Abstract
Background and Purpose
The “stroke belt” is described as an 8-state region with high stroke mortality across the southeastern US. Using spatial statistics we identified clusters of high stroke mortality (hot-spots) and adjacent areas of low stroke mortality (cool-spots) for US counties, and evaluated for regional differences in county-level risk factors.
Methods
A cross-sectional study of stroke mortality was conducted using Multiple Cause of Death data (Centers for Disease Control and Prevention) to compute age-adjusted adult stroke mortality rates for US counties. Local indicators of spatial association (LISA) statistics were used for hot-spot mapping. County-level variables were compared between hot- and cool-spots.
Results
Between 2008 and 2010 there were 393,121 stroke-related deaths. Median age-adjusted adult stroke mortality was 61.7 per 100,000 persons (IQR=51.4–74.7). We identified 705 hot-spot counties (22.4%), and 234 cool-spot counties (7.5%). 44.5% of hot-spot counties were located outside of the stroke belt. Hot-spots had greater proportions of black residents, higher rates of unemployment, chronic disease, and healthcare utilization, and lower median income and educational attainment.
Conclusions
Clusters of high stroke mortality exist beyond the 8-state stroke belt, and variation exists within the stroke belt. Reconsideration of the stroke belt definition and increased attention to local determinants of health underlying small area regional variability could inform targeted healthcare interventions.
Introduction
The “stroke belt,” an 8-state region in the southeastern US, defined for its disproportionately high stroke mortality rates,1, 2 has been present since at least 1940, and persists despite recent decreases in stroke mortality, overall.3 Differences in vascular risk factors may explain approximately half of the excess burden,4 yet underlying drivers in this region are not fully understood.1 Access to primary stroke centers (PSCs) is lower within the region, suggesting that differential access to care could be one contributing factor.5, 6
Using the existing state-based definition may not provide adequate geographic precision to fully understand the impact of local demographic and healthcare factors as determinants of health. We used county-level data and spatial statistics to empirically identify geographic clusters of high stroke mortality, or hot-spots, at a finer geographic resolution to compare with the traditional state-based stroke belt. We compared multiple county-level variables between high stroke mortality hot-spots and adjacent low stroke mortality cool-spots, to understand local factors contributing to stroke outcomes.
Methods
We used Multiple Cause of Death data (Centers for Disease Control and Prevention) from 2008–2010 to calculate a 3-year average age-adjusted adult stroke mortality rate for all US counties. ICD-10 codes I60-I69 were used to identify stroke as cause of death.
Local indicators of spatial association (LISA) statistics were used to describe spatial patterns of mortality rates. This technique categorizes counties as: clustered high-rate counties (High-High, HH); low-rate counties adjacent to High-High counties (Low-High, LH); clustered low-rate counties (Low-Low, LL); high-rate counties adjacent to Low-Low counties (High-Low, HL). Non-significant counties demonstrate spatial randomness among neighbors. We compared High-High and Low-High counties, respectively “hot-spots” and “cool-spots.” Hot-spots do not include HL counties and cool-spots do not include LL counties.
We analyzed county-level demographic characteristics (2008–2012 American Community Survey), healthcare resources and utilization rates (2008, 2010 Area Health Resource File), and prevalence of diabetes, obesity (2011 Food Environment Atlas), and hypertension (Institute for Health Metrics and Evaluation). Data describing access to PSCs used previously described methods.7 We used Wilcoxon rank-sum tests to compare averages. Spatial methods are further described in the online supplement.
Results
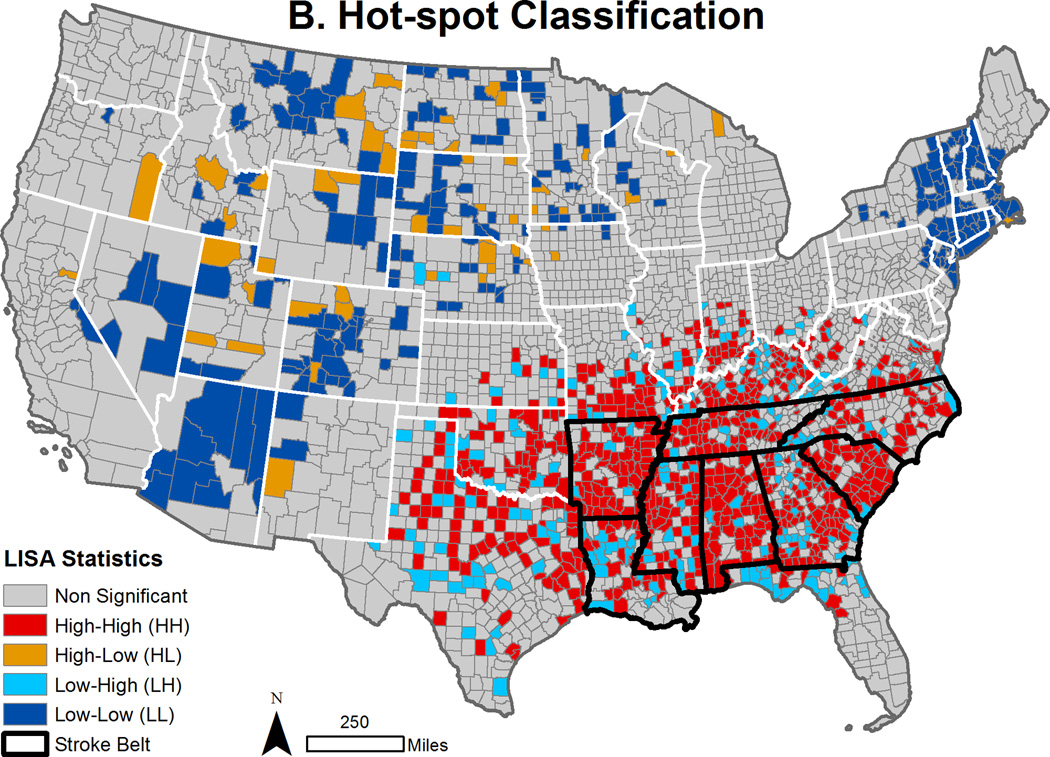
From 2008–2010, 393,121 stroke deaths were reported across 3,137 counties. Median county-level age-adjusted stroke mortality was 61.7 per 100,000 persons (IQR=51.4–74.6) (Figure 1A). The hot-spot analysis identified 705 HH (22.4%), 234 LH (7.5%), 238 LL (7.6%), and 52 HL (1.7%) counties (Figure 1B). Of the 688 counties included in the 8-state stroke belt, there were 391 HH (57.4%) and 91 LH (13.2%). The other 314 HH counties were located outside of the 8-state region.
Figure 1. Stroke Mortality Rates and Hot-spots Mapped by County.
Panel A presents a US county map showing stroke mortality rates (2008–2010). Rates are reported per 100,000 persons; binned by quintile. Panel B shows stroke mortality hot-spot classifications. Local indicators of spatial association (LISA) statistics identify counties (significance level p<0.05), as high-high (HH), low-high (LH), low-low (LL), high-low (HL) or not significant. In panels A and B, stroke belt states are outlined in black.
Compared to cool-spots, hot-spots had significantly larger proportions of black residents; higher rates of unemployment, obesity, diabetes, hypertension; more hospital admissions and emergency department visits per capita; and lower median income and educational attainment (Table 1). 60-minute access to a PSC was available for 65.2% of people nationally, 31.5% of the population in hot-spot counties, and 50.7% in cool-spot counties. Median county-level PSC access did not differ overall or stratified by urbanicity (Supplemental Table 1).
Table 1. Comparison of Hot-spot and Cool-spot Counties.
Table 1 provides national totals and county medians for multiple variables, and compares hot-spots and cool-spots using Wilcoxon rank-sum (Mann-Whitney) tests.
| All Counties n = 3,137 |
Hot-spot Counties (HH) n = 705 |
Cool-spot Counties (LH) n = 234 |
|||
|---|---|---|---|---|---|
| National Total |
Median (IQR) | Median (IQR) | Median (IQR) | P-Value | |
| Adjusted Stroke Mortality Rate (per 100k pop) |
56.1 | 61.7 (51.4–74.7) | 83.6 (76.5–95.5) | 46.1 (38.9–51.6) | <0.001 |
| Urban Population (%) | 80.6 | 40.6 (12.2–67) | 31.4 (10.4–51.5) | 26.5 (0–55.1) | 0.459 |
| Median Age (Yrs) | 37.2 | 40.4 (37.4–43.3) | 39.9 (37.6–42) | 40.4 (38–42.9) | 0.033 |
| Black Population (%) | 12.6 | 2.1 (0.5–10.4) | 10.4 (1.9–32.1) | 4.8 (1–19) | <0.001 |
| Hispanic Population (%) | 16.4 | 3.3 (1.6–8.3) | 2.6 (1.4–5.7) | 2.9 (1.5–6.3) | 0.221 |
| Median Household Income ($, 2012) |
53,046 | 43809 (37,970–50,697) |
37508 (33,333–42,256) |
40682.5 (34,848–48,596) |
<0.001 |
| Unemployment Rate (%) | 9.3 | 8.4 (6.2–10.7) | 10.2 (8–12.6) | 9 (6.9–10.7) | <0.001 |
| Education High School or Less (%) |
42.5 | 51.2 (43.8–58.7) | 58.7 (53.1–63.7) | 56 (47–62.6) | <0.001 |
| No Health Insurance (%) | 14.9 | 14.6 (11–18.5) | 17.1 (14.7–19.9) | 16.7 (13.8–20.2) | 0.131 |
| Adult Diabetes (%) | 9.0 | 9.8 (8.5–11.3) | 11.6 (10.4–12.7) | 10.7 (9.5–11.9) | <0.001 |
| Adult Obesity (%) | 26.5 | 29.1 (27.2–31) | 31.1 (29.5–32.8) | 29.9 (27.5–31.8) | <0.001 |
| Adult Hypertension (%) | 37.2 | 38.8 (37.1–41.2) | 42.2 (40.4–44.9) | 40.4 (38.7–42.9) | <0.001 |
| MDs (per 100k pop) | 30.3 | 25.5 (15.5–39.4) | 22.7 (14.5–33.3) | 20.1 (11.5–31.8) | 0.031 |
| Hospitals (per 100k pop) | 2.1 | 1 (1–2) | 1 (1–1) | 1 (0–1) | 0.034 |
| Hospital Admissions (per 100k pop) |
86.8 | 69 (27.2–119.2) | 71.6 (21.1–126.7) | 48.2 (0–95.9) | <0.001 |
| ED Visits (per 100k pop) | 396.3 | 369 (169.7–536.1) | 432.1 (110.5–603.3) | 331.7 (0–521.9) | <0.001 |
| Medicare Eligible Population (%) |
14.7 | 18.2 (15.3–21.3) | 19.1 (16.5–21.5) | 18.3 (15.1–20.6) | 0.003 |
Discussion
Our results confirmed past findings that high stroke mortality is geographically clustered in the southeast, and detected clusters of high stroke mortality existing outside of the traditional 8-state stroke belt. A state-based approach misses nearly half of counties identified empirically as hot-spots. We identified cool-spots within the stroke belt where mortality is lower than expected. County-level heterogeneity suggests that state-based analyses may limit our understanding of the underlying drivers of survival through misclassification bias. Since things that are geographically close tend to be more similar,8 identifying areas that have significantly different mortality rates, despite close proximity, may help explain the drivers of disparities in outcomes.
There was a higher rate of 60-minute PSC access for people living in hot-spots than cool-spots, however, a statistically significant difference for county-level averages was not observed. We found a paradoxical relationship between the number of physicians and mortality, with more physicians on average in hot-spots than cool-spots. These findings combined may suggest that differential access to healthcare and specialty stroke care may not be the key factor underlying geographic variability in stroke mortality. It is possible that more granular scales of analysis are needed to detect meaningful differences (the mortality data used restricted us to a county-level analysis).
We found statistically significant differences in prevalence of diabetes, obesity, and hypertension between hot-spots and cool-spots. However, differences in disease severity or disease control may be magnifying relatively small differences in prevalence.
This study has limitations. The stability of spatial patterns of mortality over time is not known, but a prior study found that 75% of stroke hospitalization clusters were stable over 10 years.9 This cross-sectional, population-level analysis cannot assess causality. Population-level associations may not apply at the individual level. Due to the low number of HL counties (n=52), comparisons of HL and LL precluded a meaningful analysis.
Conclusion
Clusters of high stroke mortality exist beyond the 8-state stroke belt, and variation exists within the stroke belt. Reconsideration of the stroke belt definition and increased attention to small area regional variability using spatial methods may allow for better classification of regional disparities and inform targeted healthcare interventions.
Supplementary Material
Acknowledgments
Funding
This work was supported by the Agency for Healthcare Research and Quality (AHRQ-R01-HS018362-01A1).
Footnotes
Disclosures
Dr. Carr spends a portion of his time as Director of the Emergency Care Coordination Center in the Office of the Assistant Secretary for Preparedness and Response. Findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the Department of Health and Human Services.
References
- 1.Howard G. Why do we have a stroke belt in the southeastern United States? A review of unlikely and uninvestigated potential causes. The American journal of the medical sciences. 1999;317:160–167. doi: 10.1097/00000441-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 3.Lanska DJ. Geographic distribution of stroke mortality in the United States: 1939–1941 to 1979–1981. Neurology. 1993;43:1839–1851. doi: 10.1212/wnl.43.9.1839. [DOI] [PubMed] [Google Scholar]
- 4.Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, et al. Traditional risk factors as the underlying cause of racial disparities in stroke: lessons from the half-full (empty?) glass. Stroke. 2011;42:3369–3375. doi: 10.1161/STROKEAHA.111.625277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mullen MT, Judd S, Howard VJ, Kasner SE, Branas CC, Albright KC, et al. Disparities in evaluation at certified primary stroke centers: reasons for geographic and racial differences in stroke. Stroke. 2013;44:1930–1935. doi: 10.1161/STROKEAHA.111.000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mullen MT, Wiebe DJ, Bowman A, Wolff CS, Albright KC, Roy J, et al. Disparities in accessibility of certified primary stroke centers. Stroke. 2014;45:3381–3388. doi: 10.1161/STROKEAHA.114.006021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Albright KC, Branas CC, Meyer BC, Matherne-Meyer DE, Zivin JA, Lyden PD, et al. ACCESS: acute cerebrovascular care in emergency stroke systems. Arch Neurol. 2010;67:1210–1218. doi: 10.1001/archneurol.2010.250. [DOI] [PubMed] [Google Scholar]
- 8.Tobler WR. A computer movie simulating urban growth in the Detroit region. Economic geography. 1970:234–240. [Google Scholar]
- 9.Schieb LJ, Mobley LR, George M, Casper M. Tracking stroke hospitalization clusters over time and associations with county-level socioeconomic and healthcare characteristics. Stroke. 2013;44:146–152. doi: 10.1161/STROKEAHA.112.669705. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.