Abstract
Background:
Non-alcoholic fatty liver disease (NAFLD) is characterized by macro vesicular steatosis in the absence of alcohol. Patients with (NAFLD)need extensive education and support in their treatment. Our aim was to investigate the effect of telenursing on liver enzymes (ALT and AST) in patients with NAFLD.
Methods:
Our study is a randomized controlled clinical trial. In this study, 60 patients were enrolled from patients who referred to subspecialty gastrointestinal clinics affiliated to Shiraz University of Medical Sciences. Specialists confirmed their diseases by ultrasound and laboratory test. Simple randomization, based on random number table, was used to randomize the participants into intervention (N=30) and control (N=30) groups. Patients in both groups received dietary advice from a nutritionist and were trained to perform physical activities. Telephone intervention in the intervention group lasted for 12 weeks, in order to see the effect of follow up on the recommended diet and physical activities given by the specialist, while; the control group subjects were only followed up as usual by their physician.
Results:
The result of an independent t-test showed that the mean difference of liver Enzymes between the two groups was statistically significant (P<0.001). The difference of AST and ALT in the intervention and control groups was 18.03, -1.27 and 40.70, 1.52, respectively.
Conclusion:
We found out that; telenursing could have a positive effect on reduction of liver enzymes (ALT, AST) in patients with NAFLD.
Trial Registration Number: IRCT2015040411691N5
KEYWORDS: Diet, Nonalcoholic fatty liver disease, Physical activity, Telenursing
INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD) represents a range of clinical pathologic conditions characterized by macro-vesicular steatosis in the absence of alcohol. It comprises of a wide spectrum of liver diseases ranging from simple steatosis to non-alcoholic liver diseases, such as non-alcoholic steatohepatitis, fibrosis, cirrhosis, and liver cancer. NAFLD is known as one of the most common liver diseases in Western countries.1 In addition, approximately 25% of their adult population suffers from this disease2 and its prevalence is 2-3 times higher than hepatitis B and C or other alcohol-related liver diseases. Besides, it is the most common cause of abnormal liver function tests.3 In Iran, the prevalence of NAFLD is reported 2.8%.1 Recent studies in Eastern Asian countries showed that the spread of the disease has increased due to changes in people’s lifestyle and dietary patterns (highfat and high-carbohydrate diet, low physical activity, obesity, and diabetes mellitus type 2).3 Recently, NAFLD has been increasing due to the prevalence of obesity.2 Amongst the patients with NAFLD, 39-100% of them are obese.1 Several studies have shown an increase in serum alanine aminotransferase (ALT) level more than aspartate aminotransferase (AST) which is a sign of NAFLD that is associated with obesity, metabolic syndromes, and insulin resistance which leads to inflammation of the liver that has resulted from accumulation of fat in the liver.4 Until now, there has been no special treatment for patients with such disease and the only pharmaceutical therapies such as metformin, teazolidy and free radical inhibitors such as vitamin E are recommended.5 All specialists confirm that the most effective way is modification in lifestyle, daily exercise, healthy diet for prevention and treatment of NAFLD.5,6 A proper diet that can reduce the weight up to 10% could solve metabolic and histological disorders associated with this disease.7,8 Moreover, evidence suggests that regular exercise 3 to 4 times a week can be beneficial.9 Tendler and colleagues conducted a study on the effects of a low-calorie diet in patients with NAFLD and observed a significant decrease in the body weight, liver enzymes (ALT and AST) as well as a significant improvement in their ultrasound result.10 In another study, Hickman and colleagues examined the effects of 15-month diet and exercise with a focus on weight loss and Modified BMI. They reported a significant reduction in BMI, liver enzymes and also improvement in the patients’ quality of life.11 From every three patients with NAFLD, one is potentially exposed to the risk of cirrhosis and advanced liver failure.12 In the absence of timely diagnosis, appropriate treatment and followups, symptoms of liver failure will prevail. Furthermore, these patients are more exposed to diseases such as coronary heart, chronic renal disorders and carotid atherosclerosis compared with healthy individuals.2,8
Follow-up is an essential part of the care. Frequent and regular follow-up in order to intervene is essential to promote healthy behavior. Patients’ followed-up can lead to change in their behavior.13 Some studies indicate that regular follow-up helps the patients and their families to participate actively in the rehabilitation process and control the disease.13-16 American Nursing Association states that (telenursing) is a sub-branch of telemedicine that focuses on providing specific nursing services.17 It is beneficial for patients as it increases the access to effective care through telecommunication devices. Technologies used in telenursing include telephone, fax, internet, and audio and visual communication devices. Among different means of communication devices, telephone is the most available device in societies. Using telephone in providing care can reduce the costs, facilitate the access to an effective care, and improve the relationship between the patients and care providers. Currently, the use of telenursing enables the nurses to perform actions such as patient monitoring, patient education, data collection, nursing interventions, pain management, and patients’ family protection.18 Therefore, by applying such method, we can provide care in a short time and replace hospital care by community-based care training and patient– oriented care.14 Thus, NLFD can be controlled in the early stages by informing the patients about the process of the disease. By providing appropriate education on dieting, weight loss, increased physical activity, and following the improvement process, we can prevent unpleasant complications. Considering the importance of such issues, we aimed to investigate the effect of telenursing on liver enzymes (ALT and AST) in the patients with NAFLD.
MATERIALS AND METHODS
This randomized controlled clinical trial study was conducted from May 2013 to Dec 2014, and ethics committee approval was obtained from the ethics committee of Shiraz University of Medical Sciences (Ethics committee code CT-92-92-62-6602). Based on the results from previous studies, we enrolled 60 patients with NAFLD who referred to subspecialty gastroenterology clinics affiliated with Shiraz University of Medical Sciences.7,9,19,20 The sample size was estimated by the following formula:
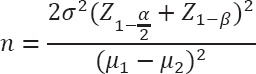
(SD1=17.5, SD2=15, μ1=48, μ2=36.2,α=0.05, 1-β=0.8)
Their disease was confirmed by a physician, using ultrasound and laboratory tests. Inclusion criteria were age 19 years old or older and overweight or obesity (BMI up to 25), capability to perform moderate physical activity confirmed by medical professionals, access to a telephone at home or a mobile phone, lack of any speech and hearing problems. The exclusion criteria included a history of chronic liver disease such as viral or drug hepatitis, confirmed diagnosis of Wilson diseases, primary hemochromatosis, hyperthyroidism or hypothyroidism, bile duct cancer, diabetes mellitus, obesity due to excessive use of corticosteroid, Cushing’s syndrome, Addison syndrome, chronic infections such as tuberculosis, use of hepatotoxic drugs within the past 6 months, incidence of gall stones in the gallbladder, having been exposed to petrochemicals, alcohol consumption, drug abuse, genetic diseases related to lipid disorders.
After obtaining written informed consent, simple randomization, based on random number table, was used to randomize the participants into intervention (N=30) and control (N=30) groups. The design and protocol of the study is shown in figure 1. The numbers 0 through 4 were allocated to the control group and numbers 5 through 9 to the intervention group. Initially, the researcher explained to all participants about the nature of the disease, factors contributing to illness, progression and prognosis, complications of the disease and the importance of the treatment and follow-ups for the patients. The researcher asked the participants to complete demographic information form. For all participants, the serum levels of ALT and AST were determined by the same laboratory. Height and weight were measured by the same meter and scale and body mass index was calculated by the researcher.
Figure 1.
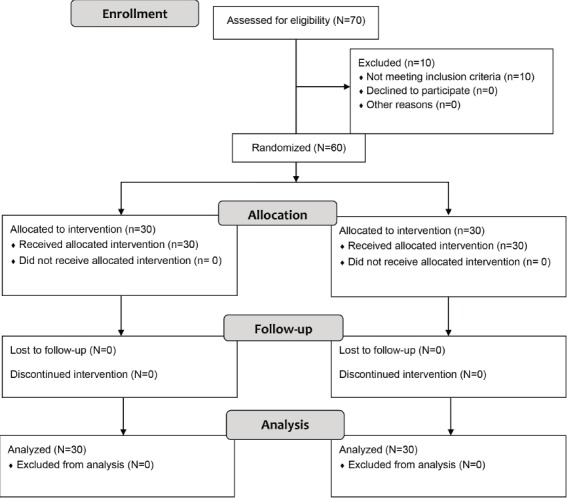
Design and protocol of the study
A nutritionist offered counseling for all participants in both intervention and control groups. They also received dietary advice provided in a written form. Then patients were asked to do some sorts of moderate physical activities at least 30 minutes a day, 4 to 5 times a week to increase their heart rate and respiration. The physical activities included jogging, cycling, aerobic exercise or any other activity that is of a similar intensity. In addition to face-to-face consultation, all the participants received a training pamphlet.
In the intervention group, telephone intervention lasted for 12 weeks in a way to follow-up the recommended diet and physical activity. The researcher contacted the patients twice a week during the first month and once a week in the second and the third months. The average duration of each call was 15 to20 minutes between 8 AM to 8 PM that was confirmed by patients.13,17
The participants were also given self-report forms, which was designed by the researcher, to record their daily diet and physical activities. This helped the patients to easily report the items based on the form during telephone follow-ups. Conversation content included evaluating the adherence to diet and physical activities. Also, if a patient did not adhere to the diet and training program, the researcher tried to identify and analyze the reason and ultimately provide a possible solution. In addition, in each telephone session, conversation was recorded in a preprepared form by the researcher.
During the intervention period, the control group received no intervention by the researcher and was only followed up as usual by a specialist and also received educational booklet after the intervention. At the end of the 12th week, serum levels of liver enzymes were measured again by the same laboratory that preformed the pretests. Also height and weight were measured by the same meter and scale and body mass index was calculated by the researcher again.
The data that were collected from the participants both before and after the intervention were analyzed using SPSS software (version 16) and Chi-square test, Paired t-test and independent t-test.
RESULTS
There were 30 patients in the intervention group, of whom 8 were women (26.7%) and 22 men (73.3%). There were also 30 in the control group of whom 6 were women (20.7%) and 23 were men (79.3%). The mean age of the patients was 40.3 and 38.3 in the intervention and control groups, respectively. In this regard, independent t-test showed no statistically significant difference between the two groups.
The results of Fisher’s exact test indicated no significant difference between the two groups with respect to marital and educational status. According to the result of Chi-square test, there was no significant difference between the two groups as to gender. Therefore, all patients in both groups were similar with regards to demographic characteristics. Also, the mean weight before the intervention in the intervention and control groups was 83.76 Kg and 84.15 kg, and the mean of BMI before the intervention in the intervention and control groups was 28.8 and 28.5, respectively. Results of the independent t-test showed no statistically significant difference between the two groups in the mean weight and BMI before the intervention (P>0.05).
After the intervention, the mean weights in the intervention and control groups were 76.75 Kg and 82.35 Kg, respectively. Results of the independent t-test revealed that only changes in the mean weight of the intervention group was statistically significant (P<0.001), and also the mean of BMI in the intervention and control groups was 26.36 and 27.92, respectively. Results of the independent t-test showed that only changes in the mean of BMI in intervention group was statistically significant after the intervention (P<0.001).
Prior to the intervention, the mean±SD, ALT in the intervention and control groups was 80.3±38.59 and 63.52±23.67 (P=0.050), and the mean±SD AST in the intervention and control groups was 46.83±17.64 and 38.52±12.09 (P= 0.039). Independent t-test showed no significant differences between the two groups regarding the changes in the mean of liver enzymes before the intervention.
According to table 1, the liver enzymes (ALT, AST) decreased in the intervention group but it increased in the control group after the intervention. Paired t-test showed that such a change in the intervention group was statistically significant (P<0.001).
Table 1.
Comparison of the means of liver enzymes in the intervention and control groups before and after the intervention
| Variables | Mean±SD | P value | |||
|---|---|---|---|---|---|
| Liver Enzymes | AST | Intervention group | Before intervention | 46.83±17.64 | <0.001 |
| After intervention | 28.80±9.85 | ||||
| Control group | Before intervention | 38.52±12.9 | 0.665 | ||
| After intervention | 39.79±15.33 | ||||
| ALT | Intervention group | Before intervention | 80.30±38.59 | <0.001 | |
| After intervention | 36.60±19.27 | ||||
| Control group | Before intervention | 63.52±23.67 | 0.739 | ||
| After intervention | 28.68±65.03 | ||||
Table 2 shows that according to the independent t-test, the mean difference of liver enzymes was statistically significant in the intervention group compared with the control group before and after the intervention (P<0.001).
Table 2.
Comparison of the mean difference of liver enzymes in the intervention and control groups before and after the intervention
| Variables | Mean±SD | P value | ||
|---|---|---|---|---|
| Liver Enzymes | AST | Intervention group | 18.03±17.01 | <0.001 |
| Control group | -1.27±15.70 | |||
| ALT | Intervention group | 40.70±34.85 | <0.001 | |
| Control group | 1.52±24.26 | |||
DISCUSSION
After 12 weeks of intervention, we observed that the mean weight and BMI decreased in the intervention group in comparison to the control group (mean weight and BMI in the intervention group were 76.75 and 26.36 and in the control group they were 82.35 and 27.92. However, based on the paired t-test, these changes were statistically significant only in the intervention group (P<0.001). The mean difference of weight (in the intervention group it was 7.01 and in the control group 1.80) and BMI (in the intervention group it was 2.45 and in the control group 0.62) was statistically significant in the intervention group before and after the intervention when compared with the control group (P<0.001). Also, according to table 1, paired t-test showed that the mean±SD of liver enzymes (ALT, AST) in the intervention group decreased significantly but it increased in the control group after the intervention. According to table 2, independent t-test showed that the mean difference of liver enzymes was statistically significant in the intervention group compared with the control group before and after the intervention (P<0.001). The reason for increased level of the liver enzyme in the control group was noncompliance with the treatment regimen, while in the intervention group subjects who had undergone the intervention, the level of liver enzyme was decreased; this reflects the impact of the telenursing on the decrease of the level of the liver enzyme in these patients.
The results of our study were also similar to those of other studies, showing the effect of diet and physical activity on improving liver serum enzyme in patients with NAFLD.5,11,21,22,23 In one study, the researchers examined the effects of a 3-month exercise and dietary modification on serum amino transferase levels and body mass of 28 patients with NAFLD. After three months of intervention, significant decreases were observed in the weight, body mass index and liver enzyme.19 The results of another study, which was performed on 27 men and women with NAFLD, showed that diet and physical activity, including walking and jogging for three months, could improve the liver aminotransferase level.24 In a similar study, the researchers observed that a 24-week low calorie diet was accompanied by weight loss and a significant improvement in ALT levels in patients.10,25 However, due to the chronic nature of such diseases, the patients’ compliance to the treatment and learning to adapt and change the lifestyle need time and continuous monitoring by a treatment team. Thus, in addition to training, follow-ups with the aim to establish and develop a continuous caring relationship is required to increase the awareness and strengthen the process of care which improves the quality of life and health care services, reduces the symptoms, and increases the client’s satisfaction.26,27 Our findings suggest that telenursing for monitoring the diet and physical activity instruction is an effective tool for NAFLD treatment.
In recent years, several studies have been undertaken by offering care through telephone and similar results were achieved with regards to the effectiveness of telenursing on the adherence to diet.13,15 In one study, the researchers investigated the effect of telenursing on adherence of diabetic patients with type 2 diabetes mellitus to their diet. The results showed that telenursing improved the dietary adherence in such patients.18 In another study, the researchers evaluated the effect of this technique on glycemic and lipid control on 60 patients with type 2 diabetes mellitus. The results indicated that after 12-weeks of telenursing glycosylated hemoglobin, cholesterol, triglyceride and LDL levels were decreased in the intervention group in comparison to the control group.28
CONCLUSION
We can conclude that telenursing could promote healthy behavior in patients with NAFLD by increasing their awareness towards the disease and a treatment that can lead to reduction in the level of liver enzymes in patients with NAFLD. Telenursing can provide counseling services by phone after receiving clinical advice from a physician as well as continuous trainings that could have a positive effect and help the patient with NAFLD to have healthy behaviors and also help to improve the results of treatment.
ACKNOWLEDGEMENT
The present article was extracted from the thesis written by Sorur Javanmardi Fard and was financially supported by Shiraz University of Medical Sciences (Grant No 6602). The authors hereby express their thanks and appreciation to all those who helped us to conduct this study and the patients who kindly participated in this research project. The authors would also like to thank the Research Consulting Center (RCC) of Shiraz University of Medical Sciences for the assistant in editing this manuscript.
Conflict of Interest: None declared.
REFERENCES
- 1.Khoushbaten M, Fatahi E, Soomi H, et al. Clinico-Biochemical comparison of patients with nonalcoholic fatty liver disease and healthy population. ZJRMS. 2009;11:13–21. [In Persian] [Google Scholar]
- 2.Jamali R, Jamali A. A Non-alcoholic fatty liver disease. Feyz, Journal of Kashan University of Medical Sciences. 2010;14:169–81. [In Persian] [Google Scholar]
- 3.Park SH. Current status of liver disease in Korea: Nonalcoholic fatty liver disease. The Korean Journal of Hepatology. 2009;15:S34–9. doi: 10.3350/kjhep.2009.15.S6.S34. [DOI] [PubMed] [Google Scholar]
- 4.Chen ZW, Chen LY, Dai HL, et al. Relationship between alanine aminotransferas levels and metabolic syndrome in nonalcoholic fatty liver disease. J Zhejiang Univ Sci B. 2008;9:616–22. doi: 10.1631/jzus.B0720016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akyüz F, Demir K, Ozdil S, et al. The effects of rosiglitazone, metformin, and diet with exercisein nonalcoholic fatty liver disease. Dig Dis Sci. 2007;52:2359–67. doi: 10.1007/s10620-006-9145-x. [DOI] [PubMed] [Google Scholar]
- 6.Caldwell S, Lazo M. Is exercise an effective treatment for NASH? Knowns and unknowns. Ann of Hepatol. 2009;8:S60–6. [PubMed] [Google Scholar]
- 7.Nikrou H, Nemati M, Sima H, Attarzadeh Hoseini R. Effect of diet with or without exercise program on anthropometric and cardiorespiratory fitness in patients with non-alcoholic steatohepatitis. Journal of North Khorasan University of Medical Sciences. 2011;3:91–9. [In Persian] [Google Scholar]
- 8.Ekstedt M. Non-Alcoholic Fatty Liver Disease: A clinical and histopathological study [thesis] Sweden: LNU; 2008. [Google Scholar]
- 9.Davoodi M, Moosavi H, Nikbakht M. The effect of eight weeks selected aerobic exercise on liver parenchyma and liver enzymes (AST, ALT) of fat liver patients. Journal of Shahrekord University of Medical Sciences. 2012;14:84–9. [In Persian] [Google Scholar]
- 10.Tendler D, Lin S, Yancy WS Jr, et al. The Effect of a Low-Carbohydrate, Ketogenic Diet on Nonalcoholic Fatty Liver Disease: A Pilot Study. Dig Dis Sci. 2007;52:589–93. doi: 10.1007/s10620-006-9433-5. [DOI] [PubMed] [Google Scholar]
- 11.Hickman IJ, Jonsson JR, Prins JB, et al. Modest weight loss and physical activity in overweight patients with chronic liver disease results in sustained improvements in alanine aminotransferase, fasting insulin, and qualityof life. Gut. 2004;53:413–9. doi: 10.1136/gut.2003.027581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hosseinzadeh T, Paryad E, Kazemnejad E, Asiri Sh. Predictors of Diet Self-Efficacyin Coronary Artery Disease Patients. Holistic Nursing and Midwifery Journal. 2010;20:8–13. [In Persian] [Google Scholar]
- 13.Aliha JM, Asgari M, Khayeri F, et al. Group Education and Nurse-Telephone Follow-Up Effects on Blood Glucose Control and Adherence to Treatment in Type 2 Diabetes Patients. International Journal of Preventive Medicine. 2013;4:797–802. [PMC free article] [PubMed] [Google Scholar]
- 14.Sadeghi T, Shahabinejad M, Derakhshan R, Balaii P. Effect of Nurse - led Telephon Follow up (Telenursing) on HbA1c among Diabetic Patients. Journal of Rafsanjan University Of Medical Sciences. 2010;9:175–84. [In Persian] [Google Scholar]
- 15.Kim HS, Oh JA. Adherence to diabetes control recommendations: impact of nurse telephone calls. J Adv Nurse. 2003;44:256–61. doi: 10.1046/j.1365-2648.2003.02800.x. [DOI] [PubMed] [Google Scholar]
- 16.Chiu CW, Wong FK. Effects of 8 week sustained follow up after a nurse consultation on hypervtension: A randomized trial. International Journal of Nursing Studies. 2010;47:1374–82. doi: 10.1016/j.ijnurstu.2010.03.018. [DOI] [PubMed] [Google Scholar]
- 17.Schlachta-Fairchild L, Elfrink V, Deickman A. Patient Safety, Telenursing, and Telehealth. In: Hughes RG, editor. Patient Safety and Quality: An Evidence Based Handbook for Nurses. US: Agency for Healthcare Research and Quality; 2008. [PubMed] [Google Scholar]
- 18.Zakeri Moghadam M, Basampur SH, Rajab A, et al. Effect of telephonefollow-up by a nurse (Telenursing) on dietary adherence in patients with diabetes mellitus type 2. Hayat. 2008;14:63–71. [In Persian] [Google Scholar]
- 19.Sreenivasa Baba C, Alexander G, Kalyani B, et al. Effect of exercise and dietary modification on serum aminotransferase levels in patients with nonalcoholic steatohepatitis. J Gastroenterol Hepatol. 2006;21:191–8. doi: 10.1111/j.1440-1746.2005.04233.x. [DOI] [PubMed] [Google Scholar]
- 20.Promrat K, Kleiner DE, Niemeier HM, et al. Randomized Controlled Trial Testing the Effects of Weight Loss on Nonalcoholic Steatohepatitis. Hepatology. 2010;51:121–9. doi: 10.1002/hep.23276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ueno T, Sugawara H, Sujaku K, et al. Therapeutic effects of restricted diet and exercise in obese patients with fatty liver. J Hepatol. 1997;27:103–7. doi: 10.1016/s0168-8278(97)80287-5. [DOI] [PubMed] [Google Scholar]
- 22.Suzuki A, Lindor K, Saver J, et al. Effect of changes on body weight and lifestyle in nonalcoholic fatty liver disease. J Hepatol. 2005;43:1060–6. doi: 10.1016/j.jhep.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 23.Wang CL, Liang L, Fu JF, et al. Effect of lifestyle intervention on non-alcoholic fatty liver disease in Chinese obese children. World J Gastroenterol. 2008;14:1598–602. doi: 10.3748/wjg.14.1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cinar K, Coban S, Idilman R, et al. Long-term prognosis of nonalcoholic fatty liver disease: Is pharmacological therapy actually necessary? J Gastroenterol Hepatology. 2006;21:169–73. doi: 10.1111/j.1440-1746.2005.04221.x. [DOI] [PubMed] [Google Scholar]
- 25.Okita M, Hayashi M, Sasagawa T, et al. Effect of a Moderately Energy-Restricted Diet on Obese Patients With Fatty Liver. Nutrition. 2001;17:542–7. doi: 10.1016/s0899-9007(01)00543-3. [DOI] [PubMed] [Google Scholar]
- 26.Sadeghian H. Effectivness of home visit program on glyceamic control in children with type 1 diabetes [Thesis] Tehran (Iran): Tarbiat Modares University; 1996. [Google Scholar]
- 27.Ahmadi F. The Design of Continuous Care Model for control of Coronary Artery Disease [Thesis] Tehran (Iran): Tarbiat Modares University; 2000. [Google Scholar]
- 28.Nesari M, Zakeri Moghadam M, Rajab A, et al. Effect of telephone follow-up by nurses on blood glucose and lipid control in patients with type 2 diabetes. Journal of Diabetes and Metabolic Disorders. 2008;8:115–22. [In Persian] [Google Scholar]


