Abstract
Background: Headaches are prevalent among Service members with traumatic brain injury (TBI); 80% report chronic or recurrent headache. Evidence for nonpharmacologic treatments, such as acupuncture, are needed.
Objective: The aim of this research was to determine if two types of acupuncture (auricular acupuncture [AA] and traditional Chinese acupuncture [TCA]) were feasible and more effective than usual care (UC) alone for TBI–related headache.
Materials and Methods: Design: This was a three-armed, parallel, randomized exploratory study. Setting: The research took place at three military treatment facilities in the Washington, DC, metropolitan area. Patients: The subjects were previously deployed Service members (18–69 years old) with mild-to-moderate TBI and headaches. Intervention: The interventions explored were UC alone or with the addition of AA or TCA. Outcome Measures: The primary outcome was the Headache Impact Test (HIT). Secondary outcomes were the Numerical Rating Scale (NRS), Pittsburgh Sleep Quality Index, Post-Traumatic Stress Checklist, Symptom Checklist-90-R, Medical Outcome Study Quality of Life (QoL), Beck Depression Inventory, State-Trait Anxiety Inventory, the Automated Neuropsychological Assessment Metrics, and expectancy of outcome and acupuncture efficacy.
Results: Mean HIT scores decreased in the AA and TCA groups but increased slightly in the UC-only group from baseline to week 6 [AA, −10.2% (−6.4 points); TCA, −4.6% (−2.9 points); UC, +0.8% (+0.6 points)]. Both acupuncture groups had sizable decreases in NRS (Pain Best), compared to UC (TCA versus UC: P = 0.0008, d = 1.70; AA versus UC: P = 0.0127, d = 1.6). No statistically significant results were found for any other secondary outcome measures.
Conclusions: Both AA and TCA improved headache-related QoL more than UC did in Service members with TBI.
Key Words: : Traumatic Brian Injury, Headache, Pain Management, Acupuncture
Introduction
Estimates of the prevalence of traumatic brain injury (TBI) among military Service members range from 9.6%1 to >20%2 with a total of >330,000 cases of TBI among Military personnel since 2000.3 Combat-related TBI is commonly associated with post-traumatic stress disorder (PTSD), sensory difficulties, sleep disturbance, and chronic pain, especially headache. Awareness of TBI-related symptoms has increased as the result of the Military conflicts in Afghanistan (Operation Enduring Freedom; OEF) and Iraq (Operation Iraqi Freedom; OIF and Operation New Dawn; OND).4
There is no universally accepted term to characterize the constellation of symptoms that can occur after sustaining physical and/or psychologic trauma. Within the populations with PTSD and TBI, it is becoming increasingly apparent that many symptoms occur together as complex, multisymptom illnesses (e.g., pain, depression, anxiety, sleep disturbance, and diminished cognition).5 The range of symptomatology that describes these coexisting sequelae has been called the trauma spectrum response (TSR).6
Conventional medical treatments usually focus on single or clusters of symptoms that are classified into diagnostic categories and treated individually. While this approach may provide symptom relief, its multiple treatment strategies and polypharmacy are often complicated by adverse effects. Acupuncture, in contrast, has been shown to elicit a dynamic, multimechanism response and has the potential to influence multiple interacting components of trauma response and recovery.7 As such, acupuncture has the potential to address multiple rather than single symptoms in order to address whole-person recovery.7 Systematic reviews of acupuncture have shown its benefits for relieving headaches of various types (e.g., migraine, tension, and chronic daily headaches),8–12 as well as sleep disturbance, anxiety, depression, PTSD, and pain.13–23 Consequently, it is a treatment approach that is well-suited for facilitating recovery after trauma. However, the optimal acupuncture treatment for post-trauma symptoms has not been well-characterized or studied.
This study was conducted to compare two types of acupuncture approaches currently being used in Military treatment facilities (MTFs) to usual care (UC). Specifically, traditional Chinese acupuncture (TCA), an auricular acupuncture (AA) protocol, and UC alone were examined to determine their comparative effectiveness for treating TBI-associated headaches and comorbid symptoms of trauma. The authors chose to investigate primarily the effects of acupuncture on headache, one of the most common TBI-related symptoms, and, secondarily, on the constellation of comorbid TSR symptoms.
Although founded on similar basic principles, TCA and AA differ in focus, diagnostic approach, needle sites, and duration of treatment. TCA is tailored to the individual and involves the insertion of thin needles at specific anatomical locations with an intention to restore dynamic regulation and stimulate healing. AA is more symptom-focused and response-driven. AA views the ear as a somatotopic map; specific points are needled in the outer ear to affect distal anatomical regions.24
TCA treatment sessions are typically longer and more involved, using an “energy balancing” framework to both contextualize and deliver treatment and judge responses.25 Presenting symptoms and underlying problems are evaluated in the context of a patient's underlying constitutional strengths and weaknesses (i.e., personality/characteristics), pulse and tongue characteristics, and pattern of symptoms. Treatment goals include symptom reduction as well as enhanced energy, long-term health maintenance, and prevention of symptom relapses.24
Conversely, AA follows a standardized algorithm that focuses on alleviating primary symptoms and takes less practitioner time to deliver. AA is not framed in terms of TCA theory; instead, using a set sequence for inserting needles and studs into the ear cartilage, AA is guided by the patient's response. With AA, indwelling ear studs are retained for longer periods of time (up to hours or days after the treatment visit), compared to TCA, in which the needles are inserted and removed during the treatment session. Another difference is that TCA takes years of specialized education and training to learn and gain mastery, whereas AA is a simple technique usually taught over the course of several days.
MTFs are often challenged by clinical-practice time constraints, the need to treat patients quickly in combat-operational environments, and the transitory nature of frequently deployed patients. While it is necessary to identify safe and effective treatments, it is also imperative to consider the feasibility of such interventions, given these unique challenges. Given that this research study was conducted during the height of the OEF/OIF/OND conflicts, a primary objective was to determine if it was feasible to deliver acupuncture as an adjunctive treatment in MTFs and whether one or both acupuncture approaches were more effective than delivering usual care alone. Specifically, this exploratory study sought to determine whether either acupuncture method was more effective than UC for patients with TBI in three areas: (1) improving headache-related quality of life (QoL); (2) decreasing headache frequency and severity; and (3) reducing comorbid symptoms associated with TBI. The central hypotheses of this study were that: (1) both acupuncture methods would improve headache-related QoL and reduce headache severity and frequency over a 6-week study period, compared to the UC-only group; and (2) comorbid symptoms would be reduced in a more-favorable direction in the TCA group, compared to AA or UC-only groups.
Materials and Methods
Study Design Overview
This randomized, controlled exploratory study compared the effect of semi-standardized TCA, an AA protocol, and UC on headaches and related symptoms in a cohort of active Duty Service members with mild-to-moderate TBI (mTBI). Study participants were randomized to usual care plus TCA or AA, or UC only. Patients who were randomized to either acupuncture group received 10 treatments during the 6-week study duration. Patients who were randomized to UC-only were asked to follow their usual medical care as delivered by their MTF clinicians and, after a 6-week wait period, were offered the option of receiving AA. A follow-up assessment was conducted on all available study participants at week 12.
Setting
The study was approved and conducted at three sites in the Washington, DC, metropolitan area: Walter Reed Army Medical Center (WRAMC, from February to August 2011), Walter Reed National Military Medical Center (WRNMMC, from September 2011 to March 2013), and Fort Belvoir Community Hospital (FBCH, from March to April 2015). The transition in sites from WRAMC to WRNMMC occurred as a result of the 2005 Base Realignment and Closure (BRAC); the opening of the study at FBCH was to increase study enrollment. In accordance with Department of Defense (DoD) guidelines, regulatory approvals were obtained from the WRAMC Human Use Committee, the Clinical Investigation Regulatory Office (CIRO), WRNMMC institutional review board (IRB), the Army CIRO, and the US Army Medical Research and Materiel Command Office of Research Protections Human Research Protections Office. All study staff had extensive clinical research experience and completed relevant Collaborative Institutional Training Initiative training.
Participants
Eligible participants were previously deployed Service members between the ages of 18 and 69 with a diagnosis of non-acute mTBI and current headaches of any etiology. Non-acute mTBI was diagnosed by an MTF clinician and based on standard DoD/Department of Veterans Affairs criteria,26 which included the following: (1) an injury event (i.e., blast, fall, motor-vehicle crash, head impact) that occurred at least 7 days prior; (2) loss of consciousness (if present) for <24 hours; and (3) alteration of consciousness or post-traumatic amnesia for <1 week. Frequent headaches were defined as at least 4 headache days per month that required the use of either prescription or over-the-counter medications to obtain relief. Satisfactory cognitive functioning was verified by a clinician who ensured that each participant had a Ranchos Los Amigos Cognitive Score of ≥7. Service members were ineligible if they had received acupuncture treatment within the past 4 weeks or had any unstable medical, psychiatric, or surgical conditions that might affect their ability to receive acupuncture over the study duration. Female Service members who were currently pregnant, lactating, or planning to become pregnant during the study were also ineligible to participate in this study.
Study Acupuncturists
Acupuncturists with Master's degrees in acupuncture from accredited institutions and licensure in Maryland and/or Virginia delivered the acupuncture interventions. In addition, the study acupuncturists obtained limited privileges through the study sites’ credentialing offices to deliver acupuncture within the context of this IRB-approved research study. These acupuncturists had extensive clinical experience, knowledge of traditional Chinese diagnosis, and expertise in treating chronic headaches and trauma. The lead study acupuncturist (A.D.) co-developed the TCA protocol and received individualized training in the AA protocol by its developer, Richard C. Niemtzow, MD, PhD, MPH, Col (Ret), U.S. Air Force. As such, she was responsible for training and supervising other study acupuncturists in both acupuncture protocols. A physician–acupuncturist (i.e., a physician with acupuncture training credentialed at the MTF) acted as a clinical supervisor.
Study Procedures
Recruitment
Research staff recruited potential study participants within the TBI, Orthopedic, and Physical Medicine and Rehabilitation Clinics at each MTF. Potentially eligible study participants learned about the study from case managers and IRB-approved study flyers. This allowed individuals to initiate contact directly with the research team if they were interested in participating in the study. Recruitment advertisements were disseminated at various locations, including hospital lobby areas and the National Intrepid Center of Excellence for Psychological Health and Traumatic Brain Injury. A Samueli Institute (Alexandria, VA) webpage with detailed study and contact information was created from IRB-approved recruitment flyers. In addition, the protocol was registered on clinicaltrials.gov.
Screening and enrollment
Research team members obtained authorization via written release of information (DD Form 2870) from interested participants prior to verifying their study eligibility. Once all eligibility criteria had been confirmed, potential study participants received a detailed explanation of the study, reviewed the IRB-approved informed consent documents (ICDs) and Health Insurance Portability and Accountability Act (HIPAA) forms together with a research team member, and had ample time for any questions to be answered. Each patient who agreed to participate in the study met with a civilian research team member in a private examination room and signed a written ICD. Study participants were informed that they were permitted to withdraw their participation at any time during the study for any reason. After signing the informed consent forms, female Service members of childbearing age underwent blood or urine pregnancy testing to ensure negative results.
Randomization procedure
The randomization sequence (TCA, AA, or UC) used a permuted block randomization, with block sizes of 6, that was generated via a computerized random-number generator and was stored in a double-password protected HIPAA-compliant database within a secure server at the Samueli Institute. When a new study participant was enrolled, a study research coordinator would refer to the randomization database and register each study participant's group assignment by the date and time of enrollment. Each participant's randomization assignment was concealed from the lead acupuncturist and the rest of the research team until after the participant's initial Traditional Chinese Medicine (TCM) assessment had been completed. Immediately after this assessment, the study acupuncturist was informed of the treatment assignment and communicated that information to the study participant. This approach offered two advantages: (1) it permitted the lead study acupuncturist to evaluate each individual without foreknowledge of their group assignment and (2) study participants randomized to TCA or AA could elect to receive their first acupuncture treatment on this initial visit.
Initial TCM assessment
The lead acupuncturist (A.D.) conducted a TCM assessment of each study participant. During this 90-minute clinical evaluation, she conducted a TCM assessment, using the 5-Element model of acupuncture diagnostic skills of evaluation and interpretation of symptoms (e.g., pulse reading and tongue diagnosis) to determine each participant's primary and secondary headache patterns. In addition, she identified each participant's constitutional type using the 5-Element acupuncture diagnostic approach of assessing color, sound, odor, and emotion, and she identified locally painful (i.e., Ah Shi) points. This information was used to characterize study participants by TCM diagnosis and formed the basis for choice of acupuncture points in the TCA-group participants.
Interventions
AA protocol
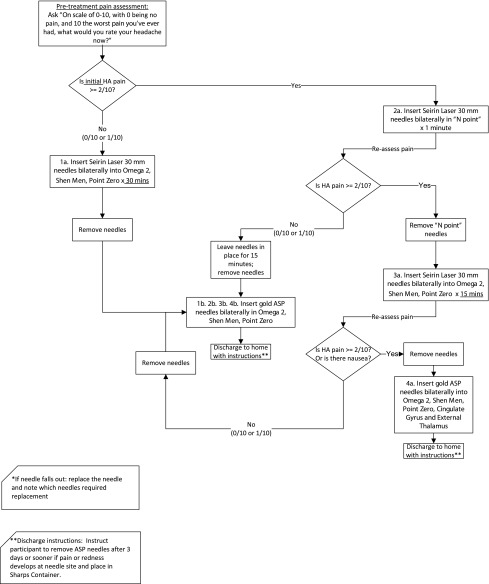
The AA protocol used in this study was created by Dr. Niemtzow, a former Active Duty Air Force physician–acupuncturist, who has used this procedure extensively in his practice and has found it to be effective for reducing chronic, refractory pain in military cohorts.27 In the AA protocol, two types of needles were used: 1-inch, SEIRIN® L type (SEIRIN L-Type LC 20 × 30 mm; SEIRIN®-America, Weymouth, MA), and gold Aiguille Semi-Permanente (ASP) needles (tiny, conical shaped studs placed in auricular points for several days; Sedatelec, Irigny, France). They were inserted at specific auricular landmarks, using a stepwise algorithmic approach. The sequence and location of needled points was determined by the participant's severity of headache pain at presentation and his/her response to needling during each session. Between six and nine points were needled in each treatment session depending on the individual's response (i.e., a decrease or persistence of headache pain on an 11-point Likert scale). Indwelling ASP needles were inserted at the end of each session and participants were instructed to remove the needles after 3 days, or sooner if pain or redness developed at a needle site. See Appendix 1 for AA protocol. For patients who were allocated to the AA group, ten 45-minute acupuncture treatment sessions were administered over 6 weeks.
TCA protocol
A semi-standardized TCA technique found to be effective for treating PTSD was the foundation for the current study's TCA protocol.28 Developed by Michael Hollifeld, MD and a team of acupuncturists, this approach predefines features of the primary condition in terms of TCM patterns and allows for a limited selection of individual acupuncture points to be used at each session. The TCA protocol used in the current study followed a similar approach. Twelve distinct TCA headache patterns and their associated acupuncture points were formulated by the study's lead acupuncturist (A.D.). This selection of patterns was based on likely conditions experienced by deployed Service members (e.g., nature of autonomic nervous system dysregulation caused by traumatic stress, exposure to extreme weather conditions or blast injuries, and comorbid symptomatology).
The TCA protocol incorporated the insertion of up to 22 acupuncture needles associated with each individual participant's: (1) primary headache pattern (up to three pairs of points); (2) secondary headache pattern (up to two pairs of points); (3) Ah Shi or tender points (up to four points); (4) constitutional points (Source points on two meridians); and, (5) up to two pairs of additional points from a selected list. See Appendix 2 for list of possible points. Point selection was reassessed every 2 weeks per TCM diagnostic and treatment principles. While the majority of points were located on the limbs, points also included local points of tenderness to the head, as well as the front and back of the torso. Acupuncture needles used in the TCA protocol were standard, sterile stainless-steel needles (SEIRIN L-Type LC 20 × 30 mm, SEIRIN L-Type 20 × 40 mm, SEIRIN J-15 JT 16 × 15 mm) and were inserted and removed at the completion of each session. Ten 60-minute TCA sessions were administered over a 6-week time period. While a consistent contextual approach (described in the following section) was implemented with all AA and TCA participants, the TCA sessions generally took about 15 minutes longer than AA sessions.
Consistent contextual approach
Anticipating that there might be differences between the two treatment groups in time (and therefore, possibly amount of attention) given to study participants, the study acupuncturists implemented a standardized approach to study participants at every encounter. This approach was designed to assist participants in orienting themselves to the present moment and fostering a sense of control and empowerment. After the treating acupuncturist greeted and escorted them to the treatment room, participants: (1) received several minutes of time to orient to the room; (2) voiced assent when they were ready for the needles to be inserted; and, (3) tracked their pain levels immediately before and after the treatment session. These data were recorded as pre–post-treatment pain levels.
UC
All study participants continued to receive routine UC for their TBI, headaches, and associated symptoms as determined by their clinical teams. A UC-only group was included in this study to assess the differences in primary outcome (i.e., headache-related QoL from pre- to postintervention) when acupuncture was added to UC. UC encompassed standard clinical care delivered at each MTF for treating TBI-associated headaches and included antidepressants; antiseizure agents; and beta-blockers for prevention; nonsteroidal anti-inflammatory drugs, triptans, and combination medications; and nonmedication treatment options, such as physical, occupational, and speech therapy for ongoing management.29 After completion of week 6 outcome measures, the UC group participants were offered a 6-week course of AA.
Outcome Measures
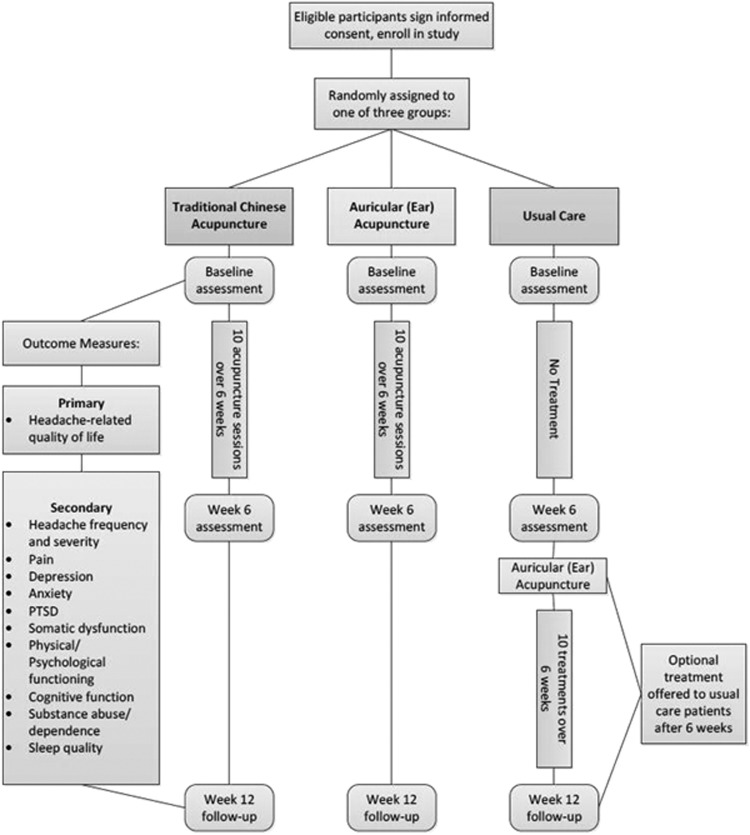
Outcome measures were obtained at three timepoints: (1) at baseline (prior to beginning the treatment period); (2) at week 6 (completion of 6 weeks of acupuncture treatment or UC only); and (3) at week 12 (completion of a no-treatment, 6-week follow-up time period). Primary and secondary outcome measures are depicted in Figure 1.
FIG. 1.
Study design. PTSD, post-traumatic stress disorder.
Primary outcome measure
The primary outcome was headache-related QoL as measured by the Headache Impact Test (HIT), a standardized 6-item questionnaire that is used to assess an individual's perception of headache burden over the past month.30,31
Secondary outcome measures
The following secondary outcomes were obtained using validated assessment measures. These measures were chosen to encompass the spectrum of TSR symptoms (chronic pain, sleep disturbance, anxiety, depression, PTSD, emotional function, cognitive function, somatic function, and fatigue).
Global pain severity was measured on a 0–10 point Numerical Rating Scale (NRS). Participants rated their current (Pain Now), usual (Pain Usual), best (Pain Best), and worst (Pain Worst) overall pain over the previous 7-day time period.32 Sleep quality was assessed with the Pittsburgh Sleep Quality Index (PSQI), which is used to assess sleep quality and disturbances over a 1-month time interval.33 PTSD was measured by the Post Traumatic Stress Checklist—Civilian Version (PCL-C),34 a self-report measure developed for assessing PTSD symptom severity. Somatic dysfunction was evaluated using the Symptom Checklist-90-R (SCL-90-R), which is used to evaluate a broad range of psychologic symptoms. Physical and psychologic functioning was assessed with the Medical Outcome Study Quality of Life (MOS SF-36), which is used to measure eight general health-related concepts.
Depression was initially assessed with the Hamilton Depression Rating Scale (HAM-D), a clinician-administered questionnaire. Because of limited availability of a licensed neuropsychologist to administer this measure, the depression measure was subsequently switched to the Beck Depression Inventory (BDI-II), a 21-question multiple choice self-report inventory. For the same reason, while anxiety was initially assessed with the Hamilton Anxiety Rating Scale (HAM-A), anxiety measurement was subsequently changed to the State-Trait Anxiety Inventory (STAI), a 40-item self-report assessment used to measure the severity of overall, state and trait anxiety symptoms. Cognitive function was evaluated through performance on the Automated Neuropsychological Assessment Metrics (ANAM), a common neurocognitive assessment tool used by the DoD. This tool is used to detect both the speed and accuracy of attention as well as memory and thinking ability.
Two assessments were designed specifically for this study. Daily headache frequency and severity and prescription and over-the-counter medication use, were documented in a Daily Headache Diary/Medication log. Participants were asked to enter their medication use and headache severity at the same time each day over the course of the study. A 2-item Expectancy Scale was adapted for this study by the research team in order to gauge participants’ preconceived expectations regarding acupuncture. The questions were delivered at baseline only and measured (1) expectancy of headache relief (“Using a scale from 0 to 10, with 0 being no improvement and 10 being complete recovery, how much improvement in your headaches do you expect in 6 weeks?”); and, (2) expectancy of acupuncture's effectiveness (“Using a scale from 0 to 10, with 0 being not at all helpful and 10 being extremely helpful, how helpful do you believe that acupuncture will be for your headaches?”).
Statistical Analyses
Sample size calculations were based on the expected minimal detectable effect size. With a 5% significance level and 80% power, the required sample size was estimated to be roughly 24 participants per group to detect a 0.91 minimal detectable effect size in change in the primary outcome measure. Assuming a 20% dropout rate, therefore, a starting size of 90 individuals was calculated for a definitive answer to the question.
For baseline univariate analysis, participant characteristics were reported, using descriptive statistics (e.g., for categorical variables and frequency counts, and for continuous variables, sample sizes, medians, means, and standard deviations). Baseline bivariate analyses were based on the entire study population using the full data set. For non–normally distributed continuous variables, a nonparametric ANOVA (Kruskal-Wallis Test) was utilized to test if there were differences between distributions. For normally distributed continuous variables, an ANOVA was utilized to test if participants were indeed randomly allocated to different treatment groups. For categorical variables, a Mantel-Haenszel χ2-test was utilized unless one of the cell counts was lower than 5, in which case, an extension of Fisher's exact test to r × c tables was utilized.
The primary and secondary hypotheses were tested based on a per-protocol population wherein only subjects who completed treatment were considered. This was because providing information regarding equivalence or non-inferiority between the TCA and AA groups wherein the per-protocol (i.e., analyzing only patients who completed treatment) approach is more appropriate than the intention-to-treat (i.e., analyzing all patients enrolled and randomized regardless of whether or not they completed treatment) approach.35 To test the effectiveness of acupuncture treatment, a nonparametric ANOVA (Kruskal-Wallis Test) was used to compare the pre–post differences among the treatment groups. The results were confirmed with repeated measures ANOVA (RMANOVA) analyses. The treatment group versus the control group was compared further, using two-sample Wilcoxon rank-sum tests, and was confirmed with two-sample t-tests. For the Wilcoxon rank-sum test, because the sample size was small, the large-sample normal approximation might not have been adequate; consequently, exact P-values were reported. Given that some tests were multiple comparisons and the significance level had to be adjusted (e.g., Bonferroni correction), P-values were reported and the interpretation of “statistically significant” results were used judiciously.36 Cohen's d effect sizes were also reported whenever possible.
Data analyses were carried out with SAS software, version 9.3 of the SAS System for Windows; SAS Institute Inc., Cary, NC. The Cohen's d effect size was calculated using a SAS macro created by Kadel and Kip.37
Results
Participant Flow
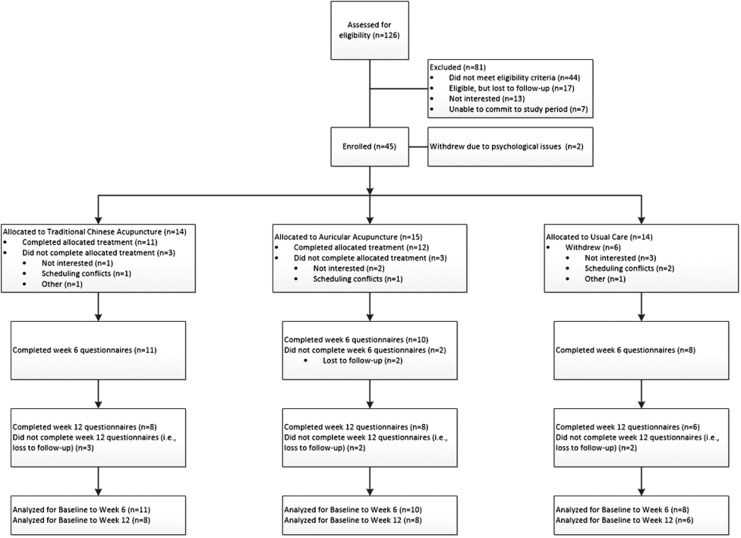
Research coordinators screened a total of 126 potential participants for eligibility at the three study sites (WRAMC, from February to August 2011; WRNMMC, from September 2011 to March 2013; and FBCH, from March to December 2013). Of these potential participants, 81 were excluded for various reasons, most often for not meeting all study inclusion criteria (n = 44, 54%; see Fig. 2). Forty-five participants were enrolled in the study. Two participants withdrew at baseline because of psychologic issues that precluded their ability to stay on-study for the 6-week duration. Therefore, the research coordinators assigned the randomized intervention to 43 participants: TCA (n = 14); AA (n = 15); and UC (n = 14). Twelve enrolled participants (28%) withdrew during the course of the study (TCA = 3, AA = 3, UC = 6); their reasons for withdrawing study participation are described in Figure 2. Six participants were considered lost to follow-up as they failed to complete the week 12 follow-up measures (Fig. 2).
FIG. 2.
Consolidated Standards of Reporting Trials (CONSORT) diagram.
Baseline Data
The majority of study participants were male (88.4%), Caucasian (57.9%), and had attended some college or obtained a college degree (65.1%). Their mean age was 34 years. The majority of participants (74.5%) had deployed 1–3 times, with more than half deployed for 18–36 months (53.5%). Most of the enrolled participants (76.7%) reported they had sustained more than one head injury. No baseline differences in any parameter were observed among the 3 groups except marital status (P = 0.0111) and rank (P = 0.0346). See Table 1.
Table 1.
Baseline Characteristics of Participants and Comparisons Among Groups
| Characteristics | TCA | AA | UC | Total | P-value |
|---|---|---|---|---|---|
| Participants, n | 14 | 15 | 14 | 43 | |
| Age, mean (SD) | 37 (9.4) | 35 (8.0) | 30 (8.2) | 34 (8.8) | |
| Gender, n (%) | NS | ||||
| Male | 12 (85.7) | 13 (86.7) | 13 (92.9) | 38 (88.4) | |
| Female | 2 (14.3) | 2 (13.3) | 1 (7.1) | 5 (11.6) | |
| Ethnicity, n (%) | NS | ||||
| Hispanic | 2 (14.3) | 4 (26.7) | 2 (14.3) | 8 (18.6) | |
| Non-Hispanic | 10 (71.4) | 11 (73.3) | 12 (85.7) | 33 (76.7) | |
| Not answered | 2 (14.3) | 0 (0.0) | 0 (0.0) | 2 (4.7) | |
| Race, n (%) | NS | ||||
| Caucasian | 8 (57.1) | 7 (46.7) | 7 (50.0) | 22 (51.1) | |
| Black or African American | 3 (21.4) | 1 (6.7) | 1 (6.7) | 5 (11.6) | |
| Other | 1 (7.1) | 5 (33.3) | 5 (35.7) | 11 (25.6) | |
| Not answered | 2 (14.3) | 2 (13.3) | 1 (7.1) | 5 (11.6) | |
| Education level, n (%) | NS | ||||
| High-school graduate or less | 3 (21.4) | 2 (13.3) | 4 (28.6) | 9 (20.9) | |
| Some college/college graduate | 9 (64.3) | 9 (60.0) | 10 (71.4) | 28 (65.1) | |
| Graduate-level degree | 1 (7.1) | 3 (20.0) | 0 (0.0) | 4 (9.3) | |
| Not answered | 1 (7.1) | 1 (6.7) | 0 (0.0) | 2 (4.7) | |
| Marital status, n (%) | 0.0111 | ||||
| Single/separated | 7 (50.0) | 2 (14.3) | 10 (71.4) | 19 (45.2) | |
| Married | 7 (50.0) | 12 (85.7) | 4 (28.6) | 23 (54.8) | |
| Rank, n (%) | 0.0346 | ||||
| Officer | 1 (7.1) | 5 (33.3) | 0 (0.0) | 6 (14.0) | |
| Enlisted | 13 (92.9) | 10 (66.7) | 14 (100.0) | 37 (86.0) | |
| Number of times deployed, n (%) | NS | ||||
| 1 time | 2 (14.3) | 3 (20.0) | 6 (42.9) | 11 (25.6) | |
| 2 times | 3 (21.4) | 3 (20.0) | 5 (35.7) | 11 (25.6) | |
| 3 times | 4 (28.6) | 4 (26.7) | 2 (14.3) | 10 (23.3) | |
| 4 times | 3 (21.4) | 3 (20.0) | 1 (7.1) | 7 (16.3) | |
| 5 or more times | 2 (14.2) | 1 (6.7) | 0 (0.0) | 3 (7.0) | |
| N/A | 0 (0.0) | 1 (6.7) | 0 (0.0) | 1 (2.3) | |
| Total of months deployed, n (%) | NS | ||||
| 1–3 months | 0 (0.0) | 0 (0.0) | 1 (7.1) | 1 (2.3) | |
| 4–6 months | 0 (0.0) | 2 (13.3) | 0 (0.0) | 2 (4.7) | |
| 7–11 months | 1 (7.1) | 0 (0.0) | 3 (21.4) | 4 (9.3) | |
| 12–17 months | 1 (7.1) | 1 (6.7) | 3 (21.4) | 5 (11.6) | |
| 18–23 months | 4 (28.6) | 3 (20.0) | 2 (14.3) | 9 (20.9) | |
| 24–36 months | 4 (28.6) | 5 (33.3) | 5 (35.7) | 14 (32.6) | |
| >36 months | 4 (28.6) | 2 (13.3) | 0 (0.0) | 6 (14.0) | |
| N/A | 0 (0.0) | 2 (13.3) | 0 (0.0) | 2 (4.7) | |
| Total number of head injuries, n (%) | NS | ||||
| 1 | 3 (21.4) | 3 (20.0) | 4 (28.6) | 10 (23.3) | |
| > 1 | 11 (78.6) | 12 (80.0) | 10 (71.4) | 33 (76.7) |
TCA, traditional Chinese acupuncture; AA, auricular acupuncture; UC, usual care; SD, standard deviation; NS, nonsignificant; NA, not answered.
Primary outcome
The mean HIT scores decreased in both the AA and TCA groups, but slightly increased in the UC group from baseline to week 6 (AA, −10.2% [−6.4 points]; TCA, −4.6% [−2.9 points]; UC, +0.8% [+0.6 points]). This change in HIT scores from baseline to week 6 in each acupuncture group, compared to UC, is shown in Figure 3A and in Table 2. The between-group differences showed that the AA group had a statistically significant reduction in mean HIT scores, compared to UC (AA versus UC: −7.03; P = 0.0079; Cohen's d = 1.28). The TCA group also had greater mean improvements in HIT than UC, but these differences were not statistically significant (TCA versus UC: −3.53; P = 0.1566; d = 0.72). When both acupuncture groups were combined (Acup), HIT scores showed a significant improvement over UC (Acup versus UC: −5.20; P = 0.0213; d = 0.98; Table 2, Fig. 3B). The within-group differences in HIT scores did not reach statistical significance for either acupuncture group; however, decreases of 6.4 points (AA group) and 2.9 points (TCA group) in the HIT likely represents clinically meaningful improvements.
FIG. 3.
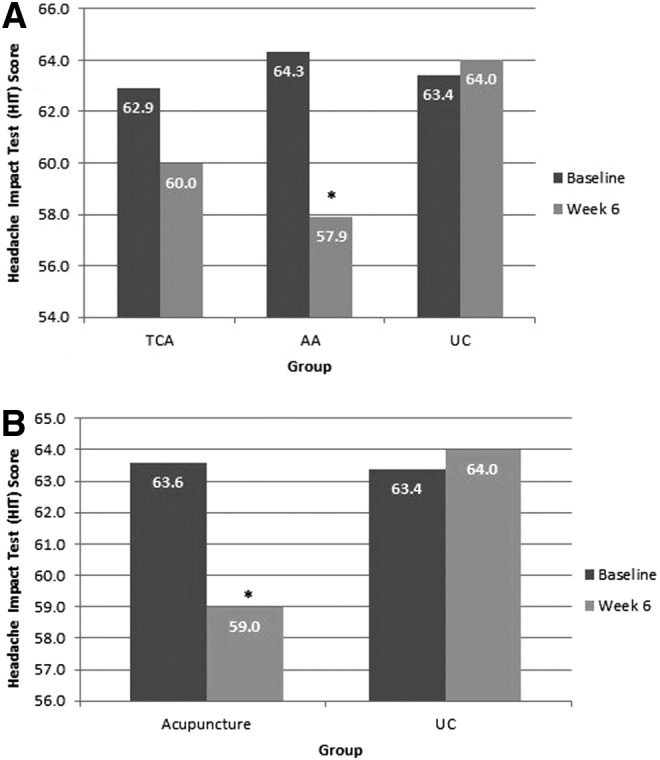
(A) Average Headache Impact Test (HIT) scores from baseline to week 6, between groups: Treatment versus usual care. (B) Average HIT scores from baseline to week 6: acupuncture versus UC. *P = 0.009 for AA versus UC and *P = 0.0234 for acupuncture versus UC.
Table 2.
Between-Group Differences from Baseline to Week 6: Treatment Versus Usual Care
| TCA vs UC | AA vs UC | Acupuncture vs UC | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measure | Mean Diff | SD | P-value | d* | Mean Diff | SD | P-value | d | Mean Diff | SD | P-value | d |
| HIT | −3.53 | 4.67 | NS§ | 0.72 | −7.03 | 4.99 | 0.0079 | 1.28 | −5.20 | 5.20 | 0.0213 | 0.98 |
| NRS: Pain Now | −2.23 | 1.42 | 0.0036 | 1.54 | −1.80 | 1.42 | 0.0155 | 1.25 | −2.02 | 1.43 | 0.0021 | 1.42 |
| NRS: Pain Usual | −2.13 | 1.50 | 0.0166 | 1.43 | −1.40 | 1.45 | NS | 1.04 | −1.78 | 1.58 | 0.0153 | 1.25 |
| NRS: Pain Best | −2.08 | 1.38 | 0.0008 | 1.70 | −1.72 | 1.19 | 0.0127 | 1.60 | −1.91 | 1.39 | 0.0004 | 1.66 |
| NRS: Pain Worst | −0.34 | 1.34 | NS | 0.24 | −1.45 | 1.99 | NS | 0.69 | −0.87 | 1.75 | NS | 0.50 |
| PSQI | −0.09 | 5.06 | NS | 0.36 | 0.00 | 5.29 | NS | 0.26 | −0.05 | 4.67 | NS | 0.33 |
| PCL-C: Global Score | −6.02 | 10.74 | NS | 0.40 | −3.85 | 11.04 | NS | 0.22 | −4.99 | 11.90 | NS | 0.32 |
| SCL-90-R: Anxiety | −0.02 | 0.56 | NS | 0.28 | 0.22 | 0.57 | NS | −0.50 | 0.10 | 0.61 | NS | −0.31 |
| SCL-90-R: Depression | −0.19 | 0.59 | NS | 0.01 | −0.31 | 0.44 | NS | 0.61 | −0.25 | 0.54 | NS | 0.33 |
| MOS SF-36 Health Survey: General Health | 0.38 | 5.67 | NS | −0.08 | 1.74 | 4.29 | NS | −0.45 | 1.03 | 4.95 | NS | −0.20 |
| BDI-II | −1.43 | 3.39 | NS | 0.42 | −0.44 | 10.27 | NS | 0.17 | −0.90 | 8.44 | NS | 0.21 |
| STAI: State | −3.52 | 6.40 | NS | 0.54 | −0.42 | 12.94 | NS | 0.09 | −1.87 | 11.02 | NS | 0.21 |
| STAI: Trait | −2.45 | 5.48 | NS | 0.41 | 0.46 | 11.72 | NS | −0.14 | −0.90 | 9.94 | NS | −0.01 |
P-values were calculated using the Wilcoxon rank-sum test with exact P-value
Cohen's d for effect size. Standard deviations were calculated using the change score of each group.
TCA, traditional Chinese acupuncture; UC, usual care; AA, auricular acupuncture; diff, difference, SD, standard deviation; HIT, Headache Impact Test; NRS, Numerical Rating Scale; PSQI, Pittsburgh Sleep Quality Index; PTSD, post-traumatic stress disorder; PCL-C, Post Traumatic Stress Checklist—Civilian Version; SCL, Symptom Checklist; MOS-SF, Medical Outcome Study-Short Form; BDI, Beck Depression Index; STAI, State-Trait Anxiety Inventory; NS, nonsignificant.
Secondary outcomes
The change in current global pain (mean NRS: Pain Now scores) for both TCA and AA groups decreased substantially from baseline to week 6, compared to UC (TCA P = 0.0036, d = 1.54; AA P = 0.0155, d = 1.25). Usual pain (mean NRS: Pain Usual scores) decreased more in the TCA group (P = 0.0166, d = 1.43) than in the AA group (P = 0.10, d = 1.04), compared to UC. Both acupuncture groups had sizable decreases in NRS: Pain Best, compared to UC (TCA versus UC: P = 0.0008, d = 1.70; AA versus UC: P = 0.0127, d = 1.6; (Table 2). Similar results emerged when both acupuncture groups were combined; there were significant between group differences in the combined acupuncture group versus UC in three of the global pain measures (NRS Pain Now, P = 0.0021; NRS Pain Usual, P = 0.0153; NRS Pain Best, P = 0.0004; Table 2).
There were no statistically significant results in any other secondary outcome measure, including depression, anxiety, somatic dysfunction, physical/psychologic functioning, cognitive function, or sleep (Table 2). Daily headache pain and prescription medication use could not be analyzed as only 25% (n = 6) of participants had maintained their daily headache entries consistently. Group differences were not calculated for HAM-A and HAM-D because of the small sample sizes at baseline and week 6.
For the ANAM, only two subset scores showed marginally significant between-group differences from baseline to Week 6 (Simple Reaction Time Repeated throughput score P = 0.0256 and throughput standard score P = 0.0263). These two scores are essentially equivalent as they measure the same construct in different ways. Mean Simple Reaction Time Repeated throughput score decreased by −10.8% in TCA, increased by 42.6% in AA, and increased by 13.2% in UC. The throughput measure is the number of correct responses in a set time interval and measures both speed and accuracy. Therefore, the AA group's larger increase suggests that this group had a performance improvement. Mean Simple Reaction Time Repeated standard score decreased by 11.1% in the TCA group, increased by 54.8% in the AA group, and increased by 17.3% in the UC group. There were similar results when acupuncture groups were combined (data not shown).
Additional analyses
Pretreatment expectations
At a single timepoint (baseline prior to randomization), participants were asked to rate their expectations about (1) headache improvement (i.e., if they expected their headaches to improve over the course of the 6-week study) and (2) acupuncture effectiveness (i.e., if they believed that acupuncture would be effective for relieving their headaches) on an 11-point Likert scale. The majority of participants (62.8%) had moderate-to-high expectation (>5) that their headaches would improve while on-study. A higher proportion (83.7%) expressed a moderate-to-high expectation (>5) that acupuncture would be helpful for relieving their headaches. When baseline expectations were analyzed after study completion, expectations of headache improvement and acupuncture effectiveness were highly correlated (r = 0.679). Expectations of headache improvement and acupuncture effectiveness were moderately correlated with pre–post differences in usual pain (r = –0.464 for “expectation of headache improvement,” n = 26, P = 0.017; and r = –0.422 for “acupuncture effectiveness,” n = 26, P = 0.032) and sleep quality (r = –0.470, n = 28, P = 0.0112; and r = –0.498, n = 28; P = 0.007, respectively; Table 3). There were no other correlations with any other outcome measures (data not shown).
Table 3.
Correlation Matrix for Expectancy
| Measure | Headache improvement | Acupuncture effectiveness | HIT | NRS: Pain Usual | NRS: Pain Now | NRS: Pain Best | NRS: Pain Worst | PSQI |
|---|---|---|---|---|---|---|---|---|
| Headache improvement | − | 0.679§ | −0.289 | −0.464* | −0.223 | −0.164 | −0.217 | −0.470* |
| Acupuncture effectiveness | 0.679* | − | −0.067 | −0.422* | −0.261 | −0.365 | −0.193 | −0.498* |
P < 0.05.
HIT, Headache Impact Test; NRS, Numerical Rating Scale; PSQI, Pittsburgh Sleep Quality Index.
The association was checked, using a RMANOVA of expectancy and randomization group as the independent variables and outcome measures as the dependent variables. In this RMANOVA, while holding both expectancy variables constant, there were significant time by group interactions among the following outcome measures: HIT (F(2.23) = 4.78, P = 0.018); NRS: Pain Now (F(2.23) = 4.22, P = 0.028); NRS: Pain Usual (F(2.21) = 4.02, P = 0.033); and NRS: Pain Best (F(2.23) = 3.78, P = 0.039). Both acupuncture treatment groups improved more in pain-related measures than the UC group. There were no significant expectancy by time interaction effects for these outcome measures; that is, when holding the treatment groups constant, improvements in pain-related measures were not associated with expectation. However, there were significant between-group expectancy effects on PSQI scores; that is, study participants who had higher baseline expectancy of both headache improvement and acupuncture effectiveness experienced better sleep.
Changes in headache pain during treatment visits
Participants randomized to an acupuncture treatment group rated their headache pain immediately prior to and after each acupuncture treatment session. Both TCA and AA groups experienced immediate decreases in treatment-related headache pain at each visit (NRS change for TCA: mean −1.66; AA: mean −0.99); however, the mean pre–post change in treatment-related headache pain was significantly better in the TCA than in the AA group (P < 0.0001; Table 4).
Table 4.
Mean Pretreatment and Post-Treatment Differences by Treatment Group
| Group | Pretreatment pain | Post-treatment pain | Mean diff | P-value |
|---|---|---|---|---|
| TCA | 3.94 | 2.31 | −1.66 | <0.0001 |
| AA | 3.37 | 2.45 | −0.99 |
Diff, difference; TCA, traditional Chinese acupuncture; AA, auricular acupuncture.
Adverse Events
A total of 11 adverse events (AEs) occurred in seven study participants (Tables 5A-B). Two AEs were unrelated to acupuncture intervention (i.e., hand injury due to accident, contact dermatitis after poison sumac exposure). Of the remaining nine AEs that were at least possibly related to acupuncture, all were expected AEs (i.e., documented in the protocol and ICD as having previously occurred in the literature), and none were serious AEs.
Table 5A.
Summary of Adverse Events
| Summary of adverse events* | AA | TCA |
|---|---|---|
| Increased headache pain | 3 | 1 |
| Bleeding at needle site | 1 | − |
| Migraine headache after acupuncture treatment | 1 | − |
| Pain at needle site | − | 2 |
| Muscle contraction after needling | − | 1 |
| Total | 5 | 4 |
All adverse events were expected and none were serious.
AA, auricular acupuncture; TCA, traditional Chinese acupuncture.
Table 5B.
Description of Adverse Events at Least Possibly Related to Acupuncture Treatment
| Treatment group/participant # | Adverse event | Adverse event description |
|---|---|---|
| AA/1 | Slight bleeding | Outer ear at ASP needle site |
| AA/2 | Increased HA pain | HA pain increased from 4/10 to 5/10 during Rx with ASP needles |
| AA/3 | Increased HA pain | HA pain increased from 3/10 to 4/10 during Rx with ASP needles at Rx visit 2 |
| AA/3 | Increased HA pain | HA pain from 4/10 to 5/10 during Rx with ASP needles at Rx visit 4 |
| AA/3 | Migraine HA | Migraine HA after Rx visit 7 |
| TCA/1 | Pain at acupuncture needle insertion site | Pain at SP 3* at Rx visit 6 |
| TCA/1 | Pain at acupuncture needle insertion site | Finer needle used at SP 3 at Rx visit 8 |
| TCA/1 | Uncomfortable muscle contractions following needle placement | See narrative (Rx visit 9) |
| TCA/2 | Increased HA pain | HA pain increased from 4/10 to 5/10 during Rx |
Acupuncture point: Spleen meridian.
AA, Auricular acupuncture; TCA, traditional Chinese acupuncture; HA, headache; ASP, Aiguille Semi-Permanente; Rx; treatment.
Five AEs occurred in 3 participants in the AA group, including three episodes of mild increase in headache pain immediately following the placement of ASP needles (by 1 point on the 10-point Likert scale), and 1 report of a migraine headache after completion of the AA treatment. In all cases, participants were monitored closely and symptoms resolved without any intervention. On subsequent visits, specific needle placement was either withheld or the position was adjusted. No participants withdrew study participation as a result of these AEs. Four AEs occurred in 2 participants among the TCA study participants. These included two episodes of pain at a specific acupuncture needle insertion site (SP 3) and an increase in headache-related pain after placement of acupuncture needles in Ah Shi points at the base of the occiput. In all cases, subsequent treatments were adjusted with a finer needle, or if no improvement was noted, withholding needle placement at that site.
Discussion
Challenges and Limitations
A number of challenges were encountered during the course of this study that prevented us from reaching our anticipated enrollment goals. First, this acupuncture study was conducted during the height of the OEF/OIF/OND conflicts at MTFs in which many Service members were being treated for multiple traumas. Consequently, the severity of their injuries precluded them from being eligible for the study; 54% of Service members who were referred did not meet the study eligibility criteria, often because of complicating injuries. Another unexpected occurrence was that Service members who were treated for their TBI-related injuries at WRNMMC were not from the Washington, DC, area. Once they were medically stable, they returned home. Thus, it was not always possible to conduct the follow-up at the 12-week timepoint. Moreover, once enrolled on-study, it was difficult to schedule multiple study-related visits because most injured Service members were receiving care from multidisciplinary teams (i.e., Physical Medicine and Rehabilitation, Neurology, Physical Therapy, Occupational Therapy, Social Work). Enrolling in an interventional acupuncture study was not viewed by many clinical healthcare providers as a priority, given the more imminent clinical care needs of this patient population.
Another challenge encountered was institutional policies that changed over the course of this study. Licensed acupuncturists who performed all acupuncture interventions needed to obtain limited privileges through hospital credentialing departments in order to administer the study interventions. Over the course of the study, one of the institutions changed its credentialing policies and ceased providing licensed acupuncturists (i.e., who were not physicians) with limited privileges. Although licensed acupuncturists had previously been allowed to deliver acupuncture in the context of IRB-approved research studies, the mechanism to provide nonphysician acupuncturists with limited privileges was rescinded. As a result of this decision, enrollment ceased at that site. At the other site, a contract acupuncturist was hired and consequently, Service members could obtain acupuncture clinically—a circumstance that competed with study enrollment.
A second institutional change that occurred during this study was a Defense BRAC, which required changing geographic sites; during this transition period, it was not possible to enroll study participants until new IRB approval could be obtained. Despite these obstacles, the authors were able to enroll 45 participants in the study successfully.
There was an additional limitation. The number of participants who completed the outcome measures at study completion (week 6, n = 29, 64%) and follow-up (week 12, n = 22, 49%) created smaller than expected sample sizes, limiting the ability to draw definitive conclusions from the statistical analyses. While attempts were made to match both acupuncture intervention groups for equivalent clinician time and attention, the TCA group had a longer treatment time than the AA group (average, 60 minutes versus 45 minutes, respectively). This time was required for the acupuncturist to ask questions based on TCA theory to determine placement of the needles at each visit. This additional time and interaction with the acupuncturists could have affected the type of nonspecific care that patients in this group received and influenced their expectation of benefit, as could have possible differences in clinician contact time with the UC group.
Generalizability
Both AA and TCA had a larger impact on TBI-associated headaches than UC alone. Both acupuncture groups experienced headache improvement during treatment sessions (favoring TCA over AA during sessions) and over the duration of the study, compared to UC alone. AA is a more feasible intervention approach to integrate into MTF settings for TBI-related headache at this time. This is because of AA's ease of training, no need to have formal acupuncture knowledge to deliver, shorter time of administration, and flexibility for use in a variety of settings. This study could not determine which approach provided better long-term effects (past the treatment period) or a wider benefit for other TSR symptoms.
Interpretation
A mean positive difference of 7.03 was found in HIT scores in participants who received AA and there was a 3.53 difference for participants who received TCA, compared to UC. Combining acupuncture groups revealed a mean HIT score difference of 5.2 over UC. According to Coeytaux and colleagues who investigated the minimum important difference (MID) in patients with chronic daily headache, a between-group difference in HIT change scores of 2.3 units over time reflects a clinically significant headache improvement.38 Thus, acupuncture resulted in both statistically substantial and clinically meaningful benefits as measured by the HIT.
Both the TCA and AA groups in the current study experienced immediate improvement in headache pain during the course of acupuncture treatment visits, with the TCA group showing a significant mean decrease in headache pain, compared with AA. When the two acupuncture groups were compared to UC, AA showed significant improvements in HIT scores that were greater than those of TCA over the course of the study period. In summary, both acupuncture approaches decreased pain better than UC alone immediately post-treatment and over the course of the study; however, the AA group's headache outcomes were sustained more over the study period, while TCA had a larger effect immediately following the treatment.
Conclusions
This exploratory study endeavored to determine the feasibility and comparative effectiveness of two acupuncture methods to improve headache-related QoL in Service members with headaches related to TBI. The two acupuncture methods used in this study were an AA protocol that followed an algorithmic approach based on pain-symptom responses and a TCA protocol that was tailored to each participant's unique headache patterns and constitutional types. Participants in both acupuncture groups had improvements in HIT scores, compared to a UC-only group. However, headache-related QoL was greater in the AA group (Cohen's d = 1.28) than in the TCA group (d = 0.72), while treatment-specific headache pain improved more during TCA than in AA treatment sessions (NRS change for TCA: mean −1.66; AA: mean −0.99).
Secondary goals of this study were to evaluate if there were differential effects between the two acupuncture methods on trauma-related symptoms, including global pain; PTSD; anxiety; depression; sleep; and cognitive, mental and physical functioning. It was hypothesized that, compared to UC, participants receiving TCA would have more systemic symptom-based improvements than participants receiving AA. This hypothesis was not confirmed. The only secondary outcomes that showed significant between-group differences from baseline to week 6 were measures of global pain; both the TCA and AA groups experienced substantial improvements in current pain (NRS: Pain Now, NRS: Pain Best) and the TCA group in usual pain (NRS: Usual Pain). There were no other significant improvements in secondary outcomes. The sample sizes for these outcomes were likely too low to test this hypothesis adequately in this feasibility study.
In the analysis of pretreatment expectations, it was found that the majority of study participants had moderate-to-high expectation that they would experience headache improvement or acupuncture effectiveness while on-study. However, in a repeated-measure analysis, it was found that, while expectation had an effect on positive responses in select headache and pain variables, expectancy was not a major factor in explaining these responses. It was also found that both the TCA and AA groups experienced decreased headache pain during acupuncture treatment visits, with TCA participants experiencing significantly better treatment-related headache relief. The nine adverse events that were at least possibly related to acupuncture were mild, expected, and resolved either without intervention or with needle-site adjustment.
In this small exploratory study, AA and TCA acupuncture improved headache-related QoL more than UC in Service members with TBI and resulted in only a few minor adverse effects. While larger studies are needed to confirm these findings, when the data from this study are considered with other research on acupuncture, headaches and PTSD, this study supports the use of acupuncture as a part of standard care for treatment of the TSR.39
Appendix 1. Auricular Acupuncture Protocol
If initial headache is 0 or 1 on a 10-point Likert Scale, insert SEIRIN® needles bilaterally into Omega 2, Shen Men, and Point Zero for 30 minutes, then replace the needles in the same three sites with gold Aiguille Semi-Permanente (ASP) needles and discharge the patient to go home with instructions. Otherwise, if initial headache pain is 2–10, insert SEIRIN needle into the N point for 1 minute and reassess pain. If the headache decreases to 0 or 1 after 1 minute, leave needles in for another 15 minutes, then insert three gold ASP needles bilaterally in Omega 2, Shen Men, and Point Zero, and discharge the patient to go home with instructions. If the N point fails to resolve the headache after 1 minute (i.e., pain is 2–10), remove the N needle and insert SEIRIN needles bilaterally into Omega 2, Shen Men, and Point Zero for 15 minutes. If the headache decreases to 0–1, remove the SEIRIN needles and insert gold ASP needles bilaterally in Omega 2, Shen Men, and Point Zero, and discharge the patient to go home with instructions. If the headache persists (i.e., pain is 2–10) or there is nausea, remove SEIRIN needles and insert gold ASP needles bilaterally into Omega 2, Shen Men, Point Zero, Cingulate Gyrus, and External Thalamus points, and discharge the patient to go home with instructions. All participants are instructed to remove the indwelling ASP needles after 3 days, or sooner if pain or redness develops at a needle site.
Appendix 2. Traditional Chinese Acupuncture Points’ Selection
Primary and Secondary Headache Patterns
Determination of primary and secondary patterns will be based on the acupuncturist's clinical assessment of the relationship between patterns and respective weight of the signs and symptoms. Point selection will be derived from the following list of points associated with their pattern diagnoses.
| Primary and secondary headache pattern | Potential acupuncture points |
|---|---|
| Blood Stasis | LI 11, LI 4, SP 6, Liv 3; Ah Shi points |
| Liver Fire | Liv 2, SP 6, TB 5, GB 38, GB 20, Tai Yang Optional:GB 43, GB 44, LI 11 Local points: GB 4, GB 8, GB 9, GB 13, GB 14, BL 2, Yuyao, GB 1, GB 20, Optional:GB 21 |
| Liver Wind | Liv 3, SP 6, GB 20, DU 16, DU 20 |
| Liver Qi Stagnation | Liv 3, GB 34, LI 4, ST 36, DU 24, Tai Yang Optional:Liv 14, Yintang |
| Wind Damp | Lu 7, LI 6, SP 6, ST 8, DU 23 |
| Liver Yang Rising with Phlegm in Head | Liv 3, GB 20, DU 16, Liv 8, KI 3, LI 4, ST 40, CV 9, SP 9, ST 8, CV 12, GB 20, BL 20 |
| Stagnation of Cold in Liver Channel | LI 3 with moxa, DU 20 |
| Liver Yang Rising | Liv 3, Liv 8, SP 6, TB 5, Tai Yang, GB 20 Optional:KI 3 Distal points: P 6, LU 7, GB 43 Local points: GB 4, GB 5, GB 6, GB 8, GB 9, GB 13, GB 14, BL 2, Yuyao, GB 1 |
| Blood Deficiency | ST 36, SP 6, Liv 8, Ren 4, HT 5, BL 20, DU 20 |
| Qi Deficiency | ST 36, Ren 6, SP 6, GV 20 |
| Kidney Yin Deficiency | KI 3, ST 36, SP 6, Ren 4; GV 20, GB 19 |
| Kidney Yang Deficiency | KI 3, ST 36, SP 6, Ren 4, GV 20, GB 19, BL 23 with moxa |
Constitutional Type
| Water | BL 64, KI 3; plus 2 additional Constitution/Personality points |
| Wood | LI 3, GB 40; plus 2 additional Constitution/Personality points |
| Fire | PC 7, TB 4 or HT 7, SI 4; plus 2 additional Constitution/Personality points |
| Earth | ST 42, SP 3; plus 2 additional Constitution/Personality points |
| Metal | LU 9, CO 4; plus 2 additional Constitution/Personality points |
Constitution/Personality or Character Type Points
| • HT 1 | • BL 20 | • KI 22 | • TB 22 | • LI 20 |
| • HT 7 | • BL 23 | • KI 23 | • GB 1 | • ST 1 |
| • HT 9 | • BL 42 | • KI 24 | • GB 40 | • ST 42 |
| • SI 1 | • BL 43 | • KI 25 | • GB 41 | • SP 1 |
| • SI 4 | • BL 44 | • KI 26 | • Liv 1 | • SP 3 |
| • SI 19 | • BL 47 | • KI 27 | • Liv 3 | • SP 21 |
| • BL 1 | • BL 48 | • PC 1/2 | • Liv 14 | • CV 17 |
| • BL 13 | • BL 64 | • PC 7 | • LU 1 | |
| • BL 14 | • BL 67 | • PC 8 | • LU 7 | |
| • BL 15 | • KI 1 | • TB 1 | • LU 9 | |
| • BL 18 | • KI 3 | • TB 4 | • LI 4 |
Acknowledgments
The authors would like to acknowledge the study's coordinators, Ms. Alex York, MS, Ms. Meghan O'Connell, MS, and Ms. Jennifer Smith, MA, as well as the study's acupuncturists, Ms. Sarah Petty, MAc, LAc, DiplAc and Ms. Stephanie Brown, MAc, LAc, DiplAc.
Author Disclosure Statement
The authors declare that there is no conflict of interest regarding the publication of this paper. The authors have not presented this data and information before in any journal or presentation and have no professional relationships with companies or manufacturers who will benefit from the results of this present study.
CME Quiz Questions
Article Learning Objectives:
After studying this article, participants should be able to identify various methods of evaluating symptoms of the Trauma Spectrum Response (TSR) in a military Service member population; critically evaluate the effectiveness of the two acupuncture methods presented in the management of TBI related headaches and co‐morbid symptoms associated with TBI; and utilize outcomes of this exploratory study to consider acupuncture headache interventions in the TBI population.
Publication date: June 6, 2016
Expiration date: June 30, 2017
Disclosure Information:
Authors have nothing to disclose.
Richard C. Niemtzow, MD, PhD, MPH, Editor‐in‐Chief, has nothing to disclose.
Online CME Questions:
-
1. Identify one statement below that was not a central hypothesis of this study:
a) Co‐morbid symptoms would improve more in a favorable direction in both acupuncture groups as compared with the usual care (UC) group.
b) Both acupuncture methods would reduce headache severity as compared with the UC group.
c) Both acupuncture methods would reduce headache frequency as compared with UC group.
d) Both acupuncture methods would improve headache related quality of life as compared with UC group.
e) Co‐morbid symptoms would improve more in a favorable direction in the Traditional Chinese Acupuncture (TCA) group as compared with Auricular Acupuncture (AA) group.
-
2. This exploratory study sought to determine whether acupuncture methods were more effective than usual care (UC) for TBI in several areas. Choose one investigation method that was not utilized:
a) Headache Impact Test (HIT)
b) Post Traumatic Stress Checklist – Civilian Version (PCL‐C)
c) Neurobehavioral Symptom Inventory (NSI)
d) Measuring headache frequency and severity
e) Measuring possible improvements in headache ‐ related quality of life
-
3. Choose the one most correct statement regarding the study design:
a) Follow up assessments were made on all available study participants at 6 weeks, 12 weeks, and 18 weeks following entry into the study.
b) Service members were ineligible for the study if they had received acupuncture within the past four months.
c) The initial TCM assessment was performed on all participants before the randomization into the Traditional Chinese Acupuncture (TCA), Auricular Acupuncture (AA), or usual care (UC) group.
d) Those randomized to UC only were offered an option of receiving auricular acupuncture following the 6 week study period.
e) To provide a consistent contextual approach to all three branches of this study, UC participants were given a series of weekly appointments during the study period at each Military Training Facility (MTF) with the treatment focus on fostering a sense of control and empowerment.
-
4. In consideration of the acupuncture protocols utilized, choose the one statement below that is not true:
a) Twelve distinct Traditional Chinese Acupuncture (TCA) headache patterns were identified to assist in personalizing acupuncture point selection.
b) The TCA protocol utilized points that corresponded to the participant's constitutional points as well as their Ah‐Shi points.
c) Both TCA and Auricular Acupuncture (AA) protocols offered ten treatments over a six‐week time period.
d) The AA protocol included Cingulate Gyrus and External Thalamus points if the patient presented with nausea.
e) For initial headache pain of two to ten on the 10‐point Likert Scale, gold ASP needles were used at the N points and participants were instructed to remove the in‐dwelling needles after three days.
-
5. Choose the one statement below that is not a valid finding of this study:
a) Significantly more adverse events occurred in the Traditional Chinese Acupuncture (TCA) group compared with the Auricular Acupuncture (AA) group, primarily including headache exacerbation in response to treatment.
b) Headache Impact Test (HIT) scores decreased by week 6 in both acupuncture intervention groups indicating an improvement in quality of life as compared with the usual care (UC) group.
c) Daily headache pain and prescription medication use could not be analyzed as only 25% of participants maintained their daily headache entries consistently.
d) The Numerical Rating Scale (NRS) showed a significant improvement in response to both acupuncture intervention groups compared with the UC group.
e) When baseline expectations were analyzed after study completion, expectations of headache improvement and acupuncture effectiveness were highly correlated.
Continuing Medical Education – Journal Based CME Objectives:
Articles in Medical Acupuncture will focus on acupuncture research through controlled studies (comparative effectiveness or randomized trials); provide systematic reviews and meta‐analysis of existing systematic reviews of acupuncture research and provide basic education on how to perform various types and styles of acupuncture. Participants in this journal‐based CME activity should be able to demonstrate increased understanding of the material specific to the article featured and be able to apply relevant information to clinical practice.
CME Credit
You may earn CME credit by reading the CME‐designated article in this issue of Medical Acupuncture and taking the quiz online. A score of 75% is required to receive CME credit. To complete the CME quiz online, go to http://www.medicalacupuncture.org/cme – AAMA members will need to login to their member account. Non‐members have the opportunity to participate for a small fee.
Accreditation: The American Academy of Medical Acupuncture is accredited by the Accreditation Council for Continuing Medical Education (ACCME).
Designation: The AAMA designates this journal‐based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
References
- 1.Cifu DX, Taylor BC, Carne WF, Bidelspach D, Sayer NA, Scholten J, Campbell EH. Traumatic brain injury, posttraumatic stress disorder, and pain diagnoses in OIF/OEF/OND Veterans. J Rehabil Res Dev. 2013;50(9):1169–1176 [DOI] [PubMed] [Google Scholar]
- 2.Terrio H, Brenner LA, Ivins BJ, et al. Traumatic brain injury screening: Preliminary findings in a US Army Brigade Combat Team. J Head Trauma Rehabil. 2009;24(1):14–23 [DOI] [PubMed] [Google Scholar]
- 3.Defense and Veterans Brain Injury Center. DoD Worldwide Numbers for TBI. Online document at: http://dvbic.dcoe.mil/dod-worldwide-numbers-tbi (Accessed May27, 2016).
- 4.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. Soldiers returning from Iraq. N Engl J Med. 2008;358(5):453–463 [DOI] [PubMed] [Google Scholar]
- 5.Gironda RJ, Clark ME, Ruff RL, Chait S, Craine M, Walker R, Scholten J. Traumatic brain injury, polytrauma, and pain: Challenges and treatment strategies for the polytrauma rehabilitation. Rehabil Psychol. 2009;54(3):247–258 [DOI] [PubMed] [Google Scholar]
- 6.Jonas WB, Walter JAG, Fritts M, Niemtzow RC. Acupuncture for the trauma spectrum response: Scientific foundations, challenges to implementation. Med Acupunct. 2011;23(4):249–262 [Google Scholar]
- 7.Shen J. Research on the neurophysiological mechanisms of acupuncture. Review of selected studies and methodological issues. J Altern Complement Med. 2001;7(suppl1):S121–S127 [DOI] [PubMed] [Google Scholar]
- 8.Coeytaux RR, Kaufman JS, Kaptchuk TJ, Chen W, Miller WC, Callahan LF, Mann JD. A randomized, controlled trial of acupuncture for chronic daily headache. Headache. 2005;45(9):1113–1123 [DOI] [PubMed] [Google Scholar]
- 9.Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for tension-type headache. Cochrane Database Syst Rev. 2009;1:CD007587; update in: Linde K, Allais G, Brinkhause B, et al. Acupuncture for the prevention of tension-type headache. Cochrane Database Syst Rev. 2016;4: CD007587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for migraine prophylaxis. Cochrane Database of Systematic Reviews. 2009;1:CD001218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Da Silva AN. Acupuncture for migraine prevention. Headache. 2015;55(3):470–473 [DOI] [PubMed] [Google Scholar]
- 12.Khusid MA. Clinical indications for acupuncture in chronic post-traumatic headache management. Mil Med. 2015;18(2):132–136 [DOI] [PubMed] [Google Scholar]
- 13.Cao WS, Qin YX, Hou QX. Acupuncture combined with hyperbaric oxygen treatment for post-traumatic brain injury syndrome [Chinese]. Modern Rehabil 2001;5(8):110. [Google Scholar]
- 14.Kalavapalli R, Singareddy R. Role of acupuncture in the treatment of insomnia: A comprehensive review. Complement Ther Clin Pract. 2007;13(3):184–193 [DOI] [PubMed] [Google Scholar]
- 15.Pilkington K, Kirkwood G, Rampes H, Cummings M, Richardson J. Acupuncture for anxiety and anxiety disorders—a systematic literature review. Acupunct Med. 2007;25(1–2):1–10 [DOI] [PubMed] [Google Scholar]
- 16.Manber R, Schnyer RN, Allen JJ, Rush AJ, Blasey CM. Acupuncture: A promising treatment for depression during pregnancy. J Affect Disord. 2004;83(1):89–95 [DOI] [PubMed] [Google Scholar]
- 17.Smith CA, Hay PP. Acupuncture for depression. Cochrane Database Syst Rev. 2005;2:CD004046. [DOI] [PubMed] [Google Scholar]
- 18.Sniezek DP, Siddigui IJ. Acupuncture for treating anxiety and depression in women: A clinical systematic review. Med Acupunct. 2013;25(3):164–172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan YY, Lo WY, Yang SN, Chen YH, Lin JG. The benefit of combined acupuncture and antidepressant medication for depression: A systematic review and meta-analysis. J Affect Disord. 2015;176:106–117 [DOI] [PubMed] [Google Scholar]
- 20.Wheway J, Agbabiaka TB, Ernst E. Patient safety incidents from acupuncture treatments: A review of reports to the National Patient Safety Agency. Int J Risk Saf Med. 2012;24(3):163–169 [DOI] [PubMed] [Google Scholar]
- 21.Lee JH, Choi TY, Lee MS, Lee H, Shin BC, Lee H. Acupuncture for acute low back pain: A systematic review. Clin J Pain. 2013;29(2):172–185 [DOI] [PubMed] [Google Scholar]
- 22.Liu L, Skinner M, McDonough S, Mabire L, Baxter GD. Acupuncture for low back pain: An overview of systematic reviews. Evid Based Complement Alternat Med. 2015;2015:328196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Engel CC, Cordova EH, Benedek DM, et al. Randomized effectiveness trial of a brief course of acupuncture for posttraumatic stress disorder. Med Care. 2014;52(12[suppl5]):S57–S64 [DOI] [PubMed] [Google Scholar]
- 24.Barker R, Kober A, Hoerauf K, Latzke D, Adel S, Kain ZN, Wang SM. Out-of-hospital auricular acupressure in elder patients with hip fracture: A randomized double-blinded trial. Acad Emerg Med. 2006;13(1):19–23 [DOI] [PubMed] [Google Scholar]
- 25.Domingo C. Introduction to Chinese traditional medicine and acupuncture: Energy-balancing therapeutic method [in Spanish]. Rev Enferm. 2001;24(10):50–52 [PubMed] [Google Scholar]
- 26.Department of Veterans Affairs (VA), Department of Defense (DoD) eds. VA/DoD Clinical Practice Guideline for Management of Concussion/Mild Traumatic Brain Injury. Washington DC: The Management of Concussion/mTBI Working Group; 2009. Online document at: www.academia.edu/23833995/Clinical_practice_guideline_Management_of_Concussion_Mild_Traumatic_Brain_Injury Accessed May18, 2016. [Google Scholar]
- 27.Niemtzow RC, Gambel J, Helms J, Pock A, Burns SM, Baxter J. Integrating ear and scalp acupuncture techniques into the care of blast-injured United States military service members with limb loss. J Altern Complement Med. 2006;12(7):596–599 [DOI] [PubMed] [Google Scholar]
- 28.Hollifield M, Sinclair-Lian N, Warner TD, Hammerschlag R. Acupuncture for posttraumatic stress disorder: A randomized controlled pilot trial. J Nerv Ment Dis. 2007;195(6):504–513 [DOI] [PubMed] [Google Scholar]
- 29.Defense and Veterans Brain Injury Center. Updated Mild Traumatic Brain Injury (mTBI): Clinical Guidance
- 30.Bayliss M, Battenhorst A. The HIT-6™: A User's Guide. Lincoln, RI: QualityMetric Incorporated; 2002 [Google Scholar]
- 31.Coeytaux RR, Kaufman JS, Kaptchuk TJ, Chen W, Miller WC, Callahan LF, Mann JD. A randomized, controlled trial of acupuncture for chronic daily headache. Headache. 2005;45(9):1113–1123 [DOI] [PubMed] [Google Scholar]
- 32.Ferraz MB, Quaresma MR, Aquino LR, Atra E, Tugwell P, Goldsmith CH. Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol. 1990;17(8):1022–1024 [PubMed] [Google Scholar]
- 33.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213 [DOI] [PubMed] [Google Scholar]
- 34.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther. 1996;34(8):669–673 [DOI] [PubMed] [Google Scholar]
- 35.Dasgupta A, Lawson KA, Wilson JP. Evaluating equivalence and noninferiority trials. Am J Health Syst Pharm. 2010;67(16):1337–1343 [DOI] [PubMed] [Google Scholar]
- 36.Wasserstein RL, Lazar NA. The ASA's statement on p-values: Context, process, and purpose. Am Statist. 2016;March 7:e-pub ahead of print [Google Scholar]
- 37.Kadel RP, Kip KE. A SAS macro to compute effect size (Cohen's d) and its confidence interval from raw survey data [presentation]. Annual SouthEast SAS Users Group Conference, Raleigh/Durham, NC, October 14–16, 2012 [Google Scholar]
- 38.Coeytaux RR, Kaufman JS, Chao R, Mann JD, Devellis RF. Four methods of estimating the minimal important difference score were compared to establish a clinically significant change in Headache Impact Test. J Clin Epidemiol. 2006;59(4):374–380 [DOI] [PubMed] [Google Scholar]
- 39.Lee C, Crawford C, Wallerstedt D, et al. The effectiveness of acupuncture research across components of the trauma spectrum response (TSR): A systematic review of reviews. Syst Rev. 2012;1:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
To receive CME credit, you must complete the quiz online at: www.medicalacupuncture.org/cme