Abstract
Pelvic tumors in adolescent females are very uncommon. While the most common presentation is pelvic discomfort, we report the case of a 14-year-old female presenting with menorrhagia which is an unusual initial complaint for a large pelvic tumor. Adolescent females who present with heavy menstrual bleeding initially undergo assessment to rule out a bleeding disorder. In this case, careful history and physical examination helped in making a quick diagnosis and management. Ultrasound of abdomen showed a huge cystic mass due to serous cystadenoma of the ovary.
Keywords: Ovarian cystadenoma, tumor presentation, menorrhagia management
Introduction
Abnormal uterine bleeding is common among adolescent females in the immediate few years after menarche. The etiology is thought to be the physiological anovulatory cycles in the initial period prior to the maturation of hypothalamic pituitary ovarian axis. Heavy menstrual bleeding warrants evaluation for Von Willebrand disease as it is most common cause of heavy menstrual bleeding in adolescent females,1 and one in six girls who present to emergency room with heavy menstrual flow might have Von Willebrand disease.2 When associated with abdominal mass, it can be secondary to many other conditions, where the history and physical examination are extremely important in arriving at the differential diagnosis. Differential diagnosis includes tubo-ovarian abscess, ovarian torsion, ectopic pregnancy, ovarian masses either primary or secondary metastasis.
In a study conducted in by Stepanian and Cohn,3 the incidence of pediatric ovarian neoplasia was found to be 2.6/100,000. Of all ovarian malignancy, 2% occurred in females younger than 25 years.3 Epithelial ovarian tumors constitute about 19% of all pediatric ovarian tumors.3 They have a relative low occurrence in adolescent females, and it is thought that malignant epithelial tumors are a continuum starting with benign epithelial neoplasia.4
Here, we present a case of menorrhagia with anemia due to an uncommon cause in this age group where a good history and a thorough physical examination helped direct the way to the appropriate management.
Case report
A 14-year-old female was referred to our hematology clinic for evaluation of menorrhagia associated with microcytic anemia with hemoglobin of 6.7 g/dL (normal: 12–16 g/dL), hematocrit 25.5% (normal: 36%–45%), and mean corpuscular volume (MCV) of 65 fL (normal: 78–95 fL). Her complaints included shortness of breath and increased tiredness of a few weeks duration and a history of heavy menstrual bleeding of 6 weeks duration. Patient denied constipation or urinary frequency. She denied being sexually active. Patient reported a history of left ovarian cyst 2 years before presentation seen on abdomen ultrasound by a gynecologist who recommended no intervention at that time. Patient was hemodynamically stable; blood pressure 128/80 mm Hg and pulse rate 98 beat/min. Her physical examination was remarkable for pallor in skin and conjunctiva, obesity, as well as a firm mass on the left upper quadrant of the abdomen. Her body mass index (BMI) was at the 99.3th percentile for age (normal: 5th–85th percentile).
Urine pregnancy test in clinic was negative and abdominal ultrasound was ordered. Her coagulation profile and Von Willebrand factor assay were normal. Her serum iron was low at 43 mcg/dL (normal: 50–160 mcg/dL), total iron-binding capacity elevated at 486 mcg/dL (normal: 250–410 mcg/dL), iron saturation low at 9% (normal: 20%–50%), and elevated transferrin levels at 396 mg/dL (normal: 168–336 mg/dL). Ferritin level was low at 3 ng/mL (normal: 6–137 ng/dL). Alpha fetoprotein 1.1 ng/mL (normal: <7.5 ng/mL). Her liver function tests and serum creatinine were in the normal range. Since she was hemodynamically stable, she was started on ferrous sulfate by mouth for treatment of iron deficiency anemia.
Abdomen ultrasound showed a large cystic lesion occupying the majority of the pelvis, and all abdominal quadrants distorted normal anatomy and limited further evaluation. Abdominal computed tomography (CT) scan was done the same day and it revealed a large fluid-filled cyst in the anterior abdomen measuring approximately 23 × 10 cm on cross section and about 25 cm in length (Figure 1) with an otherwise normal appearing left ovary. The right ovary and uterus were normal.
Figure 1.
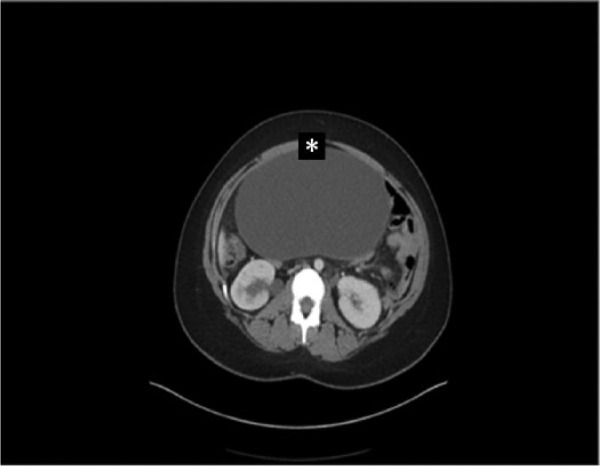
Abdominal CT scan without contrast showing the pelvic tumor (*) extending into the abdomen.
She was admitted to the hospital and underwent exploratory laparotomy, left ovarian cystectomy, and left partial oophorectomy. Patent had no complications during surgery. The large abdominal mass, which was resected intact, was not adherent to any abdominal viscera and was noted to be adjacent to left fallopian tube and arising from the left ovary. No lymphadenopathy or any other cystic structures were seen. Pathology report was consistent with serous cystadenoma (Figure 2) measuring 29 × 22 × 13 cm3 and weighed 3.9 kg. Possible residual ovarian tissue seen on the wall of the cyst and fallopian tube was normal with no pathologic changes. Her post-operative period was uneventful. She is currently doing well 2 years after surgery. Gynecologist recommended no further intervention based on the diagnosis. Follow-up pelvic ultrasound a year after of surgical excision showed no recurrence of ovarian masses.
Figure 2.
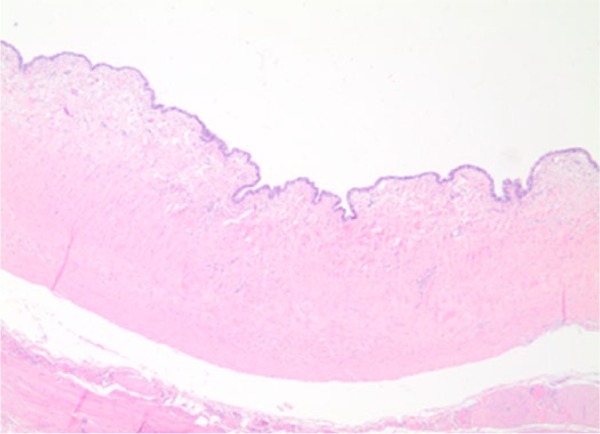
Benign serous cystadenoma; simple epithelial lining with underlying fibrous wall, no atypia or invasion is seen.
Discussion
Serous cystadenoma is an uncommon ovarian tumor in the adolescent age group, and anemia without any abdominal symptoms is an unusual presentation. Her main complaints at the time of presentation were menorrhagia and low hemoglobin that necessitated evaluation for bleeding disorder. Here, a careful physical examination suggested the need for abdominal sonogram that led to the diagnosis.
The American College of Obstetricians and Gynecologists defines heavy menstrual bleeding (menorrhagia) as “menstrual blood loss greater than 80 mL. However, this definition is used for research purposes and, in practice, excessive blood loss should be based on the patient’s perception.”5 In adolescent females, it is usually secondary to anovulatory cycles because of prematurity of the hypothalamic pituitary ovarian axis. However, bleeding disorder is an important cause and it needs to be ruled out especially when a girl presents with heavy menstrual flow at puberty. The prevalence of Von Willebrand disease and platelet dysfunction can be as high as 36% and 44% in this age group, respectively.6
Ovarian tumors are classified into epithelial, sex cord, and germ cell tumors. Ovarian neoplasia in pediatric population is rare. A recent paper was published in the Nordic federation of societies of obstetrics and gynecology showed that annual incidence of ovarian neoplasms is 2.2/100,000 in females between 0 and 15 years of age during the years 1999–2013. Mean age at presentation was 13 years for all neoplasms, and benign tumors were more common than malignant, 73% and 27%, respectively.7 In a study of pediatric ovarian masses, 73% of patients presented with abdominal pain and 29% had a palpable mass.8 While germ cell tumors are most common ovarian tumors constituting about 55%,9 epithelial ovarian tumors constitute about 19% of pediatric ovarian tumors.3 Dysmenorrhea occurs in all adolescents with epithelial tumors.10 In a review of 67 cases of pediatric ovarian tumors, only 9% had menstrual changes, while pelvic pain was most common complaint in more than half of the cases.11
Ovarian serous cystadenoma arises from the surface epithelium of the ovary. Depending on the amount of the fibrous tissue, it can be classified into cystadenoma, cystadenofibroma, adenofibroma, papillary cystadenoma, papillary cystadenofibroma, and papillary adenofibroma. Serous cystadenomas are usually oval, about 3–10 cm in diameter, with a glistening surface and cystic fluid is clear to yellowish. Microscopically, they have a single layer of ciliated simple columnar or simple cuboidal non-ciliated epithelium. Simple papillary projections can be seen, stroma has varying degrees of fibroblasts. No atypia, complexity, or invasions is seen.
American Academy of Pediatrics and American College of Obstetricians and Gynecologists have published guidelines to manage female adolescents with abnormal uterine bleeding. Assessment for hemodynamic instability would be the initial step in evaluation. Detailed history and physical examination directed toward the cause are important. Assessing the duration and severity of menstrual cycles, history of bleeding tendency and medication history are important. In addition, physical examination to assess for hemodynamic instability and for pelvic and abdominal masses could be secondary to chlamydia, gonorrhea, or even pelvic inflammatory disease. Lab investigations should include complete blood count (CBC) and a pregnancy test as well as platelet count and prothrombin time (PT) and partial thromboplastin time (PTT), with additional labs as needed; abdomen and pelvic ultrasound as well as CT scan are important imaging modality if there is any tenderness or suspicion of abdominal mass to assess for size, complexity, and location of pathology.12
Initial management includes identifying and treating the acute complications such as iron deficiency anemia. If the condition is a result of anovulatory cycles, management can be as simple as iron supplementation and close monitoring. Medical management could be hormonal treatment or treatment of a bleeding disorder such as mild hemophilia or Von Willebrand disorder. Invasive management depends on the primary disease. It can be dilation and curettage, laparoscopic surgery, or laparotomy procedure. However, for the active bleeding process, oral contraceptive pills and iron replacement are ideal, with a referral to a gynecologist and hematologist.13
Ovarian serous cystadenoma has been reported earlier in two adolescents, one who presented with abdominal distension and pain14 and the other with abdominal pain found to have ovarian edema and cyst,15 but none reported menorrhagia as initial presentation.
A study conducted in 1994 mentioned that abdomen and transvaginal ultrasonogram should be part of the initial evaluation of menorrhagia in adolescent females,16 since ovarian cystadenomas have a tendency to grow large. Earlier detection would prevent life-threatening complications such as ovarian torsion. Whether to add abdominal sonogram to the initial evaluation steps is dependent on the physical examination finding and the resources available. Detailed history taking and conducting a thorough physical examination were the keystone in managing this patient, in addition to following guidelines in managing adolescent females with menorrhagia.
Conclusion
In our case, patient was referred for concerns of low hemoglobin and menorrhagia that were attributed to bleeding disorder. However, what she had was a less common presentation for a usual ovarian mass at this age group. Therefore, we recommend, in addition to screening for bleeding disorders, screening for ovarian masses as they are still in the differential and abdomen/pelvic ultrasound is a good initial evaluation tool, especially if strongly suggested by physical examination. It is important to rule out presence of ovarian masses as benign lesions can even grow large that can result in ovarian torsion or rupture. Malignant transformation can occur. Early detection and intervention can preserve fertility. Excision is the choice for management, and annual physical examination and pelvic ultrasound are suggested to monitor for recurrence.
Acknowledgments
The authors thank Nahal Boroumand, MD, Assistant Professor, Department of Pathology, University of Texas Medical Branch, for providing the slide images of the tumor tissue. The first draft of the manuscript was written by Ahmad Abu Sulb.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: The University of Texas Medical Branch Institutional Review Board states that no written consent is needed because the information in the case report is not a systematic investigation. Verbal consent was obtained from the patient and her guardian and documented, and a legally authorized representative for anonymized patient information to be published in this article.
References
- 1. Castaman G, Federici AB, Rodeghiero F, et al. Von Willebrand’s disease in the year 2003: towards the complete identification of gene defects for correct diagnosis and treatment. Haematologica 2003; 88: 94–108. [PubMed] [Google Scholar]
- 2. Claessens EA, Cowell CA. Acute adolescent menorrhagia. Am J Obstet Gynecol 1981; 139: 277–280. [DOI] [PubMed] [Google Scholar]
- 3. Stepanian M, Cohn DE. Gynecologic malignancies in adolescents. Adolesc Med Clin 2004; 15(3): 549–568. [DOI] [PubMed] [Google Scholar]
- 4. Kurman RJ, Shih IM. Molecular pathogenesis and extraovarian origin of epithelial ovarian cancer—shifting the paradigm. Hum Pathol 2011; 42(7): 918–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. American College of Obstetricians and Gynecologists (ACOG). Clinical management guidelines for obstetrician–gynecologists. Practice Bulletin no. 128, July 2012. Washington, DC: ACOG. [Google Scholar]
- 6. James AH. Bleeding disorders in adolescents. Obstet Gyn Clin N Am 2009; 36(1): 153–162. [DOI] [PubMed] [Google Scholar]
- 7. Taskinen S, Fagerholm R, Lohi J, et al. Pediatric ovarian neoplastic tumors: incidence, age at presentation, tumor markers and outcome. Acta Obstet Gyn Scan 2015; 94(4): 425–429. [DOI] [PubMed] [Google Scholar]
- 8. Pomeranz AJ, Sabnis S. Misdiagnoses of ovarian masses in children and adolescents. Pediatr Emerg Care 2004; 20(3): 172–174. [DOI] [PubMed] [Google Scholar]
- 9. Deligeoroglou E, Eleftheriades M, Shiadoes V, et al. Ovarian masses during adolescence: clinical, ultrasonographic and pathologic findings, serum tumor markers and endocrinological profile. Gynecol Endocrinol 2004; 19(1): 1–8. [DOI] [PubMed] [Google Scholar]
- 10. Tsai JY, Saigo PE, Brown C, et al. Diagnosis, pathology, staging, treatment, and outcome of epithelial ovarian neoplasia in patients age <21 years. Cancer 2001; 91(11): 2065–2070. [DOI] [PubMed] [Google Scholar]
- 11. Schultz KAP, Sencer SF, Messinger Y, et al. Pediatric ovarian tumors: a review of 67 cases. Pediatr Blood Cancer 2005; 44: 167–173. [DOI] [PubMed] [Google Scholar]
- 12. American College of Obstetricians and Gynecologists (ACOG). ACOG committee opinion no. 557: management of acute abnormal uterine bleeding in nonpregnant reproductive-aged women. Obstet Gynecol 2013; 121(4): 891–896. [DOI] [PubMed] [Google Scholar]
- 13. Rimsza ME. Dysfunctional uterine bleeding. Pediatr Rev 2002; 23(7): 227–233. [DOI] [PubMed] [Google Scholar]
- 14. Mohammed Elhassan SA, Khan S, El-Makki A. Giant ovarian cyst masquerading as massive ascites in an 11-year-old. Case Rep Pediatr 2015; 2015: Article ID 878716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Khalbuss WE, Dipasquale B. Massive ovarian edema associated with ovarian serous cystadenoma: a case report and review of the literature. Int J Gynecol Cancer 2006; 16(Suppl. 1): 326–330. [DOI] [PubMed] [Google Scholar]
- 16. Dodson MG. Use of transvaginal ultrasound in diagnosing the etiology of menometrorrhagia. J Reprod Med 1994; 39(5): 362–372. [PubMed] [Google Scholar]


