Abstract
Objective. We aimed to identify key enablers of physician prescription of a long-term controller in patients with persistent asthma. Methods. We conducted a mailed survey of randomly selected Quebec physicians. We sent a 102-item questionnaire, seeking reported management regarding one of 4 clinical vignettes of a poorly controlled adult or child and endorsement of enablers to prescribe long-term controllers. Results. With a 56% participation rate, 421 physicians participated. Most (86%) would prescribe a long-term controller (predominantly inhaled corticosteroids, ICS) to the patient in their clinical vignette. Determinants of intention were the recognition of persistent symptoms (OR 2.67), goal of achieving long-term control (OR 5.31), and high comfort level in initiating long-term ICS (OR 2.33). Decision tools, pharmacy reports, reminders, and specific training were strongly endorsed by ≥60% physicians to support optimal management. Physicians strongly endorsed asthma education, lung function testing, specialist opinion, accessible asthma clinic, and paramedical healthcare professionals to guide patients, as enablers to improve patient adherence to and physicians' comfort with long-term ICS. Interpretation. Tools and training to improve physician knowledge, skills, and perception towards long-term ICS and resources that increase patient adherence and physician comfort to facilitate long-term ICS prescription should be considered as targets for implementation.
1. Introduction
Guided self-management is the cornerstone of the management of adults and children with asthma [1–4]. Five evidence-based recommendations for guided self-management were endorsed in national and international asthma guidelines: prescription of long-term controller medication for those with persistent asthma; provision of self-management plans; regular medical review; environmental control of known triggers; and asthma education [1–3, 5]. Suboptimal management results in frequent exacerbations, preventable hospitalizations, unsafe use and abuse of medications, absenteeism, and even death [6–8]. Yet, fewer than 30% of patients with persistent asthma use daily controller medications or have a written self-management plan [9, 10]. Although some of the responsibilities lie with the patient, physicians are also at fault as fewer than half of physicians report basing their treatment recommendations on the national asthma guidelines [9, 11, 12]. Barely two-thirds of physicians self-report recommending daily inhaled corticosteroids (ICS) in patients with persistent asthma [10], and most physicians prescribe only short courses of ICS [13–15] or provide insufficient prescription renewals to allow long-term use of ICS [16, 17].
Several studies have addressed barriers to physician adherence to asthma guidelines including use of asthma controllers [18–22], but few, if any, specifically addressed long-term therapy. Yet, the identification of relevant barriers is insufficient by itself to design an effective intervention. Indeed, many knowledge translation initiatives were unsuccessful or only modestly effective because the tested intervention did not address the relevant barriers or lacked a foundation in behavioural theory supporting the intervention [23, 24]. Thus, one must ensure that solutions are effective and implementable by the target audience. Seeking physicians' enablers and proposed solutions has emerged as an effective approach to identify such interventions [25]. In a recent qualitative study, we identified a large number of enablers proposed by physicians to optimise asthma care [26]. Marked variation across physician specialties in prescription patterns and reported barriers suggest the need to target interventions to specific settings and/or specialties [18, 19, 22, 27]. High endorsement of promising enablers by physicians and identification of operational behavioural targets are thus keys to designing a successful intervention to improve their practice [24, 28, 29].
Our main objective was to quantify physicians' endorsement of promising enablers to facilitate the prescription of long-term ICS. We also wished to ascertain physician-reported behaviour regarding the prescription of long-term asthma controller in a poorly controlled patient with persistent asthma and the determinants of this behaviour.
2. Methods
2.1. Study Design
The current paper reports the survey of randomly selected Quebec physicians treating patients with asthma. The protocol received approval from the Institutional Review Board of the Sainte-Justine University Health Centre. All participants received an information letter and consent was assumed if they returned the completed questionnaire.
2.2. Participants
Physicians were eligible if they were registered in July 2013 with the College des Médecins du Québec as family medicine physicians, pediatricians, or emergency physicians and held an active practice licence. Physicians were excluded if they had obtained their diploma more than 30 years earlier, were not practicing, were not seeing patients with asthma, were in training, or had participated in the questionnaire pretest; the former criteria was meant to exclude physicians most likely to be retired by the time a specific knowledge translation intervention would be ready for testing. Physicians were randomly selected using a stratified sampling procedure based on specialty.
2.3. Materials
2.3.1. Item Generation
In the first phase of the study [26] where we conducted qualitative semistructured interviews of 42 physicians, we identified 867 enablers of optimal guided self-management and specifically of the prescription of long-term ICS.
2.3.2. Item Reduction
We retained enablers most frequently endorsed by interviewed physicians; among those, a 2-step Delphi approach was conducted among 7 coauthors with expertise in pediatric and adult respirology, family medicine, pediatrics, pharmacoepidemiology, and behaviour change to identify enablers most likely to be implementable.
2.3.3. Presentation and Scaling
The self-report questionnaire had five main sections. The first section served to describe the characteristics and practice setting of physicians. In the second section, participants were asked to select one of 4 clinical vignettes that most closely reflected their practice, namely, a school-aged child or an adult with poorly controlled asthma who presented either for an acute exacerbation or in the clinic setting when stable (Table E1 in Supplementary Material available online at http://dx.doi.org/10.1155/2016/4169010). Based on the selected vignette, participants were asked to report their treatment recommendations and follow-up strategy (i.e., behaviour), assessment of asthma control and phenotype (i.e., knowledge and skills), and treatment objectives (i.e., goals). The third section pertains to physicians' comfort level in performing key tasks associated with optimal asthma management (i.e., confidence about capabilities), perceived risk-benefit associated with prescription of long-term ICS for certain groups of patients (i.e., knowledge of risk-benefit), and endorsement of resources to assist in patient-specific decision-making and/or patient's adherence to ICS. The fourth and fifth sections, pertaining to written action plans and pharmacists' professional activities, are the object of other reports. Responses were recorded on a 6-point Likert scale ranging from 0 to 5.
2.3.4. Pretesting for Clarity
Pretested in six physicians, the questionnaire took between 20 and 30 minutes to be complete. It was endorsed by and included the logos of the Institut National d'Excellence en Santé et Services Sociaux (INESSS), Association des Pédiatres du Québec, Association des Spécialistes en Médecine d'Urgence du Québec, and Fédération des Médecins Omnipraticiens du Québec.
2.3.5. Survey Procedures
Using the Tailored Design Methods [30], a prenotification postcard was sent, followed 10 days later by the information letter, questionnaire, and a $25 cheque, a thank you/reminder postcard on day 21, and, for nonresponders, a second questionnaire on day 37, followed by up to three phone calls. Where feasible, another physician was selected to replace those identified as ineligible (by phone or questionnaire). The deadline for returning completed questionnaires was April 2014.
2.4. Statistical Analysis
A sample size of 500 physicians was required to obtain a precision of ±5% for endorsement proportions of 50%. Assuming a 60% response rate, the questionnaire was sent to 838 physicians.
The distribution of endorsement was presented as median (25%, 75%), after adjustment for the stratified sampling of physicians by specialty (91.0% for family physicians, 7.6% pediatricians, and 1.4% emergency physicians); we illustrated key results with diverging stacked bar charts [31]. We classified physicians as “intenders” or “nonintenders” based on their reported behaviour on the selected clinical vignette to prescribe long-term asthma controller for at least 3 months or until the patient sees his/her treating physician. Physicians were deemed to be in “strong agreement” if they responded 4 or 5 on the Likert-like scale of 0 to 5. We explored the determinants of physicians' intention to prescribe long-term ICS, using bivariate logistic regression analyses to identify those significantly associated with the outcome; these were offered as candidate variables in the multivariate logistic regression analysis, forcing medical specialty in the model. Potential determinants included the following: physician characteristics; selected vignette; assessment of control; treatment goals; comfort level with initiating long-term ICS; and level of hesitation about risk-benefit of long-term ICS in various patients. All tests were two-sided with estimates presented with 95% confidence intervals. Analyses were performed on SAS® 9.3 software (SAS Institute Inc., Cary, NC 27513, USA). P values less than 0.05 indicated statistical significance, with no correction for multiple testing and no imputation for missing data.
3. Results
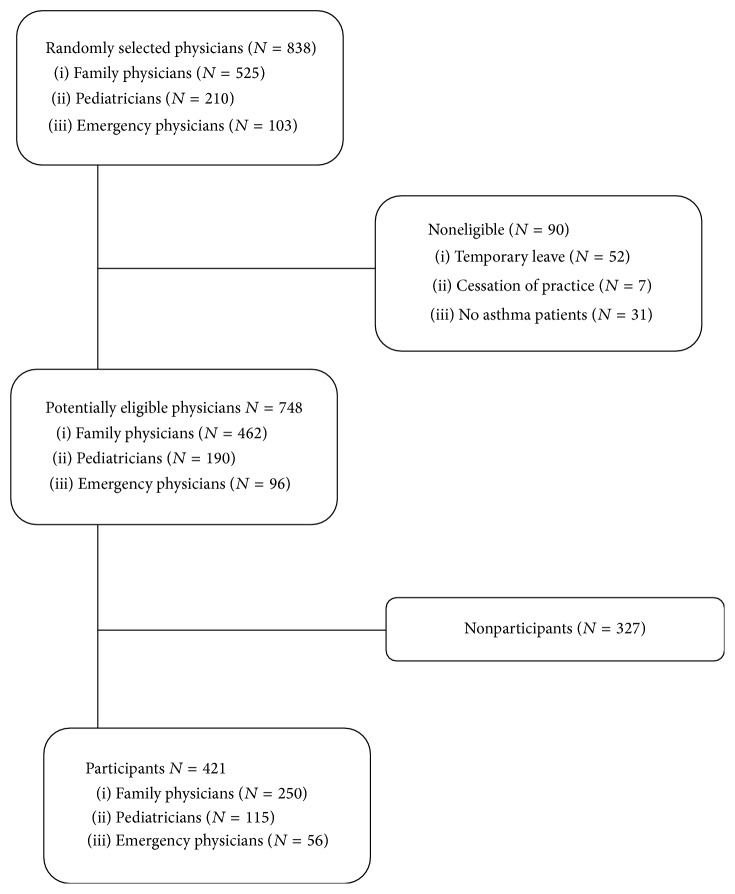
The survey was sent to 838 physicians: 525 family physicians, 210 pediatricians, and 103 emergency physicians. After excluding 90 (10.7%) noneligible physicians, 421 (56%) of 748 potentially eligible physicians returned the completed questionnaire (Figure 1). Nonrespondents were similar to the respondents in specialty and practice area but had been in practice for a median of 7 years longer with a higher proportion of males (Table E2). Participants were predominantly women (69%), working in an urban environment (93%) and nonacademic institution (44%); patients with asthma represented about a quarter of their clientele (Table 1).
Figure 1.
The flow of participants is depicted from screening to analysis.
Table 1.
Characteristics of respondents.
| Participants (N = 421) | |
|---|---|
| Male sex, n (%) | 131 (31) |
| Years in practice, median (25%, 75%) | 13 (5, 21) |
| Speciality, n (%) | |
| Family medicine | 250 (60) |
| Pediatrics | 115 (27) |
| Emergency medicine | 56 (13) |
| Primary practice location, n (%) | |
| Urban | 390 (93) |
| Rural | 31 (7) |
| Completed training, n (%)∗ | |
| Family medicine (residency) | 272 (65) |
| Pediatrics (residency or fellowship) | 121 (29) |
| Respirology (residency or fellowship) | 117 (28) |
| Emergency medicine (residency or fellowship) | 69 (16) |
| Other (residency or fellowship) | 55 (13) |
| Practice setting, n (%) | |
| Clinic with appointment | 285 (68) |
| Walk-in clinic | 168 (40) |
| Emergency room | 168 (40) |
| Intensive care unit | 26 (6) |
| Hospital wards | 171 (41) |
| Home care | 40 (10) |
| Others | 77 (18) |
| Proportion of clientele with asthma, median (25%, 75%) | 27 (18, 27) |
| Proportion of children in clientele, median (25%, 75%) | 55 (9, 82) |
| Practice in an asthma clinic, n (%) | 13 (3) |
| Self-reported being an asthma specialist, n (%) | 50 (12) |
| Usual work environment, n (%) | |
| Academic institution | 185 (44) |
| Nonacademic institution | 48 (11) |
| Private, group, or community practice | 187 (45) |
∗The training completed was not mutually exclusive. Indeed, several physicians reported two or more training programs such as family medicine (or pediatric) with emergency medicine, a popular training to serve as general (or pediatric) emergency physicians.
Approximately 60% of participants selected the acute-care vignettes, with the remainder, the clinic vignettes, equally distributed between the pediatric and adult cases. Characteristics of respondents selecting each clinical vignette, their assessment, and intended prescription are displayed in Table E3. Although nearly all physicians recognised the suboptimal asthma control, about a quarter of respondents perceived the patient as having intermittent symptoms. The overwhelming majority (94.2%) would prescribe an asthma controller, usually ICS, as monotherapy or combination therapy, and 86.0% would prescribe the controller for long-term use. Short-term treatment objectives were sought by most, particularly in acute-care vignettes, yet the overwhelming majority of physicians also reported long-term treatment goals.
Most physicians reported being comfortable with diagnosing asthma, distinguishing between intermittent and persistent asthma, assessing asthma control, and initiating long-term ICS, and reported low hesitation regarding the risk-benefit ratio of prescribing long-term ICS in the age group selected in the vignette. However, the overall comfort level was low for distinguishing between intermittent and persistent asthma without lung function tests, with significant hesitation regarding the risk-benefit ratio of prescribing long-term ICS in patients with intermittent or mild asthma (Table E4).
The three most important determinants of the intention to prescribe a long-term controller, after adjustment for speciality, were the following: the physician's goal of achieving long-term asthma control, recognition of symptoms as being persistent, and comfort level in initiating a therapy of long-term ICS (Table 2). When the comfort level was removed as a candidate variable, it was replaced by low hesitation level regarding the risk-benefit of prescribing long-term ICS (Table E5).
Table 2.
Multivariate analysis of intention of prescribing long-term asthma controller.
| Intenders¶ (N = 338) | Nonintenders¶ (N = 82) | All cases | Pediatric case vignettes | Adult case vignettes | |
|---|---|---|---|---|---|
| Odd ratios∫ (95% CI) | Odd ratios∫ (95% CI) | Odd ratios∫ (95% CI) | |||
| Types of symptoms ∗, n (%) | |||||
| Persistent | 281 (83.1) | 49 (59.8) | 2.67 (1.54, 4.63) | 2.40 (1.44, 5.02) | |
| Treatment objective ∗, n (%) | |||||
| Improving long-term control | 298 (88.4) | 42 (51.2) | 5.31 (2.74, 10.3) | 7.56 (2.99, 19.28) | |
| Level of comfort †, median (25%, 75%) | |||||
| Initiating long-term inhaled corticosteroids | 4.0 (1.0, 5.0) | 3.0 (1.0, 5.0) | 2.33 (1.67, 3.24) | 5.98 (3.00, 11.92) | 1.50 (1.02, 2.21) |
| Specialty, n (%) | |||||
| Pediatrics | 104 (30.8) | 11 (13.4) | 0.87 (0.43, 1.77) | 0.59 (0.24, 1.43) | |
| Emergency medicine | 31 (9.2) | 25 (30.5) | 0.81 (0.43, 1.54) | 0.91 (0.32, 2.62) | 0.64 (0.28, 1.46) |
| Family medicine | 203 (60.1) | 46 (56.1) | 1 | 1 | 1 |
Blank cells indicate that the variable was not statistically significant.
¶Physicians who reported prescribing long-term ICS to the patient in their selected vignette were considered “intenders” in contrast to their counterparts, considered “nonintenders.”
∗Regarding the patient in their selected case vignette.
†On a Likert scale of 0 (not comfortable at all) to 5 (very comfortable).
∫ Odds ratio adjusted for speciality.
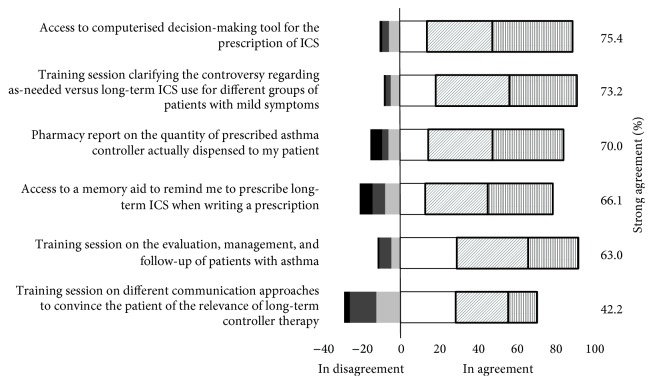
The six enablers, previously identified by physicians to support their general management approach regarding long-term ICS use [26], are depicted in Figure 2. To increase their confidence in both the patient-specific indication for, and patient adherence to, long-term ICS, physicians strongly endorsed several resources, namely, patient asthma education, lung function tests, concordant recommendation by a specialist, and shared responsibility with paramedical healthcare professionals (nurses, certified asthma educators, pharmacists, and respiratory technicians) (Table 3). Most respondents did not know the expected delay to access these resources; when known, significant median delays were reported particularly for lung function testing (1–3 months) and consultation with an asthma specialist (≥4 months) (Figure E1). There was a strong interest in having a computerised system to identify delays to these resources in various areas and to be informed of novelties in asthma management (96.1%), primarily by training days, distance online learning, and application for tablets/smartphones.
Figure 2.
This histogram depicts the physicians' endorsement, adjusted for the sampling fraction, of each proposed enablers on a Likert-like scale ranging between 5 indicating strong agreement (vertical bars), 4 (diagonal grey bars), 3 (white), 2 (light grey), 1 (medium grey), and 0 indicating strong disagreement (black). The proportion of participants with strong endorsement, that is, answering 4 or 5, is identified by a dark box in the histogram and displayed in the right column.
Table 3.
Resources that support physician's prescription of, and patient's compliance to, long-term inhaled corticosteroids (ICS).
| Enablers | ↑ physician's comfort to prescribe long-term ICS | ↑ patient adherence to long-term ICS | Access to service§ | Interest in computerised system to identify access delay |
|---|---|---|---|---|
| Adjusted proportion∗ (95% CI) | Adjusted proportion∗ (95% CI) | Adjusted proportion† (95% CI) | Adjusted proportion∗ (95% CI) | |
| Patient's asthma education | 65 (59, 71) | 95 (93, 98) | 86 (80, 90) | 67 (62, 73) |
| Finding the closest asthma education centre | — | — | — | 81 (77, 86) |
| Lung function tests for school-aged children/adults | 70 (64, 76) | 71 (65, 76)‡ | 97 (95, 99) | 70 (65, 76) |
| Lung function tests for preschoolers | 68 (62, 74) | 47 (38, 56) | ||
| Concurrent opinion from a specialist | 71 (65, 77) | 62 (57, 66) | 96 (93, 98) | 70 (65, 76) |
| Frequent follow-up visits | — | 66 (60, 71) | — | — |
| Asthma clinic to refer patients | 78 (73, 83) | — | 60 (53, 67) | 71 (65, 72) |
| Paramedical healthcare professional¶ | ||||
| To guide patient in the treatment plan | 78 (73, 83) | 92 (88, 95) | — | — |
| Available on site to provide asthma education | 76 (70, 81) | — | 52 (46, 58) | — |
| To share patient follow-up | — | — | 57 (50, 63) | — |
∗Values are reported as “adjusted proportion” of high endorsement, that is, 4 or 5 on the Likert scale, after adjustment for the stratified sampling of physicians by specialty, that is, weighting responses to reflect the distribution of physicians in the Province of Quebec using weights of 91.0% for family physicians, 7.6% for pediatricians, and 1.4% for emergency physicians.
†Values are reported as “adjusted proportion” of those that declared access, adjusted for the stratified sampling of physicians by specialty, as described above by∗.
‡Lung function testing for any age group.
¶Including nurses, certified asthma educators, pharmacists, and respiratory technicians.
4. Interpretation
In this group of randomly selected Quebec physicians, most reported that they would prescribe a long-term asthma controller, predominantly ICS, to the poorly controlled patient depicted in their selected vignette. Physicians highly endorsed training and tools to support their general management approach. With regard to patient-specific decision-making, key enablers to improve their comfort level in prescribing, and perceived patient adherence to, long-term ICS included the following: patient asthma education, lung function testing, concordant opinion by a specialist, having access to an asthma clinic to refer patients, and paramedical healthcare professionals to assist in guided self-management. The most important features distinguishing physicians who would prescribe a long-term asthma controller were the recognition of symptoms as being persistent, their high comfort level in initiating long-term ICS, and their goal of improving long-term asthma control. The substitution of comfort level in, by less hesitation regarding the risk-benefit ratio of, prescribing long-term ICS suggested that the latter is inversely and closely related to the former.
The strong endorsement of specific training sessions, decision-support tools, reminders, and pharmacy reports of drug claims to support the general management approach is aligned with prior studies [32]. In these studies, physicians voiced, as barriers to optimal asthma management, their confidence about capabilities in prescribing, and beliefs about consequences of, long-term ICS, as well as their worry about patients' noncompliance and the absence of patient follow-up [10, 33, 34]. In addition, key resources that increase physician's reported comfort in prescribing long-term ICS and perceived patient adherence were endorsed for patient-specific management, presumably because of more certainty in the management decision (i.e., lung function testing, specialist's opinion, and access to an asthma clinic), greater degree of collaborative care and patient follow-up (i.e., patient guidance and education provided by a paramedical healthcare professional) [33]. A highly valued proposal was to provide computerised systems to identify the delay for access to these resources, a solution implemented with success for emergency wait time [35]. Most strongly endorsed enablers have been shown to be effective to improve physicians' prescription in general, and of asthma controllers specifically, namely, facilitated workshops (by improving knowledge, attitude, skills, and beliefs) [36], decision-support tools [32] and, to a lesser extent, reminders [37], and organisational changes [32].
With over four-fifths prescribing long-term asthma controller to their patient in the clinical vignettes, the prescription behaviour was highly concordant with recent national and international guidelines [1, 4, 38]. Yet, it contrasted with published prescription patterns varying between 17% and 69% of patients receiving ICS in Quebec and elsewhere [10, 15, 39], often with inadequate number of renewals to enable long-term use [15, 16]. The latter suggests more emphasis on physician's short-term treatment goals and/or suboptimal prescription filling by patients [39]. Although reported prescribing behaviour may overestimate real practice patterns, the apparent discrepancy with prescriptions studies may be due in part to the fact that poorly controlled patients as described in the vignettes may represent a small proportion of patients enrolled in drug claim data; alternatively it may reflect evolving practice patterns [40].
In contrast to prior reports indicating the lowest use of long-term asthma controller by emergency physicians compared to family physicians and other specialists [10, 27, 33, 39], specialty or practice setting was not important in the multivariate analysis. Indeed, physicians' perceived patient need for ICS, treatment goals, confidence about capabilities in prescribing, and/or knowledge of risk-benefit regarding long-term ICS, all recognised domains for effective implementation of any health behaviour, appear to be the key operational constructs in the prescription of long-term ICS [27]. This is in line with prior reports, in which confidence about capabilities was associated with an 2.8 OR of prescribing ICS [10]. The strength of associations and consistency of predictors across age groups in our vignettes underline the robustness of the predictors of intention.
Despite a large sample size and the strength and precision of identified associations, we acknowledge the following study limitations. Consistent with prior physician surveys, there was a slight overrepresentation of female physicians and, importantly, those in practice for a shorter period [41]; findings may thus reflect more the practice of physicians trained under recent guidelines than those trained when guidelines and teaching methods were different. We acknowledge the possibility of a social desirability bias, that is, the tendency for physicians to report the perceived desired response rather than their true behaviour, which would overestimate actual use of ICS. To minimise such bias, we provided a large range of response options for management questions in vignettes and reversed questions, asking first about management and last about patient assessment and treatment goals. Recent data showing concordance in determinants of prescription of ICS, such as those observed in this study, suggest generalizability [10].
The study was conducted in Quebec where there is free access to medical care, free patient asthma education, and a subsidised drug plan for residents. Despite our long questionnaire, our 56% response rate (59%, assuming that 11% of nonresponders were ineligible as noted among those reached) is within expected standards (54%–60%) for physician surveys, in which higher response rates are generally not associated with less bias [41]. Our objective to have a representative sample of physicians treating patients with asthma resulted in a large proportion of respondents being family physicians. Their frequent selection of the acute-care and pediatric vignettes suggests that an important proportion of these patients are indeed treated by family physicians in Quebec, which may not be applicable to other countries. Caution is thus advised before generalization of the study results to other healthcare settings or specialties.
The overwhelming majority of surveyed physicians reported prescribing long-term ICS to the poorly controlled patient in the clinical vignette, attesting to their intention. In line with the observed determinants of intention, training sessions and decision-support tools to improve physician recognition of persistent symptoms, the importance of long-term asthma control, and confidence in, or knowledge about the risk-benefits of, initiating long-term ICS carry the best chance of improving the rate of long-term ICS prescriptions in patients with persistent asthma. Enhancing access to key resources to support patient-specific management decisions appears to be crucial enablers to optimal asthma management and may lead to greater patient adherence. The physician-endorsed strong enablers provide important insights into design promising implementation interventions to improve long-term ICS prescription.
Supplementary Material
The supplemental materiel describes the clinical vignettes (Table E1), the comparison between participants and non-participants (Table E2), the reported assessment of, and prescription for, each case vignette (Table E3), the beliefs about capabilities and consequences regarding the prescription of long-term asthma controller (Table E4), the multivariate analysis of physician's intention of prescribing long-term asthma controller (Table E5) and the reported access to each resource (Figure E1).
Acknowledgments
This work was funded through a research Grant (no. 233813) awarded through a peer-review process by the Canadian Institutes of Health Research (CIHR), Canada. The authors acknowledge the support of the Fonds de la Recherche du Québec en Santé for the infrastructure support provided to the Research Institute of the Centre Hospitalier Universitaire Sainte-Justine (CHUSJ). They are indebted to the Lucie Bergeron and Johanne St-Pierre for providing the list of the College des Médecins du Québec, Benoit Mâsse for preparing the randomisation list, and Katia Lessard, Bhupendrasinh Chauhan, Megan Jensen, Marie-France Goyer, and Annie Théorêt for assisting with the mailing of questionnaires and/or phoning of participants. They thank Annie Théorêt for assistance in paper preparation.
Abbreviations
- ICS:
Inhaled corticosteroids.
Disclosure
This work was presented in part at the annual Canadian Paediatric Society meeting, June 2014, Toronto, Canada.
Competing Interests
The authors declare that they have no competing interests.
References
- 1.GINA Global Initiative for Asthma Program. Global Strategy for Asthma Management and Prevention. Global Initiative for Asthma; 2014. http://www.ginasthma.org/ [Google Scholar]
- 2.British Thoracic Society Scottish Intercollegiate Guidelines Network. British Thoracic Society Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. Thorax. 2014;69:i1–i192. [Google Scholar]
- 3.Lougheed M. D., Lemiere C., Ducharme F. M., et al. Canadian Thoracic Society 2012 guideline update: diagnosis and management of asthma in preschoolers, children and adults. Canadian Respiratory Journal. 2012;19(2):127–164. doi: 10.1155/2012/635624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Asthma Education Prevention Program. NAEPP Expert Panel Report-Guidelines for the Diagnosis and Management of Asthma-Update on Selected Topics 2007. 2007. (NIH publication No 02-5075). [PubMed] [Google Scholar]
- 5.National Asthma Control Initiative. Putting Guideline Priorities into Action. 2013. https://www.nhlbi.nih.gov/health-pro/resources/lung/naci/discover/priorities.htm. [Google Scholar]
- 6.Vollmer W. M., Markson L. E., O'Connor E., et al. Association of asthma control with health care utilization and quality of life. American Journal of Respiratory and Critical Care Medicine. 1999;160(5):1647–1652. doi: 10.1164/ajrccm.160.5.9902098. [DOI] [PubMed] [Google Scholar]
- 7.Boulet L.-P., McIvor R. A., Marciniuk D. Respiratory guidelines implementation in Canada. Canadian Respiratory Journal. 2007;14(6):329–330. doi: 10.1155/2007/592534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McIvor R. A., Boulet L. P., FitzGerald J. M., Zimmerman S., Chapman K. R. Asthma control in Canada: no improvement since we last looked in 1999. Canadian Family Physician. 2007;53(4):672–677. [PMC free article] [PubMed] [Google Scholar]
- 9.FitzGerald J. M., Boulet L.-P., Mclvor R. A., Zimmerman S., Chapman K. R. Asthma control in Canada remains suboptimal: the reality of asthma control (TRAC) study. Canadian Respiratory Journal. 2006;13(5):253–259. doi: 10.1155/2006/753083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wisnivesky J. P., Lorenzo J., Lyn-Cook R., et al. Barriers to adherence to asthma management guidelines among inner-city primary care providers. Annals of Allergy, Asthma and Immunology. 2008;101(3):264–270. doi: 10.1016/S1081-1206(10)60491-7. [DOI] [PubMed] [Google Scholar]
- 11.Rabe K. F., Adachi M., Lai C. K. W., et al. Worldwide severity and control of asthma in children and adults: the global asthma insights and reality surveys. Journal of Allergy and Clinical Immunology. 2004;114(1):40–47. doi: 10.1016/j.jaci.2004.04.042. [DOI] [PubMed] [Google Scholar]
- 12.Cane J., O'Connor D., Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Science. 2012;7, article 37 doi: 10.1186/1748-5908-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cydulka R. K., Tamayo-Sarver J. H., Wolf C., Herrick E., Gress S. Inadequate follow-up controller medications among patients with asthma who visit the emergency department. Annals of Emergency Medicine. 2005;46(4):316–322. doi: 10.1016/j.annemergmed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 14.Ducharme F. M., Zemek R. L., Chalut D., et al. Written action plan in pediatric emergency room improves asthma prescribing, adherence, and control. American Journal of Respiratory and Critical Care Medicine. 2011;183(2):195–203. doi: 10.1164/rccm.201001-0115OC. [DOI] [PubMed] [Google Scholar]
- 15.Blais L., Beauchesne M.-F. Use of inhaled corticosteroids following discharge from an emergency department for an acute exacerbation of asthma. Thorax. 2004;59(11):943–947. doi: 10.1136/thx.2004.022475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pando S., Lemière C., Beauchesne M.-F., Perreault S., Forget A., Blais L. Suboptimal use of inhaled corticosteroids in children with persistent asthma: inadequate prescription, poor drug adherence, or both? Pharmacotherapy. 2010;30(11):1109–1116. doi: 10.1592/phco.30.11.1109. [DOI] [PubMed] [Google Scholar]
- 17.Ducharme F. M., Noya F. J. D., Allen-Ramey F. C., Maiese E. M., Gingras J., Blais L. Clinical effectiveness of inhaled corticosteroids versus montelukast in children with asthma: prescription patterns and patient adherence as key factors. Current Medical Research and Opinion. 2012;28(1):111–119. doi: 10.1185/03007995.2011.640668. [DOI] [PubMed] [Google Scholar]
- 18.Meng Y.-Y., Leung K.-M., Berkbigler D., Halbert R. J., Legorreta A. P. Compliance with US asthma management guidelines and specialty care: a regional variation or national concern? Journal of Evaluation in Clinical Practice. 1999;5(2):213–221. doi: 10.1046/j.1365-2753.1999.00177.x. [DOI] [PubMed] [Google Scholar]
- 19.Finkelstein J. A., Lozano P., Shulruff R., et al. Self-reported physician practices for children with asthma: are national guidelines followed? Pediatrics. 2000;106(4):886–896. [PubMed] [Google Scholar]
- 20.Cabana M. D., Rand C. S., Powe N. R., et al. Why don't physicians follow clinical practice guidelines?: a framework for improvement. The Journal of the American Medical Association. 1999;282(15):1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 21.Baena-Cagnani C. E., Berger W. E., DuBuske L. M., et al. Comparative effects of desloratadine versus montelukast on asthma symptoms and use of β2-agonists in patients with seasonal allergic rhinitis and asthma. International Archives of Allergy and Immunology. 2003;130(4):307–313. doi: 10.1159/000070218. [DOI] [PubMed] [Google Scholar]
- 22.Cabana M. D., Ebel B. E., Cooper-Patrick L., Powe N. R., Rubin H. R., Rand C. S. Barriers pediatricians face when using asthma practice guidelines. Archives of Pediatrics and Adolescent Medicine. 2000;154(7):685–693. doi: 10.1001/archpedi.154.7.685. [DOI] [PubMed] [Google Scholar]
- 23.Grimshaw J. M., Thomas R. E., MacLennan G., et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technology Assessment. 2004;8(6):30–72. doi: 10.3310/hta8060. [DOI] [PubMed] [Google Scholar]
- 24.Grimshaw J. M., Shirran L., Thomas R., et al. Changing provider behavior: an overview of systematic reviews of interventions. Medical Care. 2001;39(8):II2–II45. [PubMed] [Google Scholar]
- 25.Bhogal S. K., McGillivray D., Bourbeau J., et al. Focusing the focus group: impact of the awareness of major factors contributing to non-adherence to acute paediatric asthma guidelines. Journal of Evaluation in Clinical Practice. 2011;17(1):160–167. doi: 10.1111/j.1365-2753.2010.01416.x. [DOI] [PubMed] [Google Scholar]
- 26.Lamontagne A. J., Peláez S., Grad R., et al. Facilitators and solutions for practicing optimal guided asthma self-management: the physician perspective. Canadian Respiratory Journal. 2013;20(4):285–293. doi: 10.1155/2013/146839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cabana M. D., Abu-Isa H., Thyne S. M., Yawn B. Specialty differences in prescribing inhaled corticosteroids for children. Clinical Pediatrics. 2007;46(8):698–705. doi: 10.1177/0009922807301436. [DOI] [PubMed] [Google Scholar]
- 28.Bero L. A., Grilli R., Grimshaw J. M., Harvey E., Oxman A. D., Thomson M. A. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. The British Medical Journal. 1998;317(7156):465–468. doi: 10.1136/bmj.317.7156.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grimshaw J., Eccles M., Campbell M., Elbourne D. Cluster randomized trials of professional and organizational behavior change interventions in health care settings. Annals of the American Academy of Political and Social Science. 2005;599:71–93. doi: 10.1177/0002716205274576. [DOI] [Google Scholar]
- 30.Dillman D. A. Mail and Internet Surveys: The Tailored Design Method. New York, NY, USA: John Wiley & Sons; 2000. [Google Scholar]
- 31.Robbins N., Heiberger R. M. Plotting likert and other rating scales. Proceedings of the Joint Statistical Meeting; July-August 2011; Miami, Fla, USA. NBR and Temple University; pp. 1058–1066. [Google Scholar]
- 32.Okelo S. O., Butz A. M., Sharma R., et al. Interventions to modify Health care provider adherence to asthma guidelines: a systematic review. Pediatrics. 2013;132(3):517–534. doi: 10.1542/peds.2013-0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Andrews A. L., Teufel R. J., Basco W. T., Jr. Initiating inhaled steroid treatment for children with asthma in the emergency room: current reported prescribing rates and frequently cited barriers. Pediatric Emergency Care. 2013;29(9):957–962. doi: 10.1097/pec.0b013e3182a219d0. [DOI] [PubMed] [Google Scholar]
- 34.Cabana M. D., Rand C. S., Becher O. J., Rubin H. R. Reasons for pediatrician nonadherence to asthma guidelines. Archives of Pediatrics and Adolescent Medicine. 2001;155(9):1057–1062. doi: 10.1001/archpedi.155.9.1057. [DOI] [PubMed] [Google Scholar]
- 35.Resar R., Nolan K., Kaczynski D., Jensen K. Using real-time demand capacity management to improve hospitalwide patient flow. Joint Commission Journal on Quality and Patient Safety. 2011;37(5):217–227. doi: 10.1016/s1553-7250(11)37029-8. [DOI] [PubMed] [Google Scholar]
- 36.French S. D., Green S. E., O'Connor D. A., et al. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implementation Science. 2012;7, article 38 doi: 10.1186/1748-5908-7-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shojania K. G., Jennings A., Mayhew A., Ramsay C. R., Eccles M. P., Grimshaw J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database of Systematic Reviews. 2009;(3) doi: 10.1002/14651858.CD001096.pub2.CD001096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ducharme F. M., Dell S. D., Radhakrishnan D., et al. Diagnosis and management of asthma in preschoolers: a Canadian Thoracic Society and Canadian Paediatric Society position paper. Paediatrics and Child Health. 2015;20(7):135–143. doi: 10.1093/pch/20.7.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Andrews A. L., Teufel R. J., II, Basco W. T., Jr. Low rates of controller medication initiation and outpatient follow-up after emergency department visits for asthma. Journal of Pediatrics. 2012;160(2):325–330. doi: 10.1016/j.jpeds.2011.07.037. [DOI] [PubMed] [Google Scholar]
- 40.Andrews A. L., Russell W. S., Titus M. O., et al. Quality improvement methods improve inhaled corticosteroid prescribing in the emergency department. Journal of Asthma. 2014;51(7):737–742. doi: 10.3109/02770903.2014.911885. [DOI] [PubMed] [Google Scholar]
- 41.Flanigan T., McFarlane E., Cook S. Conducting survey research among physicians and other medical professionals: a review of current literature. Proceedings of the Survey Research Methods Section (AAPOR '08); 2008; New Orleans, La, USA. American Statistical Association; pp. 4136–4147. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The supplemental materiel describes the clinical vignettes (Table E1), the comparison between participants and non-participants (Table E2), the reported assessment of, and prescription for, each case vignette (Table E3), the beliefs about capabilities and consequences regarding the prescription of long-term asthma controller (Table E4), the multivariate analysis of physician's intention of prescribing long-term asthma controller (Table E5) and the reported access to each resource (Figure E1).