Abstract
The objective of this study was to develop methodologies for creating child–parent `links' in two healthcare-related data sources. We linked children and parents who were patients in a network of Oregon clinics with a shared electronic health record (EHR), using data that reported the child's emergency contact information or the `guarantor' for the child's visits. We also linked children and parents enrolled in the Oregon Health Plan (OHP; Oregon's public health insurance programs), using administrative data; here, we defined a `child' as aged <19 years and identified potential `parents' from among adults sharing the same OHP household identification (ID) number. In both data sources, parents had to be 12–55 years older than the child. We used OHP individual client ID and EHR patient ID numbers to assess the quality of our linkages through cross-validation. Of the 249,079 children in the EHR dataset, we identified 62,967 who had a `linkable' parent with patient information in the EHR. In the OHP data, 889,452 household IDs were assigned to at least one child; 525,578 with a household ID had a `linkable' parent (272,578 households). Cross-validation of linkages revealed 99.8 % of EHR links validated in OHP data and 97.7 % of OHP links validated in EHR data. The ability to link children and their parents in healthcare-related datasets will be useful to inform efforts to improve children's health. Thus, we developed strategies for linking children with their parents in an EHR and a public health insurance administrative dataset.
Keywords: Children, Electronic health records, Public health insurance, Family
Background
When parents have health insurance, their children are more likely to be insured and to receive guideline-appropriate health care [1–5]. Because of this strong association between coverage for parents and optimal health insurance and care for children, efforts to optimize children's health must be informed by coverage and health care services utilization data from both children and their parents [6–8]. Obtaining such family-level information requires the ability to link children with their parents in large healthcare-related databases.
In the past all family members were commonly covered under the same employer-sponsored health insurance plan [9], resulting in claims data that included information on all family members. Recent changes in family health insurance coverage patterns; however, make it harder to obtain coverage and utilization data with linkages between parents and their children. As employer-sponsored health plans have grown more expensive for families, fewer families have all members covered by the same insurance plan; discordant coverage within families has increased [10–13]. Children and parents are now commonly covered by different payers (e.g., parent has private coverage but child has public coverage), or some family members have coverage while others do not (e.g., child has public coverage but parent has no coverage) [14]. Even if both child and parent have some type of public coverage, administrative datasets rarely include mechanisms that enable `linking' a child to their parent.
The recent expansion of electronic health records (EHRs) present a new source of data on insurance coverage status and receipt of healthcare on multiple family members, if they receive care from the same provider (e.g., family physician), the same clinic, or group of clinics with a shared EHR [15, 16]. However, similar to the limited ability to link children with their parents in many state insurance administrative data systems [e.g., Medicaid and Children's Health Insurance Programs (CHIP)], few EHRs include a mechanism for linking children with their parents.
While data on individual patients has been linked across multiple datasets for various purposes [17–20], we know of no published methods for achieving linkages between children and their parents in EHR or public health insurance administrative data. This paper describes methodologies we developed for linking data on children and their parents within: (1) EHR data from Oregon clinics who are members of the OCHIN community health information network, and (2) administrative data from the Oregon Health Plan (OHP), which covers individuals enrolled in Oregon's Medicaid and CHIP programs.
Methods
Data Sources
OCHIN's EHR Data
OCHIN centrally hosts and maintains an EpicCare© EHR system that is shared among many community health centers [21]. (Originally called the Oregon Community Health Information Network, this organization is now “OCHIN, Inc.” as it has expanded members to >300 clinics in 16 states). Patients have a single health record accessible across all sites, and OCHIN maintains an EHR data warehouse with an enterprise-wide master patient index. This study utilized EHR data from clinics in the OCHIN network serving both children and adults in Oregon (141 clinics). OCHIN's comprehensive data warehouse has aggregate practice management data (e.g., appointments, diagnoses and procedures, similar to insurance claims data) and medical record data (e.g., problem lists, physician notes, prescription records, lab results, and referrals). The data are regularly checked and cleaned, and are stored in a central repository that can be searched electronically [22]. OCHIN's EHR is primarily used to support service delivery to individual patients at the point of care. Prior to our study, no mechanism was available for connecting children to their parents within the EHR data.
Oregon Health Plan Administrative Data
Oregon currently provides several public health insurance programs, most of which are operated by the OHP. Different programs have different eligibility criteria: for example, some children enroll via the CHIP, and others via Medicaid; pregnant women, children with special health care needs, low income adults, and disabled adults are all eligible to enroll in separate programs [23, 24]. Multiple family members may be enrolled in the OHP, yet each individual could join via different eligibility categories and/or at different times. Individuals can be tracked across programs via individual client identification (ID) numbers. OHP also identifies members of the same household with a household case ID number, but no family relationships are specified and thus, no mechanism is available to specifically identify and link children with their parents in OHP datasets.
Linkage Algorithm Descriptions
OCHIN's EHR Data
Potential child–parent links were limited to children and parents who were both patients at one of the 141 Oregon clinics in OCHIN's EHR network. Although requiring both children and parents to be patients limited the number of children whose parents we could identify, it yielded richer parent data (i.e., age, race/ethnicity, insurance status, medical diagnoses, past medical history, health care utilization patterns, etc.). Such parent-level data are necessary for analyses of how parental factors influence a child's access to insurance and receipt of health care services.
To link children with their parents in the OCHIN EHR data, we first identified children <18 years of age with at least one visit to an Oregon OCHIN clinic in 2002–2010. We chose <18 years of age because persons ≥18 are considered an adult in the OCHIN EHR. We used the only two EHR data fields containing information on an adult patient connected to a child patient to link parents and children—the `guarantor' and `emergency contact' fields.
OCHIN clinics use the guarantor field to identify the person responsible for paying for a given visit. The guarantor includes both an ID number and the type of relationship the adult has with the child. Specifically, the ID number is the patient ID of the OCHIN adult financially responsible for the child and the type of relationship includes possible familial relationships (e.g., parent, uncle, sister, etc.). Each OCHIN patient has only one patient ID, thus the ID found in the guarantor field matches to the patient record of the OCHIN adult financially responsible for the child. Twenty-six percent of the children identified in our sample had an adult OCHIN patient identified as their guarantor. OCHIN clinics also use an emergency contact field to identify a child's parent or guardian. This field was populated with an adult OCHIN patient for 5 % of the children in our sample. Approximately half of the children who had an emergency contact adult in their EHR data also had an adult guarantor listed; within this group, 99 % of the guarantor and emergency contact fields agreed on parental relationship. We excluded any potential child–parent link if the parent was not 12–55 years older than the child.
Oregon Health Plan Administrative Data
To identify child–parent links in the OHP administrative dataset, we used data from the same time period as above (2002–2010). OHP data include an individual identifier for each person—the `client ID' number. Additionally, all individuals from the same household share a `household case ID' number. As OHP covers children until they turn 19 years old, we defined anyone <19 as a child in our linkage algorithm for this dataset. The OHP data do not specify the relationship between individuals sharing a household case ID number. Thus, we developed the following criteria to identify child–parent links.
A `child' was anyone aged <19 years at any point during the study period (2002–2010) who shared a household case ID number with at least one adult who was deemed a potentially linkable parent.
A potentially linkable `parent' was anyone sharing a child's household case ID number who was aged ≥19 years at some point during the study period and was 12–55 years older than at least one child with the same household case ID number. Any adults in the household who did not meet those criteria were excluded and assumed to have another type of relationship with the identified child (e.g., sibling, significant other, grandparent, etc.). If no potentially linkable parents were identified, that child was excluded.
Within the potential child–parent links identified, only one female was considered the `mother' and only one male the `father.' Household cases with more than one potential parent of either sex were excluded, as it could not be determined which adults were the parents versus grandparent, aunt, uncle, same-sex partnership parent, etc.
If multiple children shared a household case ID number, we repeated this process for each individual child until all children in the family were either excluded or linked to a potential parent.
After we identified children who linked to at least one parent in both OCHIN EHR and OHP administrative data, we compared the demographic characteristics of these children to children who did not link to a parent within each data source.
Cross-Validation of Child–Parent Linkages
We were able to check the quality of our linkage processes by using the subset of cases from the OHP data in which both child and parent had an OCHIN EHR patient ID and the subset of OCHIN EHR cases in which the child had an OHP client ID. To perform this cross-validation, we compared the child–parent links in one dataset (tested data set) with the child–parent links in the other data set (validating data set). This study was reviewed and approved by our institutional review board [#00006727].
Results
Linking Children and Parents in OCHIN's EHR Data
We identified 249,079 children aged<18 years of age who had at least one visit to an Oregon clinic with the OCHIN EHR in 2002–2010; of the identified children, 13,455 had an emergency contact adult who was also a patient in the EHR data, 67,073 had a related adult patient identified as the guarantor for visits, and 8,447 had both an emergency contact adult and a guarantor. We excluded 1,718 children whose potentially linkable adults were not 12–55 years older than the child. An additional 5,596 children were excluded because the adult listed as guarantor was identified as someone other than the child's parent (e.g., aunt, sister, grandfather), or because the child linked to more than two potential parents. This process successfully linked 62,967 children to parents who were also patients in the same clinic network (Fig. 1).
Fig. 1.
Linking children and parents in OCHIN's EHR data. Asterisk The guarantor is the person responsible for paying for a given visit. Double asterisk Of the linked children and parents with both an emergency contact and a guarantor ID, we used the guarantor relationship if they did not agree
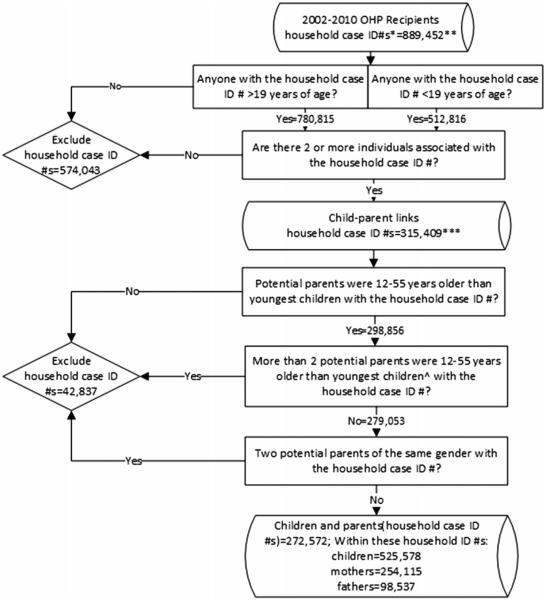
Linking Children and Parents in the Oregon Health Plan Administrative Data
Between 2002 and 2010, the OHP dataset contained information on 1,017,984 distinct children aged<19 with 889,452 distinct household case ID numbers assigned to at least one child. We excluded 574,043 household case ID numbers because they included only household members <19 years of age (only children, no potential parents). We excluded another 42,837 household case ID numbers because they did not include any adults who were 12–55 years older than at least one child in the household, included more than two adults who were 12–55 years older than the child, or included two potential parents of the same gender. This process identified 525,578 children linked to parents in the dataset (272,572 households) (Fig. 2).
Fig. 2.
Linking children and parents in the OHP administrative data. Asterisk Household case ID numbers include all people in a household. Double asterisk Within the 889,452 household case ID numbers, 1,720,499 were unique individual client ID numbers in the dataset. Triple asterisk Within the 315,409 household case ID numbers, 1,072,616 were unique individual client ID numbers in the dataset. Hat Went to the next youngest child and then the next to see if we could identify anyone with an age difference of 12–55 years until all children with the household case ID number were excluded or linked to a potential parent
Demographic Comparisons
When comparing the 62,967 children who linked to at least one parent in the OCHIN EHR dataset and the 186,112 children who did not link to a parent, we found significant differences across many socio-demographic categories. Similarly, when comparing the 525,578 children who linked to a parent in the OHP dataset to the 492,406 who did not link to a parent, we found many differences (Table 1).
Table 1.
Demographic comparisons for not linked and linked children from the OHPa and OCHIN EHR data
| Children in OHP dataset between 2002 and 2010 (n = 1,017,984) | Children in OCHIN EHR dataset between 2002 and 2010 (n = 249,079) | |||
|---|---|---|---|---|
|
|
|
|||
| Not linked (N = 492,406) (%) | Linked (N = 525,578) (%) | Not linked (N = 186,112) (%) | Linked (N = 62,967) (%) | |
| Child race/ethnicity | ||||
| Asian | 2.21 | 2.36 | 3.37 | 2.75 |
| Black | 4.57 | 4.34 | 5.48 | 5.05 |
| Hispanic | 2.91 | 4.28 | 27.24 | 47.19 |
| AI/AN | 3.24 | 2.10 | 1.16 | 0.69 |
| Other | 0.26 | 0.31 | 0.00 | 0.00 |
| Pacific Islander | 0.48 | 0.44 | 0.64 | 0.38 |
| Unknown | 21.34 | 23.30 | 7.66 | 6.09 |
| White | 64.98 | 62.87 | 54.45 | 37.84 |
| Child gender | ||||
| Female | 54.88 | 48.41 | 55.51 | 49.26 |
| Male | 45.12 | 51.59 | 44.48 | 50.74 |
| Unknown | 0.00 | 0.00 | 0.01 | 0.00 |
| Rural/urban continuum | ||||
| Metro >1,000,000 | 39.05 | 40.53 | Not available | Not available |
| Metro | 22.83 | 22.21 | ||
| 250,000–1,000,000 | ||||
| Metro <250,000 | 16.34 | 16.49 | ||
| Rural | 21.78 | 20.77 | ||
| Child year of birth | ||||
| Prior to 2002 | 80.10 | 54.15 | 80.17 | 51.49 |
| 2002–2003 | 5.59 | 11.56 | 6.79 | 11.02 |
| 2004–2005 | 5.23 | 10.84 | 5.29 | 12.87 |
| 2006–2007 | 4.51 | 10.55 | 4.14 | 12.07 |
| 2008–2009 | 3.42 | 9.11 | 2.75 | 9.54 |
| 2010 | 1.16 | 3.79 | 0.86 | 3.00 |
All differences between not linked and linked are significant at p < 0.0001 assessed by Chi square
AI/AN American Indian/Alaskan native
OHP: Oregon's public health insurance programs
Cross-Validation of Child–Parent Linkages
We identified 11,114 child–parent links in OCHIN EHR data and 20,121 in OHP administrative data that could be cross-validated. When we validated the links found in OCHIN EHR data through comparison with the OHP dataset, we found only 24 (0.2 %) cases where linkages were in conflict (e.g., we had identified a different mother or father for the child in the OHP versus the OCHIN dataset). When we validated the links found in the OHP data by comparing against the OCHIN EHR dataset, we found only 456 (2.3 %) cases where the OHP links were in conflict with the OCHIN EHR validation set (Table 2).
Table 2.
Cross-validation of child–parent linkages identified within the OHPa and OCHIN EHR data
| Tested data set | N pairs | Validating data set | Agreement | N pairs (%) | In conflict | N (%) |
|---|---|---|---|---|---|---|
| OCHIN EHR child–parent links | 11,114 | All OHP child–parent linkages in which both child and parent had an OCHIN ID | No conflict in parent(s) identified for child | 11,090 (99.8) | Different parent identified for child in OHP data | 24 (0.2) |
| OHP child–parent links | 20,121 | All OCHIN EHR child–parent linkages in which the child had an OHP individual client ID | No conflict in parent(s) identified for child | 19,664 (97.7) | OHP linked parent identified as non-parent in OCHIN EHR data, or different parent identified for child within OCHIN EHR data | 456 (2.3) |
OHP: Oregon's public health insurance programs
Discussion
Parental health insurance status is significantly associated with children's insurance status and receipt of evidence-based health care [1–8]. Further, treating a patient within the context of the family is consistent with more comprehensive and holistic care [25–27]. Thus, reliable information about health insurance coverage status and health care for children and their parents is needed to inform efforts to optimize children's health. However, no straightforward processes for linking children with parents currently exist for many datasets used in research, policy, and practice. To address this need, we developed methods for linking children and their parents within two commonly used data sources. Our methods may inform future efforts to link children and their parents in EHR data, public health insurance administrative data, and similar datasets.
Practice and Policy Implications
As the number of families receiving coverage through employer-sponsored programs decreases [11–13, 28], fewer insurance databases will include information about all family members on a single plan held by one parent (the covered employee). An increasing percentage of American children are now insured through Medicaid or CHIP, and their data is de-coupled from that of parents who are insured elsewhere or are uninsured. With the Affordable Care Act (ACA), more individuals will have access to coverage and parents may gain insurance coverage through new plans; however, parents who gain new coverage might not be insured by the same plan as their children (e.g., a parent may obtain private coverage through health insurance exchanges, while their children obtain public coverage through the CHIP) [29–31]. Even when parents `join' their children in public insurance programs through states' expanded Medicaid eligibility [32], it may be difficult to link children with their parents in state administrative datasets because of differing eligibility requirements, enrollment dates, and programmatic enrollment procedures (as in Oregon). All-payer claims databases may mitigate some of these issues but still do not provide an easy way to link parents to their children [33]. Thus, the methods described here will continue to be necessary to make these linkages, even for families where both children and parents have coverage through the same public program.
Even with ACA changes in policy, the current US policy environment makes it difficult for many families to enroll all family members in the same health insurance plan. For example, income requirements for public plans are different for children and adults [34]. In addition, employer-sponsored plans only have to be affordable for the employee (not the family) to comply with ACA regulations, which may lead to an inability of parents to afford such coverage for their children [35]. With family members increasingly insured by different plans, it has become difficult to link children and parents in health insurance datasets. Further, as payment moves towards global capitation and away from fee-for-service, insurance claims data will likely contain less complete information about health care services. EHR data may provide an important alternative source of data containing information on both children and their parents and a richer source of information related to health care services received and the health status of individual patients and families. For family members who receive care at the same clinic, EHR data can provide more complete information than health insurance data. As heath information exchanges improve, it will also be possible to link family members with information in different EHRs. As the use of EHR data for tracking and coordinating care and informing future policies increases, child–parent linkages in EHR data will become increasingly relevant to informing practice and policy decisions.
Linking children to their parents could inform research, policy, and practice in several ways. First, it could allow for treatment that targets the whole family. For example, obesity; since obesity is often a problem for children and their parents, treatment options could be directed at the whole family if clinicians are aware of the child and parents weight and other relevant biomarkers. Second, it could help inform recommendations for disease. For example, asthma; if the child's parent is a documented smoker in the EHR, this information could prompt a provider to offer additional education on its impact on the child's disease and resources to help a parent quit. Third, having known linkages between parents and children in their medical records might facilitate better coordination of care for families. For example, a provider could be electronically prompted to remind a mother at her visit about her child's immunizations that are overdue and help get them scheduled. Lastly, these linkages could be used to better understand and diagnose children by being able to see the medical issues suffered by their parents.
The linkage methods we developed were time-consuming and resource-intensive. The data had to be cleaned, managed, validated, and processed through algorithms using deductive logic to define child–parent links. Given the importance of using EHR data for the purposes described here, further investigation and validation of these linkage methods is needed. Processes for easily and automatically linking families within other large healthcare-related data sets are also needed.
Strengths and Limitations
One strength of our approach to linking children and parents within OCHIN's EHR data was the use of all relevant relationship information. Another strength in using this methodology in an EHR dataset was the large number of children for whom a potential parent could be identified.
Our process shares a weakness inherent to all secondary data analyses—the quality of the available data is determined by the quality and consistency of the data entered into the system. For example, the use of the guarantor and emergency contact fields in the EHR may vary by clinic. We did not, however, assess the extent to which completion of these data fields differed between clinics, nor were we able to assess the percentage of children who could not be linked to a parent because of missing or erroneous data, which means we likely missed many potential links. Further, as stated above, we captured only a subset of child–parent links in the EHR because we only linked children with parents who were also patients within the same health care system. We also could not find parents to link with the majority of children in the OHP dataset because the eligibility requirements for children to qualify for Medicaid or CHIP are much more inclusive than the requirements for adults. Many parents of children enrolled in OHP do not quality for this coverage due to having an income that exceeds the limit for adult eligibility. Thus, demographics differed between children who linked to a parent versus children who did not link to a parent in the datasets because certain subpopulations are more likely to have both children and parents qualify for OHP coverage or to receive health care from the same clinic.
Certain assumptions were necessary. In most cases, we believe a `true' parent was found; however, ID of a parent was premised on the assumption that an adult in the household who was 12–55 years older than the child was a `parent' or one of the child's primary guardians. We attempted to identify only children with the most probable primary guardians and excluded any in which this relationship was not easily identifiable (e.g., children linked to multiple adults of a single gender, or linked to more than two adults) so as to minimize the chances of linking to non-parent adults (e.g., grandparents, aunts/uncles, roommates, siblings, etc.). Thus, some children with same-sex parents who should have been included in the final number of linked pairs were likely excluded. Researchers wishing to exclude fewer children could relax these criteria but it may yield linkages that are less precise. We were not able to assess the percentage of children who could not be linked to a parent because of missing or erroneous data. Of note, our results are specific to one state's Medicaid and linked EHR data; applying these algorithms to different states and health systems may not be possible or may yield different linkage rates.
Conclusions
The ability to link children and their parents in large healthcare-relevant datasets is necessary for informing efforts to optimize children's health care. We developed strategies for successfully linking children with their parents in two such data sets, which are being used to study the impact of recent policy changes that increased discordant health insurance patterns in families. These algorithms could also be used to inform and evaluate future practice and policy changes.
Acknowledgments
This work was financially supported by the Agency for Healthcare Research and Quality (AHRQ) (1 R01 HS018569), the Patient-Centered Outcomes Research Institute (PCORI), and the Oregon Health & Science University, Department of Family Medicine. The funding agencies had no involvement in the preparation, review, or approval of the manuscript. We would also like to acknowledge OCHIN, Inc. and all clinics in the network for participating in this research. The authors are grateful for editing and publication assistance from Ms. LeNeva Spires, Publications Manager, Department of Family Medicine, Oregon Health & Science University, Portland, OR.
References
- 1.Yamauchi M, Carlson MJ, Wright BJ, Angier H, Devoe JE. Does health insurance continuity among low-income adults impact their children's insurance coverage? Maternal and Child Health Journal. 2012 doi: 10.1007/s10995-012-0968-0. Epub 2012/02/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wisk LE, Witt WP. Predictors of delayed or forgone needed health care for families with children. Pediatrics. 2012;130(6):1027–1037. doi: 10.1542/peds.2012-0668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DeVoe JE, Tillotson CJ, Wallace LS, Angier H, Carlson MJ, Gold R. Parent and child usual source of care and children's receipt of health care services. Annals of Family Medicine. 2011;9(6):504–513. doi: 10.1370/afm.1300. Epub 2011/11/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DeVoe JE, Tillotson CJ, Wallace LS. Children's receipt of health care services and family health insurance patterns. Annals of Family Medicine. 2009;7(5):406–413. doi: 10.1370/afm.1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sarnoff R, Hughes D. Increasing health insurance coverage in the first year of life. Maternal and Child Health Journal. 2005;9(4):343–350. doi: 10.1007/s10995-005-0023-5. [DOI] [PubMed] [Google Scholar]
- 6.DeVoe JE, Krois L, Edlund C, Smith J, Carlson NE. Uninsured but eligible children: Are their parents insured? Recent findings from Oregon. Medical Care. 2008;46(1):3. doi: 10.1097/MLR.0b013e31815b97ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guendelman S, Megan W, Veronica A, Doug O. The effects of child-only insurance coverage and family coverage on health care access and use: Recent findings among low-income children in California. Health Services Research. 2006;41(1):125–147. doi: 10.1111/j.1475-6773.2005.00460.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeVoe JE, Krois L, Edlund T, Smith J, Carlson NE. Uninsurance among children whose parents are losing Medicaid coverage: Results from a statewide survey of Oregon families. Health Services Research. 2008;43(1 Pt 2):401–418. doi: 10.1111/j.1475-6773.2007.00764.x. Epub 2008/01/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ziegenfuss JY, Davern ME. Twenty years of coverage: An enhanced current population survey-1989–2008. Health Services Research. 2010;46(1 Pt 1):199–209. doi: 10.1111/j.1475-6773.2010.01171.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blakely S. Employers, workers, and the future of employment-based health benefits. EBRI Issue Brief. 2010;339:1–23. [PubMed] [Google Scholar]
- 11.Gould E. Employer-sponsored health insurance erosion continues in 2008 and is expected to worsen. International Journal of Health Services. 2010;40(4):743–776. doi: 10.2190/HS.40.4.j. Epub 2010/11/10. [DOI] [PubMed] [Google Scholar]
- 12.Kaiser Family Foundation and Health Research & Educational Trust Employer health benefits 2012 annual survey. 2012 Cited 2013 May 28, http://ehbs.kff.org/?page=abstract&id=1.
- 13.Vistnes JP, Zawacki A, Simon K, Taylor A. Declines in employer-sponsored insurance coverage between 2000 and 2008: Examining the components of coverage by firm size. Health Services Research. 2012;47(3 Pt 1):919–38. doi: 10.1111/j.1475-6773.2011.01368.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Angier H, DeVoe JE, Tillotson CJ, Wallace LS. Changes in US family health insurance coverage patterns: Comparing 2003 to 2008. Family Medicine. 2013;45(1):26–32. [PMC free article] [PubMed] [Google Scholar]
- 15.Hsiao C-J, Hing E, Socey TC, Cai B. Electronic health record systems and intent to apply for meaningful use incentives among office-based physician practices: United States, 2001–2011. [PubMed] [Google Scholar]
- 16.111th Congress American Recovery and Reinvestment Act of 2009. 2009 Cited 2013 May 28, http://www.gpo.gov/fdsys/pkg/PLAW-111publ5/pdf/PLAW-111publ5.pdf.
- 17.Kho AN, Lemmon L, Commiskey M, Wilson SJ, McDonald CJ. Use of a regional health information exchange to detect crossover of patients with MRSA between urban hospitals. Journal of the American Medical Informatics Association. 2008;15(2):212–216. doi: 10.1197/jamia.M2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newman TB, Brown AN. Use of commercial record linkage software and vital statistics to identify patient deaths. Journal of the American Medical Informatics Association. 1997;4(3):233–237. doi: 10.1136/jamia.1997.0040233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Victor TW, Mera RM. Record linkage of health care insurance claims. Journal of the American Medical Informatics Association. 2001;8(3):281–288. doi: 10.1136/jamia.2001.0080281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Korzeniewski SJ, Grigorescu V, Copeland G, Gu G, Thoburn KK, Rogers JD, et al. Methodological innovations in data gathering: Newborn screening linkage with live births records, Michigan, 1/2007–3/2008. Maternal and Child Health Journal. 2010;14(3):360–364. doi: 10.1007/s10995-009-0464-3. [DOI] [PubMed] [Google Scholar]
- 21.DeVoe JE, Gold R, Spofford M, Chauvie S, Muench J, Turner A, et al. Developing a network of community health centers with a common electronic health record: Description of the Safety Net West Practice-based Research Network (SNW-PBRN) The Journal of the American Board of Family Medicine. 2011;24(5):597–604. doi: 10.3122/jabfm.2011.05.110052. Epub 2011/09/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeVoe J, Sears A. The OCHIN community information network: Bringing together community health centers, information technology, and data to support a patient-centered medical village. The Journal of the American Board of Family Medicine. 2013;26:271–278. doi: 10.3122/jabfm.2013.03.120234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Howard RN, Marshall LM, Peterson JM, Kohn MA. Tracking Oregon Medicaid patients' enrollment and health utilization patterns. Journal of Public Health Management and Practice. 2002;8(4):70–76. doi: 10.1097/00124784-200207000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Oregon Department of Human Services . Oregon health plan: An historical overview. Salem, OR: Jul, 2006. Report No.: 9036. [Google Scholar]
- 25.Beardslee WR, Gladstone TR, Wright EJ, Cooper AB. A family-based approach to the prevention of depressive symptoms in children at risk: Evidence of parental and child change. Pediatrics. 2003;112(2):e119–e131. doi: 10.1542/peds.112.2.e119. Epub 2003/08/05. [DOI] [PubMed] [Google Scholar]
- 26.Schor EL. Family pediatrics: Report of the Task Force on the Family. Pediatrics. 2003;111(6 Pt 2):1541–1571. Epub 2003/06/05. [PubMed] [Google Scholar]
- 27.Melnyk BM, Alpert-Gillis L, Feinstein NF, Crean HF, Johnson J, Fairbanks E, et al. Creating opportunities for parent empowerment: Program effects on the mental health/coping outcomes of critically ill young children and their mothers. Pediatrics. 2004;113(6):e597–e607. doi: 10.1542/peds.113.6.e597. Epub 2004/06/03. [DOI] [PubMed] [Google Scholar]
- 28.Gould E. Health insurance eroding for working families: Employer-provided coverage declines for fifth consecutive year. International Journal of Health Services. 2007;37(3):441–467. doi: 10.2190/C285-1547-1L23-R1X5. Epub 2007/09/12. [DOI] [PubMed] [Google Scholar]
- 29.111th Congress Compilation of patient protection and Affordable Care Act. 2010 Cited 2013 May 28, http://docs.house.gov/energycommerce/ppacacon.pdf.
- 30. Medicaid.gov . Children's Health Insurance Program. Centers for Medicare & Medicaid Services; Baltimore, MD: 2012. Medicaid.gov Cited 2013 May 28, http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Childrens-Health-Insurance-Program-CHIP/Childrens-Health-Insurance-Program-CHIP.html. [Google Scholar]
- 31.Shoen C, Doty MM, Robertson RH, Collins SR. Affordable Care Act reforms could reduce the number of uninsured US adults By 70 Percent. Health Affairs. 2011;30(9):1762–1771. doi: 10.1377/hlthaff.2011.0335. [DOI] [PubMed] [Google Scholar]
- 32.The Henry J. Kaiser Family Foundation . Implementing the ACA's Medicaid-related health reform provisions after the Supreme Court's decision. Washington, DC: Aug, 2012. 2012. Report No.: 8348. [Google Scholar]
- 33.Love D, Custer W, Miller P. All-payer claims databases: State initiatives to improve health care transparency. 2010. Contract No.: 1439. [PubMed] [Google Scholar]
- 34.Heberlein M, Brooks T, Guyer J, Artiga S, Stephens J. Holding steady, looking ahead: Annual findings of a 50-state survey of eligibility rules, enrollment and renewal procedures, and cost sharing practices in Medicaid and CHIP, 2010–2011. Washington, DC: 2011. [Google Scholar]
- 35.Hess C, Basini LO, Plaza CI. Keeping children's coverage strong in the context of the Affordable Care Act: Perspectives from state children's health insurance leaders. Portland, ME: 2012. [Google Scholar]