Abstract
Health literacy is the first step to self-management of type II diabetes mellitus, of which physical activity is the least compliant behavior. However, no reviews have summarized the effect and the process of interventions of health literacy oriented programs on physical activity behavior among middle aged and older adults with type II diabetes mellitus. This article is the first to examine the effectiveness of health literacy oriented programs on physical activity behavior among middle aged and older adults with type II diabetes mellitus. This systematic review extracted articles from nine electronic databases between 1990 and 2013. Six interventional studies were extracted and reported in accordance with the guidance of Preferred Reporting Items for Systematic Reviews and Meta-Analyses. Findings demonstrated that health literacy oriented programs increased the frequency and duration of physical activity among patients with high health literacy. Although some studies effectively improved the health literacy of physical activity, gap in literature remains open for the indistinct and unreliable measurement of physical activity within self-management programs of type II diabetes mellitus, and the questionable cross-culture generalizability of findings. Further studies with well-knit theory-based intervention with respect to patients’ cultural background, duration of intervention and objective measurements are encouraged to elucidate the relationship between health literacy oriented programs and physical activity behavior.
Key words: Health literacy, older adult, physical activity, systematic review, type II diabetes mellitus
Introduction
The concept of health literacy (HL) emerged in early 1990s but only recently did it receive focal attention when the Office of Surgeon General of United States Department of Health and Human Services (USDHHS) considered HL as one of the four public health priorities (Cutilli, 2007; Galson, 2008). HL is the ability to obtain, understand and communicate basic information needed to make appropriate health-related decisions (Institute of Medicine, 2004). With regards to implementing self-management to one’s illness in the 21st century, the skills covered by HL such as acquiring, interpreting, analyzing and communicating relevant health information with others are essential to achieving positive outcomes (Edwards, Hill & Edwards, 2009). Chinese older adults also consider obtaining and applying of health information for health decision-making, i.e. HL, as the most important factor among their health needs. They believe that getting adequate health information could help them know about their roles and methods to cope with personal and environmental problems. Hence, HL training should, in theory, improve the wellbeing of individuals with chronic conditions (Shih, Gau, Kao, & Shih, 2005). Diabetes mellitus (DM) is a chronic disease, which causes elevated blood glucose level due to inadequate insulin production or action. DM was ranked as one of the top ten fatal diseases in middle and high-income countries and the mortality prevalence will be doubled by 2030 (World Health Organization, 2010). It can lead to serious complications such as heart problems, kidney problems, stroke, hypertension, amputations and sexual dysfunction (Mancuso, 2010; Tang, Pang, & Chan, 2008). Type II diabetes mellitus (T2DM) embraces more than 90% of the total DM cases (Colberg et al., 2010). This subtype of the disease is more common in middle aged (aged 45 or above) and older adults, thus also known as adult-onset and non-insulin-dependent diabetes. As T2DM has no cure, extensive self-management behaviors such as controlling diet, physical activity (PA), medical adherence, and self-glucose monitoring should be persistently encouraged (Mancuso, 2010), so that the glycated hemoglobin (HbA1c) level can be controlled effectively (Cutilli, 2007). Among the self-management behaviors of T2DM, PA was found the least compliant (Chan & Molassiotis, 1999; Shigaki et al., 2010). PA reduces the risk of T2DM (Galson, 2011). However, literature that concerns PA independently from other self-management behaviors among diabetic patients was extremely limited before the 2000s (Sigal, Kenny, Wsserman, & Castaneda-Sceppa, 2004). PA encompasses any bodily movement produced by the contraction of skeletal muscle that increases energy expenditure above a basal level (Chao, Foy, & Farmer, 2000). Unlike complying with diet and medication recommendations, PA requires commitment and causes sweating, discomfort even pain at times. In addition, the delay in health effects of PA could have stimulated individuals to withdraw from PA, leading to sedentary lifestyle in older adults (Chao, Foy, & Farmer, 2000; Jeon, Lokken, Hu, & van Dam, 2007).
Several researchers investigated how to encourage PA behavior in T2DM patients. Some strategies such as direct PA training, goal setting, decision making and social support were examined but efficacy was minor (Cardona-Morrell et al., 2010; Conn et al., 2003; Hudon, Fortin, & Soubhi, 2008; Jeon, Lokken, Hu, & van Dam, 2007; Shigaki et al., 2010).
Limited HL could be the cause of poor PA in T2DM patients. In fact, it was associated with the rate of diabetes complications while improving HL has been shown to improve glycemic control (Schillinger et al., 2002). Some researchers suggested that limited HL would lay the first stone for poor self-management behaviors and eventually poor health outcomes (Gazmararian, Williams, Peel, & Baker, 2003; Osborn, Paasche-Orlow, Bailey, & Wolf, 2011; Paasche-Orlow & Wolf, 2007).
In a few words, HL is an important ability to self-management behaviour in T2DM patients. PA has been found to improve health outcomes of T2DM. However, the older age groups are less active. Therefore health literacy oriented programs and PA are key factors to self management behavior of the middle aged and older adults with T2DM indirectly. Despite of that, no reviews have summarized the effect of health literacy oriented programs on PA behavior in middle aged and older adults with T2DM. Therefore, a comprehensive systematic review is needed to consolidate findings on the relationship between HL and PA behavior.
Aims
This article attempts to review current literature to examine the effectiveness of health literacy oriented programs on PA behavior in middle aged and older adults with T2DM.
Materials and Methods
Design
Only interventional articles were included in this review. The articles were screened and reported in accordance with the guidance of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Moher et al., 2010). The searching process took place in August 2012 and updated in May 2013.
Search methods
Articles were identified from nine electronic databases from January 1990 to April 2013: Medline, PubMed, CINAHL, PsycINFO, Proquest, SportDISCUS, ISI Web of Science and ERIC. The key searching terms were generated from three systematic reviews about HL, PA, older adults with T2DM (Conn et al., 2003; Cutilli, 2007; Hamel, Robbins, & Wilbur, 2011). The search terms included health literacy, literacy, numeracy, reading ability, rapid estimate of adult literacy in medicine, test of functional health literacy in adults, wide range achievement test, diabetes numeracy test, type II diabetes mellitus, type 2 diabetes mellitus, glycemic control, T2DM, older adult, older people, senior, elderly, elder, geriatric, aged, middle aged, physical activity, exercise, physical exercise, Tai Chi, walking, brisk walking, strength training, aerobic training, aerobic exercise, running, aquatic exercise, self-management, self-care, compliance and the scale of summary of diabetes self-care activities. Hand searching was performed on the reference lists of all the articles identified. To ensure a comprehensive search of international articles, the assistance of librarian from the University of Hong Kong was obtained. Table 1 lists the inclusion and exclusion criteria for selecting articles for review.
Table 1.
Inclusion and exclusion criteria for screening.
| Inclusion criteria | Exclusion criteria |
|---|---|
| i) Articles with middle aged (mean age 45-64) or older (age >65) adults; ii) articles written or translated in English; iii) articles with at least 10 participants; iv) articles related to health literacy and physical activity; v) participants included in the articles were patients with type II diabetes mellitus; vi) year of publication between 1990 and 2013 |
i) Publication based on authors’ opinion only; ii) articles did not include physical activity as a factor of self-management behaviors. |
Search outcomes
According to the PRISMA 2010 flow diagram of screening process (Moher et al., 2010), there were 366 references located; 22 duplicated, 25 non-full text articles excluded and 313 articles did not meet the inclusion criteria. Six articles were included in the qualitative synthesis. Figure 1 illustrates the screening process.
Figure 1.
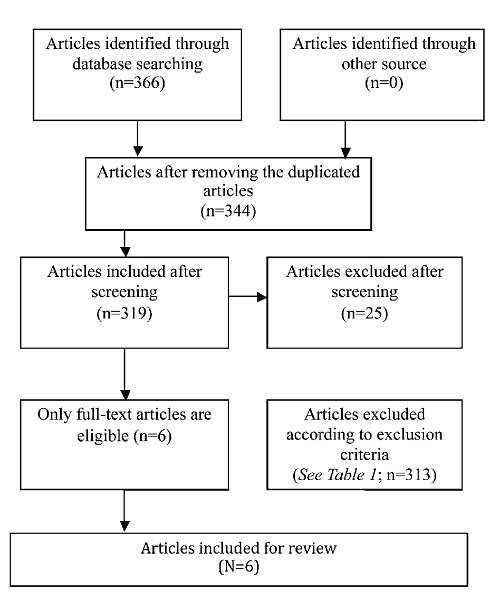
Study flow from identification to final included articles.
Quality appraisal
The authors appraised the articles according to the developed interventional review guideline developed by Schulz et al. (1995), Jadad et al. (1996), and subsequently modified by DeWalt and Hink (2009). We evaluated study design quality according to i) adequacy of study population, ii) adequacy of randomization procedure, iii) describe the withdrawals and dropouts, iv) intention to treat, v) outcome assessors blind to the intervention, vi) comparability of subjects across comparison groups, vii) validity and reliability of the literacy measurement, viii) maintenance of comparable groups, ix) appropriateness of the outcome measurement, x) appropriateness of statistical analysis and xi) adequacy of control of confounding. A score (0=poor; 1=fair; 2=good) was given to each items and we excluded the items which were not applicable to the study designs. The average score of these items on equal weighting base will be the final quality and strength grades (<1=poor; 1 to <1.5 =fair; 1.5 and >1.5 =good) (Berkman et al., 2004). Table 2 summarises the appraisal table of quality and strength of evidence from the reviewed articles. No articles were excluded based on this quality appraisal.
Table 2.
A summary of the quality and strength of evidence in reviewed studies.
| Description | Rosal et al. (2011) | Cavanaugh et al. (2009) | DeWalt et al. (2009) | Gerber et al. (2005) | Kim et al. (2004) | Rosal et al. (2005) |
|---|---|---|---|---|---|---|
| Adequacy of study population | 2 | 2 | 2 | 2 | 2 | 0 |
| Adequacy of randomization procedure | 2 | 2 | 0 | 2 | 0 | 1 |
| Describe the withdrawals and dropouts | 1 | 2 | 2 | 2 | 1 | 1 |
| Intention to treat | 0 | 0 | 0 | 0 | 0 | 0 |
| Outcome assessors blind to the intervention | 1 | 1 | 0 | 0 | 0 | 0 |
| Comparability of subjects across comparison groups | 2 | 2 | 1 | 2 | 1 | 2 |
| Validity and reliability of the literacy measurement | 1 | 2 | 2 | 2 | 2 | 1 |
| Maintenance of comparable groups | 2 | 2 | 1 | 2 | 1 | 2 |
| Appropriateness of the outcome measurement | 2 | 2 | 2 | 2 | 2 | 2 |
| Appropriateness of statistical analysis | 1 | 2 | 1 | 1 | 2 | 2 |
| Adequacy of control of confounding | 2 | 2 | 1 | 1 | 2 | 1 |
| Quality rate | Fair/Good | Good | Fair | Fair/Good | Fair | Fair |
The final included articles were formatted, assessed and analyzed by an assessment instrument used in previous systematic reviews, as represented in Supplementary Table S1. (Arden-Close, Gidron, & Moss-Morris, 2008; Montgomery & McCrone, 2010).
Data abstraction and synthesis
The two-reviewer approach was adopted to review the titles, abstracts and content of the selected articles. A data extraction form was developed and circulated for agreement between the two reviewers. As the extracted articles contained vast variation in their study aims and methods, a systematic review was carried out rather than a meta-analysis (Whittemore, 2005).
Results
Descriptive information
Six interventional articles were included in this review. There were 4 randomized controlled trial (RCT) studies (Cavanaugh et al., 2009; Gerber et al., 2005; Rosal et al., 2011; Rosal et al., 2005), as well as 2 one-group pre-test post-test interventional studies (Dewalt & Hink, 2009; Kim, Love, Quistberg, & Shea, 2004).
A total of 980 T2DM patients were involved in the six reviewed studies. Most of the patients involved were middle aged to older adults (age from 45 to 67.2). All the studies were conducted in the United States. Five articles were published between mid to late 2000s, and one other was published in 2011(Rosal et al., 2011).
The quality appraisal conducted showed that only one study was rated at good standard (Cavanaugh et al., 2009). Two studies were rated in between good and fair (Gerber et al., 2005; Rosal et al., 2011). Three studies belonged to the fair standard (DeWalt & Hink, 2009; Rosal et al. 2005; Kim et al., 2004). Instead of a conservative approach, the Intention to Treat (ITT) approach was employed to analyze the result. ITT considered every participant who began the treatment as part of the trial regardless to whether they have completed treatment (Portney & Watkins, 2009). Table 2 represents the outcomes the quality appraisal of the reviewed articles.
The effectiveness of health literacy oriented programs on physical activity
Intervention to improve HL seemed to have somewhat suggestive effect on PA behavior in middle aged and older adults with T2DM. In Rosal and colleagues’ study, highly significant differences in PA behaviors and walking habits were observed in the intervention group after the health literacy oriented programs (Rosal et al., 2005). Gerber and colleagues reported improved perceived susceptibility of diabetes complications, with a gradient of effect where participants with lower HL at baseline improved more than those with higher HL after the intervention (Gerber et al., 2005). Cavanaugh and colleagues affirmed the effectiveness of intervention with numeracy (Cavanaugh et al., 2009), a component of HL, on the self-management behaviors including PA behavior in intervention group. Kim and colleagues further confirmed that health literacy oriented programs is effective to modify the PA especially in T2DM patients with higher HL levels (Kim et al., 2004).
The changes in PA behavior accelerated with the duration of health literacy oriented programs in one article (Rosal et al., 2005). The authors showed that the differences of calories consumption through PA activities between intervention group and controlled group widened at sixth month when compared to three months ago.
Moreover, PA was nearly the most popular choice compared to medication and diet in health literacy oriented programs in two articles (Cavanaugh et al., 2009; DeWalt & Hink, 2009).
However, Rosal and colleagues rejected the effectiveness of health literacy oriented programs on PA behavior in an RCT study published in 2011 (Rosal et al., 2011). Though there was a greater trend of walking habits in intervention group, the difference was not significant. The total time of exercise and the time of walking did not improve significantly after the health literacy oriented programs.
In two articles, health literacy oriented programs significantly enhanced the self-efficacy of self-management behavior (including PA) and the knowledge of self-management behavior (including PA). Moreover, four perceived barriers of PA behaviors namely lack of prompting by clinical staff, time constraints, availability of technology, and personal factors, were identified in an RCT study (Gerber et al., 2005). However, no studies implied the mediating effect of self-efficacy, knowledge of PA and perceived barrier between health literacy oriented programs and PA behavior (Cavanaugh et al., 2009; Kim et al., 2004; Rosal et al., 2011).
Discussion
It is too early to draw conclusion on the effectiveness of health literacy oriented programs to modify PA behaviour of middle aged and older T2DM patient.The evidence supporting the effectiveness of health literacy oriented programs on PA behaviour is untenable. This review consisted of 4 randomized controlled trials (RCT) and 2 one-group pre-test post-test interventional studies, of which only one study design was rated good standard at quality appraisal. The supportive findings revealed by DeWalt and Hink (2009) and Kim et al. (2004) concerned within-group comparisons solely, which made examination of the health literacy oriented programs difficult as the effective influence on PA could be implicated by confounders (DeWalt & Hink, 2009; Kim et al., 2004).
Moreover, studies have reported conflicting findings on the effectiveness of health literacy oriented programs on PA behavior. The main study of Rosal and colleagues in 2011 (N=211) rejected their own positive finding about the effectiveness of health literacy oriented programs on PA behavior in a previous pilot RCT study (N=25) conducted in 2005 (Rosal et al., 2011; Rosal et al., 2005). The great difference in the sample size of the two studies could have influenced the investigations. Because the earlier study recruited only illiterate T2DM patients, sample bias could have confounded the positive evidence of health literacy oriented programs on PA (Rosal et al., 2005).
Though positive effects of health literacy oriented programs on PA behavior were found in other two RCT studies (Cavanaugh et al., 2009; Gerber et al., 2005), plus Kim and colleagues’ one-group study (Kim et al., 2004), PA was not distinctly and objectively investigated as a dependent variable. The majority of articles considered PA behavior as one of the components of the self-management behaviors (PA, diet, self-monitoring of blood glucose, foot care, medication adherence, etc.) with subjective self-reported measurements. No reviewed study designed health literacy oriented programs specifically to modify PA behavior of T2DM patients. Furthermore, only the frequency and duration of PA were collected as outcome measures. The intensity of exercise, which is the most important factor affecting the blood glucose control, was not measured in the reviewed articles (American College of Sports Medicine, 2010; American Diabetes Association, 2010; Shigaki et al., 2010; Sigal et al., 2004). Objective measurements with aid of pedometers and accelerometers to monitor the numbers of steps exercised by patients could provide a reliable outcome measure of PA, hence enabling researchers to elucidate the relationship between health literacy oriented programs and PA in SOBA and older T2DM patients. The limitation of our articles screening process was that only full text articles published in English were included from nine academic databases. It was uncertain that other related articles existed or not. Despite the methodological shortcomings, the message conveyed by the six reviewed studies suggested that health literacy oriented programs could foster PA behavior in SOBA and older adults with T2DM when carefully designed and investigated.
In addition, according to Institute of Medicine (2004), culture and language foster health literacy. Diversity exists in the manifestation of health literacy in different countries All the studies reviewed were conducted in the United States; therefore the generalizability of the findings remains limited. Although validated instruments were used to measure HL, four different instruments were used in the reviewed studies. The extent to which the results were affected by different instruments could not be estimated.
Conclusions
Health literacy oriented programs for T2DM patients remains unconsummated. Paache-Orlow and Wolf (2007) indicated that PA behaviour could only be modified through theoretically and systematically planned health literacy oriented programs. In Paache-Orlow and Wolf’s model, knowledge and health beliefs including self-efficacy were the mediating factors between the HL and PA behaviour. Osborn and colleagues (2011) confirmed the mediating effect of knowledge of PA and self-efficacy of PA between HL and PA behaviours of patients with hypertension. Based on the articles reviewed, potential theories or factors such as knowledge of PA, self-efficacy of PA and perceived barriers of PA could affect the health literacy oriented programs on PA behavior. Rosal and colleagues (2011) intended to align the related mediators (knowledge, attitude and self-efficacy) with the related constructs of Social Cognitive Theory to design health literacy oriented programs tailor-made for Latino population in the U.S. More sophisticated theory-based intervention should be planned for different countries, races, culture and language (Institute of Medicine, 2004).
Relevance to clinical practice
Future health literacy oriented programs on PA behavior for middle aged and older patients with T2DM shall focus on i) the objective measurement of PA of health literacy oriented programs; ii) more theoretical, cultural and language appropriate health literacy oriented programs in different countries; iii) duration of the intervention and follow up. Interventions to increase knowledge and self-efficacy of PA and reduce perceived barriers may enhance PA via health literacy programs.
Acknowledgements
The authors are grateful to the sources of support from the School of Nursing, the University of Hong Kong. A special thank is given to Professor Marion Good, visiting professor of the University of Hong Kong, for her kind advice and review of this paper. Besides, thanks to Mr Henness H. G. Wong, research manager of the Hong Kong Sport Education Association, for his assistance in editing this publication.
References
- American College of Sports Medicine. (2010). ACSM’s Guidelines for Exercise Testing and Prescription. 9th ed. Philadelphia: Lippincott Williams & Wilkins. [Google Scholar]
- American Diabetes Association. (2010). Executive Summary: Standards of medical care in diabetes 2010. Diabetes Care, 33(Suppl.1), 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arden-Close E., Gidron Y., Moss-Morris R. (2008). Psychological distress and its correlates in ovarian cancer: a systematic review. Psychooncology, 17(11), 1061-1072. doi: 10.1002/pon.1363 [DOI] [PubMed] [Google Scholar]
- Berkman N.D., DeWalt D.A., Pignone M.P., Sheridan S.L., Lohr K.N., Lux L., Bonito A.J. (2004). Literacy and health outcomes: summary. In U.S. Department of Health and Human Services (Eds.), Agency for Healthcare Research and Quality Evidence Report Summaries (p. 87). Retrieved 27 March, 2013, from http://www.ncbi.nlm.nih.gov/books/NBK11942. [PMC free article] [PubMed] [Google Scholar]
- Cardona-Morrell M., Rychetnik L., Morrell S.L., Espinel P.T., Bauman A. (2010). Reduction of diabetes risk in routine clinical practice: are physical activity and nutrition interventions feasible and are the outcomes from reference trials replicable? A systematic review and meta-analysis. BMC public health, 10(1), 653-663. doi: 10.1186/1471-2458-10-653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh K., Wallston K.A., Gebretsadik T., Shintani A., Huizinga M.M., Davis D., Rothman R.L. (2009). Addressing literacy and numeracy to improve diabetes care: two randomized controlled trials. Diabetes Care, 32(12), 2149-2155. doi: 10.2337/dc09-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan Y.M., Molassiotis A. (1999). The relationship between diabetes knowledge and compliance among Chinese with non-insulin dependent diabetes mellitus in Hong Kong. Journal of Advanced Nursing, 30(2), 431-438. [DOI] [PubMed] [Google Scholar]
- Chao D., Foy C.G., Farmer D. (2000). Exercise adherence among older adults: Challenges and strategies. Controlled Clinical Trials, 21(5 Suppl), 212-217. [DOI] [PubMed] [Google Scholar]
- Colberg S.R., Albright A.L., Blissmer B.J., Braun B., Chasan-Taber L., Fernhall B., American-Diabetes-Association. (2010). Exercise and type 2 diabetes: American College of Sports Medicine and the American Diabetes Association: joint position statement. Exercise and type 2 diabetes. Medicine and Science in Sports and Exercise, 42(12), 2282-2303. doi: 10.1249/MSS.0b013e3181eeb61c [DOI] [PubMed] [Google Scholar]
- Conn V.S., Minor M.A., Burks K.J., Rantz M.J., Pomeroy S.H. (2003). Integrative review of physical activity intervention research with aging adults. Journal of the American Geriatrics Society, 51(8), 1159-1168. [DOI] [PubMed] [Google Scholar]
- Cutilli C.C. (2007). Health literacy in geriatric patients: an integrative review of the literature. Orthopaedic Nursing, 26(1), 43-48. [DOI] [PubMed] [Google Scholar]
- DeWalt D.A., Hink A. (2009). Health literacy and child health outcomes: a systematic review of the literature. Pediatrics, 124 (Suppl 3), 265-274. doi: 10.1542/peds.2009-1162B. [DOI] [PubMed] [Google Scholar]
- Edwards M., Hill S., Edwards A. (2009). A Health literacy-achieving consumer “empowerment’ in health decisions. Edwards A., Elwyn G. (Eds.), Shared decision-making in health care: achieving evidence-based patient choice (pp. 102-107). New York: Oxford University Press. [Google Scholar]
- Galson S. (2008). Minutes of the Board of Regents, Department of Health and Human Services National Institutes of Health, National Library of Medicine. Retrieved 7 August, 2013, from http://www.nlm.nih.gov/od/bor/5-08bor.pdf. [Google Scholar]
- Gazmararian J.A., Williams M.V., Peel J., Baker D.W. (2003). Health literacy and knowledge of chronic disease. Patient Education and Counseling, 51(3), 267-275. [DOI] [PubMed] [Google Scholar]
- Gerber B.S., Brodsky I.G., Lawless K.A., Smolin L.I., Arozullah A.M., Smith E.V., Eiser A.R. (2005). Implementation and evaluation of a low-literacy diabetes education computer multimedia application. Diabetes Care, 28(7), 1574-1580. [DOI] [PubMed] [Google Scholar]
- Hamel L.M., Robbins L.B., Wilbur J. (2011). Computer- and web-based interventions to increase preadolescent and adolescent physical activity: a systematic review. Journal of Advanced Nursing, 67(2), 251-268. doi: 10.1111/j.1365-2648.2010.05493.x. [DOI] [PubMed] [Google Scholar]
- Hudon C., Fortin M., Soubhi H. (2008). Single risk factor interventions to promote physical activity among patients with chronic diseases: systematic review. Canadian Family Physician, 54(8), 1130-1137. [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2004). Health literacy: a prescription to end confusion. Washington: DC: National Academies Press. [PubMed] [Google Scholar]
- Jadad A.R., Moore R.A., Carroll D., Jenkinson C., Reynolds D.J.M., Gavaghan D.J., McQuay H.J. (1996). Assessing the quality of reports of randomized clinical trials: is blinding necessary? Controlled Clinical Trials, 17(1), 1-12. [DOI] [PubMed] [Google Scholar]
- Jeon C.Y., Lokken R.P., Hu F.B., van Dam R.M. (2007). Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care, 30(3), 744-752. doi: 10.2337/dc06-1842. [DOI] [PubMed] [Google Scholar]
- Kim S., Love F., Quistberg D.A., Shea J.A. (2004). Association of health literacy with self-management behavior in patients with diabetes. Diabetes Care, 27(12), 2980-2982. [DOI] [PubMed] [Google Scholar]
- Mancuso J.M. (2010). Impact of health literacy and patient trust on glycemic control in an urban USA population. Nursing & Health Sciences, 12(1), 94-104. doi: 10.1111/j.1442-2018.2009.00506.x. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. (2010). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International Journal of Surgery, 8(5), 336-341. doi: 10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- Montgomery M., McCrone S.H. (2010). Psychological distress associated with the diagnostic phase for suspected breast cancer: systematic review. Journal of Advanced Nursing, 66(11), 2372-2390. doi: 10.1111/j.1365-2648.2010.05439.x. [DOI] [PubMed] [Google Scholar]
- Osborn C.Y., Paasche-Orlow M.K., Bailey S.C., Wolf M.S. (2011). The mechanisms linking health literacy to behavior and health status. American Journal of Health Behavior, 35(1), 118-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paasche-Orlow M.K., Wolf M.S. (2007). The causal pathways linking health literacy to health outcomes. American Journal of Health Behavior, 31(Suppl 1), 19-26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- Portney L.G., Watkins M.P. (2009). Foundations of Clinical Research: Applications to Practice. 3rd ed. Upper Saddle River, N.J.: Pearson/Prentice Hall. [Google Scholar]
- Rosal M.C., Ockene I.S., Restrepo A., White M.J., Borg A., Olendzki B., …, Reed G. (2011). Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income latinos en control. Diabetes Care, 34(4), 838-844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosal M.C., Olendzki B., Reed G.W., Gumieniak O., Scavron J., Ockene I. (2005). Diabetes self-management among low-income Spanish-speaking patients: a pilot study. Annals of Behavioral Medicine, 29(3), 225-235. doi: 10.1207/s15324796abm2903_9 [DOI] [PubMed] [Google Scholar]
- Schillinger D., Grumbach K., Piette J., Wang F., Osmond D., Daher C., …, Bindman A. B. (2002). Association of health literacy with diabetes outcomes. The Journal of the American Medical Association, 288(4), 475-482. [DOI] [PubMed] [Google Scholar]
- Schulz K.F., Chalmers I., Hayes R.J., Altman D.G. (1995). Empirical evidence of bias. JAMA: the Journal of the American Medical Association, 273(5), 408-412. [DOI] [PubMed] [Google Scholar]
- Shigaki C., Kruse R.L., Mehr D., Sheldon K.M., Bin G., Moore C., Lemaster J. (2010). Motivation and diabetes self-management. Chronic Illness, 6(3), 202-214. doi: 10.1177/1742395310375630 [DOI] [PubMed] [Google Scholar]
- Shih S.N., Gau M. L., Kao P., Lo C. H., Shih F. J. (2005). Health Needs Instrument for hospitalized single-living Taiwanese elders with heart disease: triangulation research design. Journal of Clinical Nursing, 14(10), 1210-1222. doi: 10.1111/j.1365-2702.2005.01201.x [DOI] [PubMed] [Google Scholar]
- Sigal R.J., Kenny G.P., Wasserman D.H., Castaneda-Sceppa C. (2004). Physical activity/exercise and type 2 diabetes. Diabetes Care, 27(10), 2518-2539. [DOI] [PubMed] [Google Scholar]
- Tang Y.H., Pang S.M., Chan M.F., Yeung G.S., Yeung V.T. (2008). Health literacy, complication awareness, and diabetes control in patients with type 2 diabetes mellitus. Journal of Advanced Nursing, 62(1), 74-83. doi: 10.1111/j.1365-2648.2007.04526.x. [DOI] [PubMed] [Google Scholar]
- Whittemore R. (2005). Combining evidence in nursing research: methods andmplications. Nursing Research, 54(1), 56-62. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2011). Diabetes health topic. Retrieved 18 Febuary, 2012, from http://www.who.int/topics/diabetes_mellitus/en/.


