the age of ONFH patients and high collapse rate of ONFH, recent therapy for ONFH is aimed at inducing bone regeneration to prevent femoral head collapse [19]. This novel treatment strategy has shifted the concept of early diagnosis and aggressive intervention. In particular, to prevent femoral head collapse, precollapse stage of ONFH has become a research target for various regenerative therapies, such as cell therapy [6], [7], [8], bone substitutes [9], [10], and growth factors [11], [12], [13]. In any case, early diagnosis of ONFH is crucial to allow prevention of femoral head collapse using recently developed therapies.
4. Conclusion
We experienced a rare ONFH case associated with groin pain during intravenous corticosteroid pulse therapy for VKH syndrome. With careful attention, the patient was diagnosed with ONFH at an extremely early stage, which allowed the application of joint-preserving therapy. ONFH appears to be a rare and serious complication in uveitis patients; thus, physicians should pay close attention to the patient’s complaint for early and accurate diagnosis.
Consent
Written informed consent was obtained from the patient for publishing this article.
Conflict of interest
No conflicts of interest.
Funding
None.
Ethical approval
The treatment protocol was approved by the Ethics Committee of Kyoto University Graduate School and Faculty of Medicine. Before enrolment, written informed consent was obtained from each participant included in the study.
Author contributions
The author contributions are stated below in the mentioned categories:
-
a)
Conceived and designed the experiments: Y.K., S.M.
-
b)
Performed the experiments: Y.K., S.K.
-
c)
Contributed to the writing of the manuscript: K.Y., S.K., K.G., S.M.
Guarantor
Yutaka Kuroda.
References
- 1.Mont M.A., Cherian J.J., Sierra R.J., Jones L.C., Lieberman J.R. Nontraumatic osteonecrosis of the femoral head: where do we stand today? a ten-Year update. J. Bone Joint Surg. Am. 2015;97:1604–1627. doi: 10.2106/JBJS.O.00071. [DOI] [PubMed] [Google Scholar]
- 2.Mont M.A., Jones L.C., Hngerford D.S. Nontraumatic osteonecrosis of the femoral head: ten years later. J bone joint surg Am 88: 1117-32. review erratum in. J. Bone Joint Surg. Am. 2006;88A:1602. doi: 10.2106/JBJS.E.01041. [DOI] [PubMed] [Google Scholar]
- 3.Hernigou P., Ooignard A., Nogier A., Manicom O. Fate of very small asymptomatic stage-I osteonecrotic lesions of the hip. J. Bone Joint Surg. Am. 2004;86:2589–2593. doi: 10.2106/00004623-200412000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Min B.W., Song K.S., Cho C.H., Lee S.M., Lee K.J. Untreated asymptomatic hips in patients with osteonecrosis of the femoral head. Clin. Orthop. Relat. Res. 2008;466:1087–1092. doi: 10.1007/s11999-008-0191-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marker D.R., Seylee T.M., McGrath M.S., Delanois R.E., Ulrich S.D., Mont M.A. Treatment of early stage osteonecrosis of the femoral head. J. Bone Joint Surg. Am. 2008;90:175–187. doi: 10.2106/JBJS.H.00671. [DOI] [PubMed] [Google Scholar]
- 6.Gangji V., De Maertelaer V., Hauzeur J.P. Autologous bone marrow cell implantation in the treatment of non-traumatic osteonecrosis of the femoral head: five year follow-up of a prospective controlled study. Bone. 2011;49:1005–1009. doi: 10.1016/j.bone.2011.07.032. [DOI] [PubMed] [Google Scholar]
- 7.Hernigou P., Beaujean F. Treatment of osteonecrosis with autologous bone marrow grafting. Clin. Orthop. Relat. Res. 2002;405:14–23. doi: 10.1097/00003086-200212000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Houdek M.T., Wyles C.C., Martin J.R., Sierra R.J. Stem cell treatment for avascular necrosis of the femoral head: current perspectives. Stem Cells Cloning. 2014;7:65–70. doi: 10.2147/SCCAA.S36584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsao A.K., Roberson J.R., Christie M.J., Dore D.D., Heck D.A., Robertson D.D. Biomechanical and clinical evaluations of a porous tantalum implant for the treatment of early-stage osteonecrosis. J. Bone Joint Surg. Am. 2005;87(Suppl. 2):22–27. doi: 10.2106/JBJS.E.00490. [DOI] [PubMed] [Google Scholar]
- 10.Malizos K.N., Papasoulis E., Dailiana Z.H., Papatheodorou L.K., Varitimidis S.E. Early results of a novel technique using multiple small tantalum pegs for the treatment of osteonecrosis of the femoral head: a case series involving 26 hips. J. Bone Joint Surg. Br. 2012;94:173–178. doi: 10.1302/0301-620X.94B2.27287. [DOI] [PubMed] [Google Scholar]
- 11.Kuroda Y., Asada R., So K., Yonezawa A., Nankaku M., Mukai K. A pilot study of regenerative therapy using controlled release of rhFGF-2 for patients with precollapse osteonecrosis of the femoral head. Int. Orthop. 2015 doi: 10.1007/s00264-015-3083-1. [DOI] [PubMed] [Google Scholar]
- 12.Sun W., Li Z., Gao F., Shi Z., Zhang Q., Guo W. Recombinant human bone morphogenetic protein-2 in debridement and impacted bone graft for the treatment of femoral head osteonecrosis. PLoS One. 2014;9:e100424. doi: 10.1371/journal.pone.0100424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mont M.A., Jones L.C., Einhorn T.A., Hungerford D.S., Reddi A.H. Osteonecrosis of the femoral head—potential treatment with growth and differentiation factors. Clin. Orthop. Relat. Res. 1998;355:S314–S335. [PubMed] [Google Scholar]
- 14.Sakata V.M., da Silva F.T., Hirata C.E., Marin M.L., Rodrigues H., Kalil J., Costa R.A., Yamamoto J.H. High rate of clinical recurrence in patients with Vogt-Koyanagi-Harada disease treated with early high-dose corticosteroids. Graefes Arch. Clin. Exp. Ophthalmol. 2015;253:785–790. doi: 10.1007/s00417-014-2904-z. [DOI] [PubMed] [Google Scholar]
- 15.Cunningham E.T., Jr., Rathinam S.R., Tugal-Tutkun I., Muccioli C., Zierhut M. Vogt-Koyanagi-Harada disease. Ocul. Immunol. Inflamm. 2014;22:249–252. doi: 10.3109/09273948.2014.939530. [DOI] [PubMed] [Google Scholar]
- 16.Peretz A., Guillaume M.P., Casper-Velu L. Uveitis management: a multidisciplinary approach to assess systemic involvement and side effects of treatments. Acta Clin. Belg. 2002;57:142–147. doi: 10.1179/acb.2002.030. [DOI] [PubMed] [Google Scholar]
- 17.Smith W.M., Larson T.A., Meleth A.D., Krishnadev N., Nussenblatt R.B., Sen H.N. Corticosteroid-associated osteonecrosis: a rare, but serious, complication in uveitis. Ocul. Immunol. Inflamm. 2013;21:102–107. doi: 10.3109/09273948.2012.740129. [DOI] [PubMed] [Google Scholar]
- 18.Kuroda Y., Akiyama H., Kawanabe K., Tabata Y., Nakamura T. Treatment of experimental osteonecrosis of the hip in adult rabbits with a single local injection of recombinant human FGF-2 micro-spheres. J. Bone Miner. Metab. 2010;28:608–616. doi: 10.1007/s00774-010-0172-5. [DOI] [PubMed] [Google Scholar]
- 19.Kuroda Y., Matsuda S., Akiyama H. Joint-preserving regenerative therapy for patients with early-stage osteonecrosis of the femoral head. Inflamm. Regener. 2016;36:4. doi: 10.1186/s41232-016-0002-9. [DOI] [PMC free article] [PubMed] [Google Scholar]