Abstract
Brexpiprazole (Rexulti): a new monotherapy for schizophrenia and adjunctive therapy for major depressive disorder
INTRODUCTION
Mental health disorders affect approximately one in five adults in a given year. In the United States, approximately 1% of adults live with schizophrenia, and nearly 7% of adults have experienced at least one major depressive episode.1
The Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5), defines schizophrenia as having two or more of the following symptoms for a substantial amount of time during a one-month period that leads to a significant decrease in level of functioning. The symptoms include grossly disorganized or catatonic behavior, negative symptoms (i.e., avolition or reduced emotional expression), and at least one of these symptoms: delusions, hallucinations, or disorganized speech.2
Scientists correlate several genetic and environmental factors to alterations in neurohormonal balance and brain structure that lead to the development of schizophrenia; however, more research must be completed before the actual cause of schizophrenia can be defined. The symptomatology of schizophrenia has been well defined and focuses on three categories encompassing positive symptoms (i.e., hallucinations, delusions, disorganization), negative symptoms (i.e., anhedonia, flat affect), and cognitive symptoms (i.e., difficulties with concentration and executive functioning). Currently, there are more than 20 pharmacotherapeutic options for the treatment of schizophrenia that center on first-generation and second-generation antipsychotic therapy.3,4
Major depressive disorder (MDD) is another debilitating disorder that centers on mood dysregulation.5,6 The DSM-5 defines the diagnostic criteria for this disorder as having five or more of the following symptoms for at least a two-week period that represents a change from previous function. The symptoms include insomnia or hypersomnia, feelings of inappropriate guilt or worthlessness, loss of energy, diminished ability to concentrate, weight loss or weight gain, psychomotor retardation or agitation, suicidal ideation, and at least one of these symptoms: depressed mood or anhedonia.2 MDD has been linked with genetic, biological, environmental, and physiological factors that affect individuals differently.5,6
On July 10, 2015, the Food and Drug Administration (FDA) approved brexpiprazole (Rexulti, Otsuka Pharmaceuticals) for the treatment of schizophrenia and as adjunctive therapy for MDD.7 The suggested mechanism of brexpiprazole is thought to be due to effects on dopamine and serotonin receptors. The receptor selectivity of brexpiprazole is theorized to be an advantage because it displays partial agonism on specific dopamine and serotonin receptors while also antagonizing other serotonin receptors. The proposed differentiation of brexpiprazole from aripiprazole is the level of binding and intrinsic potency on D2 receptors and higher potency on 5-HT1A and 5-HT2A receptors. In addition, there may be other differences based on its receptor profile, and how these differences translate to efficacy or tolerability is still to be determined.
CHEMICAL PROPERTIES
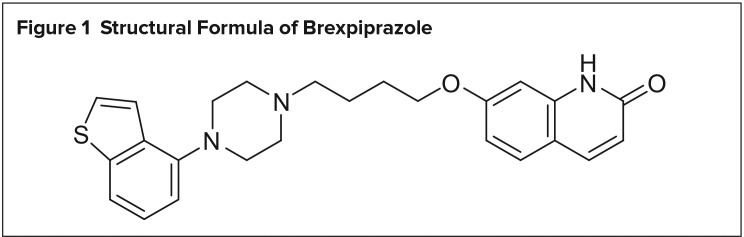
Brexpiprazole is a 5-HT1A, D2, and D3 partial agonist and a 5-HT2A, 5-HT2B, 5-HT7, alpha1A, alpha1B, alpha1D, and alpha2C antagonist with a chemical formula of 7-{4-[4-(1-Benzothiophen-4-yl) piperazin-1-yl]butoxy}quinolin-2(1H)-one. The inactive ingredients consist of lactulose monohydrate, cornstarch, microcrystalline cellulose, hydroxypropyl cellulose, low-substituted hydroxypropyl cellulose, magnesium stearate, hypromellose, talc, and colorants of titanium dioxide, iron oxide, and ferrosferric oxide. Brexpiprazole is a round tablet available in six strengths ranging from 0.25 mg to 4 mg.8
Figure 1 illustrates the drug’s structural formula.
Figure 1.
Structural Formula of Brexpiprazole
MECHANISM OF ACTION
The specific mechanism of action of brexpiprazole is currently unknown for use in schizophrenia and MDD. A suggested mechanism related to partial agonism of 5-HT1A and D2 receptors and antagonism of 5-HT2A may mediate its efficacy. Brexpiprazole binds with high affinity to numerous monoaminergic receptors encompassing D2, D3, 5-HT1A, 5-HT2A, 5-HT2B, and 5-HT7 with Ki values of 0.3 nM, 1.1 nM, 0.12 nM, 0.47 nM, 1.9 nM, and 3.7 nM, respectively. Noradrenergic alpha1A (3.8 nM), alpha1B (0.17 nM), alpha1D (2.6 nM), and alpha2C (0.59 nM) receptors are bound with the corresponding affinities by brexpiprazole. Additionally, it has low affinity for muscarinic M1 and histamine H1 receptors.8–11 Table 1 summarizes the differences between brexpiprazole and aripiprazole.8,12
Table 1.
| Brexpiprazole | Aripiprazole | |
|---|---|---|
| FDA-approved indications |
|
|
| Predominant receptor binding | 5-HT1A, D2, D3 partial agonist and 5-HT2A, 5-HT2B, 5-HT7, alpha1A, alpha1B, alpha1D, and alpha2C antagonist | D2 and 5-HT1A partial agonist and 5-HT2A antagonist |
| Predominant metabolism | CYP2D6 and CYP3A4 | CYP2D6 and CYP3A4 |
| Adverse events | Akathisia, weight gain, constipation, fatigue, somnolence, headache, tremor, dizziness, dyspepsia, and extrapyramidal symptoms | Akathisia, headache, weight gain, sedation, somnolence, dizziness, tremor, and extrapyramidal symptoms |
INDICATIONS AND DOSAGE
Brexpiprazole is FDA-approved for the treatment of schizophrenia with dose initiation starting at 1 mg once daily and titration to a target dose of 2 mg to 4 mg once daily. The titration schedule involves starting at 1 mg once daily for days 1 to 4, increasing to 2 mg once daily on days 5 to 7, and ending at 4 mg once daily on day 8 based upon the patient’s tolerability and clinical response. Based on the two studies to be discussed, the maximum recommended daily dose of brexpiprazole for the treatment of schizophrenia is 4 mg.8
Furthermore, brexpiprazole is approved as an adjunctive treatment with antidepressants for MDD. Dose initiation is recommended at 0.5 mg or 1 mg once daily, then increasing weekly to a target dose of 2 mg based on the patient’s tolerability and clinical response. When it is used as adjunctive treatment for MDD, the maximum recommended daily dose is 3 mg.8
For either indication, brexpiprazole should be taken orally and can be administered with or without food. Dosage adjustments are necessary in patients with hepatic or renal impairment. In patients with moderate-to-severe hepatic impairment (Child–Pugh score of 7 or more), the maximum daily dose for patients with schizophrenia or MDD is 3 mg and 2 mg, respectively. The maximum recommended daily dose in patients with moderate, severe, or end-stage renal impairment (creatinine clearance of less than 60 mL/minute) is 3 mg for treatment of schizophrenia and 2 mg for patients with MDD.8
PHARMACOKINETICS
After oral administration of brexpiprazole tablets, brexpiprazole is absorbed in the gastrointestinal tract, and within four hours, peak plasma concentrations can be seen. Oral bioavailability of brexpiprazole is approximately 95%, and steady-state concentrations are achieved within 10 to 12 days of initiation. Consumption with food does not affect the bioavailability of brexpiprazole, and no significant effect on maximum concentration and area under the curve was observed. Brexpiprazole is highly protein-bound; however, renal and hepatic impairment do not affect binding.8
Brexpiprazole is mainly metabolized by cytochrome P450 (CYP) 2D6 and CYP3A4 and has demonstrated no effect on inducing or inhibiting any CYP 450 isoenzymes. These CYP enzymes metabolize brexpiprazole into its major metabolite DM-3411. No therapeutic effects have been attributed to DM-3411. The half-life of brexpiprazole is 91 hours. Brexpiprazole is excreted in the urine (25%) and feces (46%) with a negligible amount excreted unchanged in the urine. Key pharmacokinetic measures are summarized in Table 2.8
Table 2.
Pharmacokinetics of Brexpiprazole8
| Oral bioavailability | 95% |
| Time to peak plasma concentration | 4 hours |
| Metabolic pathway | CYP3A4, CYP2D6, CYP1A1/1A2, CYP2A6, CYP2B6, CYP2C8/2C9, CYP2C19, CYP2E1 |
| Terminal half-life | 91 hours |
| Protein binding | > 99% |
| Elimination | Approximately 25% in urine and 46% in feces |
DRUG INTERACTIONS
Major drug interactions can be seen with brexpiprazole due to the molecule being a substrate of CYP3A4 and CYP2D6. For patients who are poor CYP2D6 metabolizers or are taking a strong CYP2D6 or CYP3A4 inhibitor, half of the usual dose should be administered. In patients taking a strong or moderate CYP2D6 inhibitor with a strong or moderate CYP3A4 inhibitor, a quarter of the usual dose should be given. Likewise, for patients who are poor CYP2D6 metabolizers and are taking a strong/moderate CYP3A4 inhibitor, a quarter of the usual dose should be administered. Any patients taking a strong CYP3A4 inducer should be administered double the usual dose over one to two weeks. No adjustments are necessary for agents that inhibit P-glycoprotein transportation. Gastric acidity is not involved in the metabolism of brexpiprazole.8
CLINICAL TRIALS
The efficacy and safety of brexpiprazole were assessed in several published placebo-controlled clinical trials. The first two studies summarized in this section discuss the drug’s efficacy and safety in the treatment of schizophrenia and the last two trials discuss its efficacy and safety as an adjunctive treatment for MDD.
Kane et al.13
This multicenter, double-blind, randomized, placebo-controlled, phase 3 study evaluated the efficacy, tolerability, and safety of fixed-dose brexpiprazole (1 mg, 2 mg, or 4 mg) versus placebo in patients 18 to 65 years of age with a diagnosis of schizophrenia who were currently experiencing an acute exacerbation of symptoms. Additional inclusion criteria consisted of patients: with a discernible worsening of usual function and psychotic symptoms; who would benefit from hospitalization; with a Clinical Global Improvement–Severity Scale (CGI–S) score of 4 or higher, a total Brief Psychiatric Rating Scale (BPRS) score of 40 or more, or a score of 4 or higher on two or more BPRS items (unusual thought content, hallucinatory behavior, suspiciousness, or conceptual disorganization); and with history of symptom exacerbation and/or relapse when not receiving antipsychotic therapy. Patients were excluded from the study if they had a current DSM-IV-TR (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition–Text Revision) Axis I diagnosis that was not schizophrenia, presentation of first-episode schizophrenia, severe akathisia, tardive dyskinesia qualifying as clinically significant, and a history within the past 180 days of substance abuse. Eligible patients were randomly assigned to receive brexpiprazole (1 mg, 2 mg, or 4 mg) or placebo in a 2:3:3:3 ratio.
The primary efficacy outcome was change in the Positive and Negative Syndrome Scale (PANSS) from baseline to week 6. Secondary outcomes encompassed change from baseline at week 6 in CGI-S score, PANSS positive and negative subscales, PANSS excited component, Clinical Global Impression–Improvement (CGI-I) score, Personal and Social Performance Scale (PSP) scores, and Marder factor scores. Furthermore, response rates and rate of discontinuation due to lack of efficacy were assessed. Safety and tolerability endpoints were evaluated throughout and after the six-week study.
A total of 674 patients were enrolled and randomized in this study. At week 6, there was a statistically significant reduction from baseline in PANSS total score with the use of brexpiprazole 4 mg compared to placebo (least-squares [LS] mean difference, −6.47; P = 0.0022). There was numerical improvement in PANSS total score with brexpiprazole 1 mg and 2 mg compared with placebo, but this did not reach statistical significance (LS mean difference, −3.37, P = 0.1588; and −3.08, P = 0.1448, respectively). Formal statistical testing was not conducted on the secondary endpoints because the comparison of brexpiprazole 4 mg to placebo was the only one that met the predefined threshold in the primary analysis. Akathisia onset (4.2%–6.5%) was most frequently reported during the first three weeks of treatment. Other frequently reported treatment-emergent adverse effects were weight gain (10%–12.2% experienced a 7% increase or more from baseline), increased creatine phosphokinase levels (7.7%–9.6%), and sedation (1.7%–3.3%).
Correll et al.14
This was a six-week, double-blind, randomized, placebo-controlled trial that assessed the efficacy, tolerability, and safety of fixed-dose brexpiprazole (0.25 mg, 2 mg, and 4 mg daily) compared to placebo in adults 18 to 65 years of age with a current acute exacerbation of schizophrenia. Patients were included in the study if they had a DSM-IV-TR diagnosis of schizophrenia, if they were currently experiencing an acute exacerbation of psychotic symptoms, and if hospitalization would be beneficial. Exclusion criteria consisted of a DSM-IV-TR Axis I diagnosis excluding schizophrenia, diagnosis of first-episode schizophrenia, history within the past 180 days of substance abuse, tardive dyskinesia qualifying as clinically significant, or a medical condition considered clinically significant. Participants were randomly assigned to receive 0.25 mg, 2 mg, or 4 mg brexpiprazole or placebo once daily in a 1:2:2:2 ratio. Dosages of 2 mg and 4 mg of brexpiprazole were titrated at initiation of the trial.
The primary endpoint was change from baseline to week 6 in PANSS total score. Secondary endpoints were change from baseline to week 6 in the PANSS positive and negative symptom subscale scores, PANSS score on the excited component, CGI-S rating, CGI-I rating, and PSP score. Additional outcomes measured at week 6 were rate of response and discontinuation rate due to lack of efficacy. Safety and tolerability outcomes were assessed throughout the study.
A total of 636 patients made up the safety population and 632 patients comprised the efficacy population. The primary efficacy outcome was statistically significant for the 2-mg and 4-mg doses of brexpiprazole at week 6 (P < 0.0001 and P = 0.0006, respectively). A mean change in the CGI-S score from baseline at week 6 was statistically significant in both the 2-mg and 4-mg brexpiprazole groups compared to placebo. Similarly, other secondary efficacy endpoints that reached statistical significance from baseline to week 6 in the brexpiprazole 2-mg and 4-mg groups were PANSS positive and negative subscales and PANSS excited component score. In the 2-mg and 4-mg brexpiprazole arms, responder rates were higher than in the placebo arm (P < 0.05); however, only the 4-mg brexpiprazole group demonstrated significance in discontinuation due to lack of efficacy (P = 0.02). The most common reported adverse effect with the use of brexpiprazole was akathisia. Additional adverse effects reported throughout the study were increased body weight and changes in metabolic parameters.
Thase et al.15
In a phase 3, randomized, placebo-controlled trial, brexpiprazole 1 mg and 3 mg were evaluated for efficacy, safety, and tolerability as an augmentation therapy to antidepressant treatments in adults who were 18 to 65 years of age and met the DSM-IV-TR criteria for major depressive disorder without psychotic features (single or recurrent). Additional inclusion criteria encompassed having major depressive disorder for at least eight weeks, reporting an inadequate response to a trial of one to three antidepressants, and a Hamilton Depression Rating Scale (HDRS-17) score of 18 or higher at screening and on the first day of treatment. An inadequate response to antidepressant therapy is outlined as a 50% or less reduction in symptoms based on self-reports on the Massachusetts General Hospital Antidepressant Treatment Response Questionnaire (ATRQ). Exclusion criteria consisted of various concomitant medication regulations. Patients received one of the following antidepressants during the eight-week treatment phase: fluoxetine, duloxetine, paroxetine controlled-release, escitalopram, venlafaxine extended-release, or sertraline. All antidepressants were titrated to the maximal tolerated dose. Randomization occurred in a 1:1:1 manner to brexpiprazole 1 mg, brexpiprazole 3 mg, or placebo for six weeks in addition to antidepressant therapy.
A total of 669 patients were evaluated for the primary efficacy endpoint of mean reduction in Montgomery-Asberg Depression Rating Scale (MADRS) total score from baseline to week 6. Brexpiprazole 3 mg demonstrated a statistically significant reduction in MADRS total score from baseline compared to placebo in the per-final-protocol efficacy population (LS mean difference, −1.95; P = 0.0079). CGI-I-defined response rate, CGI-I, and MADRS-defined response rate at week 6 showed greater improvement in the brexpiprazole 3-mg group compared to placebo. In addition, at week 6, MADRS-defined response rate and CGI-I demonstrated improvement in the brexpiprazole 1-mg group; however, brexpiprazole 1 mg did not reach statistical significance in reducing MADRS total score from baseline. Treatment-emergent adverse events frequently reported during the study (more than 5%) were nasopharyngitis, headache, weight gain, akathisia, somnolence, and tremor.
Thase et al.16
A phase 3, randomized, placebo-controlled efficacy and safety study was conducted evaluating the use of brexpiprazole 2 mg adjunctively with antidepressant therapy in adults 18 to 65 years of age with a DSM-IV-TR diagnosis of major depressive disorder without psychosis who had an inadequate response to prior antidepressant treatment. Patients were included if they met criteria for a single or recurrent episode of MDD that was at least eight weeks in duration, received an adequate trial of one to three antidepressants and self-reported an inadequate response (outlined as less than a 50% reduction in ATRQ score), and had a score of 18 or more on the HDRS-17 scale at screening and on the first day of treatment. This fixed-dose study involved a single-blind treatment component that continued for eight weeks and then transitioned into the six-week double-blind, randomized trial comparing brexpiprazole and placebo. One of the following anti depressants was used during the eight-week treatment phase: fluoxetine, duloxetine, paroxetine controlled-release, escitalopram, venlafaxine extended-release, or sertraline. All antidepressants were titrated to the maximal tolerated dose. Randomization to antidepressant therapy and placebo or antidepressant therapy and brexpiprazole was completed in a 1:1 ratio.
The MADRS, HDRS-17, CGI-S, and CGI-I were assessed for efficacy endpoints. A total of 371 patients were included in the efficacy population while 353 patients were included in the efficacy population per final protocol. Brexpiprazole demonstrated a significant reduction from baseline in MADRS score compared with placebo in the efficacy population and efficacy population per final protocol group (LS mean difference, −3.12, P = 0.0001; and −3.21, P = 0.0002, respectively). Furthermore, there was a statistically significant improvement in the brexpiprazole group in HDRS-17, CGI-S, and CGI-I scores compared to placebo. According to the safety and tolerability assessments, the most frequently reported treatment-emergent adverse effects with brexpiprazole were weight gain (8%) and akathisia (7.4%). No suicides, attempted suicides, or deaths were reported throughout the study.
ADVERSE DRUG REACTIONS
Common adverse drug events associated with brexpiprazole in pooled clinical trials for MDD were akathisia, weight gain, constipation, fatigue, somnolence, headache, tremor, and dizziness. Anxiety and restlessness were also reported. Results from pooled clinical trial data for schizophrenia demonstrated a higher incidence of akathisia, tremor, sedation, dyspepsia, and weight gain. Diarrhea and increased blood creatine phosphokinase were also documented. The occurrence of extrapyramidal symptoms and dystonic reactions, excluding akathisia, with brexpiprazole treatment was greater than with placebo in both MDD and schizophrenia.8,13–16
CONTRAINDICATIONS
In patients with a known hypersensitivity to brexpiprazole or any of its components, administration is contraindicated. Reactions have involved facial swelling, rash, urticaria, and anaphylaxis.8
WARNINGS AND PRECAUTIONS
Brexpiprazole is categorized as an antipsychotic medication, and this class of agents has been associated with an increased risk of mortality in elderly patients with dementia-related psychosis. In addition, placebo-controlled trials demonstrated a higher incidence of cerebro-vascular events, including stroke, in this patient population. Brexpiprazole should not be used in patients with dementia-related psychosis.8
As a result of brexpiprazole’s antidepressant activity, there is a concern of worsening suicidal thoughts and behaviors in children, adolescents, and young adults. Monitoring for worsening of symptoms is recommended, especially in the initial few months of treatment. Patient caregivers should be counseled on this possible change in behavior and should understand when to alert health care professionals.8
Additional warnings for brexpiprazole encompass neuroleptic malignant syndrome, tardive dyskinesia, exacerbation of metabolic parameters, orthostatic hypotension, dysregulation of body temperature, seizures, and dysphagia, which is similar to other atypical anti psychotics. Motor/cognitive impairment, neutropenia, leukopenia, and agranulocytosis should be monitored with brexpiprazole therapy.8
P&T COMMITTEE CONSIDERATIONS
Based on the clinical trial data, brexpiprazole has shown itself to be effective as a treatment regimen for schizophrenia and as an adjunctive treatment regimen for major depressive disorder. When taken as directed, this agent demonstrates efficacy with a well-tolerated adverse effect profile.13–16 In regard to tolerability, the most common adverse effects reported with medication administration were weight gain and akathisia.8,13–16 Brexpiprazole has a current average wholesale price of approximately $1,122 for a 30-day supply with all doses priced the same.17 Established efficacy and safety data with brexpiprazole allows consideration of this agent as an alternative to other anti-psychotic agents for schizophrenia and as an adjunctive agent for major depressive disorder.
Footnotes
Disclosure: Dr. Rey has received honoraria from and has served on the advisory board for Otsuka America Pharmaceuticals. Dr. Eaves reports no commercial or financial interests in regard to this article.
REFERENCES
- 1.National Alliance on Mental Illness Mental health by the numbers. Available at: www.nami.org/Learn-More/Mental-Health-By-the-Numbers. Accessed August 16, 2015.
- 2.American Psychiatric Association, DSM-5 Task Force . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, D.C.: American Psychiatric Publishing; 2013. [Google Scholar]
- 3.National Institute of Mental Health Schizophrenia. Feb, 2016. Available at: www.nimh.nih.gov/health/topics/schizophrenia/index.shtml#part_145427. Accessed August 16, 2015.
- 4.Department of Health and Human Services Schizophrenia. Available at: www.mentalhealth.gov/what-to-look-for/psychotic-disorders/schizophrenia. Accessed August 16, 2015.
- 5.National Institute of Mental Health Depression. May, 2016. Available at: www.nimh.nih.gov/health/topics/depression/index.shtml. Accessed August 16, 2015.
- 6.Department of Health and Human Services Depression. Available at: www.mental-health.gov/what-to-look-for/mood-disorders/depression. Accessed August 16, 2015.
- 7.Otsuka America Pharmaceutical, Inc. U.S. FDA approves Otsuka and Lundbeck’s Rexulti (brexpiprazole) as adjunctive treatment for adults with major depressive disorder and as a treatment for adults with schizophrenia. Jul 10, 2015. Available at: www.otsuka-us.com/newsroom/Pages/NewsArticle.aspx?ItemId=13. Accessed August 17, 2015.
- 8.Rexulti (brexpiprazole) prescribing information. Rockville, Maryland: Otsuka America Pharmaceutical, Inc.; 2015. Available at: www.otsuka-us.com/products/Documents/Rexulti.PI.pdf. Accessed August 15, 2015. [Google Scholar]
- 9.Maeda K, Sugino H, Akazawa H, et al. Brexpiprazole I: in vitro and in vivo characterization of a novel serotonin-dopamine activity modulator. J Pharmacol Exp Ther. 2014;350(3):589–604. doi: 10.1124/jpet.114.213793. [DOI] [PubMed] [Google Scholar]
- 10.Maeda K, Lerdrup L, Sugino H, et al. Brexpiprazole II: antipsychotic-like and precognitive effects of a novel serotonin-dopamine activity modulator. J Pharmacol Exp Ther. 2014;350(3):605–614. doi: 10.1124/jpet.114.213819. [DOI] [PubMed] [Google Scholar]
- 11.Oosterhof CA, El Mansari M, Blier P. Acute effects of brexpiprazole on serotonin, dopamine, and norepinephrine systems: an in vivo electrophysiologic characterization. J Pharmacol Exp Ther. 2014;351(3):585–595. doi: 10.1124/jpet.114.218578. [DOI] [PubMed] [Google Scholar]
- 12.Abilify (aripiprazole) prescribing information. Rockville, Maryland: Otsuka America Pharmaceutical, Inc.; 2014. Available at: http://packageinserts.bms.com/pi/pi_abilify.pdf. Accessed August 20, 2015. [Google Scholar]
- 13.Kane JM, Skuban A, Ouyang J, et al. A multicenter, randomized, double-blind, controlled phase 3 trial of fixed-dose brexpiprazole for the treatment of adults with schizophrenia. Schizophr Res. 2015;164(1–3):127–135. doi: 10.1016/j.schres.2015.01.038. Epub 2015 Feb 12. [DOI] [PubMed] [Google Scholar]
- 14.Correll CU, Skuban A, Ouyang J, et al. Efficacy and safety of brexpiprazole for the treatment of acute schizophrenia: a 6-week randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2015;172(9):870–880. doi: 10.1176/appi.ajp.2015.14101275. Epub 2015 Apr 16. [DOI] [PubMed] [Google Scholar]
- 15.Thase ME, Youakim JM, Skuban A, et al. Adjunctive brexpiprazole 1 and 3 mg for patients with major depressive disorder following inadequate response to antidepressants: a phase 3, randomized, double-blind study. J Clin Psychiatry. 2015;76(9):1232–1240. doi: 10.4088/JCP.14m09689. [DOI] [PubMed] [Google Scholar]
- 16.Thase ME, Youakim JM, Skuban A, et al. Efficacy and safety of adjunctive brexpiprazole 2 mg in major depressive disorder: a phase 3, randomized, placebo-controlled study in patients with inadequate response to antidepressants. J Clin Psychiatry. 2015;76(9):1224–1231. doi: 10.4088/JCP.14m09688. [DOI] [PubMed] [Google Scholar]
- 17.Red Book Online . Ann Arbor, Michigan: Truven Health Analytics; Accessed May 31, 2016. [Google Scholar]