Abstract
Home-based telemedicine (HBT) is a validated method of evidence-based treatment delivery for posttraumatic stress disorder (PTSD), and justification for its use has centered on closing gaps related to provider availability and distance to treatment centers. However, another potential use of HBT may be to overcome barriers to care that are inherent to the treatment environment, such as with female veterans who have experienced military sexual trauma (MST) and who must present to VA Medical Centers where the majority of patients share features with perpetrator (e.g. gender, clothing) and may function as reminders of the trauma. Delivering evidence-based therapies to female veterans with MST-related PTSD via HBT can provide needed treatment to this population. This manuscript describes an ongoing federally funded randomized controlled trial comparing Prolonged Exposure (PE) delivered in-person to PE delivered via HBT. Outcomes include session attendance, satisfaction with services, and clinical and quality of life indices. It is hypothesized that based on intent-to-treat analyses, HBT delivery of PE will be more effective than SD at improving both clinical and quality of life outcomes at post, 3-, and 6-month follow-up. This is because ‘dose received’, that is fewer sessions missed, and lower attrition, will be observed in the HBT group. Although the current manuscript focuses on female veterans with MST-related PTSD, implications for other populations facing systemic barriers are discussed.
1. Introduction
Military sexual trauma (MST) is defined as sexual assault or repeated threatening sexual harassment experienced while in the military (Veterans Affairs [VA], 2015). The VA requires providers to screen for MST and offer free evidence-based care for MST-related problems. Prevalence of MST among women who use VA services ranges between 15 and 36% depending on how MST is defined, assessment methods used, and the population sampled (for a review, see Stander & Thomsen, 2016). MST is not a psychiatric diagnosis; however, MST-related posttraumatic stress disorder (PTSD) is a widespread problem for female Veterans and PTSD is focused on for this population because it is the most common psychiatric disorder associated with MST (Kang et al., 2005; Suris et al., 2007) and Veterans with MST are approximately twice as likely than Veterans without MST to have PTSD (Klingensmith, Tsai, Mota, Southwick, & Pietrzak, 2014). Other associated disorders include depression, substance use disorders, and eating disorders (Suris & Lind, 2008).
Despite strong legislative effort, evaluation of VA-MST screening data shows that for every 5.5 women who screen positive for PTSD, only one will pursue VA mental health services (Kimerling, 2008). Further, female veterans and those with MST histories are more likely to receive pharmacological treatment for mental health conditions through primary care rather than the more effective evidence-based psychosocial treatments for PTSD [i.e., Prolonged Exposure (PE); Foa et al., 2007)], offered through VA specialty care clinics (Chatterjee et al., 2009; Maguen et al., 2010). This represents a missed opportunity since recent data indicate that PTSD treatment outcomes do not differ based on MST status (Tiet, Levya, Blau, Turchik, & Rosen, 2015). Thus, given adequate access to VA care, veterans with MST histories are likely to benefit from treatment. Yet approximately half of female veterans with an MST history do not use VA healthcare (Calhoun et al., 2016). Accordingly, it is essential to develop methods of improving access to care in this population.
One way to increase access in this population is to provide PTSD treatment via home-based telemedicine (HBT). PTSD treatment via standard telemedicine (i.e., central hub clinic to distal satellite clinic) and HBT have thus far been found to be non-inferior to the same treatment delivered in-person (Acierno et al., in press; Egede et al., 2015; Maieritsch, et al., 2015; Morland, et al., 2015); and to yield comparable dropout rates for veterans (Hernandez-Tejada, Zoller, Ruggiero, Kazley, & Acierno, 2014). HBT is thus a promising mode of PTSD service delivery to female veterans with MST that allows for enhanced treatment access. HBT has several advantages including that it removes potential barriers to receiving services including travel time and associated costs and can improve reach to rural veterans (Fortney et al., 2015).
2. Current Study
The current study is a Department of Defense funded project (W81XWH-14-1-0264) designed to compare the feasibility and efficacy of delivering PE for PTSD in-person versus via HBT for female veterans with MST. The innovative study design focuses on increasing access to a patient population that experiences significant barriers to initiating and completing PTSD-related treatment within VAMCs. Although the current trial focuses specifically on female veterans with a history of MST, there are clear implications for other patient populations who are underserved due to potential systemic barriers making it potentially difficult for female Veterans in particular to receive services at VAMCs.
The VA environment is heavily male dominated and has the potential to cue MST-related memories and distress, presenting a potential barrier to receiving treatment for female Veterans with MST histories. There is evidence that these trauma cues may be far more than discriminative stimuli for anxiety in that there are data to suggest that female veterans are at actual risk for re-victimization while at VA facilities. A recent survey of 1,205 female veterans found that 24% experienced sexual harassment while at a VAMC, although less than half reported it (Darling, Hamilton, Canelo, Haskell, & Yano, 2015). In such cases, the conditioned fear response in this male-dominated environment may be perpetuated and strengthened. Because of this potential unique barrier to care for Veterans with MST histories, the current study focuses on examining HBT to provide MST-related PTSD treatment for this population.
The current clinical trial consists of a randomized, between groups, repeated measures design assessing the impact of delivering Prolonged Exposure (PE) via HBT versus standard “in-person” delivery (SD) for female veterans with MST histories clinical outcomes such as PTSD and depression, quality of life indices, and on overall number of sessions completed (i.e., PE ‘dosing’). Targeted enrollment is n =100 female veterans with MST-related PTSD recruited from a large VAMC in the Southeastern United States and randomized to HBT or SD. Participants in both treatment conditions will receive 8-12 weekly sessions of PE and will be assessed at baseline, post-treatment, and at 3- and 6- month follow-up (see Figure 1).
Figure 1.
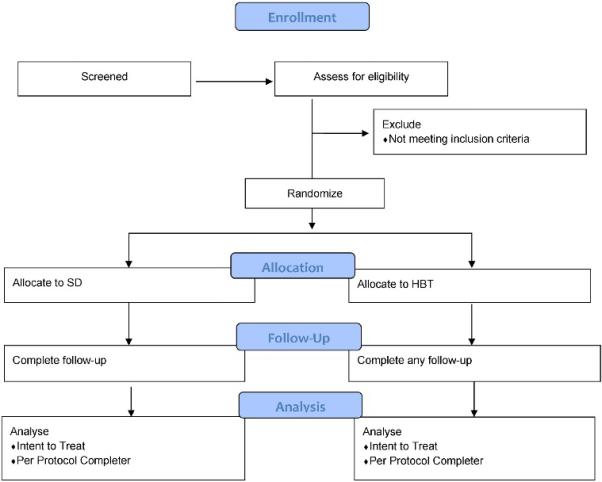
Flow Diagram
To date, the majority of research on HBT for veterans with PTSD has focused on non-inferiority designs. However, given the potential for unique access to care barriers for veterans with MST-related PTSD, we chose a superiority design in favor of HBT. More specifically, we hypothesize that, based on intent-to-treat analyses, HBT delivery of PE will be more effective than SD at improving both clinical and quality of life outcomes at post, 3-, and 6-month follow-up. This is because ‘dose received’, that is fewer sessions missed, and lower attrition, will be observed in the HBT group.
2. Methods
2.1 Participant Recruitment
Female veterans with MST-related PTSD (n = 100) are being recruited from a VAMC in the Southeastern United States. The following five strategies are used to ensure adequate recruitment of our target population: 1) referrals from the local MST Care Coordination team; 2) referrals from the local PTSD Clinical Team; 3) referrals from local VA primary care nurse practitioners; 4) letters of invitation to veterans who screen positive for MST at the VAMC and affiliated Community Based Outpatient Clinics (CBOCs) obtained from updated lists (every 3 months); and 5) general referrals from other local VAMC clinics.
Inclusion criteria are as follows: 1) MST-related index event MST-related index event on the Stressful Events for Veterans Questionnaire (adapted to integrate the National Stressful Events Survey [Kilpatrick et al., 2013] and MST screener questions [Kimerling et al., 2007] and adapt to Veterans [Miller et al., 2013]); and 2) Diagnosis of PTSD-related to MST assigned on the basis of the Clinician Administered PTSD Scale (CAPS; Blake et al., 2005; Weathers et al., 2013). CAPS for DSM-IV was used at the onset of the study for a total of 3 participants and CAPS for DSM-5 has been used since available. Potential participants will be excluded from study participation for the presence of comorbid conditions with the potential to affect their ability to participate safely in and benefit from treatment. These include: 1) Active psychosis or dementia at screening; 2) Suicidal ideation with clear intent; 3) Current substance dependence (as assessed by the MINI for DSMIV). Participants who are concurrently enrolled in another clinical trial for PTSD or depression and/or have a household member in the study (whose participation might affect their perception of/experience with study treatment) will also be excluded. In order to ensure a representative patient sample, major depressive disorder, substance use, and the use of psychotropic medications do not represent exclusionary criteria for the study. However, veterans with recent change in their psychiatric medications are asked to wait for 4 weeks before enrolling in the study. Based on previous work and the results of similar studies (e.g. Schnurr et al., 2007) we anticipate that 35% of Veterans will drop out of treatment before completion. However, to account for the dilution effect of intent to treat analyses, anticipated dropout of some participants before treatment begins, and the anticipated need to impute some missing data, we plan to over-recruit by 15%. Thus, we will enroll n=116 veterans (n=58 veterans per treatment condition) to ensure a final sample size for intent to treat analyses of n = 100.
2.2 PE Therapy
PE is a frontline treatment for PTSD in both civilian and veteran samples (e.g., Bradley et al., 2005; Beidel, Frueh, et al., 2011; Cloitre, 2009; Foa et al., 2007; Foa et al., 1991; Frueh et al., 1995; Powers, 2010); and the Institute of Medicine (2007) and VA/Department of Defense (2010) both identify PE as an empirically validated, evidence-based psychotherapies for veterans with PTSD. Based on the strong evidence base for PE, the VHA launched a national initiative to implement and disseminate PE into clinical practice VAMCs (Ruzek & Rosen, 2009). Although PE has been found to be effective in a number of studies targeting combat-related PTSD, there are few data on the efficacy of PE for female veterans with MST-related PTSD.
PE is based on emotional processing theory which suggests that traumatic events are incompletely and/or inaccurately encoded in memory as “fear networks.” Gradual exposure to corrective information through the confrontation of traumatic stimuli within a safe therapeutic environment is believed to result in a competing memory structure that inhibits the conditioned fear response. PE relies on two primary therapeutic tools: in vivo exposure and imaginal exposure. During in vivo exposure, the patient confronts feared, but safe, stimuli that cue trauma-related distress. During imaginal exposure, patients “revisit” the traumatic event, providing a detailed verbal account that includes sensory information, thoughts, feelings, and reactions experienced during the traumatic event.
PE is a manualized treatment (Foa et al., 2007) that includes the following components: a) psycho-education and treatment rationale (sessions 1 and 2); b) repeated in vivo exposure to traumatic stimuli (in vivo exercises are assigned as homework during sessions 3 through 11); c) repeated, prolonged, imaginal exposure to traumatic memories (imaginal exposure is implemented during sessions 3 through 11, patients listen to session audiotapes for homework between sessions), and d) relapse prevention strategies and further treatment planning (session 12).
2.3 Telecommunications Technology
One strategy for decreasing attrition is to make the treatment more accessible. In the case of women with a history of MST, accessibility will be enhanced by removing a barrier to care associated with the treatment environment that can potentially elicit an anxiety and avoidance response in the target population. In the current study, HBT care is delivered using via Movi/Jabber software packages installed on standard tablet devices or home computers with standard internet connections (VA side, veteran side) to teleconference (video and audio) in real time, using federal government tested and approved encryption. This software offers high-resolution images and a fluid picture, and the encryption and program meet FIPS 140-2 standards (NIST, 2002) and are HIPAA compliant. The study team has successfully implemented and used this software in two other clinical trials (HX00152; W81XWH-08-2-0047) evaluating HBT service delivery of exposure therapy to veterans with PTSD, and Jabber is now a standard program used to deliver HBT in VAMCs.
2.4 Evidence-Based PTSD Treatment via Telemedicine
Studies that have compared telemedicine with face-to-face delivery of PTSD treatment in veteran samples have consistently found that telemedicine and as face-to-face care are equally effective (Acierno et al., in press; Egede et al., 2015; Maieritsch et al., 2015; Morland et al., 2015; Yuen et al., 2015). Previous studies have compared telemedicine to in-person modalities for the treatment of PTSD using cognitive processing therapy with Iraq/Afghanistan veterans (Maieritsch et al., 2015), cognitive processing therapy with female veterans (Morland et al., 2015), and PE among veterans in RCTs (Yuen et al., 2015) and in effectiveness settings (Gross et al., 2011; Tuerk et al., 2010). Further, in relation to attrition, a recent systematic review indicated that drop-out rates did not differ between those who were treated via telemedicine and those treated in-person across samples of veterans who served in Iraq and Afghanistan (Goetter et al., 2015). However, this review did not examine gender differences in attrition or differences based on MST status due to not having an adequate representation of women by which to examine these differences. Thus, it remains unclear if delivering MST-related PTSD treatment via HBT would result in similar clinical outcomes or attrition compared to studies examining other populations.
2.6 Intervention and Assessment Procedures
Baseline assessment procedures including informed consent are completed at our local VAMC or at one of four affiliated satellite clinics (CBOCs). Veterans are randomized 1:1 to one of two conditions: HBT or SD. To avoid potential contamination, veterans are asked not to share their materials or disclose treatment assignment to study assessment personnel, who will remain blinded to treatment condition. The active intervention phase is 12 weeks. Participants randomized to HBT receive 8-12 weekly sessions of PE via HBT, and participants randomized to SD receive 8-12 sessions of PE via standard in-person care delivery. Veterans without a home computer who are randomized to HBT receive a tablet device with LTE broadband internet connectivity capable of running the televideo encryption software. All participants are assessed in person at baseline and post-treatment; and by telephone at 3 and 6 months follow-up.
All participants complete thematic interviews at post-assessment (if willing) to inform us about their reactions, preferences, and suggestions for MST services, as well as with the mode of service delivery they received. These interviews are geared towards better understanding how PTSD services can potentially be improved for non-adherers and non-responders. These interviews are completed post-treatment to determine (a) barriers to care and (b) how well the HBT addressed these barriers. Participants who drop out will also complete a revised version of the Barriers to Therapeutic Exposure Participation Scale (Kazdin, Holland, Crowley, & Breton, 1997). Of note, missing a session does not result in classification as a dropout; sessions will be rescheduled within the same week whenever possible. Efforts to minimize attrition includes collecting additional contact information from veterans, making reminder calls for sessions, and ensuring flexibility of scheduling. Additionally, veterans receive $20 for completing the baseline assessment, $20 for completing the post-treatment assessment, $25 for completing the 3-month follow-up assessment, and $35 for completing the 6-month follow-up assessment for a combined possible total of $100.00.
2.7 Measures
Participants are screened at the outset of the study to ensure they meet inclusion and exclusion criteria related to the study hypotheses. Planned screening measures include a demographic form, the Clinician Administered PTSD Scale (CAPS; Blake et al., 1995), and the Mini-International Neuropsychiatric Interview (MINI; Sheehan et al., 1998). The CAPS is also be used to assess treatment outcome as will the PTSD Checklist (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993), and the Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996). New versions of these questionnaires referencing DSM-5 criteria will be adopted as psychometric evidence supporting their validity becomes available (e.g. the PTSD Checklist for DSM-5; Blevins, Weathers, Davis, Witte, & Domino, 2016).
2.8 Power
Our target sample size of n=100 (n = 50 per treatment condition) was selected to provide 80% power to detect a small to moderate effect size (.03) between groups. This estimate is predicated on the assumptions that data collection will occur across four time points, and with 50 veterans in each group, the study will have 81% power to detect and improvement in retention from 40% to 62% which we judged to be adequate. However, to account for the dilution effect of intent to treat analyses, anticipated dropout of some participants before treatment begins, and the anticipated need to impute some missing data, we are over-recruiting by 15%. Thus, we will enroll n=116 veterans (n=58 veterans per treatment condition) to ensure a final sample size for intent to treat analyses of n = 100.
2.9 Data Analytic Strategy
The data analytic strategy includes a mixed methods approach with both qualitative and quantitative analyses. Prior to evaluation of the primary study hypotheses, we will examine demographic variables to both identify potential confounds and determine variables associated with drop-out. Analyses at each step will rely on an intent to treat strategy (no participants will be excluded from analyses). We plan to use logistic regression to identify any meaningful relationships between missingness and treatment condition, although missing data will ultimately be imputed. A significance level of .05 will be referenced as the standard for significance in testing a priori hypotheses, and we will apply Bonferrroni corrections in secondary analyses.
Evaluation of the primary study hypotheses (i.e. that HBT will be superior to SD based on intent to treat analyses) will be accomplished using general linear mixed modeling (GLMM). This approach was selected to accommodate the different distributional assumptions underlying variables of interest (count vs. continuous variables). Values will be compared across the three outcome timepoints—immediate post-treatment, and at −3 and −6 months using Tukey-Kramer multiple comparison adjustment. Effect sizes will also be estimated to assess the clinical significance of any observed differences between the SD and HBT conditions in PTSD symptoms on the CAPS and PCL. Secondary analyses will include investigation of a treatment completers sample to compliment and help to interpret primary analysis outcomes. Completers are defined as anyone who completes at least 8 sessions or terminates early due to clinically significant improvement (1.5 standard deviation decrease) on the PCL.
Interactions (treatment group x demographic variables) will also be included in the GLMM to gauge if various demographic variables function as moderators of the treatment group/outcome relationship. Finally, process variables such as patient satisfaction and thematic interviews (i.e., qualitative data collected for treatment drop-out and non-responders) will be examined to improve the treatment of female veterans with MST-related PTSD in future clinical trials. Qualitative data from thematic interviews will also undergo content analyses using multiple coders; and both data and methods triangulation, and investigator and theory triangulation will be applied as verification strategies. We believe that the above novel study design that incorporates quantitative and qualitative data and clinical and process outcomes will allow for a comprehensive evaluation of our study hypotheses and will concomitantly serve to inform how to increase access and improve outcomes in female veterans with MST. These data, in turn, will provide valuable information to guide future directions for development of tailored PE intervention for this population or to inform the benefit of HBT delivered care for other patient populations facing similar barriers to care.
3. Discussion
MST-related PTSD is associated not only with adverse physical and emotional consequences, but also practical and financial costs for victims, families, and the annual medical costs are on average $13,460 for every veteran with a history of MST (Suris, Lind, Kashmer, Borman, & Petty, 2004). The primary objective of the current clinical trial is to assess the efficacy of PE delivered via HBT compared to PE delivered face-to-face in female veterans with MST-related PTSD. As noted previously, despite strong legislative support for veterans with MST by the VHA, there remains a significant gap in recommended policy versus service delivery practices for this veteran group. Thus, there is a significant need for novel treatment approaches that can potentially circumvent the demonstrably influential barriers to care that are unique to female veterans with MST accessing and benefiting from evidence-based treatments for PTSD.
Reducing Barriers to Treatment
As stated, female veterans with a history of MST face several unique barriers to receiving evidence-based psychotherapy for MST-related PTSD. Avoidance of anxiety-inducing external cues related to one's trauma is often a central feature of PTSD (Asmundson, Stapelton, & Taylor, 2004). The VA medical center environment is a male-dominated setting characterized by trauma cues. These cues include, but are not limited to, a patient population predominated by male patients likely to share characteristics with the MST perpetrators. For some female survivors of MST, such cues are likely to make it difficult to visit the VA once, let alone weekly. Additionally, VAMCs have traditionally served males and the majority of VAMCs have not yet provided treatment environments that would minimize barriers to care (e.g., female-only waiting rooms for privacy, separate entrances for women to prevent sexual harassment exposure from occurring; Yano et al., 2010).
There are several models for increasing treatment access when the barrier to treatment is environmentally bound. PE treatment involves developing an in vivo exposure hierarchy, where patients expose themselves to situations that trigger trauma symptoms in a graduated fashion. Thus, it would be expected in the course of PE treatment for the therapist and the patient to collaboratively develop a hierarchy to facilitate approaching rather than avoiding a triggering environment like the VA. However, PE does not call for patients to be flooded with trauma cues prior to engaging in treatment as might happen when an MST positive veteran presents to the VA. Asking female veterans to come in to the VA for PTSD treatment is not unlike asking a patient with agoraphobia to come in for treatment regularly. If they were able to come to treatment, they likely would not be in need of treatment (e.g., agoraphobia would not be interfering with functioning). Therefore, it is necessary to provide treatment to individuals without unsurmountable barriers to receiving treatment.
Strengths and Limitations
This study has several noteworthy strengths. Most broadly, it offers a potential solution to address treatment under-utilization in a high-risk population. It also provides for the systematic assessment and elimination of existing barriers to treatment ranging from the presence of trauma cues to lack of available transportation to the VA. The methodology is designed to be flexible, targeted to enhance both treatment retention and generalizability of the results. Additionally, the study team has significant experience designing and implementing telemedicine interventions, and is arguably uniquely well-suited to anticipate and address and potential problems that may arise.
Some study limitations also warrant mention. These include that at least at the outset of the study and until updated measures are validated and made available, assessment instruments will reflect DSM-IV rather than DSM-5 criteria for PTSD. Second, other studies utilizing HBT (e.g. Yuen et al., 2015) have reported some issues with connectivity and technological difficulties, especially for rural participants and during the first few sessions. Third, although participants will be briefed on the potential risks of HBT with regard to privacy, and measures will be put in place to ensure patient confidentiality, these risks cannot be completely eliminated. Fourth, because avoidance is a central feature of PTSD, concern that providing in home treatment might encourage avoidance, or that treatment gains might not generalize outside the home must be considered. However, these concerns could be addressed with the eventual integration of VA facility visits into treatment. Finally, because recruitment occurs within the VA, participants will not include those veterans for whom the barriers of coming to treatment are the most prominent: female veterans who never initiate treatment at the VA to begin with.
Implications
Aside from the potential benefits to the target population, findings from this study can have significant implications for the treatment of psychiatric disorders among other groups who face systemic barriers to accessing, engaging, or fully benefiting from treatment. For example, if this treatment is found to be more effective when delivered via HBT thereby reducing the initial exposure of trauma cues to individuals in need of trauma treatment, it is possible that other populations may benefit from this mode of treatment delivery. Specifically, it may be possible to use HBT to increase treatment access for women suffering from other physical or psychiatric difficulties associated with their MST histories. This mode of treatment delivery may also be helpful for male veterans with a history of MST. Finally, study data can also be used to legitimize the efficacy of PE delivered by-HBT for veterans who face logistical barriers such as time constraints, distance to VA facilities, etc. Similar barriers to care might include discrimination based on other factors including illegal discrimination against sexual minorities, trans populations, and racial/ethnic minorities to name a few. Although, like sexual harassment in this population, discrimination within medical treatment facilities is illegal, it may still happen and while systemic changes are occurring, it is necessary to provide individuals with ways to access care while such changes are being made.
Conclusions
The VA is the largest health organization in the world to have mandated sexual trauma screening. It has also begun to integrate telemedicine services into healthcare services. However, to date, no research has considered whether leveraging expanding VA telemedicine capabilities would lead to increased service use by female veterans and active duty personnel with MST-related PTSD, a group that underutilizes VA mental health specialty care services and is ideally suited for HBT given the unique nature of their trauma. The innovation of delivering evidence based therapy for MST-related PTSD directly into the home of active duty personnel and veterans provides a means by which to sustain force strength and diminish emotional suffering by overcoming those specific barriers of stigma and cues of MST-related memories overtly cited by women as reasons they chose not to continue receiving evidence based treatment. That is, HBT can allow veterans with MST histories to receive mental health services in a manner and location they prefer, thereby enhancing force readiness, and ultimately, reducing psychological suffering. It is important to note that this mode of treatment delivery should not take the place of reducing systemic barriers to female veterans. Instead, it should only be considered a place holder to provide treatment to women in need while reducing systemic barriers.
Acknowledgements
Data collection and manuscript preparation was supported by grants from the Department of Defense (W81XWH-14-1-0264; PI: Acierno) and from the National Institute of Mental Health (T32 MH18869, PIs: Kilpatrick & Danielson).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acierno R, Gros DF, Ruggiero K, Hernandez-Tejada MA, Knapp B, Lejuez C, Tuerk P. Behavioral activation and therapeutic exposure for post-traumatic stress disorder: A non-inferiority trial of treatment delivered in person vs. home-based telehealth. Depression and Anxiety. doi: 10.1002/da.22476. in press. [DOI] [PubMed] [Google Scholar]
- Asmundson GJ, Stapleton JA, Taylor S. Are avoidance and numbing distinct PTSD symptom clusters? Journal of Traumatic Stress. 2004;17(6):467–475. doi: 10.1007/s10960-004-5795-7. doi: 10.1007/s10960-004-5795-7. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck depression inventory-II. San Antonio: 1996. [Google Scholar]
- Beidel DC, Frueh BC, Uhde TW, Wong N, Mentrikoski JM. Multicomponent behavioral treatment for chronic combat-related posttraumatic stress disorder: A randomized controlled trial. Journal of Anxiety Disorders. 2011;25:224–231. doi: 10.1016/j.janxdis.2010.09.006. doi: 10.1016/j.janxdis.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. doi: 10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Witte TK, Davis MT. November). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evidence. Journal of Traumatic Stress. 2012;29:1–10. doi: 10.1002/jts.22059. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. The American Journal of Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Calhoun PS, Schry AR, Dennis PA, Wagner HR, Kimbrel NA, Bastian LA, Beckham JC, Kudler H, Straits-Tröster K. The association between military sexual trauma and use of VA and non-VA health care services among female veterans with military service in Iraq or Afghanistan. Journal of Interpersonal Violence. Advance online publication. 2016 doi: 10.1177/0886260515625909. doi: 10.1177/0886260515625909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee S, Rath ME, Spiro A, Eisen S, Sloan KL, Rosen AK. Gender differences in veterans’ health administration mental health service use: Effects of age and psychiatric diagnosis. Women's Health Issues. 2009;19:352. doi: 10.1016/j.whi.2009.03.002. doi: 10.1016/j.whi.2009.03.002. [DOI] [PubMed] [Google Scholar]
- Cloitre M. Effective psychotherapies for posttraumatic stress disorder: A review and critique. CNS Spectrums. 2009;13:32–43. [PubMed] [Google Scholar]
- Darling JE, Hamilton AB, Canelo IA, Haskell S, Yano EA. Women Veterans’ experience of stranger harassment at VA medical centers.. Paper presented at the national meeting of VA HSR&D / QUERI; Philadelphia, PA.. Jul, 2015. [Google Scholar]
- Department of Veterans Affairs and Department of Defense VA/DoD Clinical Practice Guideline for Management of Post-Traumatic Stress. 2010 Retrieved from: http://www.healthquality.va.gov/guidelines/MH/ptsd/cpg_PTSD-FULL-201011612.pdf.
- Egede LE, Acierno R, Knapp RG, Lejuez C, Hernandez-Tejada M, Payne EH, Frueh BC. Psychotherapy for depression in older veterans via telemedicine: a randomized, open-label, non-inferiority trial. The Lancet Psychiatry. 2015;2(8):693–701. doi: 10.1016/S2215-0366(15)00122-4. doi: 10.1016/s2215-0366(15)00122-4. [DOI] [PubMed] [Google Scholar]
- Foa E, Hembree E, Rothbaum BO. PE for PTSD: Emotional processing of traumatic events, therapist guide. Oxford University Press; New York: 2007. [Google Scholar]
- Foa E, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59(5):715. doi: 10.1037//0022-006x.59.5.715. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Fortney JC, Pyne JM, Turner EE, Farris KM, Normoyle TM, Avery MD, Hilty DM, Unützer J. Telepsychiatry integration of mental health services into rural primary care settings. International Review of Psychiatry. 2015;27:525–539. doi: 10.3109/09540261.2015.1085838. doi: 10.3109/09540261.2015.1085838. [DOI] [PubMed] [Google Scholar]
- Frayne SM, Skinner KM, Sullivan LM, Tripp TJ, Hankin CS, Kressin NR, Miller DR. Medical profile of women Veterans Administration outpatients who report a history of sexual assault occurring while in the military. Journal of Women's Health & Gender-Based Medicine. 1999;8(6):835–845. doi: 10.1089/152460999319156. doi: 10.1089/152460999319156. [DOI] [PubMed] [Google Scholar]
- Frueh BC, Turner SM, Beidel DC. Exposure therapy for combat-related PTSD: A critical review. Clinical Psychology Review. 1995;15(8):799–817. doi: 10.1016/0272-7358(95)00049-6. [Google Scholar]
- Goetter EM, Bui E, Ojserkis RA, Zakarian RJ, Brendel RW, Simon NM. A Systematic Review of Dropout From Psychotherapy for Posttraumatic Stress Disorder Among Iraq and Afghanistan Combat Veterans. Journal of Traumatic Stress. 2015;28(5):401–409. doi: 10.1002/jts.22038. doi: 10.1002/jts.22038. [DOI] [PubMed] [Google Scholar]
- Gros DF, Yoder M, Tuerk PW, Lozano BE, Acierno R. Exposure therapy for PTSD delivered to veterans via telehealth: Predictors of treatment completion and outcome and comparison to treatment delivered in person. Behavior Therapy. 2011;42(2):276–283. doi: 10.1016/j.beth.2010.07.005. doi: 10.1016/j.beth.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Haskell SG, Mattocks K, Goulet JL, Krebs EE, Skanderson M, Leslie D, Justice A, Yano E, Brandt C. The burden of illness in the first year home: Do male and female VA users differ in health conditions and healthcare utilization. Women's Health Issues. 2011;21(1):92–97. doi: 10.1016/j.whi.2010.08.001. doi: 10.1016/j.whi.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez-Tejada MA, Zoller JS, Ruggiero KJ, Kazley AS, Acierno R. Early Treatment Withdrawal from Evidence-Based Psychotherapy for PTSD: Telemedicine and in-Person Parameters. The International Journal of Psychiatry in Medicine. 2014;48(1):33–55. doi: 10.2190/PM.48.1.d. doi: 10.2190/pm.48.1.d. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine Treatment of PTSD: An Assessment of the Evidence. 2007 Retrieved from: https://iom.nationalacademies.org/~/media/Files/Report%20Files/2007/Treatment-of-PTSD-An-Assessment-of-The-Evidence/PTSDReportBriefFINAL2.pdf.
- Kang H, Dalager N, Mahan C, Ishii E. The role of sexual assault on the risk of PTSD among Gulf War veterans. Annals of Epidemiology. 2005;15(3):191–195. doi: 10.1016/j.annepidem.2004.05.009. doi: 10.1016/j.annepidem.2004.05.009. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Holland L, Crowley M, Breton S. Barriers to treatment participation scale: Evaluation and validation in the context of child outpatient treatment. Journal of Child Psychology and Psychiatry. 1997;38:1051–1062. doi: 10.1111/j.1469-7610.1997.tb01621.x. [DOI] [PubMed] [Google Scholar]
- Kimerling R, Street AE, Gima K, Smith MW. Evaluation of universal screening for military-related sexual trauma. Psychiatric Services. 2008;59(6):635–640. doi: 10.1176/ps.2008.59.6.635. doi: 10.1176/appi.ps.59.6.635. [DOI] [PubMed] [Google Scholar]
- Kimerling R, Street AE, Pavao J, Smith MW, Cronkite RC, Holmes TH, Frayne SM. Military-related sexual trauma among Veterans Health Administration patients returning from Afghanistan and Iraq. American Journal of Public Health. 2010;100(8):1409. doi: 10.2105/AJPH.2009.171793. doi: 10.2105/ajph.2009.171793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klingensmith K, Tsai J, Mota N, Southwick SM, Pietrzak RH. Military sexual trauma in US veterans: Results from the National Health and Resilience in Veterans Study. Journal in Clinical Psychiatry. 2015;75:e1133–1139. doi: 10.4088/JCP.14m09244. doi: 10.4088/JCP.14m09244. [DOI] [PubMed] [Google Scholar]
- Maieritsch KP, Smith TL, Hessinger JD, Ahearn EP, Eickhoff JC, Zhao Q. Randomized controlled equivalence trial comparing videoconference and in person delivery of cognitive processing therapy for PTSD. Journal of Telemedicine and Telecare. 2015 doi: 10.1177/1357633X15596109. epub ahead of print. doi: 10.1177/1357633X15596109. [DOI] [PubMed] [Google Scholar]
- Maguen S, Ren L, Bosch JO, Marmar CR, Seal KH. Gender differences in mental health diagnoses among Iraq and Afghanistan veterans enrolled in veterans affairs health care. American Journal of Public Health. 2010;100(12):2450–2456. doi: 10.2105/AJPH.2009.166165. doi: 10.2105/ajph.2009.166165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland LA, Mackintosh MA, Rosen CS, Willis E, Resick P, Chard K, Frueh BC. Telemedicine versus in-person delivery of cognitive processing therapy for women with posttraumatic stress disorder: A randomized noninferiority trial. Depression and Anxiety. 2015;32(11):811–820. doi: 10.1002/da.22397. doi: 10.1002/da.22397. [DOI] [PubMed] [Google Scholar]
- National Institute of Standards and Technology (NIST Federal informational processing standards 140-2. 2002 Retreived from: http://csrc.nist.gov/publications/fips/fips140-2/fips1401.pdf.
- Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review. 2010;30(6):635–641. doi: 10.1016/j.cpr.2010.04.007. doi: 10.1016/j.cpr.2010.04.007. [DOI] [PubMed] [Google Scholar]
- Resnick HS. Psychometric review of trauma assessment for adults (TAA). Measurement of Stress, Trauma, and Adaptation. 1996:362–365. [Google Scholar]
- Ruzek JI, Rosen RC. Disseminating evidence-based treatments for PTSD in organizational settings: A high priority focus area. Behaviour Research and Therapy. 2009;47(11):980–989. doi: 10.1016/j.brat.2009.07.008. doi: 10.1016/j.brat.2009.07.008. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, Bernardy N. Cognitive behavioral therapy for posttraumatic stress disorder in women: a randomized controlled trial. JAMA. 2007;297(8):820–830. doi: 10.1001/jama.297.8.820. doi:10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Skinner KM, Kressin N, Frayne S, Tripp TJ, Hankin CS, Miller DR, Sullivan LM. The prevalence of military sexual assault among female Veterans' Administration outpatients. Journal of Interpersonal Violence. 2000;15(3):291–310. doi: 10.1177/088626000015003005. [Google Scholar]
- Stander VA, Thomsen CJ. Sexual harassment and assault in the U.S. military: A review of policy and research trends. Military Medicine. 2016;181:1–20. doi: 10.7205/MILMED-D-15-00336. doi: 10.7205/MILMED-D-15-00336. [DOI] [PubMed] [Google Scholar]
- Surís A, Lind L. Military sexual trauma: A review of prevalence and associated health consequences in veterans. Trauma, Violence, & Abuse. 2008;9:250–269. doi: 10.1177/1524838008324419. doi: 10.1177/1524838008324419. [DOI] [PubMed] [Google Scholar]
- Surís A, Lind L, Kashner TM, Borman PD, Petty F. Sexual assault in women veterans: an examination of PTSD risk, health care utilization, and cost of care. Psychosomatic Medicine. 2004;66(5):749–756. doi: 10.1097/01.psy.0000138117.58559.7b. doi: 10.1177/0886260506295347. [DOI] [PubMed] [Google Scholar]
- Surís A, Lind L, Kashner TM, Borman PD. Mental health, quality of life, and health functioning in women veterans differential outcomes associated with military and civilian sexual assault. Journal of Interpersonal Violence. 2007;22(2):179–197. doi: 10.1177/0886260506295347. doi: 10.1097/01.psy.0000138117.58559.7b. [DOI] [PubMed] [Google Scholar]
- Tiet QQ, Leyva YE, Blau K, Turchik JA, Rosen CS. Military sexual assault, gender, and PTSD treatment outcomes of US Veterans. Journal of Traumatic Stress. 2015;28(2):92–101. doi: 10.1002/jts.21992. doi: 10.1002/jts.21992. [DOI] [PubMed] [Google Scholar]
- Tuerk PW, Yoder M, Ruggiero KJ, Gros DF, Acierno R. A pilot study of prolonged exposure therapy for posttraumatic stress disorder delivered via telehealth technology. Journal of Traumatic Stress. 2010;23(1):116–123. doi: 10.1002/jts.20494. doi: 10.1002/jts.20494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veterans Health Administration Military sexual trauma. 2015 doi: 10.2105/AJPH.2006.092999. Retrieved from http://www.mentalhealth.va.gov/docs/mst_general_factsheet.pdf. [DOI] [PMC free article] [PubMed]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) 2013 doi: 10.1037/pas0000486. Interview available from the National Center for PTSD at www.ptsd.va.gov. [DOI] [PMC free article] [PubMed]
- Yano EM, Hayes P, Wright S, Schnurr PP, Lipson L, Bean-Mayberry B, Washington DL. Integration of women veterans into VA quality improvement research efforts: What researchers need to know. Journal of General Internal Medicine. 2010;25(Suppl 1):56–61. doi: 10.1007/s11606-009-1116-4. doi: 10.1007/s11606-009-1116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen EK, Gros DF, Price M, Zeigler S, Tuerk PW, Foa EB, Acierno R. Randomized Controlled Trial of Home-Based Telehealth Versus In-Person Prolonged Exposure for Combat-Related PTSD in Veterans: Preliminary Results. Journal of Clinical Psychology. 2015;71(6):500–512. doi: 10.1002/jclp.22168. doi :10.1002/jclp.22168. [DOI] [PubMed] [Google Scholar]


