Abstract
Objectives
Late-life bereavement is associated with an increased risk of mortality. This study assesses the associations among bereavement, cardiovascular disease (CVD), and depressive symptoms on mortality in older men and women.
Methods
We examined data from the Cardiovascular Health Study, a prospective population-based cohort study of older adults. We compared mortality in those who became bereaved from 1989–1999 (n=593) to an age- and sex-matched sample of individuals who remained married (n=593). Cox regression was used to examine the association between bereavement and 3-year all-cause mortality and whether or not the association differed by sex, presence of CVD or post-bereavement depressive symptoms.
Results
One hundred ninety-nine (16.8%) individuals died. There was no association of bereavement with mortality, HR= 0.98 (0.74, 1.30). However, there were significant interaction effects of bereavement with participant sex (p<.001) and CVD (p=.010). Bereavement decreased the risk of mortality in women (HR=0.67 (0.46, 0.97)) and increased the risk of mortality in men (HR=1.77 (1.14, 2.75)). Within sex, the association of bereavement with mortality differed according to CVD status. The reduced risk of mortality associated with bereavement in women was only observed in women with CVD and the increased risk in men was only observed in men without CVD. High levels of depressive symptoms attenuated the relation between bereavement and mortality in men without CVD.
Conclusions
The relation between bereavement and mortality was different in men and women and varied by CVD status. Bereavement decreased mortality in women with CVD and increased mortality in men without CVD.
Keywords: older adults, spousal bereavement, cardiovascular disease, gender differences, depressive symptoms, mortality
It is well documented that late-life spousal bereavement is associated with excess risk of mortality. (1,2) Excess mortality in widowed populations is highest in the early months after bereavement and decreases over time. (3,4) Even though the mortality of bereavement has been described in several populations, the role of modifying factors after bereavement such as incident cardiovascular disease (CVD) and depressive symptoms are not well understood. (3) Bereavement increases the risk for cardiovascular events (5) and depressive symptoms (6). Each of these factors—bereavement, (1–4) CVD, (7) and depression (7) – have been independently linked to mortality, but they have not been examined together in a single study. It is not known whether CVD and depression modify the association between bereavement and mortality. The goals of this study are to determine whether or not CVD and depression modify the association of bereavement with 3-year mortality in older men and women. We also want to determine whether depression after spousal death attenuates the association between bereavement and mortality.
Traditional perspectives of bereavement (cumulative stress hypotheses) suggest that spousal death is a significant source of psychological stress. Individuals must cope with the loss of their spouse and at the same time cope with the stressors associated with the new role of being a widow/widower. (8) Those who are overwhelmed by grief may discontinue daily tasks that are essential for the maintenance of their health, which increases the risk for early death. Both CVD and depression also increase the risk for early death in older adults. (7) The cumulative stress perspective would argue that the combined effects of spousal death, CVD, and/or depression deplete older adults’ coping resources making them even more vulnerable to early death. We would expect that older adults with CVD and older adults with high levels of depression are particularly vulnerable to the increased mortality risk after bereavement.
A more recent opposing perspective (stress reduction hypotheses) suggests that spousal death is associated with stress reduction and relief when it occurs in the context of long term chronic illness with high levels of patient suffering prior to death. (9–11) The process of dying likely entails intense spousal caregiving demands along with exposure to the suffering of a loved one. (10,12) According to this view, spousal death results in the removal of these stressors, which may contribute to survival. Based on this perspective, women may benefit more from the death of their spouse than men because they are more sensitive to the suffering of their spouse and are more likely to be involved in providing care for their spouse. (12)
Existing research on bereavement, CVD, and mortality has a number of limitations. First, most studies follow participants for an average of 11 years even though the increased risk of death has been most consistently observed in the first few years after bereavement. (1) Second, studies have relied on self-report methods to determine physical health status, (13–17) and several of these studies limit their analyses to baseline prevalent disease assessed before becoming bereaved. (13–15) Third, among the bereavement studies that examine physical health status as a predictor of mortality, none include depressive symptoms as a covariate in testing predictive models. (1, 13–17) The present study addresses these limitations by testing the association of spousal loss to 3-year mortality and whether or not the association differs by sex, CVD status or in the presence of post-bereavement depressive symptoms.
Our study had two objectives. First, we examined the relation between spousal loss and 3-year all-cause mortality. We hypothesized that bereaved elders would be at increased risk of mortality compared to age- and sex-matched married controls. Because the effects of spousal chronic illness and suffering are typically greater on women than men, we hypothesized that spousal loss would interact with participant sex such that the impact of bereavement on mortality would be less negative for women than for men (10). We also hypothesized that spousal loss would interact with prevalent CVD status prior to death to affect mortality.
Second, we expanded on previous research by examining post-bereavement variables in our model including incident CVD and depression. We hypothesized that bereavement would interact with CVD to affect mortality. We also hypothesized bereavement would interact with post-bereavement depressive symptoms to affect mortality. We expected that bereaved elders with a greater frequency of depressive symptoms post-bereavement would be at increased risk for mortality compared to bereaved elders with less frequency of depressive symptoms. Finally, we also examined whether depression after spousal loss is the process or mechanism linking bereavement to mortality. We expected that depression would attenuate the relation between bereavement and mortality.
Participants and Methods
Study Population
The Cardiovascular Health Study is a prospective, observational study designed to determine the risk factors for and consequences of cardiovascular disease in older adults. Participants aged 65 and older were recruited from random samples of Medicare eligibility lists in four communities: Sacramento County, California; Washington County, Maryland; Forsyth County, North Carolina; and Pittsburgh, Pennsylvania, and from age-eligible participants in the same household. Potential participants were excluded if they were institutionalized, wheelchair bound in the home, or under active treatment for cancer. A total of 5,201 men and women aged 65 or older were enrolled in 1989 – 1990 (n= 5,201) and a supplemental cohort of 687 African Americans was enrolled in 1992 – 1993. Participants underwent annual clinical examinations and completed an extensive array of demographic and health assessments. Additional information regarding the design and sampling procedures have been published previously. (18) The CHS sample included 1,332 married couples. Of these, 593 experienced the death of a spouse between 1989 and 1999. This constituted our bereaved sample. Each bereaved spouse was randomly matched one-to-one to a non-bereaved married participant on sex, CHS cohort (1989/90 or 1992/93), survival to and age (within 1 year) at the time of bereavement.
Bereavement
Deaths were confirmed through CHS reviews of obituaries, medical records, death certificates, National Death Index searches, searches of Medicare claims data, and proxy interviews. The CHS has complete follow-up on mortality. All deaths were adjudicated by a group of physicians who reviewed all documentation about the circumstances of death to determine underlying cause of death. The CHS classification categories for underlying cause of death have been previously reported. (22) We focused on surviving spouses’ mortality in the first 3 years after the date of spousal death. The married controls’ follow-up waves were matched to the bereaved sample. Baseline for this study was defined as the date of spousal death for the matched pair.
Predictors of Mortality
Sociodemographic information included age at the time of spousal death (and the corresponding time for controls), sex, and race, coded as Black or non-Black due to the small number identifying as other racial groups.
Cardiovascular disease (CVD) was evaluated at CHS entry by clinical and laboratory examination. Incident events were ascertained via surveillance calls every six months, annual clinic visits, medical records, and/or participant-initiated phone calls. Both cardiovascular and cerebrovascular endpoints were adjudicated by the CHS events committee. (19) CVD was measured as: [1] Clinical disease including angina pectoris, myocardial infarction, bypass, congestive heart failure, intermittent claudication, stroke, and transient ischemic attack; and [2] Subclinical disease indicators including the Rose questionnaires for claudication and angina1, ratio of ankle to arm blood pressure, major ECG abnormality, and carotid stenosis at the closest interview visit prior to spousal death. The methods used to determine clinical and subclinical and diseases in the CHS have been previously published. (20,21) CVD was examined in two ways. First, prevalent CVD status prior to spousal death was analyzed as a fixed variable. It was defined as baseline clinical disease and any incident events that occurred prior to death of spouse. Second, we examined CVD as a time-dependent covariate by updating CVD status to include incident non-fatal CVD events occurring after spousal death.
Depressive symptoms were assessed using the 10-item version of the Center for Epidemiological Studies Depression Scale (CES-D 10). The scale ranges from 0–30, with higher scores indicating a greater frequency of depressive symptoms. CES-D scores ≥ 8 are associated with an increased risk of developing major depression. (22) Because we were interested in the depression after bereavement we used the CES-D collected during the closest interview visit following the date of spousal death. The mean time between the widowhood date for the matched pair and the date of the next visit was 192 days. 1,080 participants had a visit following the widowhood date, and 910 completed the CES-D questionnaire.
Analytical Methods
To compare baseline characteristics of participants who became bereaved versus those who did not, we used the Wilcoxon rank-sum test for continuous variables and the Pearson χ2 test for categorical variables. To examine the relationship between bereavement and 3-year all-cause mortality, we performed survival analyses using Cox regression models, censoring follow-up time at 3 years for participants still alive at that time. The interaction of bereavement with sex was tested and found significant, leading to the decision to stratify analyses by sex. Models were built sequentially, beginning with an unadjusted model, then adjusting for age and race, and then for clinical and subclinical CVD, and finally for post-bereavement depressive symptoms and time-dependent CVD status. Interactions of bereavement status with CVD and depressive symptoms were assessed.
It is important to note that depressive symptoms post bereavement was missing for 276 individuals (23%). Missingness is informative, as participants who died shortly after the bereavement date would not have had the opportunity to attend a clinic visit and complete the depression scale. To preserve the full data set, we categorized the depression scale into 3 groups based on having a depression score <8 (unlikely to be depressed) ≥8 (at risk for depression), or missing. The coefficient of the missing indicator is not interpretable, but it kept the full data set intact. In sensitivity analyses, we compared the results of this approach with one using the observed data only and modeling the score linearly, and with each of two models where the missing depression scores were coded either 0 or 1 in order to put bounds on the estimated hazard ratios. In no case was there a significant interaction of widowhood with depressive symptoms, and the upper and lower bounds for the coefficient of widowhood from the sensitivity analyses were within the estimated confidence interval for the method chosen. Results of the complete case analyses were also consistent with the method chosen. For all analyses, p values smaller than 0.05 were considered to be statistically significant. All analyses were performed using SPSS, version 20.0 and STATA, version 12.
Results
Table 1 reports descriptive statistics for all model variables. At the time of spousal death, bereaved and married control participants were approximately 78 years of age (SD=5.6 years). Approximately 73% of the total sample was female. Most of the sample (94%) was White. There were no baseline differences in the matching variables or in prevalent and subclinical CVD between the bereaved and married control samples. After 3 years of follow-up, 199 (16.8%) deaths occurred evenly divided between the bereaved and non-bereaved participants. Among the 99 bereaved elders who died, 63 participants died from non-CVD (e.g., dementia, cancer, infection, and accidents), 34 participants died from coronary heart diseases (CHD), and 2 participants died from other CVD. Among the 100 married controls who died, 51 participants died from non-cardiovascular diseases, 44 participants died from CHD, and 5 participants died from other CVD. The distribution of deaths between the bereaved and married control samples was not significantly different, χ2 (4) = 4.86, p=.31.
Table 1.
Participant Characteristics and Descriptions of Variables at the Time of Spousal Death
| Characteristics | Married Sample (n=593) | Bereaved Sample (n=593) | p Value, married vs. bereaved |
|---|---|---|---|
| Age, mean (SD), years | 77.75 (5.67) | 77.77 (5.69) | 0.96 |
| Range (median), years | 66–95 (77.0) | 66–95 (77.0) | |
| Sex | >.99 | ||
| Women | 430 (72.5) | 430 (72.5) | |
| Men | 163 (27.5) | 163 (27.5) | |
| Race | |||
| White | 555 (93.6) | 559 (94.3) | 0.25 |
| Black | 36 (6.1) | 31 (5.2) | |
| Asian/Pacific Islander | 0 (0) | 2 (0.3) | |
| American Indian | 2 (0.3) | 0 (0) | |
| Other | 0 (0) | 1 (0.2) | |
| Prevalent disease, overall | 184 (31.0) | 193 (32.5) | 0.31 |
| Angina pectoris | 119 (20.1) | 130 (21.9) | 0.48 |
| Myocardial infarction | 61 (10.3) | 68 (11.5) | 0.58 |
| Bypass | 32 (5.4) | 37 (6.2) | 0.31 |
| Congestive heart failure | 49 (8.3) | 55 (9.3) | 0.61 |
| Intermittent claudication | 13 (2.2) | 14 (2.4) | >.99 |
| Stroke | 42 (7.1) | 49 (8.3) | 0.51 |
| Transcient ischemic attack | 21 (3.5) | 33 (5.6) | 0.06 |
| Subclinical disease, overall | 208 (35.1) | 210 (35.4) | 0.48 |
| Rose questionnaire for claudication | 5 (0.8) | 10 (1.7) | 0.29 |
| Rose questionnaire for angina | 15 (2.5) | 15 (2.5) | >.99 |
| Ratio of ankle to arm blood pressure | 63 (10.6) | 57 (9.6) | 0.63 |
| Right and left ankle to arm blood pressure indicating atherosclerotic obstruciton to blood flow in the legs; measured in clinic, ≤ 0.90 | |||
| Major ECG abnormality | 157 (26.5) | 175 (29.5) | 0.27 |
| Measured during baseline ECG, any of the following: ventricular conduction defects, major Q/Qs wave abnormalities, left ventricular hypertriphy, isolated major ST-T-wave abnormalities, atrial fibrillation, or first-degree antriocentricular block | |||
| Carotid stenosis | 244 (41.1) | 239 (40.3) | 0.81 |
| Measured during baseline carotid ultrasound for left or right: carotid stress > 25th percentile | |||
| No prevalent or subclinical disease | 201 (33.9) | 190 (32.0) | 0.27 |
Notes. All data are presented as number (percentage) unless otherwise indicated.
EEG= electrocardiogram.
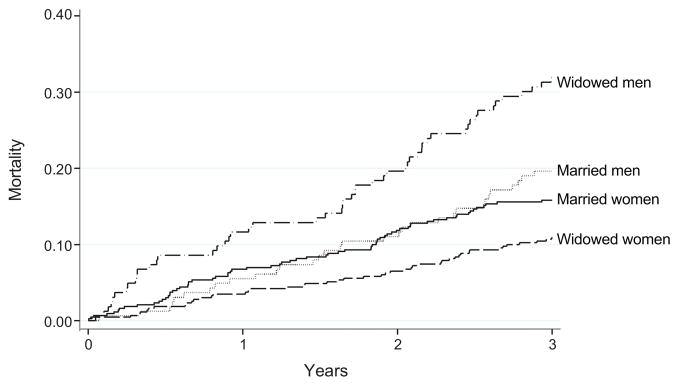
In the full sample, there was no association of widowhood with mortality, HR= 0.98 (0.74, 1.30). p=.91. There was a significant interaction of sex with widowhood, p=.001. Unadjusted, the HR of widowhood for women was 0.67 (0.46, 0.96), p=.032 and for men was 1.77 (1.14, 2.75), p=.011 (Figure 1 and Table 2.)
Figure 1.
Kaplan-Meier curves for 3-year mortality for bereaved and married men and women
Table 2.
Hazard Ratios for Bereavement for Older Men and Women
| Model | Men N=326 |
Women N=860 |
||
|---|---|---|---|---|
| HR (95% CI) | p -value | HR (95% CI) | p -value | |
| 1 | 1.77 (1.14, 2.75) | 0.011 | 0.67 (0.46, 0.96) | 0.032 |
| 2 | 1.76 (1.13, 2.73) | 0.012 | 0.63 (0.43, 0.91) | 0.015 |
| 3 | 1.63 (1.04, 2.55) | 0.032 | 0.98 (0.58, 1.66) if no CVD | 0.938 |
| 0.40 (0.23, 0.68) with CVD | 0.001 | |||
| 4 | 2.89 (1.22, 6.85) if no CVD | 0.030 | 0.96 (0.50, 1.83) if no CVD | 0.890 |
| 0.95 (0.56, 1.61) with CVD | 0.847 | 0.37 (0.23, 0.60) with CVD | <.001 |
Notes. 1 Unadjusted
2 Adjusted for age and race
3 Adjusted for subclinical CVD and prevalent CVD with an interaction of widowhood with prevalent CVD; p-value for interaction term =.21 in men and .019 in women.
4 Includes post bereavement depression and an interaction with time-dependent CVD; p-value for interaction term=.033 in men and .022 in women
Pre-bereavement predictors of mortality
In the full sample, in addition to a significant interaction with sex, there was also a significant interaction of widowhood with prevalent CVD (p=.010). When stratified, the interaction did not reach statistical significance in men until adjustment model 4, when CVD status was updated. Table 3 shows the number of deaths by marital status, sex, and prevalent CVD. Bereaved men without CVD were more likely to die than married men without CVD (26.6% vs. 14.3%), but bereavement status did not significantly affect 3-year mortality in men with CVD. In women without CVD, there was no difference in mortality by bereavement status, but in women with CVD, those who became bereaved were less likely to die within 3 years than those who remained married (17.4% vs. 34.5%).
Table 3.
Number (%) of Participants who died within 3 Years by Marital Status, Sex, and Prevalent CVD at the Time of Bereavement.
| Men
|
Women
|
|||
|---|---|---|---|---|
| No CVD | with CVD | No CVD | with CVD | |
| Married | ||||
| Total N | 98 | 65 | 311 | 119 |
| # (%) died | 14 (14.3) | 18 (27.7) | 27 (8.7) | 41 (34.5) |
|
| ||||
| Bereaved | ||||
| Total N | 79 | 84 | 321 | 109 |
| # (%) died | 21 (26.6) | 31 (36.9) | 28 (8.7) | 19 (17.4) |
|
| ||||
| p value* | 0.041 | 0.24 | 0.99 | 0.004 |
Notes. Total number of participants is 1186. Total # deaths = 199 (16.8% [women = 115; men = 84]).
Chi-square test for bereavement within groups defined by sex and prevalent CVD.
Table 3 shows the hazard ratios for bereavement for men and women with several levels of adjustment. Unadjusted, the HR of bereavement for women was 0.67 (0.46, 0.96), p<.05 and in the opposite direction for men, 1.77 (1.14, 2.75), p<.05 (model 1). Adjusting for age at the time of bereavement and race, the HRs of bereavement for women and men remained significant, p<.05 (model 2). In a model adjusted for subclinical CVD and an interaction between bereavement and prevalent CVD, bereavement decreased the risk of 3-year mortality in women with CVD by more than half, but did not significantly alter the risk of mortality in women who did not have CVD. Bereavement increased the risk of 3-year mortality in men (model 3). Each year of age increased the risk of death by 14% (data not shown). Participant race and subclinical CVD were not significant predictors of mortality.
Post-bereavement predictors of mortality
Associations of bereavement with 3-year mortality were consistent with additional adjustment for time-dependent non-fatal CVD and depressive symptoms post bereavement (model 4). There was a significant interaction of bereavement with updated CVD status in both men and women. Participants with a CES-D score >=8 were more likely to die within 3 years than participants with a score <8 (HR (95% CI) =1.74 (1.13, 2.68)), but there was no significant interaction between depressive symptoms and bereavement (data not shown). Adding depressive symptoms attenuated the association of bereavement with mortality in men without CVD and results were not attenuated with the addition of depression for women with CVD.
Post-hoc Analyses
The finding that bereavement reduced the risk of mortality for women with CVD raised questions about the health status of their spouses prior to death. This would provide some information on whether bereaved women were more likely to be caregivers than bereaved men. Bereaved women’s spouses had significantly more prevalent CVD than bereaved men’s spouses at the wave prior to death (62% vs. 51%; p=.025). We also looked at the deceased spouses’ cause of death. Bereaved women’s spouses died from more Atherosclerotic CVD than bereaved men’s spouses (30% vs. 22%; p=.031).
Discussion
Adjusting for sociodemographic variables and subclinical disease prior to spousal death, these data show that the relation between bereavement and 3-year mortality varies by participant sex. Bereavement decreased the risk of mortality in women and increased the risk of mortality in men. Within sex, the association of bereavement with mortality differed according to CVD status. We found that bereavement decreases mortality risk in women with CVD prior to and shortly after their husband’s death. Bereavement did not affect mortality for men with CVD. However, bereaved men without CVD had significantly higher mortality rates than married men without CVD. Finally, high levels of depressive symptoms were significantly associated with mortality. High levels of depressive symptoms attenuated the association between bereavement and mortality in men.
These findings pose two important questions: Given the existing literature suggesting bereavement increases mortality risk, [1] why did we find this association only for bereaved men without CVD, and [2] why was bereavement protective for women with CVD? The increased mortality among bereaved compared to non-bereaved men without CVD is consistent with a small number of studies that have found that good physical health does not protect individuals from mortality after bereavement. (16, 17, 25). These studies hypothesize that good physical health is not protective in the context of spousal loss because most of the excess mortality after bereavement is due to unexpected cardiac and respiratory events. (15, 24, 28). It is important to note that the lack of an association between bereavement and mortality in men with CVD may be partially attributable to the fact that most CVD in men is fatal. (29) The effect of CVD on mortality in men may be so strong that experiencing spousal loss does not increase risk of death. Men in good physical health may also experience the greatest relative impact of bereavement on mortality. Indeed, we found that depression attenuated the association between bereavement and mortality in men without CVD. High levels of depressive symptoms after spousal death may be the process or mechanism linking bereavement to early mortality in men in good physical health. This is an important finding that should be explored in future studies.
Bereaved women with CVD might benefit more in terms of reduced mortality rates when compared to married women with CVD because the death of their spouse eliminates a major life stressor for them (stress reduction perspective). Women are more likely than men to provide care to their physically declining spouse and are more negatively affected by the suffering of a dying spouse. (10, 12) Thus, spousal death would eliminate the stress of caregiving and exposure to suffering, allowing bereaved women with CVD to focus on managing their own chronic and incident disease, which in turn would promote their survival. (10, 12) Bereaved women with existing or incident CVD may also be more vigilant and protective of their health than married women with chronic disease. The death of one’s husband may heighten perceptions of vulnerability among women with chronic disease and possibly foster better self-care. Research is needed to determine whether the removal of caregiver stress or perceptions of vulnerability are the mechanisms linking bereavement to survival in women with CVD.
Contrary to our hypothesis, we did not find a significant interaction between depressive symptoms and bereavement. There were also no differences in the association of depressive symptoms with CVD status. There are several possible explanations for why we did not find a significant interaction between depressive symptoms and bereavement. First, the mental health effects of bereavement include a combination of symptoms that include depression, post-traumatic stress, and/or grief. (1, 30) Including only one mental health outcome in our bereavement model may not have provided a comprehensive view of psychological adjustment following spousal death. Second, to the extent that the depression-mortality link may be driven by cardiovascular, metabolic, inflammatory, and behavioral pathways, our length of follow-up (3 years) may have been too short to observe a significant depressive effect. (31) One study that found a significant association between depression and mortality after bereavement included a 7 year follow-up. (32)
The present study had several limitations. First, we did not have available data on subclinical disease at every interview visit prior to spousal death. In order to preserve our sample size, we examined subclinical disease status at the closest interview visit prior to spousal death (1989/1999, 1992/1993 or 1998/1999). Second, we did not have information on clinical diagnoses of major depressive disorder. It is possible that the association of bereavement with mortality would be mitigated among those who successfully completed depression treatment in the early months after bereavement. Third, we do not have information about the length of the marriage and do not know if this was their first (or second) marriage or if they were previously bereaved. Finally, we did not have available data on social support (emotional, tangible) and behavioral (nutrition, physical activity, sleep) changes at every interview visit prior to and after spousal death. Future studies should focus on these mechanisms underlying the association between bereavement and mortality.
In conclusion, our findings suggest that the relation between bereavement and mortality differs in men and women and varies by cardiovascular disease status. Bereavement decreased mortality in women with CVD and increased mortality in men without CVD. Depressive symptoms post-bereavement may be the mechanism linking bereavement to mortality in physically healthy men. These findings support the notion that bereavement is a time-dependent dynamic process. It is possible that women with CVD exhibited stress reduction effects and men without CVD showed cumulative stress effects. However, there is a need for further research on older women with CVD to understand how they are differentially affected by bereavement compared to older women without CVD. Additional research is also needed to understand why physically healthy men are at the greatest risk of mortality after bereavement. Given these complex interactions, we encourage replication of our tested model with a focus on possible mechanisms underlying the bereavement by CVD difference in men in women. Finally, these findings highlight the need for health care professionals to monitor the physical health of bereaved individuals and to offer universal support after spousal death to improve longevity.
Acknowledgments
Source of funding
This research was supported by contracts HHSN268201200036C, HHSN268200800007C, N01HC55222, N01HC85079, N01HC85080, N01HC85081, N01HC85082, N01HC85083, N01HC85086, and grant U01HL080295 from the National Heart, Lung, and Blood Institute (NHLBI), with additional contribution from the National Institute of Neurological Disorders and Stroke (NINDS). Additional support was provided by R01AG023629 from the National Institute on Aging (NIA). A full list of principal CHS investigators and institutions can be found at CHS-NHLBI.org. Preparation of this manuscript was also supported in part by grants from NIH P30 MH090333-01A1, MHO19986, NR009573, NR013450, AG026010, AG032370, NSF 0540865, and MH103467.
Abbreviations
- CES-D
Center for Epidemiologic Studies Depression Scale
- CHS
Cardiovascular Health Study
- CI
confidence interval
- CVD
cardiovascular disease
- ECG
electrocardiogram
- HR
hazard ratio
Footnotes
Rose G, McCartney P, Reid DD. Self-administration of a questionnaire on chest pain and intermittent claudication. Br J Prev Soc Med. 1977 Mar;31(1):42–48.
Conflicts of Interest
All authors report no competing interests.
References
- 1.Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet. 2007;370:1960–1973. doi: 10.1016/S0140-6736(07)61816-9. [DOI] [PubMed] [Google Scholar]
- 2.Stroebe MS, Stroebe W. The mortality of bereavement: A review. In: Stroebe MS, Stroebe W, Hanson RO, editors. Handbook of bereavement: Theory, Research, and Intervention. New York: Cambridge University Press; 1993. pp. 175–195. [Google Scholar]
- 3.Moon JR, Kondo N, Glymour N, Subramanian SV. Widowhood and mortality: A meta-analysis. PLos ONE. 2011;6:e23465. doi: 10.1371/journal.pone.0023465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roelfs DJ, Shor E, Curreli M, Clemow L, Burg MM, Schwartz JE. Widowhood and mortality: A meta-analysis and meta-regression. Demography. 2012;49:575–606. doi: 10.1007/s13524-012-0096-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carey IM, Shah SM, DeWilde S, Harris T, Victor CR, Cook DG. Increased risk of acute cardiovascular events after partner bereavement: A matched cohort study. JAMA Intern Med. 2014;174:598–605. doi: 10.1001/jamainternmed.2013.14558. [DOI] [PubMed] [Google Scholar]
- 6.Buckley T, Bartopr R, McKinley S, Ward C, Bramwell M, Roche D, Mihailidou AS, Morel-Kopp MC, Spinaze M, Hocking B, Goldston K, Tennant C, Tofler G. Prospective study of early bereavement on psychological and behavioural cardiac risk factors. Intern Med J. 2009;39:370–378. doi: 10.1111/j.1445-5994.2009.01879.x. [DOI] [PubMed] [Google Scholar]
- 7.Schulz R, Beach SR, Ives DG, Martire LM, Ariyo AA, Kop WJ. Association between depression and mortality in older adults. Arch Intern Med. 1999;60:1761–1768. doi: 10.1001/archinte.160.12.1761. [DOI] [PubMed] [Google Scholar]
- 8.Stroebe M, Schut The dual process model of coping with bereavement: A decade on. Omega. 2010;61(4):273–289. doi: 10.2190/OM.61.4.b. [DOI] [PubMed] [Google Scholar]
- 9.Schulz R, Mendelsohn AB, Haley WE, Mahoney D, Allen RS, Zhang S, Thompson L, Belle SH. End of life care and the effects of bereavement on family caregivers of persons with dementia. New Engl J Med. 2003;349(20):1936–1942. doi: 10.1056/NEJMsa035373. [DOI] [PubMed] [Google Scholar]
- 10.Schulz R, Beach SR, Hebert R, Martire LM, Monin JK, Tompkins CA, Albert SM. Spousal suffering and partner’s depression and cardiovascular disease: The Cardiovascular Health Study. Am J Geriat Psychiat. 2009;17(3):246–254. doi: 10.1097/JGP.0b013e318198775b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schulz R, Beach SR, Lind B, Martire LM, Zdaniuk B, Hirsch C, Jackson S, Burton L. Involvement in caregiving and adjustment to death of a spouse: findings from the caregiver health effects study. JAMA. 2001;285:3123–3129. doi: 10.1001/jama.285.24.3123. [DOI] [PubMed] [Google Scholar]
- 12.Monin J, Schulz R. Interpersonal Effects of Suffering in Older Adult Caregiving Relationships. Psychol Aging. 2009;24:681–695. doi: 10.1037/a0016355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Newman AB, Sachs MC, Arnold AM, Fried LP, Kronmal R, Cushman M, Psaty BM, Harris TB, Robbins JA, Burke GL, Kuller LH, Lumley T. Total and cause-specific mortality in the cardiovascular health study. Journals Gerontol A-Biol. 2009;64:1251–1261. doi: 10.1093/gerona/glp127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hart CL, Hole DJ, Lawlor DA, Smith DG, Lever TF. Effect of conjugal bereavement on mortality of the bereaved spouse in participants of the Renfrew/Paisley Study. J Epidemiol Commun H. 2007;61:455–460. doi: 10.1136/jech.2006.052043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elwert F, Christakis NA. The effect of widowhood on mortality by the causes of death of both spouses. Am J Public Health. 2008;98:2092–2098. doi: 10.2105/AJPH.2007.114348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boyle PJ, Feng Z, Raab G. Does widowhood increase mortality risk?: Testing for selection effects by comparing causes of spousal death. Epidemiology. 2011;22:1–5. doi: 10.1097/EDE.0b013e3181fdcc0b. [DOI] [PubMed] [Google Scholar]
- 17.Shah SM, Carey IM, Harris T, DeWilde S, Victor CR, Cook DG. Do good health and material circumstances protect older people from the increased risk of death after bereavement? Am J Epidemiol. 2012;176:689–698. doi: 10.1093/aje/kws162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, Kuller LH, Manolio TA, Mittelmark MB, Newman A, O’Leary DH, Psaty B, Rautaharju P, Tracy RP, Weiler PG. The cardiovascular health study: Design and rationale. Ann Epidemiol. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 19.Ives DG, Fitzpatrick AL, Bild DE, Psaty BM, Kuller LH, Crowley PM, Cruise RG, Theroux S. Surveillance and ascertainment of cardiovascular events: The cardiovascular health study. Ann Epidemiol. 1995;5:278–285. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- 20.Psaty BM, Kuller LH, Bild D, Burke GL, Kittner SJ, Mittelmark M, Price TR, Rautaharju PM, Robbins J. Methods of assessing prevalent cardiovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1995;5:270–277. doi: 10.1016/1047-2797(94)00092-8. [DOI] [PubMed] [Google Scholar]
- 21.Kuller J, Shemanski L, Psaty BM, Borhani NO, Gardin J, Haan MN, O’Leary DH, Savage PJ, Tell GS, Tracy R. Subclinical disease as an independent risk factor for cardiovascular disease. Circulation. 1995;92:720–726. doi: 10.1161/01.cir.92.4.720. [DOI] [PubMed] [Google Scholar]
- 22.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression scale) Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 23.Ives DG, Samuel P, Psaty BM, Kuller LH. Agreement between nosologist and Cardiovascular Health Study Review of Deaths: Implications for Coding Differences. J Am Geriatr Soc. 2009;57:133–139. doi: 10.1111/j.1532-5415.2008.02056.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martikainen P, Valkonen T. Mortality after the death of a spouse: rates and causes of death in a large Finnish cohort. Am J Public Health. 1996;86(8):1087–1093. doi: 10.2105/ajph.86.8_pt_1.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schaefer C, Quesenberry CP, Wi S. Mortality Following Conjugal Bereavement and the Effects of a Shared Environment. Am J Epidemiol. 1995;141:1142–1152. doi: 10.1093/oxfordjournals.aje.a117387. [DOI] [PubMed] [Google Scholar]
- 26.Ryan DH. Is there a desolation effect after dementia? A comparative study of mortality rates in spouse of dementia patients following admission and bereavement. Int J Geriatr Psychiatry. 1992;7:331–339. [Google Scholar]
- 27.Shah SM, Carey IM, Harris T, DeWilde S, Victor CR, Cook DG. The effect of unexpected bereavement on mortality in older couples. Am J Public Health. 2013;103:1140–1145. doi: 10.2105/AJPH.2012.301050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buckley T, McKinley S, Tofler G, Bartrop R. Cardiovascular risk in early bereavement: a literature review and proposed mechanisms. Int J Nurs Stud. 2010;47(2):229–238. doi: 10.1016/j.ijnurstu.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 29.Institute of Medicine (US) Committee on a National Surveillance System for Cardiovascular and Select Chronic Diseases. Cardiovascular Disease. Washington (DC): National Academies Press (US); 2011. A Nationwide Framework for Surveillance of Cardiovascular and Chronic Lung Diseases; p. 2. Available from: http://www.ncbi.nlm.nih.gov/books/NBK83160/ [PubMed] [Google Scholar]
- 30.Shear MK, Simon N, Wall M, Zisook S, Neimeyer R, Duan N, Reynolds C, Leibowitz B, Sung S, Ghesquiere A, Gorscak B, Clayton P, Ito M, Nakajima S, Konishi T, Meert K, Schiff M, O’Connor MF, First M, Sareen J, Bolton J, Skritskaya N, Mancini AD, Keshaviah A. Complicated grief and related bereavement issues for DSM-5. Depression and Anxiety. 2012 Sep 10;28(2):103–117. doi: 10.1002/da.20780. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Evans DL, Charney DS, Lewis L, Golden RN, Gorman JM, Krishnan KR, Nemeroff CB, Bremner JD, Carney RM, Coyne JC, Delong MR, Frasure-Smith N, Glassman AH, Gold PW, Grant I, Gwyther L, Ironson G, Johnson RL, Kanner AM, Katon WJ, Kaufmann PG, Keefe FJ, Ketter T, Laughren TP, Leserman J, Lyketsos CG, McDonald WM, McEwen BS, Miller AH, Musselman D, O’Connor C, Petitto JM, Pollock BG, Robinson RG, Roose SP, Rowland J, Sheline Y, Sheps DS, Simon G, Spiegel D, Stunkard A, Sunderland T, Tibbits P, Jr, Valvo WJ. Mood disorders in the medically ill: Scientific review and recommendations. Biol Psychiat. 2005;58:175–89. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 32.Stimpson JP, Kuo Y, Ray LA, Raji MA, Peek MK. Risk of Mortality Related to Widowhood in Older Mexican Americans. Ann Epidem. 2007L;4:313–319. doi: 10.1016/j.annepidem.2006.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]