Abstract
Context
Tumor induced osteomalacia related to anaplastic thyroid cancer has never been reported.
Objective
We describe a case of tumor induced osteomalacia (TIO) in a patient with a fibroblast growth factor 23 (FGF-23) secreting anaplastic thyroid carcinoma. The current imaging modalities are reviewed.
Design and intervention
Clinical, biochemical, and radiological assessments were done, including computer tomography (CT) of the neck and skull to thigh positron emission tomography (PET)/CT. The patient underwent surgical tumor debulking three days after presentation due to airway compromise. Molecular studies of the resected tissue were performed using reverse transcriptase–polymerase chain reaction (RT-PCR) and gel electrophoresis for the phosphaturic mesenchymal tumor FGF-23.
Results
Resected tissue demonstrated features of anaplastic thyroid cancer with positive markers for FGF-23 protein, consistent with a FGF-23 secreting paraneoplastic tumor. The patient's metastatic burden rapidly progressed as demonstrated by a dramatic rise in serum FGF-23 levels and worsening hypophosphatemia in concert with progression of the metastatic lesions on PET/CT.
Conclusion
We believe that our patient's rapidly progressive anaplastic thyroid cancer was responsible for persistent hypophosphatemia and osteomalacia, substantiated by the finding of FGF-23 protein within the thyroid tumor cells. Our case indicates that anaplastic thyroid cancer can cause TIO.
Keywords: Anaplastic thyroid cancer, Tumor induced osteomalacia, FGF 23, Hypophosphatemia, Osteomalacia
1. Introduction
Tumor induced osteomalacia (TIO) is a rare phosphorus-wasting syndrome caused by tumors capable of secreting FGF-23 in a similar fashion as other FGF-23-mediated diseases, such as x-linked hypophosphatemia, autosomal recessive and autosomal dominant hypophosphatemia rickets. TIO is characterized by signs and symptoms of severe osteomalacia or rickets. Clinical features include bone and muscle pain, muscle weakness, skeletal deformities and recurrent fractures as well as microfractures of long bones (Drezner, 2008, Mammen and de Beur SM, 2008). Laboratory testing usually reveals low serum phosphorus, low or inappropriately normal range circulating concentration of 1,25-dihydroxyvitamin D (1,25(OH)2D), high urine fractional excretion of phosphorus, normal serum calcium and normal 25-hydroxyvitamin D 25(OH)D levels. Successful surgical resection of the FGF-23 secreting tumor is curative, thus accurate localization of the tumor is of the utmost importance (Jonsson et al., 2003). The majority of the TIO cases previously reported in the literature have been caused by small mesenchymal tumors derived from bone (Fatani et al., 2013, Westerberg et al., 2012, Gandhi et al., 2012), soft tissue (Jiang et al., 2012), skin (Gardner et al., 2013) and cartilage (Hautmann et al., 2014). TIO has also been reported in association with malignant adenocarcinomas of the ovary (Lin et al., 2014), lung (Taylor et al., 1984), prostate (Lee et al., 2014), colon (Ryan and Reiss, 1984) and head/neck (Tarasova et al., 2013, Kominek et al., 2011, Luo et al., 2013, Mathis et al., 2013). To our knowledge, TIO induced by anaplastic thyroid cancer has not been reported previously.
2. Case report
A 59 year-old white man presented to the Mayo Clinic Florida emergency department with a 3-month history of rapidly progressive dysphagia to liquids and solids, cough and hoarseness. CT of the neck with contrast revealed a 7 cm infiltrating mass centered in the anteroinferior aspect of the neck that completely encased the left carotid artery, esophagus and trachea (Fig. 1). He was evaluated by an otolaryngologist who performed a core needle biopsy of the mass, which demonstrated findings of an undifferentiated malignant neoplasm. Due to extensive infiltration of vital structures, a complete resection of the tumor was not possible. The patient underwent debulking of the tumor, tracheotomy for airway management and gastrojejunostomy tube placement for enteral feeding. Final operative histopathology was consistent with anaplastic thyroid carcinoma.
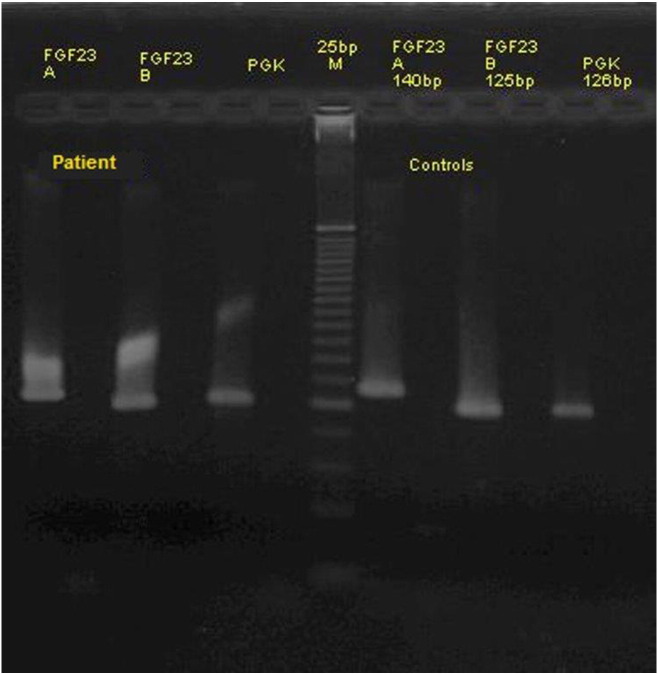
Fig. 1.
Axial CT contrast-enhanced image at the level of the upper trachea demonstrates a large soft tissue density mass in the anterior neck centered to the left of midline, compatible with the patient's known history of anaplastic thyroid cancer. The mass completely encases the left carotid artery (arrowhead), trachea and esophagus and obliterates the left jugular vein. The tracheal ring (fat arrow) is partially destroyed with tumor infiltration into the tracheal lumen. A portion of the tracheostomy tube (curved arrow) is seen just superior to its tracheal entry site.
His past medical history was significant for papillary thyroid cancer treated with right lobectomy in 1984. He underwent completion thyroidectomy in 1991 due to a recurrence. He developed vocal cord immobility after his first surgery. He appears to have mild post surgical hypoparathyroidism based on finding of low calcium with low normal PTH and high urine calcium. The patient was placed on hormone replacement therapy for expected hypothyroidism. The patient was unsure whether he underwent 131I therapy at the time of his second surgery. His phosphorus level prior to presentation is unknown.
During his hospitalization, the patient required large amounts of daily phosphorus replacement due to persistent critically low serum phosphorus levels. Biochemical evaluation (Table 1) was also noteworthy for elevated 24 h urine phosphorus secretion, low serum 1,25(OH)2D, and increased serum alkaline phosphatase activity. The serum 25(OH)D level was in the lower end of the reference range.
Table 1.
Results of laboratory tests.
| 3/19 | 3/22 | 4/11 | Normal range | |
|---|---|---|---|---|
| Serum values | ||||
| Calcium (mg/dl) | 8.8 | 8.6 | 8.8 | (8.9–10.1) |
| Phosphorus (mg/dl) | 0.7 | 0.9 | 0.9 | (2.5–4.5) |
| ALP (IU/I) | 128 | 146 | 649 | (45–115) |
| Creatinine (mg/dl) | 0.7 | 0.8 | 1.1 | (0.8–1.3) |
| BUN (mg/dl) | 7 | 11 | 28 | (8–24) |
| Intact PTH (pg/ml) | 16.1 | 9.9 | (15–65) | |
| 1,25(OH)2D (pg/ml) | 17 | < 8 | (18–78) | |
| 25(OH)2D (ng/ml) | 12.2 | 17.3 | (> 20) | |
| TSH (mIU/L) | 38.17 | 45.34 | 19.32 | (0.3–5) |
| Free T4 (ng/dL) | 1.1 | 0.8 | (0.8–1.8) | |
| TG (ng/ml) | 13.4 | (< 0.1)a | ||
| TG Ab (Iu/mL) | < 1.8 | (< 1.8) | ||
| iFGF-23 (RU/mL) | 2355 | 7950 | (< 180) | |
| Urine values | ||||
| Calcium (mg/24 h) | 391 | 636 | (25–300) | |
| Phosphorus (mg/24 h) | 1169 | 3591 | (< 1099) |
ALP- total alkaline phosphatase; TG- thyroglobulin tumor marker; TG Ab- thyroglobulin antibody.
Athyrotic individuals; iFGF 23- intact fibroblast growth factor 23.
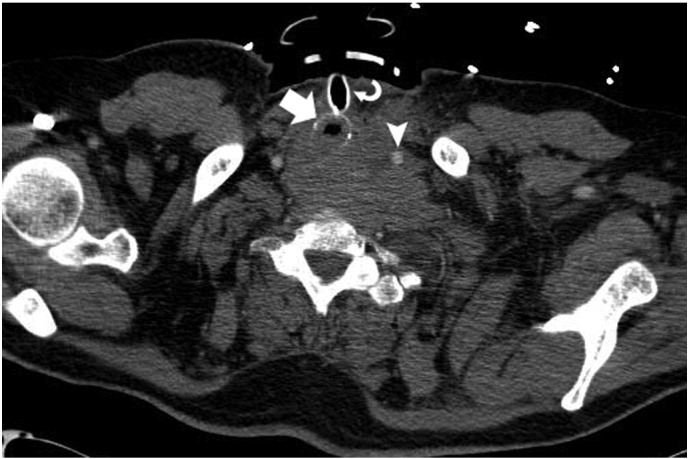
Laboratory findings are listed in Table 1. A skull-thigh PET/CT showed abnormal areas of hypermetabolism consistent with metastases in the lungs, mediastinum, liver and left greater trochanter. Repeat imaging one week later revealed progression in size and number of his lung and liver metastases (Fig. 2). Biopsy of these lesions was not feasible due to the decline of patient's health status.
Fig. 2.
Coronal fused PET/CT image demonstrates abnormal glucose hypermetabolism of a large superior mediastinal mass (arrow) corresponding the patient's known anaplastic thyroid cancer. There is abnormal hypermetabolism in the visualized mediastinal and bilateral hilar lymph nodes (arrowheads), compatible with metastatic disease.
The patient suffered a rapid decline in his overall condition and died of multiorgan failure one month after presentation. A repeat FGF-23 level at the time of his death had more than tripled from 2355 RU/mL to 7950 RU/mL.
3. Pathology and immunohistochemistry
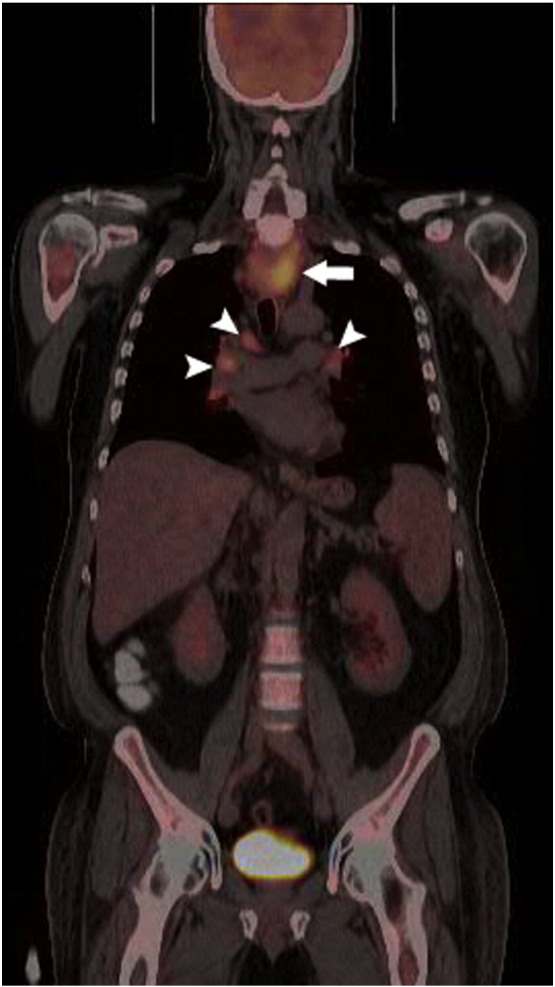
Tissue obtained from the anterior left neck measuring 6.0 cm in maximum dimension was provided for pathological analysis. Dissection revealed a 3.5 cm gray/white tumor with adherent soft tissue and skeletal muscle. Histologically, a malignant epithelioid and spindle cell tumor was identified that was infiltrating the skeletal muscle and encasing the large vessel walls. The tumor was negative for cytokeratin, thyroglobulin and TTF-1, consistent with an anaplastic thyroid carcinoma. Tissue fragments obtained during surgical debulking were analyzed using reverse transcriptase polymerase chain reaction (RT-PCR) and gel electrophoresis for phosophaturic mesenchymal tumor FGF-23 gene on RNA extracted from paraffin imbedded tissue. The tissue was positive for the presence of FGF-23 by RT-PCR (Fig. 3). The FGF-23 gene revealed positive amplification results; all controls yielded appropriate results. Molecular analysis confirmed the expression of the gene within the neoplastic cells.
Fig. 3.
RT-PCR gel of the FGF-23 tumor and the controls.
4. Discussion
TIO (also known as oncogenic osteomalacia) is a bone mineralization disorder caused by secretion of a phosphorus-wasting protein, FGF-23 from tumor cells (Jonsson et al., 2003, Shane et al., 1997, Cai et al., 1994). FGF-23 is detectable in the blood of normal individuals, but is markedly increased in cases of tumor-induced TIO due to overexpression of FGF-23 messenger RNA (mRNA) (Jonsson et al., 2003). TIO is most often caused by small benign tumors of mesenchymal origin, such as osteoblastomas, nonossifying and ossifying fibromas (Drezner, 2008, Mammen and de Beur SM, 2008). Less commonly, TIO manifests as a paraneoplastic syndrome derived from various malignant tumors. In most reported cases, complete surgical resection of the inciting tumor results in absolute resolution of the signs and symptoms of TIO. Furthermore, Shane et al found bone remineralization on iliac biopsy samples in patients who had undergone complete surgical resection (Shane et al., 1997). Although the syndrome has been reported in children, TIO typically affects adults. Importantly, TIO patients do not have a history of childhood fractures nor a family history of hypophosphatemia or osteomalacia, which help distinguish this entity from other phosphorus-wasting syndromes such as x-linked hypophosphatasia and autosomal dominant and autosomal recessive hypophosphatasia. The diagnosis of TIO is confirmed by documentation of an elevated serum FGF-23 level (Carpenter TO et al., 2011).
The mechanism by which FGF-23 is involved in phosphorus-wasting is well described (Shane et al., 1997, Cai et al., 1994, Carpenter TO et al., 2011). FGF-23 is a member of the fibroblast growth factor family responsible for phosphorus metabolism and is produced as a hormone by osteocytes and osteoblasts. Excess secretion of FGF-23 causes hypophosphatemia and impaired mineralization of the bone resulting in osteomalacia, with resultant bone pain, bone deformities, and fracture. Excess FGF-23 also inhibits renal production of 1,25(OH)2D by acting on a FGF receptor (klotho) in the kidney and inhibiting renal conversion of 25(OH)D to 1,25(OH)2D, which interferes with intestinal and kidney phosphorus absorption, respectively. Low plasma phosphorus is also known to stimulate renal production of 25-hydroxyvitmain D-1α hydroxylase, resulting in conversion of 25 (OH)D to 1,25 (OH)2 D. However, in TIO, impaired renal phosphorus reabsorption lowers 1,25 (OH)2 D synthesis. Low or inappropriately normal serum levels of 1,25(OH)2 D (in the setting of a low phosphorus level) is the most common biochemical feature of the disease. This patient also had hypercalcuria which we suspect is related to hypoparathyroidism as evidenced by consistently low PTH and low calcium since admission.
The diagnosis of TIO should be suspected from the clinical signs and symptoms including acquired hypophosphatemia, osteomalacia, bone fractures, and generalized muscle weakness in association with renal phosphate wasting (but no other proximal tubular defects) and an inappropriately low or normal plasma calcitriol concentration. Delayed diagnosed is typical in TIO, with times from symptom onset to diagnosis reported to range from approximately 1.5–28 years with an average of 6.7 years (Jiang et al., 2012, de Jan et al., 2002). Male to female ratio is approximately 1:1 with an average age of 42 years (Jiang et al., 2012).
Once a clinical diagnosis of TIO is made, the most challenging aspect of the disease is localization of the FGF-23 producing tumor. A stepwise approach that involves a thorough history, physical examination for palpable tumors, and imaging should be undertaken. Selective venous sampling, and tissue biopsy are seldom essential to discriminate a functional mass when multiple suspicious lesions are discovered. Wide surgical excision is important to avoid late recurrence and provides the best chance for complete cure. Radiofrequency ablation of the tumor has also been described as an alternate method of treatment (Jadhav et al., 2014).
Conventional imaging with CT, ultrasound, angiography and magnetic resonance imaging (MRI) have a high failure rate in localizing the causative mesenchymal tumors because they are often small and can be situated in obscure locations such as a distal extremity. For this reason, whole body imaging is essential (de Jan et al., 2002). Tumors associated with TIO express somatostatin receptors 2 and 5 so radiolabeled somatostatin analog scintigraphy (octreoscan) is frequently used to detect these tumors (de Jan et al., 2002, Jadhav et al., 2014, Rj et al., 2013, Seufert et al., 2001). Jan de Beur et al reported 111Indium-pentetreotide scintigraphy localized the offending tumor in 5 of 7 patients, whereas only 3 of the tumors were detected with conventional imaging (de Jan et al., 2002). Tumors were located at various sites including the ethmoid sinus, cranial fossa, humeral head, hand, and lower leg. Once identified with an octreoscan, MRI was used for direct anatomic visualization of the tumors, which were all later confirmed with surgery (de Jan et al., 2002). Rhee et al was also able to localize a mesenchymal TIO tumor in the bone marrow of the femoral neck with 111indium-octreotide scintigraphy (Rhee et al., 2001). Octreoscan with SPECT/CT has also been reported to improve localization (Rodrigues et al., 2014). Unfortunately, the high sensitivity of octreotide scintigraphy is limited to tumors expressing somatostatin receptor subtypes 2 and 5, and this imaging technique cannot detect those tumors expressing subtypes 1 or 4 (de Jan et al., 2002, Rhee et al., 2001). Although less sensitive than an octreoscan, whole body 18Fluorodeoxyglucose (FDG) PET/CT is an alternate imaging modality that can be used to detect FGF-23-secreting tumors. (PET/CT) allows for whole body functional imaging together with CT for anatomic localization (Chong et al., 2013). In a series of 31 patients, Chong et al reported that octreoscan was able to accurately localize TIO mesenchymal tumors in 18/21 patients and exclude the disease in 7/9 patients. Conversely, FDG PET/CT was able to accurately localize the tumor in only 14/21 patients (Chong et al., 2013). Furthermore, octreoscan was superior in localization of the tumor in 7/20 (35%) patients. Thus the authors suggested that octreoscan should be the initial imaging modality used in the attempt to localize a TIO-inducing tumor, with FDG PET/CT as an alternate for scintigraphically occult tumors (Chong et al., 2013). Once the tumor is detected by radiolabeled somatostatin scintigraphy, local imaging with MRI of the suspicious site was used to provide a precise anatomic location prior to surgery (Chong et al., 2013, Chong et al., 2011). Recent reports investigating a hybrid of somatostatin receptor imaging with PET/CT show promising results in the detection of tumors that are otherwise occult by octreoscan or octreoscan-SPECT/CT (Rj et al., 2013, Breer et al., 2014). Clifto-Bligh et al reported that Gallium-68 DOTA-octreotide (DOTA-TATE) somatostatin receptor PET/CT hybrid imaging localized tumors in 6/6 patients with histologically proven TIO (Rj et al., 2013). Similarly, Breer et al reported5/5 patients had successful detection of their tumor by using 68GaDTA-TATE PET/CT, whereas only 1/5 of these patients had tumor detected by 111indium octreotide scintigraphy (Breer et al., 2014). Other imaging techniques that utilize somatostatin receptor analogs and selective venous sampling have also been reported with varying degrees of success (Chong et al., 2013, Chong et al., 2011, Breer et al., 2014, Sood et al., 2013, Jin et al., 2013, Fukumoto, 2014, Agrawal et al., 2015). Frequently, multiple imaging studies and continuous clinical monitoring are necessary to localize these tumors, especially when small.
TIO has been described in association with adenocarcinomas of the ovary, lung, prostate, colon and head/neck (Fatani et al., 2013, Westerberg et al., 2012, Gandhi et al., 2012, Jiang et al., 2012, Gardner et al., 2013, Hautmann et al., 2014, Lin et al., 2014, Taylor et al., 1984, Lee et al., 2014, Ryan and Reiss, 1984, Tarasova et al., 2013, Kominek et al., 2011, Luo et al., 2013, Mathis et al., 2013). There has been one case report of a patient with thyroid cancer presenting with TIO and bone metastasis. Although this patient had a history of papillary thyroid cancer, testing indicated that the patient's TIO and bone metastases were due to a phosphaturic mesenchymal tumor (Morimoto et al., 2014). Genetic mechanism by which tumors express FGF-23 is not well known. Recent identification of a novel FN1-FGFR1 genetic fusion was reported (Lee et al., 2015). Future studies are needed for better understanding.
In summary, a phosphorus level should be obtained during the evaluation of patients with a clinical picture suspicious for osteomalacia. TIO should be considered in patients with low serum phosphorus levels and signs and symptoms of osteomalacia. Whole body imaging for tumor detection is essential. The disease can be cured by successful resection of the causative tumor with remineralization of bone and complete resolution of symptoms. This case report illustrates that anaplastic thyroid cancer can potentially secrete FGF 23 and be a cause of TIO.
Disclosure statement
The authors have nothing to disclose.
Acknowledgment
No funding was received.
References
- Drezner M.K. Phosphorus homeostasis and related disorders. In: Bilezikian J.P., Raisz L.G., Martin T.J., editors. Principles of Bone Biology. Academic Press; San Diego, CA, U.S.A.: 2008. pp. 465–486. [Google Scholar]
- Mammen J., de Beur SM Jan. Tumor induced osteomalacia. In: Bilizikian J.P., Raisz L.G., Martin T.J., editors. Principles of Bone Biology. third ed. Academic Press; San Diego, CA, U.S.A.: 2008. pp. 1549–1557. [Google Scholar]
- Jonsson K.B., Zahradnik R., Larsson T., White K.E., Sugimoto T., Imanishi Y. Fibroblast growth factor 23 in oncogenic osteomalacia and X-linked hypophosphatemia. N. Engl. J. Med. 2003;348:1656–1663. doi: 10.1056/NEJMoa020881. [DOI] [PubMed] [Google Scholar]
- Fatani H.A., Sunbuli M., Lai S.Y., Bell D. Phosphaturic mesenchymal tumor: a report of 6 patients treated at a single institution and comparison with reported series. Ann. Diagn. Pathol. 2013;17(4):319–321. doi: 10.1016/j.anndiagpath.2012.06.005. [DOI] [PubMed] [Google Scholar]
- Westerberg P., Linde T., Vanderschueren D., Billen J., Jans I., Ljunggren O. A case of oncogenic osteomalacia illustrating the effect of fibroblast growth factor 23 on phosphate homeostasis. Clin. Kidney J. 2012;0:1–4. doi: 10.1093/ckj/sfs031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi G.Y., Shah A.A., Wu K.J., Gupta V., Shoraka A.R. Tumor-induced osteomalacia caused by primary fibroblast growth factor 23 secreting neoplasm in axial skeleton: a case report. Case Reports in Endocrinology. 2012;2012:185454. doi: 10.1155/2012/185454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Y., Xia Wei-bo, Xiao-ping X., Silva C., M L.I., Wang O. Tumor-induced osteomalacia: an important cause of adult-onset hypophosphatemic osteomalacia in china: report of 39 cases and review of the literature. J. Bone Miner. Res. 2012;27(9):1967–1975. doi: 10.1002/jbmr.1642. [DOI] [PubMed] [Google Scholar]
- Gardner K.H., Shon W., Folpe A.L., Wieland C.N., Tebben P.J., Baum C.L. Tumor induced osteomalacia resulting from primary cutaneous phosophaturic mesenchymal tumor: a case and review of the medical literature. J. Cutan. Pathol. 2013;40(9):780–784. doi: 10.1111/cup.12209. [DOI] [PubMed] [Google Scholar]
- Hautmann A.H., Schroeder J., Wild P. Tumor-induced osteomalacia: increased level of FGF-23 in a patient with a phosphaturic mesenchymal tumor at the tibia expressing periostin. Case Reports in Endocrinology. 2014;2014:729387. doi: 10.1155/2014/729387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H.A., Shih S.R., Tseng Y.T., Chen C.H., Wy Chiu, Hsu C.Y., Tsai K.S. Ovarian cancer-related hypophosphatemia osteomalacia—a case report. J. Clin. Endocrinol. Metab. 2014;99(12):4403–4407. doi: 10.1210/jc.2014-2120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor H.C., Fallon M.D., Velasco M.E. Oncogenic osteomalacia and inappropriate antidiuretic hormone secretion due to oat-cell carcinoma. Ann. Intern. Med. 1984;101(6):786–788. doi: 10.7326/0003-4819-101-6-786. [DOI] [PubMed] [Google Scholar]
- Lee Ek, Martinez M.C., Blakely K., Santos K.D., Hoang V.C., Chow A., Emmeneger U. FGF23: mediator of poor prognosis in a sizeable subgroup of patients with castration-resistant prostate cancer presenting with severe hypophohatemia? Med. Hypotheses. 2014;83(4):482–487. doi: 10.1016/j.mehy.2014.08.005. [DOI] [PubMed] [Google Scholar]
- Ryan E.A., Reiss E. Oncogenous osteomalacia. Review of the world literature of 42 cases and report of two new cases. Am. J. Med. 1984;77(3):501–512. doi: 10.1016/0002-9343(84)90112-8. [DOI] [PubMed] [Google Scholar]
- Tarasova V.D., Trepp-Carrasco A.G., Thompson R., Recker R.R., Chong W.H., Collins M.T., Armas L.A. Successful treatment of tumor-induced osteomalacia due to an intracranial tumor by fractionated stereotactic radiotherapy. J. Clin. Endocrinol. Metab. 2013;98(11):4267–4272. doi: 10.1210/jc.2013-2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kominek P., Starek I., Geierova M., Atousek P., Zelenik K. Phosphaturic mesenchymal tumour of the sinonasal area: case report and review of the literature. Head Neck Oncol. 2011;3(16):1–4. doi: 10.1186/1758-3284-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo L., Low N., Vandervord J. Mandibular phosphaturic mesenchymal tumor-mixed connective tissue variant in a young girl. Cleft Palate Craniofac J. 2013;50(6):751–753. doi: 10.1597/12-085. [DOI] [PubMed] [Google Scholar]
- Mathis D.A., Stehel E.J., Beshay J.E., Mickey B.E., Folpe A.L., Raisanen J. Intracranial phosphaturic mesenchymal tumors: report of 2 cases. J. Neurosurg. 2013;118(4):903–907. doi: 10.3171/2012.12.JNS12598. [DOI] [PubMed] [Google Scholar]
- Shane E., Parisien M., Henderson J.E., Dempster D.W., Feldman F., Hardy M.A. Tumor-induced osteomalacia: clinical and basic studies. J. Bone Miner. Res. 1997;12(9):1502–1511. doi: 10.1359/jbmr.1997.12.9.1502. [DOI] [PubMed] [Google Scholar]
- Cai Q., Hodgson S.F., Kao P.C., Lennon V.A., Klee G.G., Zinsmiester A.R., Kumar R. Brief report: inhibition of renal phosphate transport by a tumor product in a patient with oncogenic osteomalacia. N. Engl. J. Med. 1994;330(23):1645–1649. doi: 10.1056/NEJM199406093302304. [DOI] [PubMed] [Google Scholar]
- Carpenter TO, Imel E.A., Holm I.A., Jan de Beur S.M., Insogna K.L. A clinician's guide to x-linked hypophosphatemia. J. Bone Miner. Res. 2011;26(7):1381–1388. doi: 10.1002/jbmr.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jan de Beur S.M., Streeten E.A., Civelek A.C., McCarthy E.F., Uribe L., Marx S.J. Localisation of mesenchymal tumours by somatostatin receptor imaging. Lancet. 2002;359:761–763. doi: 10.1016/s0140-6736(02)07846-7. [DOI] [PubMed] [Google Scholar]
- Jadhav S., Kasaliwal R., Shetty N.S., Kulkarni S., Rathod K., Opat B. Radiofrequency ablation, an effective modality of treatment in tumor-induced osteomalacia: a case series of three patients. J. Clin. Endocrinol. Metab. 2014;99(9):3049–3054. doi: 10.1210/jc.2013-4515. [DOI] [PubMed] [Google Scholar]
- Rj Clifton Bligh, Hofman M.S., Duncan E., lew Si, Darnell D., Clakson A. Improving diagnosis of tumor-induced osteomalacia with gallium-68 DOTATATE PET/CT. J. Clin. Endocrinol. Metab. 2013;98(2):687–694. doi: 10.1210/jc.2012-3642. [DOI] [PubMed] [Google Scholar]
- Seufert J., Ebert K., Muller J., Eulert J., Hendrich C., Werner E. Octreotide therapy for tumor induced osteomalacia. N. Engl. J. Med. 2001;345(26):1883–1888. doi: 10.1056/NEJMoa010839. [DOI] [PubMed] [Google Scholar]
- Rhee Y., Lee J.D., Shin K.H., Lee H.C., Huh K.B., Lim S.K. Oncogenic osteomalacia associated with mesenchymal tumour detected by indium-111 octreotide scintigraphy. Clin. Endocrinol. 2001;54(4):551–554. doi: 10.1046/j.1365-2265.2001.01056.x. [DOI] [PubMed] [Google Scholar]
- Rodrigues N.R., Calich A.L., Etchebehere M., Ichiki W.A., Pereira F.P., Amstalden E.M., de Sa Etchebehere E.C. Whole-body 99mTc-octreotide scintigraphy with SPECT/CT to detect occult tumor inducing paraneoplastic osteomalacia. Clin. Nucl. Med. 2014;00:00-00. doi: 10.1097/RLU.0000000000000341. [DOI] [PubMed] [Google Scholar]
- Chong W.H., Adreopoulou P., Chen C.C., Reynolds J., Guthrie L., Kelly M., Garni R.I., Bhhattacharyya N., Boyce A.M., El-Maouche D., Crespo D.O., Sherry R., Change R., Wodajo F.M., Kletter G.B., Dwyer A., Collins M.T. Tumor localization and biochemical response to cure in tumor induced osteomalacia. J. Bone Miner. Res. 2013;28(6):1386–1398. doi: 10.1002/jbmr.1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong W.H., Yavuz S., Patel S.M., Chen C.C., Collins M.T. The importance of whole body imaging in tumor-induced osteomalacia. J. Clin. Endocrinol. Metab. 2011;96(12):3599–3600. doi: 10.1210/jc.2011-1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breer S., Brunhorst T., Beil F.T., Peldschus K., Heiland M., Klutmann S. 68Ga DOTA-TATE PET/CT allows tumor localization in patients with tumor-induced osteomalacia but negative 111in-octreotide SPECT/CT. Bone. 2014;64:222–227. doi: 10.1016/j.bone.2014.04.016. [DOI] [PubMed] [Google Scholar]
- Sood A., Agarwal K., Shukla J., Goel R., Dhir V., Bhattacharya A., Rai Mittal B. Bone scintigraphic patterns in patients' of tumor induced osteomalacia. Indian J. Nucl. Med. 2013;28(2):173–175. doi: 10.4103/0972-3919.119541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin X., Jing H., Li F., Zhuang H. Osteomalcia-inducing renal clear cell carcinoma uncovered by 99mTc-hydrazinonictinyl-Tyr3-octreotide (99mTc-HYNIC-TOC) scintigraphy. Clin. Nucl. Med. 2013;38(11):922–924. doi: 10.1097/RLU.0b013e3182a20ded. [DOI] [PubMed] [Google Scholar]
- Fukumoto S. Diagnostic modalities for FGF23-producing tumors in patients with tumor induced osteomalacia. Endocrinol. Metab. 2014;29(2):136–143. doi: 10.3803/EnM.2014.29.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal K., Bhadada S., Mittal B.R., Shukla J., Sood A., Bhattacharya A., Bhansali A. Comparison of 18F-FDG and 68Ga DOTATATE PET/CT in localization of tumor causing oncogenic osteomalacia. Clin. Nucl. Med. 2015;40(1):e6–e10. doi: 10.1097/RLU.0000000000000460. [DOI] [PubMed] [Google Scholar]
- Morimoto T., Takenaka S., Hashimoto N., Araki N., Myoui A., Yoskikawa H. Malignant phosphaturic mesenchymal tumor of the pelvis: a report of two cases. Oncol. Lett. 2014;8(1):67–71. doi: 10.3892/ol.2014.2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.C., Jeng Y.M., Su S.Y., Wu C.T., Tsai K.S., Lee C.H., Lin C.Y., Carter J.M., Huang J.W., Chen S.H., Shih S.R., Mariño-Enríquez A., Chen C.C., Folpe A.L., Chang Y.L., Liang C.W. Identification of a novel FN1-FGFR1 genetic fusion as a frequent event in phosphaturic mesenchymal tumour. J. Pathol. 2015;235(4):539–545. doi: 10.1002/path.4465. [DOI] [PubMed] [Google Scholar]