Abstract
The population residing Sub-Sahara Africa (SSA) continues to suffer from communicable health problems such as HIV/AIDS, malaria, tuberculosis, and various neglected tropical as well as non-communicable diseases. The disease burden is aggravated by shortage of medical personnel and medical supplies such as medical devices and minimal access to essential medicine. For long time, human beings through observation and practical experiences learned to use different plant species that led to the emergence of traditional medicine (TM) systems. The ancient Pharaonic Egyptian TM system is one of the oldest documented forms of TM practice in Africa and the pioneer of world’s medical science. However, the medical practices diffused very fast to other continents being accelerated by advancement of technologies while leaving Africa lagging behind in the integration of the practice in formal health-care system. Challenging issues that drag back integration is the development of education curricula for training TM experts as the way of disseminating the traditional medical knowledge and practices imbedded in African culture. The few African countries such as Ghana managed to integrate TM products in the National Essential Medicine List while South Africa, Sierra Leone, and Tanzania have TM products being sold over the counters due to the availability of education training programs facilitated by research. This paper analyses the contribution of TM practice and products in modern medicine and gives recommendations that Africa should take in the integration process to safeguard the SSA population from disease burdens.
KEY WORDS: Bantu, curricula, formal system, integration, practice, products, Sub-Sahara Africa, traditional medicine
INTRODUCTION
The Contribution of Ancient African Traditional Medicine (TM) Practices in Modern Medicine
The Sub-Sahara Africa (SSA) continues suffering from the burden of diseases despite being a rich source of biodiversity from which many hospital medicines have been tapped, and a lot more are untapped. This untapped avenue has contributed minimally in solving health problems since TM has not yet been formally integrated into the existing conventional health-care delivery [1]. The reasons being partly because there are few TM curricula that are geared to trained human resources to undertake quality services and development of materia medica used in treatments in this region. However, different countries or continents elsewhere have their TM practices supported by documented material medica and the underlying philosophy for disease diagnosis and treatments such as Unani TM, Chinese TM, Ayurvedic medicine, Naturopathy, Homoeopathy, and Korean oriental medicine [2-4]. Therefore, the philosophy and theories of disease symptoms, diagnosis, and treatment used in African TM need to be established and learned because the surge for the use of TM is now not limited to countries of origin rather a trans-territory and a choice of many people even in developed countries [5-8]. African TM practices are imbedded in the indigenous knowledge of one’s culture or society thus also serves as backups of what the local communities have maintained for centuries for their survival and prosper within their ecosystem.
In the written record, the ancient Pharaonic Egyptians medical practices are the oldest documented form of TM practice in Africa. From the beginning of the civilization in about 3300 BC until the Persian invasion in 525 BC, Egyptian medical practices were highly advanced for its time including simple non-invasive surgery, bones setting, and an extensive set of pharmacopeia in the form of papyri. The Ebers Papyrus (c. 1500 BC) is among the oldest preserved medical documents and contains some 700 magical formulas and remedies. Records show that the diagnosis of diabetes disease was described in Ebers Papyrus as disease of “urine pass through” [9]. The Edwin Smith papyrus (c. 1600 BC) includes a description of simple non-invasive surgery whereby the position of diagnosis of breast cancer and its management is described as a “tumor do thou nothing there against” [10]. Several other papyri collected in Egypt influenced TM of other traditions, including the Greeks and Romans, but later other parts of the world [11].
No much is recorded about TM practices in Africa until the 19th century when Africa was partitioned and missionaries’ works started. For example in by then Germany East Africa and British East Africa, which compose the current East Africa Community countries, one British traveller [12] witnessed cesarean section being performed by Ugandan people to serve the baby and mother. Similar reports of surgical practices were reported from Rwanda, whereby botanical preparations were used to anesthetize the patient to perform a cesarean and promote wound healing [12]. In Tanzania, the German ship’s doctor Dr. Weck, Adolf Bastian (1826-1905), W. H. R. Rivers (1864-1922), and C. G. Seligman (1873-1940) observed and wrote a number of diseases being managed by TM in the Hehe community [13,14]. These few examples of ancient indigenous practices show the significant contribution to the modern practices of diagnosis and disease management since some still hold to date.
TM in SSA
In Africa, the Bantu-speaking peoples make up a major part of the population of nearly all African countries south of the Sahara. They belong to over 300 groups, each with its own language or dialect [15]. Despite the diverse culture and ethnic groups in SSA, still, most societies are dominated by the Bantu culture and believe [15]. Therefore, TM in the SSA region is rational in the context of Bantu cultures and is like theories in western medicine. The Bantu believes a human being is holistic yet corporate, in terms of the family, clan and whole ethnic group. Therefore, it is required never to do harm to the patient unless it is in his or her best interests or for the good of the community because if he suffers, he does not suffer alone but with his corporate group: When he rejoices, he is not alone but with his kinsmen, neighbors, and relatives. In the modern health-care system, this is a principle worth emulating; never to do harm to a patient unless the nurse or doctor, after serious consideration, believes that it is in the interests of the patient or it is necessary for the protection of other patients or the public [16-18]. The African Union Commission adopted the WHO/Afro (1976) definition of African TM as the total of all practices, measures, ingredients, and procedures of all kind whether material or not which guard against disease/illness to alleviate suffering and cure himself [19]. Thus, African TM does not regard man as a purely physical entity but also takes into consideration the sociological (family or other), whether living or dead (ancestors) and the “intangible forces” (God, gods,) of the universe [19,20]. Thus, disease is not merely a result of dysfunction of an organ caused by the invasion of microscopic organisms (Germ theory) but also may be due to intangible forces. Therefore, treatment in African TM is by use of both material substances and resources drawn from the cosmic world all together not separated (Holistic theory) in an attempts to restore a state of wholesomeness using various methods including plant remedies [19,20].
Interdependence of Traditional and Modern Medicine
The pharaonic pharmacopeia papyri described several plants including the bark of the willow tree, in which Hippocrates (° 460-370 B.C.) who is acknowledged as a father of western medicine used to control headaches and other body pains [21]. It was through chemistry, the active molecule which is salicylic acid was identified, in 1889, and later aspirin, paracetamol, diclofenac, mefenamic acid, ibuprofen, etc., were synthesized based on the structure of salicylic acid [21,22]. Several other useful hospitals medicines and vaccination, such as quinine, ephedrine, amodiaquine, primaquine, chloroquine, mefloquine, atropine, reserpine, digoxin, tubocurarine, metformin, Scopolamine, taxol, and calanolide A, are now synthetically made from a structure of an initial naturally isolated compound from medicinal plants while others are semi-synthetically derived from the natural product precursors [22,23]. Several medicinal plants, such as Madagascar’s rosy periwinkle Catharansus roseus, remain the basic source of anticancer drugs vincristine and vinblastine [23]. This indicates the potential of medicinal plants and its current contribution to hospital medicine, in which most of these are an essential medicine dispensed worldwide for treatment of different diseases. This confirms the contribution of both modern and TM in the advancement of the current health systems not only in SSA but worldwide.
Opportunities and Challenges to Promote TM Practices and Products in SSA
The contribution of TM and its practitioners was recognized, in 1978, by the Alma-Ata Declaration as important resources in achieving health for all by the year 2000 [24]. A number of resolutions and declarations have been adopted by the WHO governing bodies at regional and global levels including Resolution AFR/RC49/R5 on Essential Drugs in the WHO African Region. The resolution required the WHO to support Member States to carry out research on medicinal plants and to promote their use in health-care delivery systems [25]. The Regional Committee that adopted resolution AFR/RC49/R5 also called on the WHO to develop a comprehensive strategy on African TM with the focus on producing evidence [25-27]. Since then, African countries have been supporting these initiatives in different ways such as documenting ethnobiomedical information, scientific evidence/research, media promotion, implementing international and national plans and policies including the plan of action on the decade of TM for (2001-2010) that was extended to cover the period 2010-2020 [28,29]. Indeed, African Nations are aligning to these international plans to pull efforts of promoting TM uses including developing robust policies and legislatives. Further, many African countries are signatories to the TRIPs 1994, CBD 1998, and Nagoya Protocol 2010, which require governments to put mechanisms for recognition and protection of the vast available local knowledge and associated used genetic materials including those in TM. This is the commendable direction taken in addressing the rights of traditional knowledge holders whom for centuries have transmitted this knowledge orally thus continued exposing the region in a risk of biopiracy and that some knowledge became forgotten or lost during oral transmission. The ethnobiomedical information originating from African culture could be appropriately coordinated and disseminated through formal training and research to bring about reliability and allow adoption for sustainability of the TM services that benefit the majority of the SSA population. Notably, only a few apprenticeships and formal training can be traced in SSA.
METHODOLOGY
The current review intends to appraise the trend and situation of African TM education training curricula in SSA as one element in the integration process in the formal health-care system. Analytical methodology used for this appraisal was through internet search from Google, Google Scholar, PubMed, HINARI, ISI, Global health training center, and Popline (K4 Health) database using the terms or key words: Curriculum or courses, or program in traditional or herbal medicine in Africa alone and combination. In additional terms such as degree, college, SSA, or country names were used in combination with the search titles. A manual evaluation of searched titles and reference lists of relevant studies and reviews was also conducted. Furthermore, all articles related to the subject were selected and web-link or the authors’ affiliation to view the institutional webpage whether they offer any course or training program in TM. Basic courses or program in phytochemistry, pharmacognosy, natural products chemistry, and phytomedicine are not included in this appraisal because it is a science of the materia medica without necessarily having a reflection on two key characteristic aspects of TM, that is, practices accompanied with the use of materia medica.
RESULTS RETRIEVED
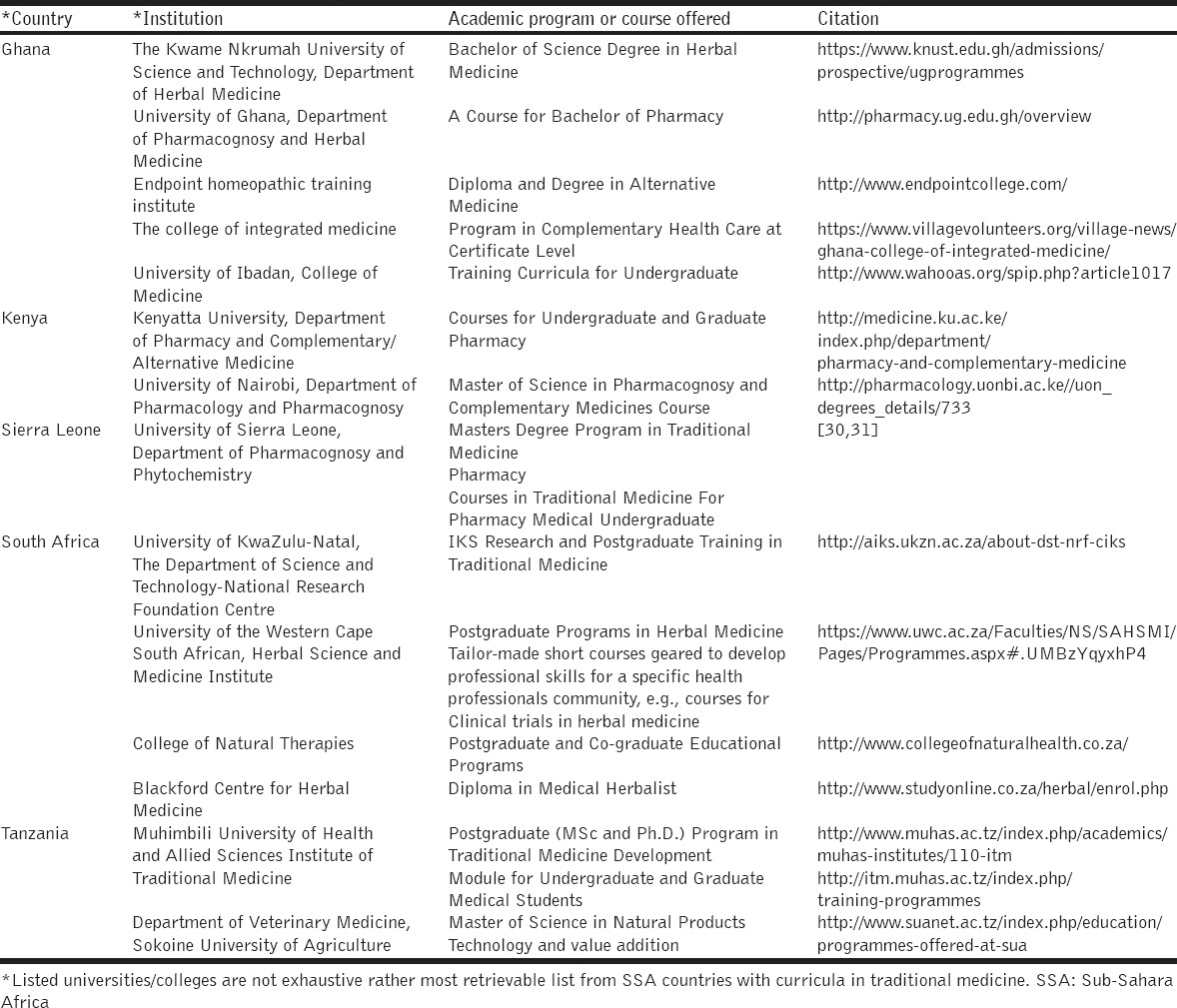
The analytical review of the information related to the subject on “curriculum or courses, or program in traditional or herbal medicine in Africa” revealed only a few institutions mostly universities or colleges in the countries residing SSA that undertake training in TM or complementary and alternative medicine [Table 1]. Many of the retrievable information indicated TM training to be tailor-made short courses geared to develop professional skills for a specific community of professionals. Furthermore, noted that, funds for most of the short courses were donor-based thus not sustainable beyond funding period, e.g., the Multi-disciplinary University Traditional Health Initiative project of South Africa. Some private owned colleges do conduct alternative and complementary medicine education training such as homeopathy as shown in Table 1. Most of the TM education programs in public universities are geared at analyzing the efficacy, safety, and quality of TM products while the clinical practices were being mostly left to private sector entities. Notably, several universities and research institutions in SSA countries are running some basic courses in phytochemistry, pharmacognosy, natural products chemistry, and phytomedicine. However, those universities/colleges are not listed as they are out of the scope of the present appraisal.
Table 1.
Some universities and colleges in Sub-Sahara Africa that offer formal education training in traditional medicine
DISCUSSION
Previously Chitindingu et al., 2014 pointed out the training components in African TM that was offered in South Africa to have a theoretical approach rather than problem-solving approach [32]. Further, reports indicated difficulties in the initial stages of introducing TM curriculum in biomedical universities for undergraduates [4,30,32,33]. Nevertheless, the importance of TM in SSA call for setting priorities of developing medicines from materia medica while streamlining TM practices alongside with other health professional training and services. There only only limited huddles on TM products that are used in treatments as many are crude extracts or are in the form of raw materials containing the therapeutic active ingredients [34]. Some may have been used for centuries by individuals within their environment in the communities, and their efficacy and safety is well-known by the entire community and may be acceptable. These can be a good start-up that may proceed to be essential medicines to be streamlined in formal health system delivery services if they satisfy the health care needs of the majority of the population and the prescribers are made aware of their efficacy and safety. The few African countries that have managed to integrate TM products in the National Essential Medicine List such as Ghana is because it was able to develop curriculum which is used to train TM experts as the way of disseminating the indigenous medical knowledge and practices to several health professionals [35]. Several African countries such as South Africa, Sierra Leone, and Tanzania have TM products being sold over the counters facilitated by the research and training programs undertaken in these countries [30,31,32,36-39].
FUTURE PROSPECTS AND RECOMMENDATIONS
Notably, few on-going attempt to integrate TM in formal health care can be spotted in some SSA countries whereby collaborative initiatives of some Traditional Health Practitioners Organization such THETA-Uganda; TAWG-Tanzania; and ZINATHA-Zimbabwe work closely with the Ministry of Health in addressing the prevention and care of HIV/AIDS patients [40,41]. These attempts are good model toward integration of TM to the formal system if embraced by formal training of practitioners that participate in such collaboration. The training program will instill skills and confidence to Traditional Health Practitioners to work in partnership with modern doctors in the existing formal health system. Other areas that need improvement in the integration process are modernization of TM to allow easy keeping, dispensing, and transportation in bulk; Clinical studies of herbal formulas need to be advocated to overcome the fear of being poisoned; Biodiversity depletion due to use of herbal material from wild source has to be addressed by engaging into extensive cultivation while adhering to Good Agricultural Practices. It is equally important that traditional practices and the philosophy for disease diagnosis and treatment be disseminated through education curricula, and the relevant research should be promoted sustainably.
ACKNOWLEDGMENT
I thank THETA-Uganda for inviting me to deliver a keynote presentation during the 3rd Annual National TM Conference organized jointly by THETA-Uganda and Uganda National Health Research Organization (UNHRO), thus stimulated compilation of this work.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Mendelsohn R, Balick MJ. The value of undiscovered pharmaceuticals in tropical forests. Econ Bot. 1995;49:223–8. [Google Scholar]
- 2.Payyappallimana U. Role of traditional medicine in primary health care: An overview of the perspectives and challenges. Yokohama J Soc Sci. 2009;14:69–72. [Google Scholar]
- 3.WHO. Benchmarks for Training in Traditional/Complementary and Alternative Medicine: Benchmarks for Training in Traditional Chinese Medicine: (WB 55.C4) Geneva, Switzerland: WHO; 2010. [Google Scholar]
- 4.Kim do Y, Park WB, Kang HC, Kim MJ, Park KH, Min BI, et al. Complementary and alternative medicine in the undergraduate medical curriculum: A survey of Korean medical schools. J Altern Complement Med. 2012;18:870–4. doi: 10.1089/acm.2011.0179. [DOI] [PubMed] [Google Scholar]
- 5.Dixon A, Riesberg A, Weinbrenner S, Saka O, Le Grand J, Buse R Traditional and Alternative Medicine in the UK and Germany. Research and Evidence on Supply and Demand. London: Anglo-Germany Foundation for the Study of Industry Society; 2003. [Google Scholar]
- 6.Salomonsen LJ, Skovgaard L, la Cour S, Nyborg L, Launsø L, Fønnebø V. Use of complementary and alternative medicine at Norwegian and Danish hospitals. BMC Complement Altern Med. 2011;11:4. doi: 10.1186/1472-6882-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States 2002. Sem Int Med. 2004;2:54–71. [PubMed] [Google Scholar]
- 8.Mak JC, Faux S. Complementary and alternative medicine use by osteoporotic patients in Australia (CAMEO-A): A prospective study. J Altern Complement Med. 2010;16:579–84. doi: 10.1089/acm.2009.0425. [DOI] [PubMed] [Google Scholar]
- 9.Zajac J, Shrestha A, Parin P, Poretsky L. The main events in the history of diabetes mellitus. In: Peretsky L, editor. The Principles of Diabetes Mellitus. New York: Springer; 2010. pp. 3–8. [Google Scholar]
- 10.Khaled HM. Breast cancer at diagonosis in women of Africa and the Middle East. In: William CK, Olopade OI, Falkson CI, editors. Breast Cancer in Women of Africa Decent. Netherland: Springer; 2006. pp. 81–90. [Google Scholar]
- 11.Janzen JM, Green EC. Continuity, change, and challenge in African medicine. In: Selin H, editor. Medicine across Cultures: History and Practice of Medicine in Non-Western Cultures. Vol. 3. Britain: Kluwer Academic Publisher; 2003. pp. 85–114. [Google Scholar]
- 12.Felkin RW. Notes on labour in Central Africa. Edinb Med J. 1884;29:922–30. [PMC free article] [PubMed] [Google Scholar]
- 13.Bastian A. Weck and the study of traditional Hehe medicine. Tanzania Notes Rec. 1969;70:29–40. [Google Scholar]
- 14.Bastian A. Weck, Der Wahehe Arzt und seine Wissenschaft, [The Wahehe Doctor and His Professional Knowledge] Berlin: Deutsches Kolonialblatt; 1908. pp. 1048–51. [Google Scholar]
- 15.Van Lehman D, Eno O. Culture Profile. Vol. 16. Washington, USA: Center for Applied Linguistics; 2003. The Somali Bantu Their History and Culture; pp. 1–33. [Google Scholar]
- 16.Onwuanibe RC. The philosophy of African medical practice. J Opin. 1979;9:25–8. [Google Scholar]
- 17.Kasenene P. African ethical theory and the four principles. In: Gillon R, editor. Principles of Health Care Ethics. New York: Basic Books; 1994. pp. 183–92. [Google Scholar]
- 18.Mbiti J. African Religions and Philosophy. Oxford: Heinemann; 1969. p. 101. [Google Scholar]
- 19.WHO. African Traditional Medicine. The AFRO Technical Report Series, 1. Brazzaville: Report of the Regional Expert Committee; 1976. pp. 3–4. 20. [Google Scholar]
- 20.Okpako DT. In: Science Interrogating Belief: Bridging the Old and New Traditions of Medicine in Africa. Nworu CS, Akah PA, editors. Ibadan, Nigeria: Book Builders; 2015. [Google Scholar]
- 21.Sneader W. Drug Discovery: A History. West Sussex, England: John Wiley & Sons, Inc; 2005. [Google Scholar]
- 22.Sneader W. Drug Discovery: The Evolution of Modern Medicines. Chichester, England: Wiley; 1985. [Google Scholar]
- 23.Newman DJ, Cragg GM. Natural products as sources of new drugs over the last 25 years. J Nat Prod. 2007;70:461–77. doi: 10.1021/np068054v. [DOI] [PubMed] [Google Scholar]
- 24.WHO. Alma-Ata Primary Health Care. Geneva: World Health Organization; 1978. [Google Scholar]
- 25.WHO. Resolution, AFR/RC28/R3 on the Use of Essential Medicines and the African Pharmacopoeia. Brazzaville: WHO Regional Office for Africa; 1978. [Google Scholar]
- 26.WHO. Resolution WHA41.19. Traditional Medicine and Medicinal Plants. Geneva: World Health Assembly; 1988. [Google Scholar]
- 27.WHO. Resolution, AFR/RC49/R5 on Essential Drugs in the WHO African Region: Situation and Trend Analysis. Windhoek Namibia: Final Report of the WHO Regional Committee for Africa; 1999. [Google Scholar]
- 28.WHO. Promoting the Role of Traditional Medicine in Health Systems: A Strategy for the African Region 2001-2010. Document Reference AFR/RC50/Doc.9/R. Harare: World Health Organization; 2000. [Google Scholar]
- 29.Berger M, Murugi J, Buch E, Ijsselmuiden C, Moran M, Guzman J, et al. Strengthening pharmaceutical innovation in Africa. Council on Health Research for Development (COHRED); New Partnership for Africa’s Development (NEPAD) Gaborone, Botswana: COHRED; 2010. pp. 20–3. [Google Scholar]
- 30.James PB, Bah AJ. Awareness, use, attitude and perceived need for complementary and alternative medicine (CAM) education among undergraduate pharmacy students in Sierra Leone: A descriptive cross-sectional survey. BMC Complement Altern Med. 2014;14:438. doi: 10.1186/1472-6882-14-438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kasilo OM, Trapsida JM, Mwikisa CN, Lusamba-Dikassa PS. An overview of the traditional medicine situation in the African region. Afr Health Monit. 2010;13:7–15. [Google Scholar]
- 32.Chitindingu E, George G, Gow J. A review of the integration of traditional, complementary and alternative medicine into the curriculum of South African medical schools. BMC Med Educ. 2014;14:40. doi: 10.1186/1472-6920-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DeJong J. Policy, Research, and External Affairs Working Papers; No. WPS 735. Population, Health, and Nutrition. Washington, DC: World Bank; 1991. Traditional medicine in Sub-Saharan Africa: Its importance and potential policy options. [Google Scholar]
- 34.WHO. General Guidelines for Methodologies on Research and Evaluation of Traditional Medicine. WHO/EDM/TRM/2000.1. Geneva: World Health Organization; 2000. [Google Scholar]
- 35.Anquandah J. African Ethnomedicine: An Anthropological and Ethno-Archaeological Case Study in Ghana. Afr Q Rev Stud Doc Ital Inst Afr East. 1997;52:289–98. [Google Scholar]
- 36.Kayombo EJ. Impact of training traditional birth attendants on maternal mortality and morbidity in Sub-Saharan Africa. Tanzan J Health Res. 2013;15:134–42. doi: 10.4314/thrb.v15i2.7. [DOI] [PubMed] [Google Scholar]
- 37.Mahunnah RL, Uiso FC, Kayombo EJ. Documentary of Traditional Medicine in Tanzania: A Traditional Medicine Resource Book. Tanzania: Dar-es-Salaam University Press; 2012. [Google Scholar]
- 38.Kayombo EJ, Mahunnah RL, Uiso FC. Prospects and challenges of medicinal plants conservation and traditional medicine in Tanzania. Anthropol. 2013;1:3. [Google Scholar]
- 39.Abdullahi AA. Trends and challenges of traditional medicine in Africa. Afr J Tradit Complement Altern Med. 2011;8(5 Suppl):115–23. doi: 10.4314/ajtcam.v8i5S.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kayombo EJ, Uiso FC, Mbwambo ZH, Mahunnah RL, Moshi MJ, Mgonda YH. Experience of initiating collaboration of traditional healers in managing HIV and AIDS in Tanzania. J Ethnobiol Ethnomed. 2007;3:6. doi: 10.1186/1746-4269-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mbwambo ZH, Mahunnah RL, Kayombo EJ. Traditional health Practitioner and Scientist: Bridging the gap in contemporary research in Tanzania. Tanzania Health Bull. 2007;9:115–20. doi: 10.4314/thrb.v9i2.14313. [DOI] [PubMed] [Google Scholar]