Abstract
BACKGROUND
Merkel-cell carcinoma is an aggressive skin cancer that is linked to exposure to ultraviolet light and the Merkel-cell polyomavirus (MCPyV). Advanced Merkel-cell carcinoma often responds to chemotherapy, but responses are transient. Blocking the programmed death 1 (PD-1) immune inhibitory pathway is of interest, because these tumors often express PD-L1, and MCPyV-specific T cells express PD-1.
METHODS
In this multicenter, phase 2, noncontrolled study, we assigned adults with advanced Merkel-cell carcinoma who had received no previous systemic therapy to receive pembrolizumab (anti–PD-1) at a dose of 2 mg per kilogram of body weight every 3 weeks. The primary end point was the objective response rate according to Response Evaluation Criteria in Solid Tumors, version 1.1. Efficacy was correlated with tumor viral status, as assessed by serologic and immunohistochemical testing.
RESULTS
A total of 26 patients received at least one dose of pembrolizumab. The objective response rate among the 25 patients with at least one evaluation during treatment was 56% (95% confidence interval [CI], 35 to 76); 4 patients had a complete response, and 10 had a partial response. With a median follow-up of 33 weeks (range, 7 to 53), relapses occurred in 2 of the 14 patients who had had a response (14%). The response duration ranged from at least 2.2 months to at least 9.7 months. The rate of progression-free survival at 6 months was 67% (95% CI, 49 to 86). A total of 17 of the 26 patients (65%) had virus-positive tumors. The response rate was 62% among patients with MCPyV-positive tumors (10 of 16 patients) and 44% among those with virus-negative tumors (4 of 9 patients). Drug-related grade 3 or 4 adverse events occurred in 15% of the patients.
CONCLUSIONS
In this study, first-line therapy with pembrolizumab in patients with advanced Merkel-cell carcinoma was associated with an objective response rate of 56%. Responses were observed in patients with virus-positive tumors and those with virus-negative tumors. (Funded by the National Cancer Institute and Merck; ClinicalTrials.gov number, NCT02267603.)
The programmed death 1 (PD-1) immune checkpoint pathway, which comprises the PD-1 T-cell coinhibitory receptor and its ligands PD-L1 and PD-L2 expressed on tumor and immune cells in the tumor microenvironment, mediates local immune resistance.1 Monoclonal antibodies blocking this pathway are active against advanced tumors of several different types, providing a “common denominator” for cancer therapy.2 PD-L1 expression in pretreatment tumor specimens may identify patients and tumor types that are more likely to have a response to PD-1 pathway blockade, and PD-L1 immunohistochemical tests were recently approved by the Food and Drug Administration to guide clinical decision making for patients with advanced non–small-cell lung cancer and melanoma who are candidates for anti–PD-1 therapy.3 An elevated tumor mutational burden, creating new determinants (neoantigens) for immune recognition, has also been associated with tumor regressions in individual patients and the responsiveness of tumor subtypes to anti–PD-1 therapy.4,5
Merkel-cell carcinoma is a rare but aggressive skin cancer. For advanced Merkel-cell carcinoma, cytotoxic chemotherapy offers a median progression- free survival of only 3 months.6,7 Merkel-cell carcinoma has long been considered to be an immunogenic cancer because it occurs more frequently and has a worse prognosis in immunosuppressed persons than in those with no immune suppression.8 Two major causative factors have been identified: ultraviolet (UV) light and the Merkel-cell polyomavirus (MCPyV), whose large T antigen is expressed in tumor cells and inactivates p53 and Rb.9 Approximately 80% of Merkel-cell carcinomas are associated with MCPyV, and patients with these carcinomas often produce MCPyV T-antigen–specific T cells and antibodies that increase with disease progression and decrease with effective therapy.10–12 Virus-associated Merkel-cell carcinomas carry extremely low mutational burdens, in contrast to UV-induced, MCPyV-negative Merkel-cell carcinomas, which are characterized by a mutational load that is approximately 100 times as high.13–15 Several studies have shown that approximately 50% of Merkel-cell carcinomas express PD-1 on tumor-infiltrating lymphocytes and express PD-L1 on tumor cells or infiltrating macrophages in an “adaptive resistance” pattern (with expression concentrated at the leading edges of the tumor), which suggests an endogenous tumor-reactive immune response that might be unleashed by anti–PD-1 or anti–PD-L1 drugs.11,16–18
The current study was undertaken to assess the efficacy of pembrolizumab, an anti–PD-1 therapy, in patients with advanced Merkel-cell carcinoma who had not previously received systemic therapy and to correlate treatment outcomes with tumor MCPyV and PD-L1 status.
Methods
Patients
Eligible patients were at least 18 years old and had distant metastatic or recurrent locoregional Merkel-cell carcinoma that was not amenable to definitive surgery or radiation therapy; measurable disease according to Response Evaluation Criteria in Solid Tumors, version 1.1; an Eastern Cooperative Oncology Group (EGOG) performance status of 0 or 1 (on a scale of 0 to 5, with lower scores indicating less disability); and normal organ and bone marrow function.19,20 Key exclusion criteria were previous systemic therapy for unresectable Merkel-cell carcinoma, a diagnosis of immunodeficiency or ongoing systemic immunosuppressive therapy, active autoimmune disease, concurrent second cancer, and active central nervous system metastases.
Study Design
This phase 2, single-group, Simon’s two-stage, multicenter study was sponsored by the National Cancer Institute (NCI) and Merck and was developed by the authors in collaboration with the Cancer Immunotherapy Trials Network, the Cancer Therapy Evaluation Program, and Merck. According to Simon’s two-stage design for efficacy estimation, at least one response among the first group of nine treated patients was required in order to enroll additional patients. Pembrolizumab, a humanized monoclonal IgG4 antibody (mAb) that blocks PD-1, was administered intravenously at a dose of 2 mg per kilogram of body weight every 3 weeks. Treatment was allowed to continue for a maximum of 2 years or until a complete response, dose-limiting toxic effects, or progressive disease occurred. Patients who appeared to have progression in target or non-target lesions or to have new lesions were allowed to continue therapy if they were asymptomatic, had an ECOG performance status of 0 or 1, and had no evidence of rapid progression; patients were evaluated 4 weeks later to assess possible further progression.
The objective of this study was to determine the clinical efficacy of pembrolizumab as first systemic therapy for patients with advanced Merkel-cell carcinoma. The primary end point was the objective response rate measured according to RECIST, version 1.1.19 Secondary end points were progression-free survival, overall survival, and duration of response. All adverse events were assessed according to NCI Common Terminology Criteria for Adverse Events, version 4.21 Major exploratory objectives were to examine potential laboratory correlates for the clinical activity of pembrolizumab. The protocol is available with the full text of this article at NEJM.org.
Study Oversight
The protocol was approved by the institutional review board at each participating center, and the study was conducted in accordance with the Declaration of Helsinki and the International Conference on Harmonisation Good Clinical Practice guidelines. All the patients provided written informed consent before study entry. The principal investigators, in collaboration with the NCI and Merck, were responsible for the design and oversight of the study and the development of the protocol. The NCI was responsible for the collection and maintenance of the data. The manuscript was written and prepared by the authors with editorial oversight by the NCI. All the authors vouch for the accuracy and completeness of the data reported and adherence to the study protocol. No one who is not an author contributed to writing the manuscript.
Clinical Assessments
All patients underwent computed tomographic scanning of the chest and abdomen (as well as other areas in which the target lesions occurred) at the time of screening and 12 weeks after starting therapy and at 9-week intervals there-after. After 1 year of treatment, the scanning frequency was decreased to 12-week intervals. Evaluations of scans according to RECIST, version 1.1, were conducted at the institutional level, with central radiologic review performed by the NCI for patients who had a response. Pretreatment tumor specimens were obtained from all patients. The period between the pretreatment tumor biopsy and treatment initiation ranged from 7 days to 8.4 years (median, 5.2 months). Blood samples were drawn for correlative laboratory analyses at the time of radiologic studies. Post-treatment biopsies were obtained when clinically feasible.
Tumor MCPyV Status
Recent or archival tumor specimens from all patients were assessed for expression of the MCPyV large T antigen oncoprotein through immunohistochemical analysis with a murine monoclonal IgG2b antibody (clone CM2B4, Santa Cruz Biotechnology).22,23 Patients were also assessed for the presence of serum antibodies or circulating T cells specific for MCPyV oncoproteins (see the Methods section in the Supplementary Appendix, available at NEJM.org).12 Because B-cell and T-cell reactivities against MCPyV oncoproteins are restricted to patients with MCPyV-positive tumors, patients with indeterminate tumor immunohistochemical results who were positive for serum antibodies or circulating MCPyV-specific T cells were categorized as having MCPyV-positive tumors.11,12,24
Immunohistochemical Tumor Analysis
PD-L1 and PD-1 staining was performed at Merck Research Laboratories on formalin-fixed, paraffin-embedded tissue sections. Slides were subjected to heat-induced epitope retrieval and blocking of endogenous peroxidase before incubation with the primary antibody (anti–PD-L1 mAb clone 22C3 [Merck Research Laboratories] or goat anti–PD-1 polyclonal antibody [R&D Systems]). Antigen–antibody binding was visualized with the use of 3,3′-diaminobenzidine (Dako) for PD-L1 or Alexa Fluor 488 (Invitrogen) for PD-1. Samples were considered to be positive for PD-L1 if 1% or more of tumor cells expressed PD-L1. Tumor sections were also stained with anti-CD8 (clone 144B, Dako) to detect CD8+ T cells. Intratumoral CD8+ T cells (completely surrounded by tumor and not abutting stroma) were scored by a dermatopathologist who was unaware of patient characteristics, as described previously25 and in Figure S2 in the Supplementary Appendix. Selected specimens were assessed with multispectral immunohistochemical analysis, which provided simultaneous detection and quantitation of neuron-specific enolase (Merkel tumor cells), CD8, CD68 (macrophages), PD-1, and PD-L1 (see the Methods section in the Supplementary Appendix).
Statistical Analysis
Patients who received at least one dose of pembrolizumab were included in the safety and efficacy analyses. Data are reported as of February 12, 2016. Radiologic and physical-examination assessments according to RECIST, version 1.1, were used to determine treatment responses.19 The best overall response was defined as the best response recorded from the start of the treatment until disease progression or recurrence. The objective response rate was calculated as the percentage of patients who had a complete or partial response that was confirmed by a subsequent radiologic imaging study according to RECIST, version 1.1,19 among all the patients who received at least one dose of pembrolizumab and had at least one evaluation during treatment. Clopper–Pearson exact confidence intervals were generated for the response rate. Time to response was defined as the time interval between the first administered dose of the drug and the date of first response. Duration of response was defined as the time interval between the date of first response and the date of disease progression or death. For patients who did not have disease progression or die, the end date for response duration was the later of the last disease assessment or last treatment administration. Progression-free survival was defined as the time interval from the date of the first dose of pembrolizumab to the date of disease progression or death, whichever occurred earlier, and was estimated with the use of the Kaplan–Meier method.26 An unconditional exact test was used to assess associations between PD-L1 expression and clinical response or viral status.27 The Mann–Whitney U test was used to compare distributions of CD8 scores between virus-positive patients and virus-negative patients.
Results
Patient Characteristics
A total of 26 patients with stage IIIB or IV Merkel-cell carcinoma and an ECOG performance status of 0 or 1 were enrolled from January 2015 until December 2015 and received at least one dose of pembrolizumab. Patient characteristics at baseline are shown in Table 1. The median age of the patients was 68 years (range, 57 to 91). Nine patients were classified as having MCPyV-negative tumors (35%), and 17 were classified as having MCPyV-positive tumors (65%). No patients had received previous systemic therapy for advanced Merkel-cell carcinoma; however, one patient had received adjuvant chemotherapy more than 6 months before beginning study treatment.
Table 1.
Patient Characteristics.*
| Characteristic | All Patients (N = 26) |
Patients with Virus-Positive Tumors (N = 17) |
Patients with Virus- Negative Tumors (N = 9) |
|---|---|---|---|
| Age at enrollment — yr | |||
| Mean | 70.5±8.1 | 67.5±6.0 | 76.3±8.6 |
| Median (range) | 68 (57 to 91) | 67 (57 to 83) | 76 (64 to 91) |
| Sex — no. (%) | |||
| Female | 10 (38) | 4 (24) | 6 (67) |
| Male | 16 (62) | 13 (76) | 3 (33) |
| Disease stage at study entry — no. (%) | |||
| IIIB | 2 (8) | 2 (12) | 0 |
| IV | 24 (92) | 15 (88) | 9 (100) |
| Previous duration of disease — wk† | |||
| Mean | 58.8±56.8 | 71.3±63.5 | 35.2±32.6 |
| Median (range) | 39 (3 to 227) | 53 (3 to 227) | 27 (5 to 104) |
| Baseline extent of disease — mm‡ | |||
| Mean | 81.7±53.9 | 88.7±63.1 | 68.6±28.7 |
| Median (range) | 69 (13 to 182) | 62 (13 to 182) | 75 (36 to 123) |
Plus–minus values are means ±SD.
Previous duration of disease was measured from the date of diagnosis to the date of the first dose of study treatment. An unknown day of diagnosis was imputed as mid-month for one patient.
The extent of disease was measured before treatment initiation as the sum of the longest diameters of tumor target lesions.
Clinical Activity
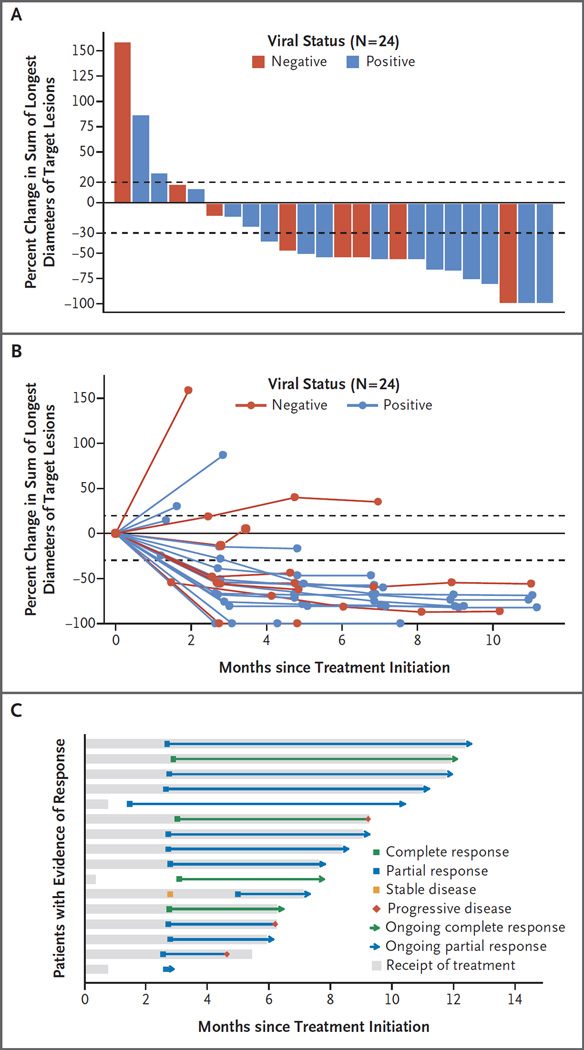
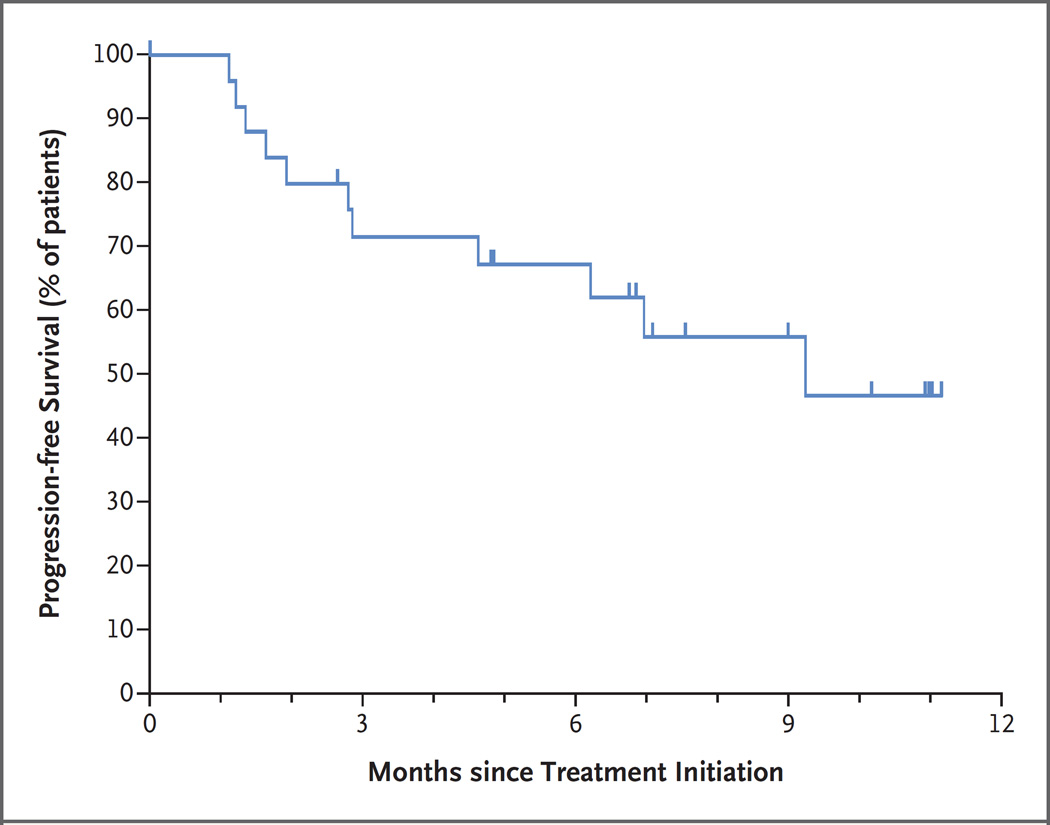
The characteristics of response to anti–PD-1 are shown in Figure 1. A total of 25 patients had at least one tumor assessment during treatment, of whom 14 had a confirmed response (4 with a complete response and 10 with a partial response), representing an objective response rate of 56% (95% confidence interval [CI], 35 to 76). In addition, 1 patient with an unconfirmed partial response continues to receive treatment. One of the 25 patients (4%) had stable disease, and 9 (36%) had progressive disease. The 26th patient has not yet undergone a radiologic assessment for response. Twelve of the 14 confirmed responses (86%) were ongoing at last follow-up. The median follow-up was 33 weeks (range, 7 to 53). With respect to tumor viral status among the 25 patients whose response to treatment could be evaluated, 10 of 16 patients (62%) with virus-positive tumors and 4 of 9 (44%) with virusnegative tumors had an objective response (Fig. 1A and 1B). Among all 26 patients, the median treatment duration was 27 weeks (range, 3 to 57), and 14 patients continue to receive treatment. Among 14 patients with an objective response, the response duration ranged from at least 2.2 months to at least 9.7 months (Fig. 1C). Kaplan–Meier analysis yielded an estimated rate of progression-free survival at 6 months of 67% (95% CI, 49 to 86) (Fig. 2). Among 9 patients who had progressive disease, progression occurred in preexisting target lesions (4 patients), new metastatic sites (2 patients), or both (3 patients). In 2 of the 14 patients with confirmed responses (14%), disease progression developed later, with new metastatic sites in the central nervous system (frontal lobe of the brain in one patient and leptomeningeal sites in the other patient).
Figure 1. Clinical Characteristics of Tumor Response to Pembrolizumab in Patients with Merkel-Cell Carcinoma.
Panel A shows the maximum percent change from baseline in the sum of the longest diameters of target lesions in the 24 patients who underwent radiologic evaluation after treatment initiation. Viral status refers to whether patients had tumors that were positive or negative for the Merkel-cell polyomavirus (MCPyV). Horizontal dashed lines indicate criteria in the Response Evaluation Criteria in Solid Tumors (RECIST), version 1.1, for partial response (≥30% decrease in the sum of the longest diameters of target lesions, with the assumption of no new lesions) and progressive disease (≥20% increase in target-lesion diameters). Data from 2 of the 26 patients are not shown: one had radiographic evidence of disease progression with new lesions, without radiographic evaluation of target lesions, and thus discontinued therapy; the other had not yet undergone radiologic evaluation after initiating pembrolizumab therapy, as of the date of analysis. Panel B shows the kinetics of change in target-lesion diameters over time during pembrolizumab therapy. Rapid and durable reductions in target-lesion diameters were observed in most patients. Two patients with confirmed responses (1 with a partial response and 1 with a complete response) subsequently had progression in nontarget lesions, which are not represented here. Panel C shows the characteristics of 16 patients who initially had evidence of response according to RECIST, version 1.1. Each horizontal bar represents 1 patient. Most responses were observed at the first tumor assessment (approximately 12 weeks after treatment initiation), and 13 of the 16 initial responses (81%) were ongoing at the time of analysis. A total of 14 patients had a confirmed response (2 of whom later had progressive disease); in addition, 1 patient with an unconfirmed partial response continues to receive therapy (bottom bar), and one patient with a transient partial response (i.e., not confirmed by follow-up computed tomographic scanning) subsequently had progressive disease (next-to-bottom bar).
Figure 2. Kaplan–Meier Curve Showing Progression-free Survival among 26 Patients with Merkel-Cell Carcinoma Who Received Pembrolizumab.
Progression-free survival was measured from treatment initiation to disease progression or death, whichever occurred first. Data from patients without an event were censored at the last date of disease assessment (tick marks). The estimated rate of progression-free survival at 6 months was 67% (95% confidence interval [CI], 49 to 86). The median progression-free survival was 9 months (95% CI, 5 months to not reached). As of February 12, 2016, a total of 11 events of disease progression or death had occurred.
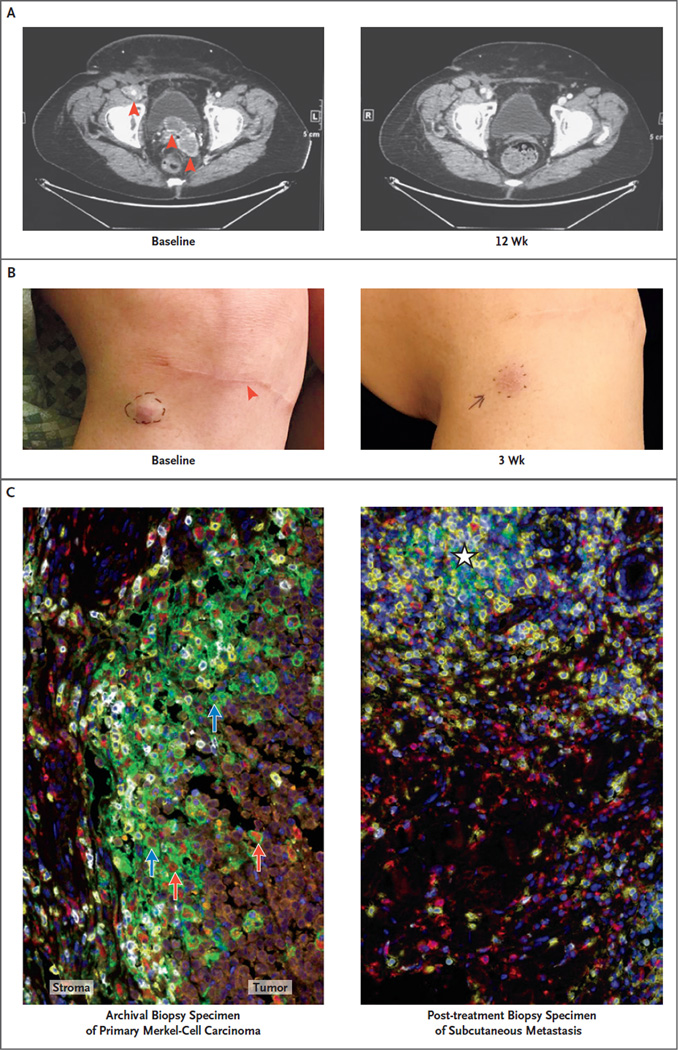
Aspects of the clinical course in a virus-positive patient with a partial tumor regression are shown in Figure 3. This patient with multiorgan metastases showed a substantial reduction in pelvic tumors at the first radiologic evaluation (Fig. 3A) and a complete regression, as assessed by pathological evaluation, of a subcutaneous metastasis 3 weeks after initiating pembrolizu mab therapy (Fig. 3B, and Fig. S1 in the Supplementary Appendix). Multispectral immunohistochemical analysis of an archival specimen of the primary tumor showed PD-L1+ tumor cells and infiltrating macrophages abutting PD1-expressing CD8 cells. Examination of the post-treatment biopsy sample from the adjacent regressing subcutaneous metastasis (which was present at the time of the first pembrolizumab dose) showed inflammation, as evidenced by infiltrates of CD68+ macrophages and CD8+ T cells, without evidence of tumor (Fig. 3C, and Fig. S1 in the Supplementary Appendix).
Figure 3 (facing page). Response to Pembrolizumab in a Patient with Stage IV Merkel-Cell Carcinoma.
This 69-year-old woman received a diagnosis of a primary cutaneous lesion on the right knee and was treated with wide local excision, sentinel lymph-node biopsy, and inguinal lymph-node dissection in November 2013. Recurrent Merkel-cell carcinoma developed in September 2014, with a pelvic mass measuring 11 cm by 7 cm by 14 cm, which was associated with worsening lymphedema and moderate-to-severe right hydroureterone-phrosis requiring a ureteral stent. The patient received radiation therapy to the pelvic mass but in January 2015 was found to have new peritoneal and lymph-node metastases (Panel A, red arrows), as well as several subcutaneous metastases on the right thigh and just below the site of excision of the primary tumor (Panel B; red arrow indicates the site of previous excision of the primary tumor, just below the knee). As shown, these metastatic sites regressed rapidly during anti–programmed death 1 (PD-1) therapy. Also shown are the results of pathological analysis of the primary tumor (Panel C, left) and adjacent post-treatment subcutaneous metastasis (Panel C, right) with multispectral immunohistochemical analysis. Orange indicates Merkel carcinoma cells expressing neuron-specific enolase, yellow CD8+ T cells, red CD68+ macrophages, white PD-1, green the PD-1 ligand PD-L1, and blue nuclear DNA stained with 4′,6-diamidino-2-phenylindole (DAPI). Analysis of the archival biopsy specimen shows an immune infiltrate that is most intense at the tumor–stromal interface, including CD68+ macrophages and CD8+ T cells infiltrating the tumor parenchyma. PD-1 is expressed on 56% of CD8 cells in this microscopic field. PD-L1 is expressed on tumor cells (10% of tumor cells in this field, blue arrows) and macrophages (43% of macrophages in this field, red arrows) and is seen immediately adjacent to PD-1+ lymphocytes. Analysis of the post-treatment biopsy specimen shows a diffuse immune-phagocytic infiltrate and no evidence of residual tumor. The immune infiltrate includes CD68+ macrophages and CD8+ T cells, with an early lymphoid aggregate (white star) where PD-1 and PD-L1 expression is observed.
Safety
Treatment-related adverse events of any grade occurred in 77% of the patients. The most common adverse events were fatigue and laboratory abnormalities (Table S1 in the Supplementary Appendix) — findings that were similar to those in previous reports.3,28 Grade 3 or 4 treatment-related adverse events were observed in 4 of the 26 patients (15%). Two patients had a grade 4 adverse event; one had myocarditis after having received one dose of pembrolizumab and another had elevated levels of alanine aminotransferase and aspartate aminotransferase after having received two doses of pembrolizumab. Both patients had a reduction in the adverse events after discontinuation of pembrolizumab and initiation of glucocorticoid treatment. Both also had tumor regressions that are ongoing (one partial and one complete) (Fig. 1C).
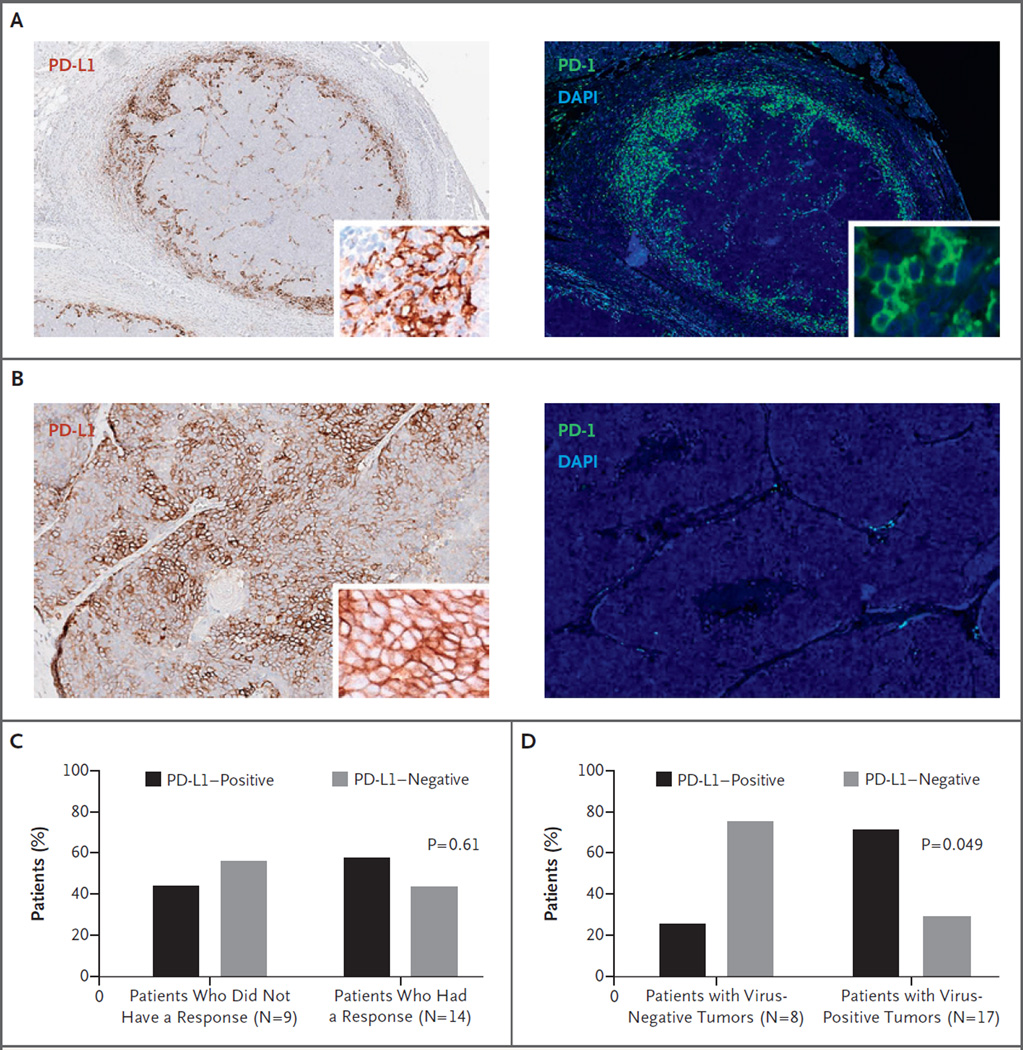
Correlation of Tumor Pathologic Features with Clinical Outcomes
PD-L1 expression could be evaluated in pretreatment tumor specimens from 25 of the 26 patients. PD-L1, the major ligand for PD-1, can be expressed on tumor cells or on infiltrating immune cells (such as macrophages), which are a prominent feature of Merkel-cell carcinoma (Fig. 3C).17,18,29 Furthermore, PD-L1 expression can occur on either cell type in an “adaptive” pattern (i.e., at the interface with infiltrating lymphocytes and presumably promoted by inflammatory cytokines) (Fig. 4A) or on tumor cells in a “constitutive” pattern (i.e., uniform expression not associated with infiltrating lymphocytes, probably driven by genetic or epigenetic events intrinsic to tumor cells) (Fig. 4B). In our analysis of tumors from 25 patients, neither PD-L1 expression on tumor cells (Fig. 4C) nor expression on infiltrating immune cells (not shown) correlated significantly with clinical response to pembrolizumab. PD-L1 expression was more frequent in virus-positive tumors than in virus-negative tumors (71% vs. 25%, P = 0.049) (Fig. 4D). There was no significant correlation of intratumoral CD8 T-cell infiltration with clinical response or with viral status (Fig. S2 in the Supplementary Appendix).
Figure 4. Expression of PD-1 and PD-L1 in Pretreatment Tumor Specimens, Detected by Immunohistochemical Testing.
Tumor-cell expression of PD-L1 (≥1% of tumor cells) was observed in 56% of tumors (14 of 25). Panels A and B show the results of chromogenic staining for PD-L1 (brown), immunofluorescent staining for PD-1 (green), and DAPI staining for nuclear DNA (blue). In most PD-L1+ tumors (11 of 14; 79%), PD-L1 expression was observed only in association with PD-1+ lymphoid infiltrates, typical of an “adaptive immune resistance” pattern (Panel A). One tumor (Panel B) showed broad, constitutive tumor-cell expression of PD-L1 that was independent of lymphoid infiltrates, with only a small focal area (not shown) of adaptive PD-L1 expression at the tumor periphery. The remaining two PD-L1+ tumors showed geographic areas of both constitutive and adaptive patterns of PD-L1 expression (not shown). As shown in Panel C, no significant association was observed between pretreatment tumor PD-L1 expression and response to pembrolizumab according to RECIST, version 1.1, among the 23 patients included in this analysis (P = 0.61 by unconditional exact test on a two-by-two contingency table). Of the 3 patients who were not included in this analysis, 1 had not yet undergone a response evaluation, 1 had an unconfirmed response, and 1 had a stained tumor specimen that was technically inadequate. Samples were considered to be PD-L1–positive if at least 1% of tumor cells expressed PD-L1. Panel D shows the correlation of tumor MCPyV status with PD-L1 expression. A total of 71% of virus-positive tumors also showed PD-L1 expression on tumor cells; in contrast, only 25% of virus-negative tumors were positive for PD-L1 (P = 0.049 by unconditional exact test). Only 25 of the 26 patients were included in this analysis, because 1 patient had a stained tumor specimen that was technically inadequate.
Discussion
The PD-1–blocking antibodies pembrolizumab and nivolumab are promising therapies for patients with advanced metastatic melanoma and non–small-cell lung cancer, and nivolumab was approved for the treatment of renal-cell carcinoma, on the basis of clinical trials showing durable antitumor efficacy and a favorable safety profile.3,28,30–33 Clinical trials in additional cancer types have shown encouraging results,5,34–36 whereas some other cancers appear to be refractory to anti–PD-1 therapy.3 Potential factors associated with response, including tumor PD-L1 expression, the presence of CD8 T cells at the “invading tumor margin,”37 and high tumor mutational load, are currently under investigation.
Merkel-cell carcinoma exemplifies the intersection of several exploratory biomarker categories: it is often associated with PD-L1 expression and CD8 infiltrates, and it can have a high mutational burden (carcinogen [ultraviolet light]–induced) or can be virus-associated. The presence of oncogenic viruses in virus-associated cancers, wherein viral antigens serve as tumor-specific antigens, has recently been proposed as a potential mechanistic marker that can predict response to anti–PD-1 therapy. More than 20% of all cancers worldwide are virus-associated and may have low or modest mutational burdens owing to tumorigenesis driven by the dominant effects of viral oncogenes. Viral antigens are foreign and thus potentially strong immune stimulants, and many virus-associated tumors are characterized by robust immune infiltrates and PD-L1 expression.17,38
These observations provide a strong rationale for assessing the efficacy of PD-1 pathway blockade in patients with advanced, previously untreated Merkel-cell carcinoma, an orphan disease for which available systemic cancer therapies do not meaningfully extend survival. In this study, response to pembrolizumab did not correlate with PD-L1 expression, a finding that contrasts with reports on some other cancer types. This may be because the response rate is relatively high and thus larger numbers of patients may be required to discern the discriminatory capacity of this test, although technical factors such as tumor sampling error and the use of archival tissues may also play a role. Ongoing studies correlating other features of the tumor microenvironment with clinical outcomes of anti–PD-1 or anti–PD-L1 therapy — examining the expression of additional immune checkpoints; the composition, density, and geography of T-cell infiltrates; gene-expression profiles; and single-variable vs. multiplex analyses — are anticipated to reveal more specific and powerful predictors. As of now, none of the predictive tests are sufficiently robust to be used in clinical decision making regarding whether to use or not to use PD-1 blockers in Merkel-cell carcinoma.
In the current study of pembrolizumab therapy in Merkel-cell carcinoma, we observed a 56% objective response rate. Tumor regressions occurred in multiple organ sites and in patients with bulky disease. Regressions appeared to be durable within an observation period of up to 9.7 months after initial documentation of a response. Twelve of 14 confirmed responses were ongoing at the time of analysis, and the estimated rate of progression-free survival at 6 months was 67%. Although additional experience with longer follow-up and larger patient cohorts is needed, these early findings compare favorably with results for standard chemotherapy regimens for this tumor,7,39 for which retrospective studies show a median progression-free survival of approximately 3 months, with progressive disease developing in 90% of patients within 10 months.6 Pembrolizumab was associated with previously described toxic effects in the relatively elderly patient population included in this study (median age, 68 years); we observed a 15% rate of grade 3 or 4 adverse events that were managed by discontinuation of pembrolizumab and initiation of glucocorticoid treatment as needed, without clear adverse effects on the magnitude or duration of tumor response.
We observed responses to anti–PD-1 in both MCPyV-positive and MCPyV-negative Merkel-cell carcinomas, which are reported to have markedly dichotomous mutational burdens. The median of 1121 mutations per exome reported in virus-negative Merkel-cell carcinoma exceeds the mutational burdens reported for other cancers that are responsive to anti–PD-1 or anti–PD-L1 therapies, including melanoma, squamous and nonsquamous non–small-cell lung cancers, and cancers of the bladder, head and neck, and kidney.15,40 Conversely, the median of 12.5 mutations per exome observed in virus-positive Merkel-cell carcinoma is below those reported for tumor types that are poorly responsive to anti–PD-1, such as prostate and pancreatic cancer. Thus, potentially through distinct mechanisms (viral antigen expression or high tumor mutational load), both virus-positive and virus-negative Merkel-cell carcinomas appear to be immunogenic and susceptible to immune therapy by inhibition of the PD-1 pathway. Our current understanding of the mechanism of antitumor immunity induced by PD-1 blockade centers on the unleashing of an endogenous repertoire of T cells specific for neo-epitopes generated by a small subset of somatic mutations in the tumor — so-called mutation-associated neoantigens. However, because the mutational load of MCPyV-positive Merkel-cell carcinoma is so low, our findings, together with previous findings of MCPyV T-antigen–specific T cells in patients with virus-positive Merkel-cell carcinoma, suggest that antigens expressed by oncogenic viruses represent a distinct category of T-cell targets for immune checkpoint blockade.
Supplementary Material
Acknowledgments
Supported by grants (1U01CA154967, to Dr. Cheever; K24-CA-139052 and R01-CA-162522, to Dr. Nghiem; and R01CA142779, to Dr. Taube) from the National Cancer Institute and by Merck.
We thank the patients and their families and caregivers for participating in this study; Jared Lunceford of Merck for bio-statistical advice; Judith Kaiser of the Cancer Immunotherapy Trials Network (CITN) for oversight of the budgetary and legal issues for this trial; Nirasha Ramchurren of the CITN Immune Monitoring Lab for assistance with correlative marker studies; Nichole Pelz of the Seattle Cancer Care Alliance for study patient care; and Haiying Xu, Aleksandra Ogurtsova, and Peter Nguyen of Johns Hopkins University for technical assistance.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12:252–264. doi: 10.1038/nrc3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell. 2015;27:450–461. doi: 10.1016/j.ccell.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti–PD-1 antibody in cancer. N Engl J Med. 2012;366:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rizvi NA, Hellmann MD, Snyder A, et al. Cancer immunology: mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348:124–128. doi: 10.1126/science.aaa1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le DT, Uram JN, Wang H, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med. 2015;372:2509–2520. doi: 10.1056/NEJMoa1500596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iyer J, Blom A, Doumani R, et al. Response rate and durability of chemotherapy for metastatic Merkel cell carcinoma among 62 patients. J Clin Oncol. 2014;32(Suppl):52. abstract. [Google Scholar]
- 7.Tai PT, Yu E, Winquist E, et al. Chemotherapy in neuroendocrine/Merkel cell carcinoma of the skin: case series and review of 204 cases. J Clin Oncol. 2000;18:2493–2499. doi: 10.1200/JCO.2000.18.12.2493. [DOI] [PubMed] [Google Scholar]
- 8.Paulson KG, Iyer JG, Blom A, et al. Systemic immune suppression predicts diminished Merkel cell carcinoma-specific survival independent of stage. J Invest Dermatol. 2013;133:642–646. doi: 10.1038/jid.2012.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feng H, Shuda M, Chang Y, Moore PS. Clonal integration of a polyomavirus in human Merkel cell carcinoma. Science. 2008;319:1096–1100. doi: 10.1126/science.1152586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iyer JG, Afanasiev OK, McClurkan C, et al. Merkel cell polyomavirus-specific CD8+ and CD4+ T-cell responses identified in Merkel cell carcinomas and blood. Clin Cancer Res. 2011;17:6671–6680. doi: 10.1158/1078-0432.CCR-11-1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Afanasiev OK, Yelistratova L, Miller N, et al. Merkel polyomavirus-specific T cells fluctuate with Merkel cell carcinoma burden and express therapeutically targetable PD-1 and Tim-3 exhaustion markers. Clin Cancer Res. 2013;19:5351–5360. doi: 10.1158/1078-0432.CCR-13-0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paulson KG, Carter JJ, Johnson LG, et al. Antibodies to Merkel cell polyomavirus T antigen oncoproteins reflect tumor burden in Merkel cell carcinoma patients. Cancer Res. 2010;70:8388–8397. doi: 10.1158/0008-5472.CAN-10-2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong SQ, Waldeck K, Vergara IA, et al. UV-associated mutations underlie the etiology of MCV-negative Merkel cell carcinomas. Cancer Res. 2015;75:5228–5234. doi: 10.1158/0008-5472.CAN-15-1877. [DOI] [PubMed] [Google Scholar]
- 14.Harms PW, Vats P, Verhaegen ME, et al. The distinctive mutational spectra of polyomavirus-negative Merkel cell carcinoma. Cancer Res. 2015;75:3720–3727. doi: 10.1158/0008-5472.CAN-15-0702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goh G, Walradt T, Markarov V, et al. Mutational landscape of MCPyV-positive and MCPyV-negative Merkel cell carcinomas with implications for immunotherapy. Oncotarget. 2016;7:3403–3415. doi: 10.18632/oncotarget.6494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taube JM, Anders RA, Young GD, et al. Colocalization of inflammatory response with B7-h1 expression in human melanocytic lesions supports an adaptive resistance mechanism of immune escape. Sci Transl Med. 2012;4:127ra37. doi: 10.1126/scitranslmed.3003689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lipson EJ, Vincent JG, Loyo M, et al. PD-L1 expression in the Merkel cell carcinoma microenvironment: association with inflammation, Merkel cell polyomavirus and overall survival. Cancer Immunol Res. 2013;1:54–63. doi: 10.1158/2326-6066.CIR-13-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dowlatshahi M, Huang V, Gehad AE, et al. Tumor-specific T cells in human Merkel cell carcinomas: a possible role for Tregs and T-cell exhaustion in reducing T-cell responses. J Invest Dermatol. 2013;133:1879–1889. doi: 10.1038/jid.2013.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45:228–247. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 20.Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–655. [PubMed] [Google Scholar]
- 21.National Institutes of Health, National Cancer Institute. Common terminology criteria for adverse events v4.0. 2009 May 28; ( http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_8.5x11.pdf)
- 22.Shuda M, Arora R, Kwun HJ, et al. Human Merkel cell polyomavirus infection I. MCV T antigen expression in Merkel cell carcinoma, lymphoid tissues and lymphoid tumors. Int J Cancer. 2009;125:1243–1249. doi: 10.1002/ijc.24510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Doumani R, Moshiri A, Yelistratova L, et al. Detection of the Merkel cell polyomavirus in human Merkel cell carcinomas and the clinical implications of tumor viral status. J Invest Dermatol. 2015;135(Suppl S44) abstract. [Google Scholar]
- 24.Lyngaa R, Pedersen NW, Schrama D, et al. T-cell responses to oncogenic Merkel cell polyomavirus proteins distinguish patients with Merkel cell carcinoma from healthy donors. Clin Cancer Res. 2014;20:1768–1778. doi: 10.1158/1078-0432.CCR-13-2697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paulson KG, Iyer JG, Tegeder AR, et al. Transcriptome-wide studies of Merkel cell carcinoma and validation of intratumoral CD8+ lymphocyte invasion as an independent predictor of survival. J Clin Oncol. 2011;29:1539–1546. doi: 10.1200/JCO.2010.30.6308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 27.Berger RL. More powerful tests from confidence interval p values. Am Stat. 1996;50:314–318. [Google Scholar]
- 28.Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti–PD-1) in melanoma. N Engl J Med. 2013;369:134–144. doi: 10.1056/NEJMoa1305133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Behr DS, Peitsch WK, Hametner C, et al. Prognostic value of immune cell infiltration, tertiary lymphoid structures and PD-L1 expression in Merkel cell carcinomas. Int J Clin Exp Pathol. 2014;7:7610–7621. [PMC free article] [PubMed] [Google Scholar]
- 30.Robert C, Long GV, Brady B, et al. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med. 2015;372:320–330. doi: 10.1056/NEJMoa1412082. [DOI] [PubMed] [Google Scholar]
- 31.Garon EB, Rizvi NA, Hui R, et al. Pembrolizumab for the treatment of non–small-cell lung cancer. N Engl J Med. 2015;372:2018–2028. doi: 10.1056/NEJMoa1501824. [DOI] [PubMed] [Google Scholar]
- 32.Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous-cell non–small-cell lung cancer. N Engl J Med. 2015;373:123–135. doi: 10.1056/NEJMoa1504627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Motzer RJ, Escudier B, McDermott DF, et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373:1803–1813. doi: 10.1056/NEJMoa1510665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ansell SM, Lesokhin AM, Borrello I, et al. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin’s lymphoma. N Engl J Med. 2015;372:311–319. doi: 10.1056/NEJMoa1411087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Seiwert TY, Haddad RI, Gupta S, et al. Antitumor activity and safety of pembrolizumab in patients with advanced squamous cell carcinoma of the head and neck: preliminary results from KEYNOTE-012 expansion cohort. J Clin Oncol. 2015;33(Suppl) doi: 10.1200/JCO.2016.68.1478. LBA6008. abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Powles T, Eder JP, Fine GD, et al. MPDL3280A (anti-PD-L1) treatment leads to clinical activity in metastatic bladder cancer. Nature. 2014;515:558–562. doi: 10.1038/nature13904. [DOI] [PubMed] [Google Scholar]
- 37.Tumeh PC, Harview CL, Yearley JH, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515:568–571. doi: 10.1038/nature13954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lyford-Pike S, Peng S, Young GD, et al. Evidence for a role of the PD-1:PD-L1 pathway in immune resistance of HPV-associated head and neck squamous cell carcinoma. Cancer Res. 2013;73:1733–1741. doi: 10.1158/0008-5472.CAN-12-2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Voog E, Biron P, Martin JP, Blay JY. Chemotherapy for patients with locally advanced or metastatic Merkel cell carcinoma. Cancer. 1999;85:2589–2595. doi: 10.1002/(sici)1097-0142(19990615)85:12<2589::aid-cncr15>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 40.Lawrence MS, Stojanov P, Polak P, et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature. 2013;499:214–218. doi: 10.1038/nature12213. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.