Abstract
Purpose:
To describe an unusual retinal manifestation of dengue fever in an endemic region.
Case Report:
A 35 year old male presenting with acute onset decreased vision in his right eye, was found to have a massive retinal pigment epithelial detachment (PED) extending up to the vascular arcades. He had been diagnosed with acute hypokalemic quadriparesis in dengue fever in the preceding week, which had resolved following treatment. The patient was managed conservatively. At three months follow up, there was spontaneous flattening of the PEDs with improvement in visual acuity.
Conclusion:
Dengue fever complicated by acute hypokalemic quadriparesis can be associated with PED, which can be large. The condition resolves spontaneously and bears a good prognosis.
Keywords: Dengue Fever, Flaccid Quadriparesis, Hypokalemia, Pigment Epithelial Detachment
INTRODUCTION
Dengue is a major public health problem in the tropics and subtropics.[1] Ocular involvement in dengue fever is uncommon.[2,3] Herein, we describe a young man diagnosed with acute hypokalemic quadriparesis due to dengue infection, who presented with unilateral visual impairment and was found to have massive retinal pigment epithelial detachment (PED).
CASE REPORT
A 35-year-old man presented with sudden-onset decreased vision in his right eye since 5 days before. One week earlier, he had presented to the medical emergency with high grade fever and progressive weakness of all four limbs for 2 days. Based on blood investigations including a positive dengue NS1 antigen, a diagnosis of dengue fever with thrombocytopenia (platelet count 40,000/mm3) and hypokalemic acute flaccid motor paralysis was made. He was started on intravenous potassium chloride infusion. Within 8 hours, his motor power in all limbs improved significantly and serum potassium levels increased from 1.8 meq/liter at presentation, to 4.2 meq/liter by day 2 of treatment. He was discharged after one week of hospitalization, with no neurological sequelae, and presented to the ophthalmology department a few days later. There was no history of hypertension during this period.
On examination, best corrected visual acuity (BCVA) was 20/200 in the right and 20/20 in the left eye. Anterior segments of both eyes were unremarkable, with intraocular pressures measuring 16 mm Hg bilaterally. The pupillary reactions were normal. Fundus examination of the right eye showed a large PED occupying almost the entire macula with linear streaks of altered pigmentation on the surface [Figure 1a]. The left eye showed two PEDs [1b]. Fluorescein angiography (FA, VISUPAC and FF450 plus, Carl Zeiss Meditec, Inc., Dublin, California, USA) demonstrated intense hyperfluorescence from pooling of dye in the PEDs [Figure 1c and d]. Hypofluorescence was seen corresponding to the linear streaks on the surface of the PED in the right eye. In addition, another small PED was noted superotemporal to the disc in the right eye. Spectral domain optical coherence tomography (SD-OCT, RTVue, Optovue Inc., Fremont, California, USA) confirmed the serous nature of the PEDs [Figure 1e and f]. The massive PED in the right eye also showed a pocket of subretinal fluid at its apex and retinal pigment epithelium (RPE) heaping in the area of the linear streaks.
Figure 1.
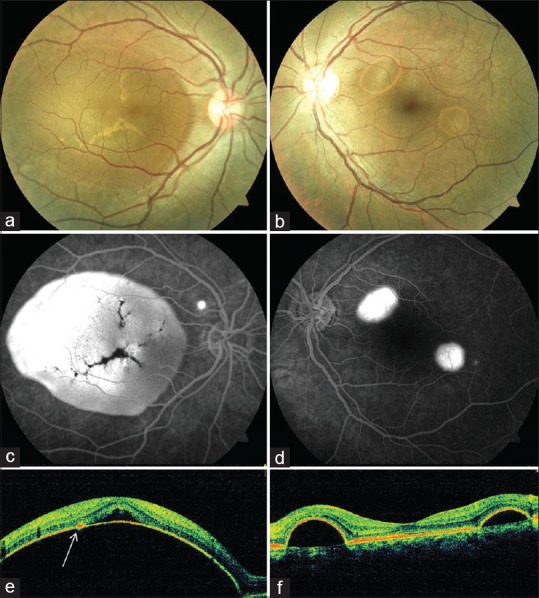
Fundus findings at presentation. Massive pigment epithelial detachment (PED) occupying the right macula (a) and two small PEDs in the left eye (b). Fluorescein angiography (c and d) show pooling with hypofluorescent streaks corresponding to altered pigmentation on the PED surface in the right eye (c). Spectral domain optical coherence tomography demonstrates serous PEDs (e and f); PED in the right eye had subretinal fluid at its apex with retinal pigment epithelium hyperplasia (arrow).
The patient was a nonsmoker and had no history of steroid intake in any form. Blood pressure monitoring was within normal range. Repeat hemogram including platelet count, serum electrolytes, renal and liver function tests were within normal limits. A conservative approach was taken and the patient was advised to attend regular follow-up.
Three months following the acute presentation, BCVA in his right eye improved to 20/40 while that of the left eye was maintained at 20/20. Fundus examination showed the faint outline of the collapsed PED in the right eye with linear hypopigmented streaks in the vicinity of the fovea [Figure 2a]. FA showed window defects in the region previously occupied by the PED, with hypofluorescence due to the streaks. The small PED superotemporal to the disc persisted [Figure 2c]. Fundus examination in the left eye appeared unremarkable, however small window defects in the area of the PEDs were present on FA [Figure 2b and d]. SD-OCT confirmed flattening of the PEDs in both eyes with RPE hyperplasia corresponding to the streaks in the right eye [Figure 2e and f]. The patient was advised to maintain regular follow-up and self-check his vision using an Amsler grid.
Figure 2.
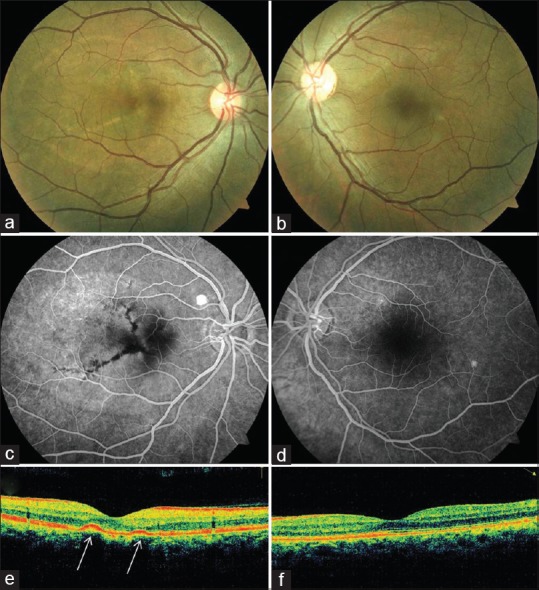
After 3 months, flattening of the pigment epithelial detachments (PEDs) was noted clinically (a and b), angiographically (c and d) and on spectral domain optical coherence tomography (e and f) (except one PED superotemporal to the right disc). In the right eye, linear streaks of altered pigmentation persisted, which blocked fluorescence and were likely retinal pigment epithelium hyperplasia (arrows).
DISCUSSION
The four serotypes of the dengue virus can cause a wide spectrum of diseases ranging from a nonspecific febrile illness to classic dengue fever, dengue hemorrhagic fever or dengue shock syndrome. Various atypical manifestations have also been recognized such as neurological involvement.[4] Acute neuromuscular weakness may occur in dengue due to myositis, Guillain– Barre syndrome or hypokalemia;[5,6] this remains an uncommonly described entity. The possible mechanism for development of hypokalaemia could be transient self-limited renal tubular defects secondary to infection leading to urinary potassium wasting or intracellular shift of potassium due to increased catecholamine levels in response to the stress of the infection and secondary insulin release.[6]
Dengue related ocular complications are uncommon; however, an increasing incidence has been reported over the past few years.[2,3,7] While several ocular features such as subconjunctival hemorrhages, intraretinal hemorrhages and Roth's spots are the manifestations of the thrombocytopenia and resultant bleeding diathesis; the presence of retinal vasculitis, macular edema, anterior uveitis and optic neuritis suggests that an inflammatory or immune-mediated pathophysiology may also be considered after acute dengue infections.[3,8] The prevalence of dengue maculopathy (macular swelling, yellow spots in the macula and macular hemorrhages) was found to be 10% among seropositive patients hospitalized for dengue fever during an epidemic by Su et al.[7] The onset of visual impairment usually occurs at the nadir of thrombocytopenia. Prognosis is generally good as the disease is often self-limited.[3]
Acute onset, reversible, pure motor quadriparesis complicating dengue fever was attributed to hypokalemia in our patient. Other causes of hypokalemia had been ruled out by clinical examination and appropriate investigations, and the patient demonstrated dramatic recovery with potassium supplementation. Visual complaints ensued on the 5th day of the illness. To the best of our knowledge, this is the first report of a large PED following dengue fever complicated by acute hypokalemic quadriparesis. There was spontaneous flattening of the PEDs by 3 months with improvement in BCVA. Considering the risk of choroidal neovascularization, the patient was kept on regular follow-up.
Although more commonly associated with serous retinal detachment, isolated PEDs can occur in systemic diseases with inflammatory, renal, hematologic or neoplastic origin.[9] While it may not be possible to attribute a single definitive pathophysiological basis for this occurrence, the putative mechanism for both the hypokalemia and the PEDs might be increased catecholamine levels due to the stress of the infection. Hyperactivity of the adrenomedullary system and elevated levels of catecholamines have been shown to play a role in the pathogenesis of idiopathic central serous chorioretinopathy.[10] Clinicians, especially in endemic areas, should be aware of such an association and its potential for spontaneous resolution.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Gubler DJ. Dengue and dengue hemorrhagic fever. Clin Microbiol Rev. 1998;11:480–496. doi: 10.1128/cmr.11.3.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lim WK, Mathur R, Koh A, Yeoh R, Chee SP. Ocular manifestations of dengue fever. Ophthalmology. 2004;111:2057–2064. doi: 10.1016/j.ophtha.2004.03.038. [DOI] [PubMed] [Google Scholar]
- 3.Chan DP, Teoh SC, Tan CS, Nah GK, Rajagopalan R, Prabhakaragupta MK, et al. Ophthalmic complications of dengue. Emerg Infect Dis. 2006;12:285–289. doi: 10.3201/eid1202.050274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gulati S, Maheshwari A. Atypical manifestations of dengue. Trop Med Int Health. 2007;12:1087–1095. doi: 10.1111/j.1365-3156.2007.01891.x. [DOI] [PubMed] [Google Scholar]
- 5.Hira HS, Kaur A, Shukla A. Acute neuromuscular weakness associated with dengue infection. J Neurosci Rural Pract. 2012;3:36–39. doi: 10.4103/0976-3147.91928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jha S, Ansari MK. Dengue infection causing acute hypokalemic quadriparesis. Neurol India. 2010;58:592–594. doi: 10.4103/0028-3886.68657. [DOI] [PubMed] [Google Scholar]
- 7.Su DH, Bacsal K, Chee SP, Flores JV, Lim WK, Cheng BC, et al. Prevalence of dengue maculopathy in patients hospitalized for dengue fever. Ophthalmology. 2007;114:1743–1747. doi: 10.1016/j.ophtha.2007.03.054. [DOI] [PubMed] [Google Scholar]
- 8.Wen KH, Sheu MM, Chung CB, Wang HZ, Chen CW. The ocular fundus findings in dengue fever. Gaoxiong Yi Xue Ke Xue Za Zhi. 1989;5:24–30. [PubMed] [Google Scholar]
- 9.Wolfensberger TJ, Tufail A. Systemic disorders associated with detachment of the neurosensory retina and retinal pigment epithelium. Curr Opin Ophthalmol. 2000;11:455–461. doi: 10.1097/00055735-200012000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Sun J, Tan J, Wang Z, Yang H, Zhu X, Li L. Effect of catecholamine on central serous chorioretinopathy. J Huazhong Univ Sci Technolog Med Sci. 2003;23:313–316. doi: 10.1007/BF02829525. [DOI] [PubMed] [Google Scholar]


