Abstract
The aim of this study is to explore the information needs of men with prostate cancer and their partners retrospectively at various points in the treatment process. An online questionnaire was used to collect information from men with prostate cancer and their partners about information needs, and when these developed. Readers of a Prostate Care Cookbook and members of a Prostate Cancer Charity were invited to participate: 73 men with prostate cancer and 25 partners completed the questionnaire. Responses showed that participants develop their information needs close to diagnosis. Less educated men with prostate cancer and partners developed their needs closer to the time after diagnosis than those with higher education. Partners develop an interest on information related to treatment and interaction earlier than patients. Patients prioritised treatment and disease-specific information. Patients and partners differ in how their information needs develop. Medical information is prioritized by patients as opposed to practical information by partners. Health care provision can be tailored to meet the different needs of prostate cancer patients and their partners at different times in the treatment process.
Key words: Information needs, prostate cancer, partners, family support
Introduction
Information provision is an important component of interventions, aiming to support patients after diagnosis with a serious health condition (Rees, Ford, & Sheard, 2003; Sebregts, Falger, & Bär, 2000). However, in order for information to be useful, there is a need to understand the nature of information that patients and their partners require. Information-seeking behaviour may provide increased certainty in finding meaning to cancer patients’ experiences (Rees et al., 2003). A theoretical framework has been proposed (McCaughan, & McKenna, 2007) which proposes patients pass through several stages on their journey of making sense of their condition: from taking in and experiencing the stressful event of the diagnosis, through taking hold of the experience and engaging in information-seeking behaviour, to taking on where cancer is considered as a life-changing experience. Attempts to take control succeed a period of blocking response after diagnosis and this can be the period when cancer patients develop an information-seeking behavior (Wallace & Storms, 2007).
Recent findings from a 1-year longitudinal study with 34 prostate cancer patients undergoing surgery and their partners show that the need for information is associated with coping with prostate cancer diagnosis after elevated stress as a result of diagnosis (Gray, Fitch, Phillips, Labrecque, & Klotz, 1999). Other research also suggests that the information needs of patients are not satisfied (McPherson, Higginson, & Hearn, 2001; Sinfield, Baker, Agarwal, & Tarrant, 2008). Needs related to support, knowledge of recurrence and side effects of the illness are the most commonly unmet (Boberg et al., 2003). Moreover, the three main interests that cancer patients have after being diagnosed are related to treatment, their body’s response and possible side effects (Lee, Francis, Walker, & Lee, 2004).
Multiple questions about their illness sends patients in search of available information, and the way they process information impacts decisions. A recent study (Noh et al., 2009) explored the means by which cervical cancer patients search for information, suggesting that information acquisition needs are higher closer to the time of diagnosis and when patients’ educational level is higher. On the other hand, there is also evidence that at the time of diagnosis patients are not receptive to information due to anxiety, stress and their inability to think clearly (Friis, Elverdam, & Schmidt, 2003).
Improved treatment and survival means the number of men living with prostate cancer is growing. Significant others play an important role in the men’s coping process and, as a consequence, often experience adverse psychological, physical and social effects (Karademas, & Giannousi, 2013). The interests and concerns of partners are largely similar to those of patients (Lemon, Zapka, & Clemow, 2004), although it has been suggested that the partners of prostate cancer patients are more concerned with treatment-related worry (pain and physical symptoms) whereas patients themselves are more concerned about sexual functioning (Cliff, & MacDonagh, 2000). Some evidence suggests that partners have higher levels of psychological distress than patients (Couper et al., 2006; Kornblith, Herr, Ofman, Scher, & Holland, 1994), though other research does not confirm this (Baider, Ever-Hadani, Goldzweig, Wygoda, & Peretz, 2003).
This cross-sectional descriptive study explore prostate cancer patients’ retrospective patterns of information seeking post diagnosis. Its specific aims are to: i) explore the relationship between participants’ educational level and expressed need for information, and ii) compare the information needs of prostate cancer patients with that of partners of prostate cancer patients. No hypotheses were made as this is a hypothesis generating study and findings can inform the design of a future longitudinal study rather than reporting causal relationships.
Materials and Methods
Research design
An exploratory cross-sectional research design was used. The study received a favourable ethical opinion from the University of Surrey Ethics Committee. Participants completed an online questionnaire through which they were screened to ensure they met the inclusion criteria: i) to have been diagnosed with prostate cancer or to have been a partner of a person diagnosed with prostate cancer, and ii) to be able to complete the online questionnaire. Participants were recruited in the UK through an invitation placed in the Prostate Care Cook Book (Rayman, Gibbons, & Dilley, 2009) and a link to the questionnaire on the Prostate Cancer Charity’s website and monthly bulletin Voices.
Measures
Demographic and medical information
All participants were asked to provide details on their age, gender, marital status, level of education and employment status (see Table 1 for details of the scales used). Prostate cancer patients were also asked to provide information on their treatment status and time since diagnosis information.
Table 1.
Typology of information needs used in the study.
| Information need | Type of information | Comments |
|---|---|---|
| Available treatments/options | Treatment-related | Item’s name same with source |
| More information about prostate cancer | Cancer-specific | Item’s name not in the source as a separate need but used a name that captures the type of information |
| Likely progress of disease | Prognosis | Item’s name not in the source as a separate need but used a name that captures the type of information |
| Self-care issues or home care during recovery | Rehabilitation | Item’s name same with source |
| Effect on family, friends or caregivers | Interpersonal/social | Item’s name same with source |
| Emotional reactions, emotional support, coping with cancer | Coping | Item’s name same with source |
| Interaction issues with health care providers | Medical system | Item’s name same with source |
| Sexuality | Body image/sexuality | Item’s name same with source |
| Cost of treatment, insurance coverage, or other financial issues | Financial/legal | Item’s name same with source |
| Maintaining psychological health | Surveillance and health | Item’s name same with source |
| Diet and nutrition | None | New item |
All information needs were included in Rutten et al.’s (2005) review except “Diet and nutrition”.
Information needs
The items related to information needs were derived from those identified in a systematic review (Rutten, Arora, Bakos, Aziz, & Rowland, 2005), which identified a typology of cancer patients’ information needs. More specifically the review identified ten types of information needs identified in the literature from which we used one item for each type or created a new item based on the type of information (Table 1). One extra item was added: diet and nutrition in order to account for information which we perceive as underrepresented in health care information provision, thus resulting in eleven items. For each of the eleven needs, participants were asked To what extent were you interested in getting information in relation to the following after being diagnosed and the partners were asked …after the person you are significantly linked with was diagnosed on a 5-point Likert Scale ranging from not interested at all to extremely interested.
Time of information need development
Participants were asked to respond on how soon after diagnosis (or after their partner was diagnosed) they developed an interest in each of the eleven items. Possible responses were immediately, less than 1 month, 1-3 months, 4-6 months and more than 6 months.
Data analysis
Descriptive statistics and percentages were used to see when patients developed their information needs based on the 5 points of the Likert Scale (immediately, less than 1 month, 1-3 months, 4-6 months and more than 6 months). Normality of distribution was not confirmed for all variables therefore non-parametric tests were used. To investigate the role of educational level on information needs at various points in the treatment process, and compare the needs of patients and significant others, a series of Jonckheere’s tests was used: i) one for comparing between different levels of education and iii) one for comparing between patients and significant others. Three education categories were combined: no formal education, less than primary and primary education completed. Mann-Whitney tests were used to follow up these findings. A Bonferroni correction was applied so all effects are reported at P=0.016 level of significance. Mean Ranks of the participants’ responses are reported with a higher mean rank indicating higher agreement with the need for obtaining an information need and longer time of development since diagnosis in the case of the time of information need development questions.
Results
Participants
In total 98 people participated in the study, 73 of which were diagnosed with prostate cancer and 25 were a partner to someone diagnosed with prostate cancer (not the patients participating in this study). The participants’ ages ranged from 23 to 81 for those diagnosed with prostate cancer and 23 to 70 for the partners (Table 2).
Table 2.
Characteristics of respondents (N=98).
| Prostate cancer patients | Partners | |||||||
|---|---|---|---|---|---|---|---|---|
| N | % | M | SE | N | % | M | SE | |
| Age | 73 | 50.9 | 2 | 25 | 47.2 | 3.2 | ||
| Age of diagnosis | 73 | 58.3 | 2.5 | |||||
| Gender | ||||||||
| Male | 73 | 100 | ||||||
| Female | 0 | 0 | 25 | 100 | ||||
| Relationship with patient | ||||||||
| Member of family | 14 | 56 | ||||||
| Relative | 2 | 8 | ||||||
| Friend | 5 | 20 | ||||||
| Other | 4 | 16 | ||||||
| Marital status | ||||||||
| Married/living as married | 54 | 74 | 16 | 64 | ||||
| Living with another adult(s) | 10 | 13.7 | 7 | 28 | ||||
| Single/living alone | 9 | 12.3 | 2 | 8 | ||||
| Education | ||||||||
| No formal education | 14 | 19.2 | 11 | 44 | ||||
| Less than primary school | 3 | 4.1 | 1 | 4 | ||||
| Primary school completed | 3 | 4.1 | 0 | 0 | ||||
| Secondary school/job-related qualifications | 14 | 19.2 | 3 | 12 | ||||
| Tertiary education | 26 | 35.6 | 6 | 24 | ||||
| Postgraduate degree | 13 | 17.8 | 4 | 16 | ||||
| Employment status | ||||||||
| Full-time paid work | 45 | 61.6 | 12 | 48 | ||||
| Part-time paid work | 7 | 9.5 | 4 | 16 | ||||
| Retired/not working | 21 | 18.9 | 9 | 36 | ||||
| Treatment status | ||||||||
| Under treatment | 21 | 60 | ||||||
| In complete remission | 3 | 8.6 | ||||||
| Recurrent | 6 | 17.1 | ||||||
| Not reported | 5 | 14.3 | ||||||
| Treatment type | ||||||||
| Surgery | 14 | 19.2 | ||||||
| Radiation therapy | 16 | 21.9 | ||||||
| Chemotherapy | 1 | 1.4 | ||||||
| Other/unspecified | 42 | 57.5 | ||||||
The majority of the respondents were married or living as married (n=87) while fewer were single/living alone (n=11). Regarding the participants’ educational level, most had received education from secondary school or gained a job-related qualification and higher (n=59) and fewer had only a primary education or no schooling (n=39).
Participants accessing the online questionnaire through the Prostate Cancer Charity reported having completed significantly more education than participants accessing the online questionnaire through the Prostate Care Cook Book χ2 (1, =98)=4.58, P<0.05. No significant differences were found between the two recruitment sources and marital status, χ2 (1, N=98)=1.19, P>0.05, nor their age, t (98)=0.95, P=0.34.
The time of developing information needs
In general, men developed their information needs closer after diagnosis than later, with 56.8% developing their information needs immediately and 15.8% during the first month after diagnosis as opposed to 3.8% and 6.8% who developed their needs during the first to third month and fourth to sixth month after diagnosis respectively. When it comes to significant others a higher proportion (73%) developed their information needs immediately and a lower proportion developed their needs later (Figure 1).
Figure 1.
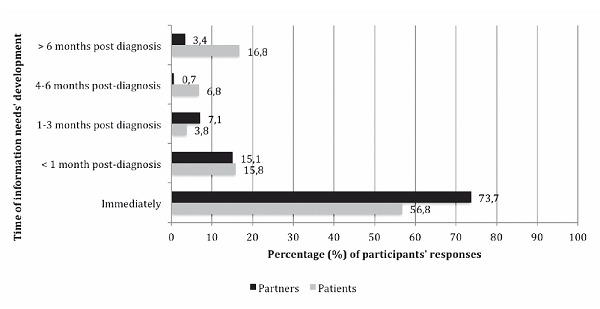
The patient and partners’ time of information needs’ development.
The role of educational level on information needs
Comparing the need for information by educational level
Both patient and partners’ responses were used for these analyses. In general, the Jonckheere’s tests showed that the less educated participants were less in need of all the types of information after their diagnosis or the diagnosis of their partner. Mann-Whitney post-hoc tests confirmed these findings with participants with education ranging from no education to primary school being less in need of information than the other 3 groups (Table 3). The effect size was large for all information needs. Higher educated patients were more in need of information on sexuality while less educated significant others were more in need of information on the cost of treatment, insurance coverage and other financial issues.
Table 3.
Differences between different levels of education and time of information needs’ development (N=98).
| Information need | No education-primary (n=32) | Secondary (n= 17) | U | r | No education-primary (n=32) | Tertiary (n=32) | U | r | No education-primary (n=32) | Post-graduate (n= 7) | U | r |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Available treatments/options | 24.5 | 25.9 | 256 | 0.07 | 29.2 | 33.8 | 407 | 0.18 | 21.9 | 30.9 | 171* | -0.4 |
| More information about prostate cancer | 24.6 | 25.8 | 259 | 0.05 | 30.5 | 32.5 | 449 | 0.07 | 21.6 | 31.5 | 162* | -0.4 |
| Likely progress of disease | 24.6 | 25.9 | 257.5 | 0.06 | 28.8 | 34.4 | 394 | 0.19 | 21.8 | 31.1 | 168* | -0.38 |
| Self-care issues or home care during recovery | 23 | 28.8 | 207 | 0.25 | 24.4 | 39.1 | 253** | 0.45 | 18.9 | 36.4 | 78** | -0.66 |
| Effect on family, friends or caregivers | 23.5 | 27.8 | 224 | 0.19 | 25.6 | 37.7 | 293* | 0.39 | 19.9 | 34.6 | 109** | -0.56 |
| Emotional reactions, emotional support, coping with cancer | 22.9 | 28.9 | 205.5 | 0.26 | 26.3 | 37 | 314* | 0.35 | 19.3 | 35.8 | 88** | -0.64 |
| Interaction issues with health care providers | 22.9 | 28.9 | 206 | 0.25 | 25.5 | 37.9 | 288* | 0.39 | 18.9 | 36.4 | 78** | -0.66 |
| Sexuality | 23.9 | 27.1 | 236 | 0.15 | 23.9 | 39.6 | 236** | 0.49 | 20.4 | 33.6 | 126** | -0.52 |
| Cost of treatment, insurance coverage, or other financial issues | 21.7 | 31.2 | 166* | 0.42 | 23.1 | 40.5 | 210** | 0.55 | 17.9 | 38.3 | 46** | -0.78 |
| Maintaining psychological health | 23.4 | 28 | 221 | 0.2 | 36.8 | 36.8 | 322* | 0.33 | 19.8 | 34.9 | 104** | -0.58 |
| Diet and nutrition | 22.6 | 29.6 | 194 | 0.31 | 26.9 | 36.5 | 331* | 0.33 | 19.1 | 36.2 | 81** | -0.66 |
*P<0.01
**P<0.001. Mann-Whitney U Test, Mean Ranks are reported: the highest the Mean Rank the later the participant indicates to the 5-point Likert Scale that they developed a need for the information.
Comparing the information needs at various time points by educational level
Results revealed that the educational level of the participants was significantly associated with the time of information need development regarding all types of information needs. Jonckheere’s tests for all types of information needs revealed that the less educated participants were, the more they were in need of information closer to diagnosis. Post-hoc tests confirmed these findings (Table 4). The effect of education was higher when the difference on the level of education was larger. For example, participants with education ranging from no education to primary school significantly differed from participants with a secondary education only as regards information on cost of treatment, insurance coverage and other financial issues (U=166, r=-0.42) but with participants with no formal to primary education significantly more in need of all types of information closer to diagnosis than patients with postgraduate education. Also, between no education to primary school and secondary education three types of information had a higher effect size and significance level than others: self-care issues or home care during recovery (U=253, r=45), sexuality (U=36, r=0.49) and cost of treatment, insurance coverage and other financial issues (U=210, r=0.55).
Table 4.
Differences between patients and partners on time of information needs’ development (N=98).
| Information need | Patients (n=73) | Partners (n=25) | U | r |
|---|---|---|---|---|
| Available treatments/options | 50.7 | 42.1 | 729 | -0.15* |
| More information about prostate cancer | 50.7 | 42.4 | 734.5 | -0.18* |
| Likely progress of disease | 50.2 | 43.6 | 764.5 | -0.16 |
| Self-care issues or home care during recovery | 51.4 | 40.3 | 681.5 | -0.12* |
| Effect on family, friends or caregivers | 50.7 | 42.3 | 731.5 | -0.19 |
| Emotional reactions, emotional support, coping with cancer | 49.9 | 44.4 | 785.5 | -0.14 |
| Interaction issues with health care providers | 53 | 35.9 | 571.5 | -0.09** |
| Sexuality | 49.3 | 46.3 | 833 | -0.29 |
| Cost of treatment, insurance coverage, or other financial issues | 50 | 44.3 | 782.5 | -0.05 |
| Maintaining psychological health | 51 | 41.4 | 709 | -0.15* |
| Diet and nutrition | 50.7 | 42.3 | 731.5 | -0.09 |
*P<0.05
** P<0.01. Mann-Whitney U Test, Mean Ranks are reported; the highest the Mean Rank the later the participant indicates to the 5-point Likert Scale that they developed a need for the information.
Comparing the information needs of patients and partners
Patients and partners did not significantly differ on the type of information need they developed. However, partners were found to develop the need for particular types of information earlier than patients, namely for available treatments/treatment options (U=729, r=-0.15), more information about prostate cancer (U=734.5, r=-0.18), self-care issues or home care during recovery (U=681.5, r=-0.12), interaction issues with health care providers (U=571.5, r=-0.09) and maintaining psychological health (U=709, r=-0.15). All of the effect sizes were small.
Discussion
In general, less educated patients and less educated partners were less in need of information after diagnosis but developed their needs closer to diagnosis compared to higher educated patients and partners who developed their information needs later. Among participants in this study the types of information needs that partners develop earlier than patients are available treatments/treatment options, more information about prostate cancer, self-care issues, interaction issues with health care providers and maintaining psychological health.
Based on the percentages of participants’ self-reports in this study, it is not clear why patients’ interest in having information increased following the 3rd month after diagnosis (Figure 1). However, these results provide an indication of the trajectory of interest in information, which could be, explored further using a longitudinal research design. It may be that once the blocking response period is over (McCaughan, & McKenna, 2007), patients seem to want to receive information. It may also be that stress levels are lower after the third month so more patients are in need of information. The study’s findings are contrary to some other studies (Friis, Elverdam, & Schmidt, 2003; McCaughan, & McKenna, 2007; Salminen, Bishop, Poussa, Drummond, & Salminen, 2004), which suggested that patients’ interest in acquiring information about cancer linearly increases from the time of diagnosis. However, the measures used in this study are more nuanced than previous ones. There is a point after cancer diagnosis where the teachable moment is lost (Stead, Caswell, Craigie, Eadie, & Anderson, 2012). Other studies have explained a period of blocking information suggesting that the shock from a cancer diagnosis can be associated with information avoidance (McCaffery et al., 2001; Miles, Voorwinden, Chapman, & Wardle, 2008). Moreover patients may at that time have experienced and evaluated the symptoms and consequences of cancer during the first months and will then seek information for coping purposes.
Previous findings (Hathaway, 1986; Hervouet et al., 2005; Lee-Jones, Humphris, Dixon & Bebbington Hatcher, 1997; Sanson-Fisher et al., 2000; Steginga, Occhipinti, Mccaffrey & Dunn, 2001; Suls & Wan, 1989) provide indications on the development of information needs in the trajectory of cancer. Before treatment and after diagnosis, patients were found to need treatment-related information (Hathaway, 1986; Suls & Wan, 1989). While during and immediately after treatment, they need side-effects-related information (Hervouet et al., 2005; Sanson-Fisher et al., 2000), emotional health-related and interaction-related information at the same time they are focusing on coping with new roles (Steginga et al., 2001). After treatment they need relapse-related information (Lee-Jones et al., 1997).
Previous studies have shown that cancer patients have a range of unmet needs post-diagnosis, which can explain the great need for information in the immediate period post-diagnosis found in this study (Boberg et al., 2003; McPherson et al., 2001; Sanson-Fisher et al., 2000; Steginga et al., 2001). Their coping process can also be associated with reassurance seeking, which has been found to cause health anxiety (Stark et al., 2004) and is developed gradually after diagnosis where the patient seeks medical consultations, asks friends and family about symptoms and reads about the illness.
This study confirmed the findings of other studies that also showed a desire for information to increase together with patients’ educational level (Noh et al., 2009; Salminen et al., 2004). Information needs like treatment-related information, likely progress of the disease and available treatments and options were not as significantly different between education groups as other types of information. This information is seen as vital because they may be conceptualized as life and death issues, which are crucial for coping with cancer. On the other hand practical information like self-care issues are considered more important and are developed much earlier for less educated patients and partners. Furthermore, the more educated patients usually have the resources to seek information from various sources and to gain second opinions from health-care professionals.
The interest of partners in obtaining information on decision-making and problem-solving activities related to the cancer is higher than that of patients (Lavery, & Clarke, 1999) and so are more in need for information immediately after diagnosis compared to the later. In this study, although partners did not differ in how much they were interested in information, they were more in need of acquiring information about treatment and interaction issues earlier than the patients. This can be interpreted in the context of the partner’s role. While a patient can be in denial or experience the shock of diagnosis, the significant other can strive for information in order to support the patient and prompting them to understand the disease so as to they can be part of the patients’ coping process.
Furthermore, the differences between patients and partners on specific needs can be seen in the context of the partner’s needs. Partners have been shown to experience higher levels of stress (Murray et al., 2010; Persson & Sundin, 2008) and lower levels of quality of life compared to patients. They are found to develop a need earlier for information early on that will provide them with reassurance and practical information (treatment-related) to help them deal with the changes to their lives. Findings are also supporting a systematic review (Adams, Boulton & Watson, 2009) which found partners and significant others of cancer patients to have unmet needs related to supportive care rather than medical information.
There are other issues to consider. The study’s research design limits the accuracy of its findings because a retrospective self-report is used and the period after diagnosis is not examined in a longitudinal design. However, this study’s purpose is not to draw cause-effect relationships but rather to explore the needs of patients and partners providing evidence for designing further longitudinal research. Perceptions, behaviours and needs when assessed using self-report measures are prone to self-report bias. The participants’ age at diagnosis and the time since diagnosis differed so the coping stage they were at the time of recruitment was not homogeneous. Also, the participants’ varying cultural backgrounds may have affected the study’s results. Finally one issue to consider is whether participants in this study are representative of the general prostate cancer population since they were readers of a cookbook, sufficiently interested to respond and have access to the web. However, assuming generalizability of findings is not the purpose of this study but rather to explore relationships to inform suture research and generate hypotheses.
Conclusions
Expanding upon previous work, we can argue that there is an indication that the closer the time to diagnosis, the greater the need for prostate cancer-related information. Finally patients may be more in need for treatment and medical information and there are increased reports of need for information after the third month post-diagnosis whereas partners are more in need for practical information and earlier. These findings require further investigation.
The findings are indicative of further researching the trajectory of patient and partners’ information needs. It is similar to the importance of establishing the patients’ stage of change (Palmeira et al., 2007; Prochaska & Velicer, 1997) to enable healthcare professionals to implement stage-specific interventions. Identifying the most opportune time to provide advice after cancer diagnosis is essential (Pinto & Trunzo, 2005). Findings from this study add to the understanding of the stages through which patients pass after diagnosis. Also, identifying patients’ information needs can benefit treatment-related choices. Finally, family interventions can benefit both patients and their partners whereas partners seem to constitute a well-defined population for healthcare providers to focus on delivering appropriate family and systemic therapies as well as psycho-education, which may benefit patients and their families.
Future research needs to follow the journey of patients and partners after diagnosis, taking into account the different stages of coping with prostate cancer diagnosis and the psychological processes which diagnosis triggers. Educational interventions may be effective if they take into account the point after which a patient is discharged from cancer follow-up back to their health professional. The perception of healthcare providers can also be compared with patients’ actual information needs.
Acknowledgements
We would like to thank the following for their contribution in this study: Prof. Chris Fife-Schaw for his comments on the manuscript and Prof. Margaret Rayman, the Prostate Cancer Charity and the Prostate Cancer Support Federation for their support in recruiting participants.
References
- Adams E., Boulton M., Watson E. (2009). The information needs of partners and family members of cancer patients: a systematic literature review. Patient Education and Counseling, 77, 179-186. [DOI] [PubMed] [Google Scholar]
- Baider L., Ever-Hadani P., Goldzweig G., Wygoda M.R., Peretz T. (2003). Is perceived family support a relevant variable in psychological distress?: A sample of prostate and breast cancer couples. Journal of Psychosomatic Research, 55, 453-460. [DOI] [PubMed] [Google Scholar]
- Boberg E.W., Gustafson D.H., Hawkins R.P., Offord K.P., Koch C., Wen K.Y., …, Salner A. (2003). Assessing the unmet information, support and care delivery needs of men with prostate cancer. Patient Education and Counseling, 49, 233-242. [DOI] [PubMed] [Google Scholar]
- Cliff A.M., MacDonagh R.P. (2000). Psychosocial morbidity in prostate cancer: II. A comparison of patients and partners. BJU International, 86, 834-839. [DOI] [PubMed] [Google Scholar]
- Couper J., Bloch S., Love A., Macvean M., Duchesne G.M., Kissane D. (2006). Psychosocial adjustment of female partners of men with prostate cancer: a review of the literature. Psychooncology, 15, 937-953. [DOI] [PubMed] [Google Scholar]
- Friis L.S., Elverdam B., Schmidt K.G. (2003). The patient’s perspective. Supportive Care in Cancer, 11, 162-170. [DOI] [PubMed] [Google Scholar]
- Gray R.E., Fitch M.I., Phillips C., Labrecque M., Klotz L. (1999). Presurgery experiences of prostate cancer patients and their spouses. Cancer Practice, 7, 130-135. [DOI] [PubMed] [Google Scholar]
- Hathaway D. (1986). Effect of preoperative instruction on postoperative outcomes: a meta-analysis. Nursing Research, 35, 269-275. [PubMed] [Google Scholar]
- Hervouet S., Savard J., Simard S., Ivers H., Laverdière J., Vigneault E., …, Lacombe L. (2005). Psychological functioning associated with prostate cancer: cross-sectional comparison of patients treated with radiotherapy, brachytherapy, or surgery. Journal of Pain and Symptom Management, 30, 474-484. [DOI] [PubMed] [Google Scholar]
- Karademas E.C., Giannousi Z. (2013). Representations of control and psychological symptoms in couples dealing with cancer: a dyadic-regulation approach. Psychology & Health, 28, 67-83. [DOI] [PubMed] [Google Scholar]
- Kornblith A.B., Herr H.W., Ofman U.S., Scher H.I., Holland J.C. (1994). Quality of life of patients with prostate cancer and their spouses. The value of a data base in clinical care. Cancer, 73, 2791-2802. [DOI] [PubMed] [Google Scholar]
- Lavery J.F., Clarke V.A. (1999). Prostate cancer: Patients’ and spouses’ coping and marital adjustment. Psychology, Health & Medicine, 4, 289-302. [Google Scholar]
- Lee Y.M., Francis K., Walker J., Lee S.M. (2004). What are the information needs of Chinese breast cancer patients receiving chemotherapy? European Journal of Oncology Nursing, 8, 224-233. [DOI] [PubMed] [Google Scholar]
- Lee-Jones C., Humphris G., Dixon R., Bebbington Hatcher M. (1997). Fear of cancer recurrence: a literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psychooncology, 6, 95-105. [DOI] [PubMed] [Google Scholar]
- Lemon S.C., Zapka J.G., Clemow L. (2004) Health behavior change among women with recent familial diagnosis of breast cancer. Preventive Medicine, 39, 253-262. [DOI] [PubMed] [Google Scholar]
- McCaffery K., Borril J., Williamson S., Taylor T., Sutton S., Atkin W., Wardle J. (2001). Declining the offer of flexible sigmoidoscopy screening for bowel cancer: a qualitative investigation of the decision-making process. Social Science & Medicine, 53, 679-691. [DOI] [PubMed] [Google Scholar]
- McCaughan E., McKenna H. (2007). Never-ending making sense: towards a substantive theory of the information-seeking behaviour of newly diagnosed cancer patients. Journal of Clinical Nursing, 16, 2096-2104. [DOI] [PubMed] [Google Scholar]
- McPherson C.J., Higginson I.J., Hearn J. (2001). Effective methods of giving information in cancer: a systematic literature review of randomized controlled trials. Journal of Public Health, 23, 227-234. [DOI] [PubMed] [Google Scholar]
- Miles A., Voorwinden S., Chapman S., Wardle J. (2008). Psychologic predictors of cancer information avoidance among older adults: the role of cancer fear and fatalism. Cancer Epidemiology, Biomarkers & Prevention, 17, 1872-1879. [DOI] [PubMed] [Google Scholar]
- Murray E., Treweek S., Pope C., MacFarlane A., Ballini L., Dowrick C., …, May C. (2010). Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Medicine, 8, 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noh H.I., Lee J.M., Yun Y.H., Park S.Y., Bae D.S., Nam J.H., Park C.T., …, Chang Y.J. (2009). Cervical cancer patient information-seeking behaviors, information needs, and information sources in South Korea. Supportive Care in Cancer, 17, 1277-1283. [DOI] [PubMed] [Google Scholar]
- Palmeira A.L., Teixeira P.J., Branco T.L., Martins S.S., Minderico C.S., Barata J.T., Serpa S.O., Sardinha L.B. (2007). Predicting short-term weight loss using four leading health behavior change theories. International Journal of Behavioral Nutrition and Physical Activity, 4, 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persson C., Sundin K. (2008). Being in the situation of a significant other to a person with inoperable lung cancer. Cancer Nursing, 31, 380-388. [DOI] [PubMed] [Google Scholar]
- Pinto B.M., Trunzo J.J. (2005). Health behaviors during and after a cancer diagnosis. Cancer, 104, 2614-2623. [DOI] [PubMed] [Google Scholar]
- Prochaska J.O., Velicer W.F. (1997). The transtheoretical model of 25 health behavior change. American Journal of Health Promotion, 12, 38-48. [DOI] [PubMed] [Google Scholar]
- Rayman M., Gibbons K., Dilley K. (2009). The Prostate Care Cook Book. Prostate Cancer Research Foundation. [Google Scholar]
- Rees C.E., Ford J.E., Sheard C.E. (2003). Patient information leaflets for prostate cancer: which leaflets should healthcare professionals recommend? Patient Education Counseling, 49, 263-272. [DOI] [PubMed] [Google Scholar]
- Rutten L.J.F., Arora N.K., Bakos A.D., Aziz N., Rowland J. (2005). Information needs and sources of information among cancer patients: a systematic review of research (1980–2003). Patient Education and Counseling, 57, 250-261. [DOI] [PubMed] [Google Scholar]
- Salminen E., Bishop M., Poussa T., Drummond R., Salminen S. (2004). Dietary attitudes and changes as well as use of supplements and complementary therapies by Australian and Finnish women following the diagnosis of breast cancer. European Journal of Clinical Nutrition, 58, 137-144. [DOI] [PubMed] [Google Scholar]
- Sanson-Fisher R., Girgis A., Boyes A., Bonevski B., Burton L., Cook P. (2000). The unmet supportive care needs of patients with cancer. Cancer, 88, 226-237. [DOI] [PubMed] [Google Scholar]
- Sebregts E.H., Falger P.R., Bär F.W. (2000). Risk factor modification through nonpharmacological interventions in patients with coronary heart disease. Journal of Psychosomatic Research, 48, 425-441. [DOI] [PubMed] [Google Scholar]
- Sinfield P., Baker R., Agarwal S., Tarrant C. (2008). Patient-centred care: what are the experiences of prostate cancer patients and their partners? Patient Education and Counseling, 73, 91-96. [DOI] [PubMed] [Google Scholar]
- Stark D., Kiely M., Smith A., Morley S., Selby P., House A. (2004). Reassurance and the anxious cancer patient. British Journal of Cancer, 91, 893-899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stead M., Caswell S., Craigie A.M., Eadie D., Anderson A.S. (2012). Understanding the potential and challenges of adenoma treatment as a prevention opportunity: insights from the BeWEL formative study. Preventive Medicine, 54, 97-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steginga S.K., Occhipinti S., Mccaffrey J., Dunn J. (2001). Men’s attitudes toward prostate cancer and seeking prostate-specific antigen testing. Journal of Cancer Education, 16, 42-45. [DOI] [PubMed] [Google Scholar]
- Suls J., Wan C.K. (1989). Effects of sensory and procedural information on coping with stressful medical procedures and pain: a meta-analysis. Journal of Consulting and Clinical Psychology, 57, 372. [DOI] [PubMed] [Google Scholar]
- Wallace M., Storms S. (2007). The needs of men with prostate cancer: results of a focus group study. Applied Nursing Research, 20, 181-187. [DOI] [PubMed] [Google Scholar]


