Abstract
Study Design.
National registry cohort study.
Objective.
The aim of this study was to investigate the effect of surgical stabilization on survival of spinal fractures related to ankylosing spondylitis (AS).
Summary of Background Data.
Spinal fractures related to AS are associated with considerable morbidity and mortality. Multiple studies suggest a beneficial effect of surgical stabilization in these patients.
Methods.
In the Swedish patient registry, all patients treated in an inpatient facility are registered with diagnosis and treatment codes. The Swedish mortality registry collects date and cause of death for all fatalities. Registry extracts of all patients with AS and spinal fractures including date of death and treatment were prepared and analyzed for epidemiological purposes.
Results.
Seventeen thousand two hundred ninety-seven individual patients with AS were admitted to treatment facilities in Sweden between 1987 and 2011. Nine hundred ninety patients with AS (age 66 ± 14 years) had 1131 spinal fractures, of which 534 affected cervical, 352 thoracic, and 245 lumbar vertebrae. Thirteen percent had multiple levels of injuries during the observed period. Surgically treated patients had a greater survival than those treated nonsurgically [hazard ratio (HR) 0.79, P = 0.029]. Spinal cord injury was the major factor contributing to mortality in this cohort (HR 1.55, P < 0.001). The proportion of surgically treated spinal fractures increased linearly during the last decades (r = 0.92, P < 0.001) and was 64% throughout the observed years.
Conclusions.
Spinal cord injury threatened the survival of patients with spinal fractures related to AS. Even though surgical treatment is associated with a considerable complication rate, it improved the survival of spinal fractures related to AS.
Level of Evidence: 3
Keywords: ankylosing spondylitis, epidemiology, incidence, mortality, national registry, spinal cord injury, spinal fracture, spinal fusion, surgical treatment, survival
Ankylosing spondylitis (AS) is a rheumatoid disease involving all joints of the axial skeleton. In the end stage of the disease, all spinal segments are fused, leaving a completely ankylosed spine, the bamboo-spine.1 Depleted of their flexibility, mechanical energy cannot be absorbed in intervertebral discs, while osteoporosis weakens the skeletal structure.2,3 Thus, even minor trauma may have devastating effects, often an unstable spinal fracture with complicating neurological impairment.3–6
Nowadays, treatment recommendations favor surgical stabilization of fractures of the ankylosed spine.7 Still between 33% and 46% of these patients receive nonsurgical treatment.7,8 One reason for this is that surgical complications are common, despite the availability of multiple well-developed surgical techniques.7,9 In addition, due to complicating comorbidities, and neurological injury, the postinjury mortality is relatively high.10 A meta-analysis of 345 published cases between 1980 and 2007 finds a 3-month mortality of 18% for spinal fractures related to AS indicating the severity of this injury.8
Until now, no population-based data are available on the impact of surgical treatment on survival after spinal fractures related to AS. Furthermore, the changing treatment trend for these fractures is not well documented.
This study was designed to answer following questions using the Swedish Patient Registry (SPR) and the Swedish Mortality Registry (SMR):
Does surgical stabilization improve survival of patients with spinal fractures and end-stage AS?
What are the predictors of survival of spinal fractures related to AS?
Is there a shift in treatment trends for spinal fractures related to AS?
PATIENTS AND METHODS
In Sweden, all inpatients are registered in the Patient Registry (SPR) with personal identification number, dates for admission and interventions, diagnosis, and procedural codes. The SMR registers personal identification number, date, and cause of death for all deceased citizens. These registries are maintained by the Swedish National Board of Healthcare and Welfare (Socialstyrelsen).
After approval by the regional ethics review board of Uppsala (Dnr 210/297/1) and separate review by the unit for epidemiology of the Swedish National Board of Healthcare and Welfare (Dnr 23875/2012), a dataset was extracted from the SPR containing anonymized patient numbers (allowing identification of duplicate registration), dates for admission, date of surgery, diagnosis codes (both ICD-9 and ICD-10), procedural codes for all patients with the diagnosis code of spinal fracture, or AS from 1987 to 2011. Before anonymization, the dataset was cross-linked with the SMR and dates of death were added to the dataset allowing mortality investigations.
To identify spinal fractures, ICD-9 diagnosis codes were used until 1996: 805A, 805B, 805C, 805D, 805E, 805F, 806A, 806B, 806C, 806D, 806E, 806F. Since 1997, the ICD-10 classification was used to identify spinal fractures: S12.0, S12.1, S12.2, S12.7, S12.8, S12.9, S13.0, S13.1, S13.2, S13.3, S22.0, S22.1, S23.0, S23.1, S32.0, S32.1, S33.0, S33.1. Hereafter, all patients with AS were identified (ICD-9: 720, ICD-10: M45.9). To identify patients who underwent spine surgery procedure, codes indicating stabilizing spinal operations were used [Swedish surgical procedure classification (until 1996): 8214, 8215, 8216, 8219, 8440, 8441, 8442, 8443, 8449, Swedish clinical procedure code (from 1997): NAJ, NAG, NAT].11 Surgical treatment with decompression only was not considered as surgical stabilization, and halo-treatment was considered as conservative treatment.
Duplicate entries were identified and only counted once, using the first time of admission with the diagnosis of a spinal fracture. If a patient was readmitted with a spinal fracture more than 2 years after the previous admission, he was counted and marked as a sequential fracture case and not removed as a duplicate. In the original dataset, duplicate entries per patient reflect re-admissions possibly containing valuable diagnosis codes of comorbidities. Therefore, all diagnosis codes for comorbidities and later procedures on each patient were stored in a singular entry before erasing duplicate entries. This allowed for instance determining the Charlson Comorbidity Index (CCI) for each case.12
The software R-studio version 0.98.1091 (Free Software Foundation, Boston, MA) was used to process the dataset and perform the statistical analyses. A logistic regression model was used to determine the odds ratio (OR) of covariates on the treatment allocation. The Kaplan–Meier method was employed to determine median survival and to plot the survival curve. Five Cox proportional hazards regression models were tested and the most predictive model applied to determine the hazard ratio (HR) of covariates.13 Results were presented with 95% confidence intervals (95% CIs) and were considered as statistically significant if P value was less than 0.05.
RESULTS
A total of 32,088 hospital admissions with AS were registered in the SPR between 1987 and 2011 (Figure 1). After removal of duplicate entries, 17,297 cases remained. The inclusion flow chart is presented in Figure 1. During the included 990 hospital admissions, 1131 AS-related spinal fractures were treated. Sequential fractures with separate admissions of an individual patient were found in 61 cases. Baseline data according to treatment allocation are presented in Table 1.
Figure 1.
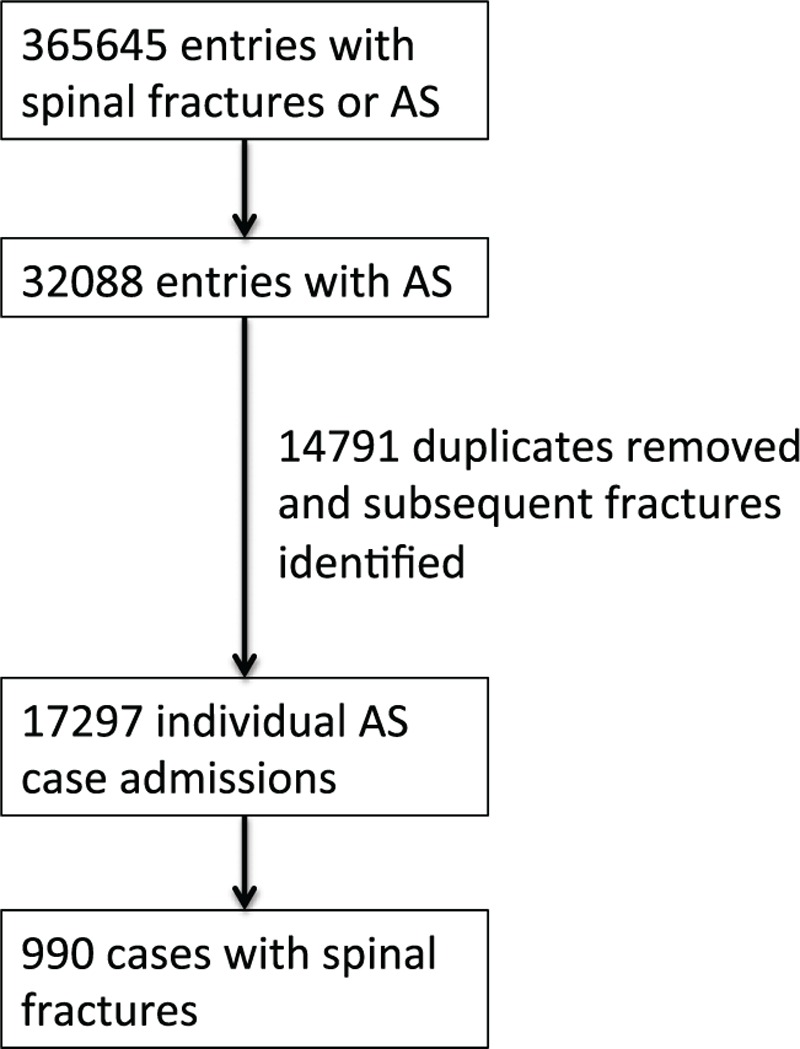
Inclusion flow diagram.
TABLE 1.
Baseline Values of Included Cases With Spinal Fractures Related to Ankylosing Spondylitis
| Age (years) | Gender | CCI | Cervical Fracture | ||||||
| Treatment | n | Mean | SD | n male | n female | Mean | SD | N | Percent |
| Surgical | 636 | 65.4 | 12.7 | 547 | 89 | 4.8 | 2.4 | 381 | 59 |
| Nonsurgical | 354 | 66.2 | 15.0 | 273 | 81 | 4.7 | 2.5 | 153 | 43 |
| All | 990 | 65.7 | 13.6 | 820 | 170 | 4.8 | 2.4 | 534 | 54 |
| Thoracic Fracture | Lumbar Fracture | Multilevel Fracture | Sequential Fracture | Spinal Cord Injury | |||||
| n | Percent | n | Percent | n | Percent | N | Percent | n | Percent |
| 238 | 37 | 115 | 18 | 91 | 14 | 40 | 6 | 122 | 19 |
| 114 | 32 | 130 | 36 | 39 | 11 | 21 | 6 | 41 | 12 |
| 352 | 36 | 245 | 25 | 130 | 13 | 61 | 6 | 163 | 16 |
Male patients and patients with spinal cord injury were more likely to be operated on, as well as patients operated during the more recent years. Table 2 presents the OR of covariates in the logistic regression model.
TABLE 2.
Odds Ratio (OR) and 95% CI of Covariates for Surgical Treatment Allocation
| OR | 95% CI | |||
| Lower | Upper | P | ||
| Age | 0.99 | 0.98 | 1.01 | 0.430 |
| Male gender | 1.52 | 1.05 | 2.19 | 0.026 |
| Cervical fracture | 1.00 | 0.27 | 4.18 | 0.999 |
| Thoracic fracture | 0.71 | 0.19 | 3.01 | 0.621 |
| Lumbar fracture | 0.35 | 0.09 | 1.46 | 0.122 |
| Multilevel fractures | 2.36 | 0.47 | 10.82 | 0.274 |
| Sequential admissions | 0.75 | 0.42 | 1.38 | 0.343 |
| Spinal cord injury | 2.73 | 1.77 | 4.31 | 0.000 |
| Charlson Comorbidity Index | 0.99 | 0.91 | 1.08 | 0.865 |
| Year of admission | 1.11 | 1.08 | 1.14 | 0.000 |
95% CI indicates 95% confidence interval; OR, odds ratio.
The proportion of surgically treated spinal fractures increased linearly during the last decades (r = 0.92, P < 0.001) and has been about 64% throughout the observed time period (Figure 2).
Figure 2.
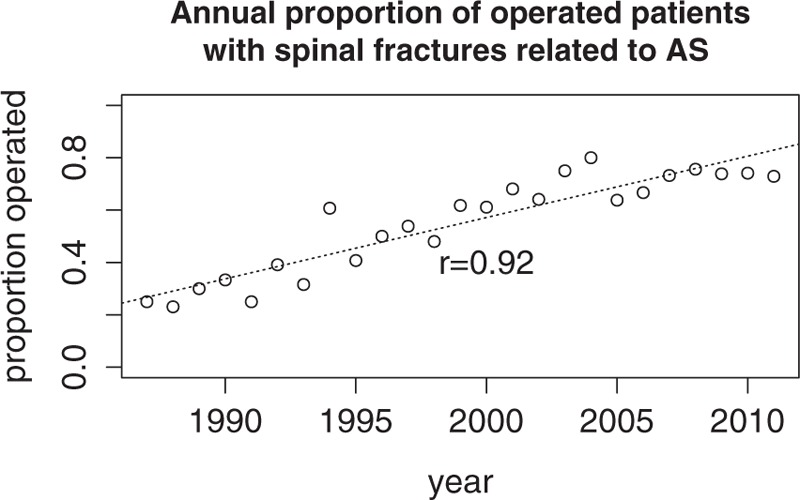
Linear trend of the annual proportion of patients treated surgically for spinal fractures related to ankylosing spondylitis (r = 0.92; P < 0.001).
Of the 17,297 cases from the SPR with AS, 4897 had already deceased according to the SMR. In the included 990 cases of AS patients with spinal fractures, the median survival was 8.9 years (95% CI 7.75–10.0); the 3-month mortality was 17% (Figure 3). Results of 5 tested Cox proportional hazard models are presented in Table 3. The most predictive Cox regression model found age, gender, SCI, and CCI contributing to mortality in this cohort (r2 = 0.339). Surgical stabilization had a positive impact on survival (HR = 0.79, P = 0.027). Survival of AS-related spinal fractures was improved by being hospitalized now and not years ago (HR = 0.96, P < 0.001). Results for covariates in the Cox proportional hazards model are presented in Table 4.
Figure 3.
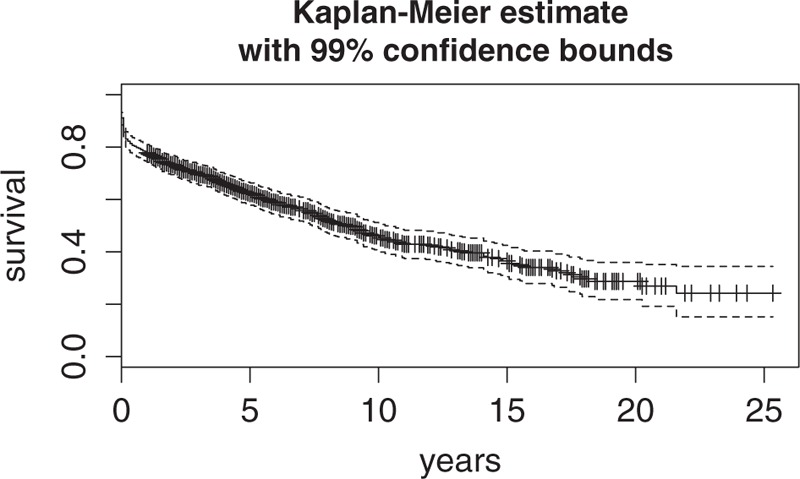
Kaplan–Meier survival curve of 990 cases with spinal fracture related to ankylosing spondylitis.
TABLE 3.
Hazard Ratio (HR) of Covariates in 5 Tested Cox Proportional Hazards Models Presented With r2
| Model | 1 | 2 | 3 | 4 | 5 |
| HR | HR | HR | HR | HR | |
| Age | 1.05** | 1.05** | 1.05** | ||
| Male gender | 1.33* | 1.29* | 1.29* | ||
| Cervical fracture | 1.21 | 1.66 | |||
| Thoracic fracture | 0.96 | 1.32 | |||
| Lumbar fracture | 0.97 | 1.33 | |||
| Multilevel fractures | 0.69 | ||||
| Sequential fractures | 0.94 | ||||
| Surgical treatment | 0.85 | 0.80* | 0.82 | 0.79* | 0.79* |
| Spinal cord injury | 1.68** | 1.57** | 1.55** | 1.55** | |
| Charlson Comorbidity Index | 1.27** | 1.28** | 1.28** | ||
| Year of admission | 0.96** | 0.96** | 0.96** | ||
| r2 | 0.003 | 0.022 | 0.335 | 0.339 | 0.338 |
| Degrees of freedom | 1 | 2 | 6 | 9 | 11 |
Levels of significance: P < 0.1; *P < 0.05; **P < 0.001. HR indicates hazard ratio.
TABLE 4.
Hazard Ratio (HR) and 95% CI of Covariates for Mortality in the Most Predictive Cox Proportional Hazards Model
| HR | 95% CI | |||
| Lower | Upper | P | ||
| Age | 1.05 | 1.04 | 1.06 | 0.000 |
| Male gender | 1.29 | 1.00 | 1.67 | 0.047 |
| Cervical fracture | 1.21 | 0.88 | 1.66 | 0.245 |
| Thoracic fracture | 0.96 | 0.72 | 1.27 | 0.761 |
| Lumbar fracture | 0.97 | 0.70 | 1.33 | 0.841 |
| Surgical treatment | 0.79 | 0.64 | 0.97 | 0.027 |
| Spinal cord injury | 1.55 | 1.22 | 1.97 | 0.000 |
| Charlson Comorbidity Index | 1.28 | 1.22 | 1.35 | 0.000 |
| Year of admission | 0.96 | 0.95 | 0.98 | 0.000 |
95% CI indicates 95% confidence interval; HR, hazard ratio.
DISCUSSION
The main findings of this study were (1) an improved survival with surgical stabilization of patients with spinal fractures related to AS, (2) a dramatic impact of spinal cord injury on the overall mortality of these patients, (3) a significant trend toward surgical management of spinal fractures related to AS, and (4) an improved survival of patients with spinal fractures related to AS during the last decades.
Improved Survival by Surgical Stabilization
In this study, surgical stabilization had a clear beneficial effect on survival of spinal fractures related to AS. Until now, little is published on the effect of surgery on survival. The meta-analysis of publications between 1980 and 2007 by Westerveld et al8 finds no significant effect of surgery on survival. In 2010, Caron et al7 review retrospectively 112 patients with spinal fractures related to AS or DISH. They find a 1-year mortality of surgically treated patients of 23% (17 of 75), compared with 51% (19 of 37) with nonsurgical treatment (χ2-test, P = 0.005). In this context, the results from our study seem valid.
For the treatment allocation in the presented dataset, a significant selection bias must be assumed. Both patients with simple nondisplaced fractures and those with considerable comorbidity are likely to receive nonsurgical treatment,8 while those with fracture dislocation, SCI, and relatively good health are more likely to be operated on. The descriptive statistics of the present dataset revealed that those with SCI were more likely to be treated surgically, but those with lumbar fractures were in the majority of cases treated nonsurgically. Patient comorbidity as measured with the CCI did not play a major role in treatment decision. Fracture location and SCI entered the COX-regression analysis as independent covariates, but surgical treatment remained a significant predictor for survival. As fracture displacement was not accessible in our database, this factor could not be adjusted for. Assuming that a fracture would be treated rather surgically the more it is displaced, adding fracture displacement could only strengthen the beneficial effect of surgical treatment.
With regard to the surgical treatment of spinal fractures related to AS, multiple complications are common. Wound infections of up to 16%, pulmonary complications of up to 63%, and mechanical complications of up to 23% are described.7,9,14–16 Some of these complications may be associated with mortality by themselves.9 However, the risk of surgical complications did not attenuate the positive effect on survival found in the SPR.
Predictors of Mortality
In our study, the 3-month mortality of patients with spinal fractures related to AS was 17%, which has intriguing similarity to the 3-month mortality of 18% in the study by Westerveld et al.8.
As in most previously investigated populations, age and sex were associated with mortality. Furthermore, patient comorbidity played a major role for surgical survival. This study confirmed that the CCI is associated with postoperative mortality.16
Spinal cord injury was related to considerable mortality in patients with AS. It is well documented that spinal cord injury in AS patients is associated with mortality, being greater the more cranial and the more complete the lesion is.17,18 A recently published cohort study finds survival of surgically treated cervicothoracic injuries in AS to be threatened by complete spinal cord injury (HR = 8.3, P = 0.02).9 The avoidance of spinal cord injury by preventive measures and proper prehospital stabilization, and the awareness of the particular circumstances required for SCI rehabilitation will reduce the mortality of spinal injuries related to AS.19
Current Treatment Trend Toward Surgery and Improved Survival
For decades, many have avoided surgical treatment of spinal fractures related to AS, as the injured patients often were in a poor condition complicated by comorbidity.20 Thus, nonsurgical treatment has been applied in many patients. External immobilization of spinal fractures related to AS requires well-experienced staff and time-consuming nursing.20 Unfortunately, even under the most optimal conditions, complications are common, and the mortality is high.7,21
During the last 2 decades, there was a trend in Sweden toward surgical treatment of these fractures being today around 70%. This reflects the growing number of recommendations to treat spinal fractures related to AS surgically.3,7,8 The rationale behind the recommendation for surgical stabilization is based on the biomechanical understanding, that fractures of the ankylosed spine resemble transverse diaphysary long bone fractures. Long lever arms cranially and caudally of the fracture interfere with bony healing, and nonunion will result if sufficient stability is not provided. Therefore, a long posterior fixation of at least level 3 above and below the fracture is recommended by several authors.7,22
Following these recommendations, the survival of spinal fractures related to AS improved in Sweden during the last decades. The positive effect of surgical treatment was significant, but only at the P less than 0.05 level, indicating that medical care improvements other than surgical treatment must have played their part. Further research should be performed to investigate, for instance, the effect of biological anti-rheumatic treatment on fracture incidence and survival.
Limitations of Registry Studies
All registry studies must be criticized for observational errors, for data are only as good as the quality of registration. Fracture underreporting may occur, while prehospital fatalities are not registered in the SPR, and causative AS-related spinal fractures remain unrecognized.23 The diagnosis registration of deceased patients during or right after treatment is most likely not pursued with the same endeavor as of those discharged in a healthier condition. Difficulties may arise, while reporting noncontiguous fractures or spinal fractures in a multiple trauma context, wherein reporting of all injuries separately will cause significant documentation work for the individual surgeon. Missing information at the time of admission due to communication failures, the surgeon's defect knowledge, or the surgeon's lack of attention to detail reduce the quality of registration.24 Beyond that, poor coder training, absent quality control, misspecification, unbundling, and upcoding lead to inappropriate registration of correctly written diagnoses.24
The validation of the SPR using other quality registries confirms high validity of registered orthopedic diagnoses.25 Diagnoses of hip fractures are correctly identified in more than 95%. Since the SPR was started in the 1960s, a coding learning curve could explain an increasing incidence for most diagnosis groups. Instead, no increasing incidence of lumbar fractures was reported in the SPR during the last decades, which would have been expected if a systematic bias was present.26 Obviously, the current registration quality is good, and registration bias cannot explain the findings in this study. Besides, the Swedish reimbursement policy requires complete diagnosis registration, an effective incitement to proper coding.
The continuous increase of the incidence of spinal fractures related to AS—despite the improvements of medical treatment—may be explained by changes in the population age pyramid, greater awareness of fractures, improved diagnostics, improved emergency care reducing fatalities, and a higher activity level of patients receiving modern medical and physical therapy.7,26 For the individual surgeon, this means that the level of alert cannot be lowered for injured AS patients. An AS patient—even after minor trauma—should be managed as having a fracture until the diagnosis has been established or excluded.27 Preventive measures—as the avoidance of alcohol intoxication, contact sports (ie, rugby), high impact sports (ie, tennis), and the use of seat belts and car seat headrests at all times while driving—should not be neglected.4 First, during the upcoming decades, the optimized biological treatment will have reached a greater epidemiological effect. Until then, hopefully, the increasing trend of spinal fracture incidence related to AS has been reversed.
Key Points.
Surgical stabilization improved survival of patients with spinal fractures related to AS.
Spinal cord injury was associated with greater mortality of patients with spinal fractures related to AS.
There was a trend toward surgical management of spinal fractures related to AS.
During the last decades, an improved survival of patients with spinal fractures related to AS was seen.
Acknowledgment
The authors would like to thank the statistician Erik Onelöv of the Swedish National Board of Healthcare and Welfare for excellent collaboration with regard to data extraction.
Footnotes
The manuscript submitted does not contain information about medical device(s)/drug(s). The Swedish Society of Medicine (Grant no. SLS-324071) funds were received in support of this work. Relevant financial activities outside the submitted work: consultancy, expert testimony, payment for lectures.
References
- 1.Sawacha Z, Carraro E, Del Din S, et al. Biomechanical assessment of balance and posture in subjects with ankylosing spondylitis. J Neuroeng Rehabil 2012; 9:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carter S, Lories RJ. Osteoporosis: a paradox in ankylosing spondylitis. Curr Osteoporos Rep 2011; 9:112–115. [DOI] [PubMed] [Google Scholar]
- 3.Heyde CE, Fakler JK, Hasenboehler E, et al. Pitfalls and complications in the treatment of cervical spine fractures in patients with ankylosing spondylitis. Patient Saf Surg 2008; 2:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heyde CE, Robinson Y, Kayser R, et al. [Fatal complex fracture of the cervical spine in a patient with ankylosing spondylitis after a fall from a racing bicycle]. Sportverletz Sportschaden 2007; 21:148–151. [DOI] [PubMed] [Google Scholar]
- 5.Weiss RJ, Wick MC, Ackermann PW, et al. Increased fracture risk in patients with rheumatic disorders and other inflammatory diseases -- a case-control study with 53,108 patients with fracture. J Rheumatol 2010; 37:2247–2250. [DOI] [PubMed] [Google Scholar]
- 6.Muñoz-Ortego J, Vestergaard P, Rubio JB, et al. Ankylosing spondylitis is associated with an increased risk of vertebral and nonvertebral clinical fractures: a population-based cohort study. J Bone Miner Res 2014; 29:1770–1776. [DOI] [PubMed] [Google Scholar]
- 7.Caron T, Bransford R, Nguyen Q, et al. Spine fractures in patients with ankylosing spinal disorders. Spine (Phila Pa 1976) 2010; 35:E458–E464. [DOI] [PubMed] [Google Scholar]
- 8.Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment: neurological status and complications. Eur Spine J 2009; 18:145–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robinson Y, Robinson AL, Olerud C. Complications and survival after long posterior instrumentation of cervical and cervicothoracic fractures related to ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis. Spine (Phila Pa 1976) 2015; 40:E227–E233. [DOI] [PubMed] [Google Scholar]
- 10.Schoenfeld AJ, Harris MB, McGuire KJ, et al. Mortality in elderly patients with hyperostotic disease of the cervical spine after fracture: an age- and sex-matched study. Spine J;11:257–264. [DOI] [PubMed] [Google Scholar]
- 11.Socialstyrelsen. Classification of Surgical Procedures Version 1.9. Lindesberg, Sweden: Bergslagens Grafiska; 2004. [Google Scholar]
- 12.Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol 1994; 47:1245–1251. [DOI] [PubMed] [Google Scholar]
- 13.Bradburn MJ, Clark TG, Love SB, et al. Survival analysis Part III: multivariate data analysis -- choosing a model and assessing its adequacy and fit. Br J Cancer 2003; 89:605–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olerud C, Frost A, Bring J. Spinal fractures in patients with ankylosing spondylitis. Eur Spine J 1996; 5:51–55. [DOI] [PubMed] [Google Scholar]
- 15.de Peretti F, Sane JC, Dran G, et al. [Ankylosed spine fractures with spondylitis or diffuse idiopathic skeletal hyperostosis: diagnosis and complications]. Rev Chir Orthop Reparatrice Appar Mot 2004; 90:456–465. [DOI] [PubMed] [Google Scholar]
- 16.Chikuda H, Yasunaga H, Horiguchi H, et al. Impact of age and comorbidity burden on mortality and major complications in older adults undergoing orthopaedic surgery: an analysis using the Japanese diagnosis procedure combination database. BMC Musculoskelet Disord 2013; 14:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wilson JR, Cadotte DW, Fehlings MG. Clinical predictors of neurological outcome, functional status, and survival after traumatic spinal cord injury: a systematic review. J Neurosurg Spine 2012; 17:11–26. [DOI] [PubMed] [Google Scholar]
- 18.Alaranta H, Luoto S, Konttinen YT. Traumatic spinal cord injury as a complication to ankylosing spondylitis. An extended report. Clin Exp Rheumatol 2002; 20:66–68. [PubMed] [Google Scholar]
- 19.Bradley Jacobs W, Fehlings MG. Ankylosing spondylitis and spinal cord injury: origin, incidence, management, and avoidance. Neurosurg Focus 2008; 24:E12. [DOI] [PubMed] [Google Scholar]
- 20.Graham B, Van Peteghem PK. Fractures of the spine in ankylosing spondylitis: diagnosis, treatment, and complications. Spine 1989; 14:803–807. [DOI] [PubMed] [Google Scholar]
- 21.Chaudhary SB, Hullinger H, Vives MJ. Management of acute spinal fractures in ankylosing spondylitis. ISRN Rheumatol 2011; 2011:150484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Backhaus M, Citak M, Kalicke T, et al. [Spine fractures in patients with ankylosing spondylitis: an analysis of 129 fractures after surgical treatment]. Orthopäde 2011; 40:917–920, 922–924. [DOI] [PubMed] [Google Scholar]
- 23.Alker GJ, Oh YS, Leslie EV, et al. Postmortem radiology of head neck injuries in fatal traffic accidents. Radiology 1975; 114:611–617. [DOI] [PubMed] [Google Scholar]
- 24.O’Malley KJ, Cook KF, Price MD, et al. Measuring diagnoses: ICD code accuracy. Health Serv Res 2005; 40:1620–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health 2011; 11 1:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robinson Y, Sandén B, Olerud C. Increased occurrence of spinal fractures related to ankylosing spondylitis: a prospective 22-year cohort study in 17,764 patients from a national registry in Sweden. Patient Saf Surg 2013; 7:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pedersen W, Clausen S, Kriegbaum NJ. Spinal lesions in patients with ankylosing spondylitis. Scand J Rheumatol 1987; 16:381–382. [DOI] [PubMed] [Google Scholar]


