Abstract
A better understanding of overall survival among patients with clinically localized prostate cancer (PCa) in the US Veterans Health Administration (VHA) is critical to inform PCa treatment decisions, especially in light of data from the Prostate Intervention Versus Observation Trial (PIVOT). We sought to describe patterns of survival for all patients with clinically localized PCa treated by the VHA. We created an analytic cohort of 35 954 patients with clinically localized PCa diagnosed from 1995 to 2001, approximating the PIVOT inclusion criteria (age of diagnosis ≤75 yr and clinical stage T2 or lower). Mean patient age was 65.9 yr, and median follow-up was 161 mo. Overall, 22.5% of patients were treated with surgery, 16.6% were treated with radiotherapy, and 23.1% were treated with androgen deprivation. Median survival of the entire cohort was 14.1 yr (25th, 75th percentiles, range: 7.8–18 yr). Among patients who received treatment with curative intent, median survival was 17.9 yr following surgery and 12.9 yr following radiotherapy. One-third of patients died within 10 yr of diagnosis compared with nearly half of the participants in PIVOT. This finding sounds a note of caution when generalizing the mortality data from PIVOT to VHA patients and those in the community.
Patient summary
More than one-third of patients diagnosed with clinically localized prostate cancer treated through the US Veterans Health Administration from 1995 to 2001 died within 10 yr of their diagnosis. Caution should be used when generalizing the estimates of competing mortality data from PIVOT.
Keywords: Prostate cancer, Survival, Competing risks of mortality, Veterans Health Administration
The comparative effectiveness of treatment for clinically localized prostate cancer (PCa) is widely debated [1]. Half or more of identified cases of PCa are clinically insignificant, as they are unlikely to cause symptoms or death [2]. The Prostate Intervention Versus Observation Trial (PIVOT) randomized 731 men with localized PCa to surgery versus observation. Enrollees were diagnosed between 1994 and 2001, were from US Veterans Health Administration (VHA) and National Cancer Institute sites, were aged ≤75 yr, had serum prostate-specific antigen (PSA) <50 ng/ml, had biopsy-proven stage T1 or T2 PCa, and were deemed medically fit for radical prostatectomy, with an estimated life expectancy >10 yr. Survival was not different for patients treated with prostatectomy versus observation across the entire cohort [3].
Current clinical guidelines for PCa recommend using life expectancy estimates to guide the choice between definitive therapy and surveillance because PCa patients often die of competing causes [4]. Despite the selection of men thought to have significant longevity, nearly half (48.4%) of PIVOT participants had died after 10 yr of follow-up [3]. It is possible that competing risks of mortality might differ in the total VHA population, but little is known about the extent of that difference in patients with localized PCa.
The VHA operates the largest national integrated health care system in the United States [5]. The VHA cares for a predominantly male population, and PCa is the most common cancer diagnosis [6]. Users of the VHA represent a population with greater physical, mental, and social challenges than otherwise similar patients [7–11]; however, many older and multimorbid veterans with PCa receive treatment with curative intent [12]. We created a cohort of men with clinically localized PCa who met criteria similar to PIVOT inclusion criteria to better understand patterns of treatment and survival of patients with localized PCa in the VHA. We hypothesized that the survival of this national cohort would be lower than that reported in PIVOT.
We restricted our cohort to patients with PCa who were diagnosed in the period from 1995 through 2001, who were aged ≤75 yr, who had clinical stage T1 or T2 disease, and who were in the Veterans Affairs Central Cancer Registry (VACCR) [6]. We excluded patients with clinical nodal or metastatic disease. The VACCR does not include PSA data for the study period; however, the vast majority of patients treated by the VHA have PSA levels <20 ng/ml [13]. The primary treatment was defined using mutually exclusive categories: surgery, radiotherapy, androgen deprivation therapy, or conservative management. We calculated survival using the US Department of Veterans Affairs Vital Status File, which compiles data from the VHA, the Centers for Medicare and Medicaid, the Social Security Administration, and the National Cemetery Association [14]. We censored patient follow-up as of January 1, 2015. We constructed Kaplan-Meier product limit estimates to determine median survival rates and survival rates at selected time points. We used SAS v9.4 (SAS Institute, Cary, NC, USA) and JMP Pro v12 (SAS Institute) for our analyses.
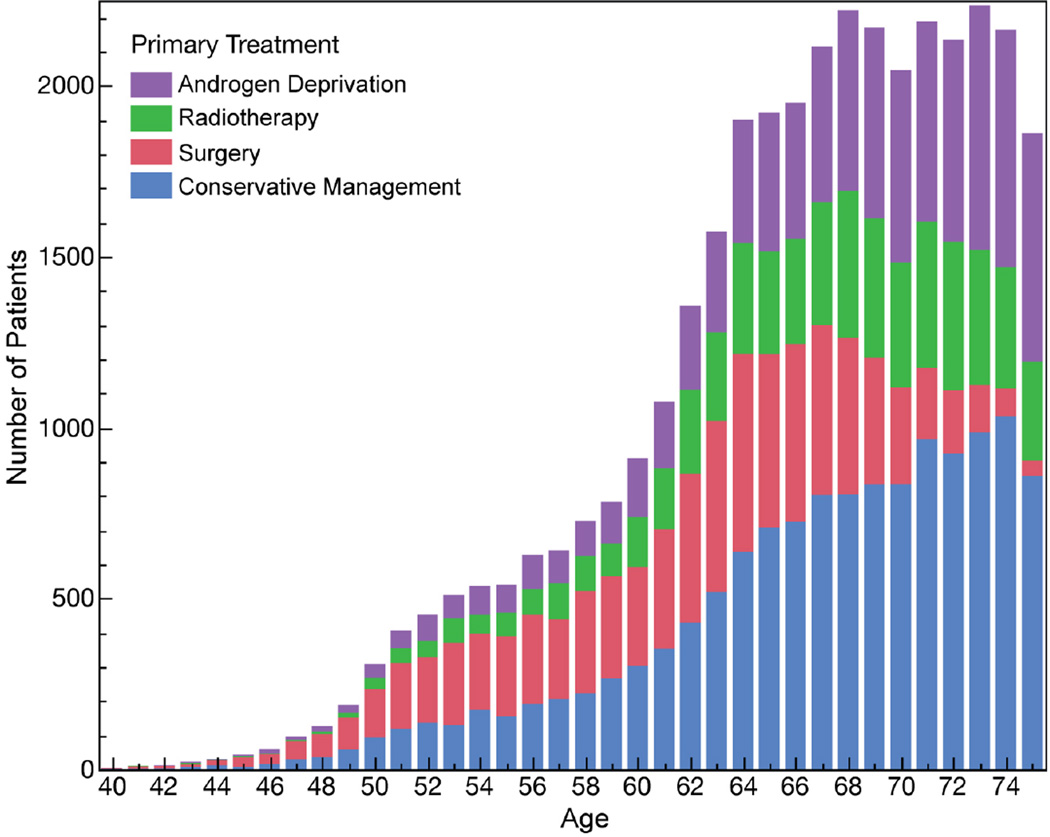
The mean age of our cohort was 65.9 yr, with 18 268 clinical stage T1 and 17 686 clinical stage T2 patients. Conservative management was the most common primary treatment (n = 13 601, 37.8%), followed by androgen deprivation therapy (n = 8314, 23.1%), surgery (n = 8073, 22.5%), and radiotherapy (n = 5966, 16.6%). Among the 12 630 patients aged ≥70 yr, 5607 received conservative management, 3815 received androgen deprivation therapy, 938 had surgery, and 2270 had radiotherapy (Fig. 1).
Fig. 1.
The primary treatment of clinically localized prostate cancer in the US Veterans Health Administration from 1995 to 2001. The total number of patients (n = 35 954) with clinically localized prostate cancer is plotted by patient age and treatment type. Surgery was the most common treatment among men aged <60 yr (2626, 42.8%) and declined steadily among men aged 60–69 yr (4509, 26.2%) and 70–75 yr (938, 7.4%). The percentage of men receiving radiotherapy increased slightly with increasing patient age (6.5% for age <50 yr, 12.7% for 50–59 yr, 17.2% for 60–69 yr, 18.0% for 70–75 yr). The number and percentage of patients treated with androgen deprivation therapy increased with patient age (11.7% for age <50 yr, 14.8% for 50–59 yr, 21.0% for 60–69 yr, 30.2% for 70–75 yr). Conservative therapy also increased with increasing patient age (30.3% for age <50 yr, 30.7% for 50–59 yr, 35.6% for 60–69 yr, 44.4% for 70–75 yr). Conservative management was the most common treatment for men aged >60 yr (39.3%).
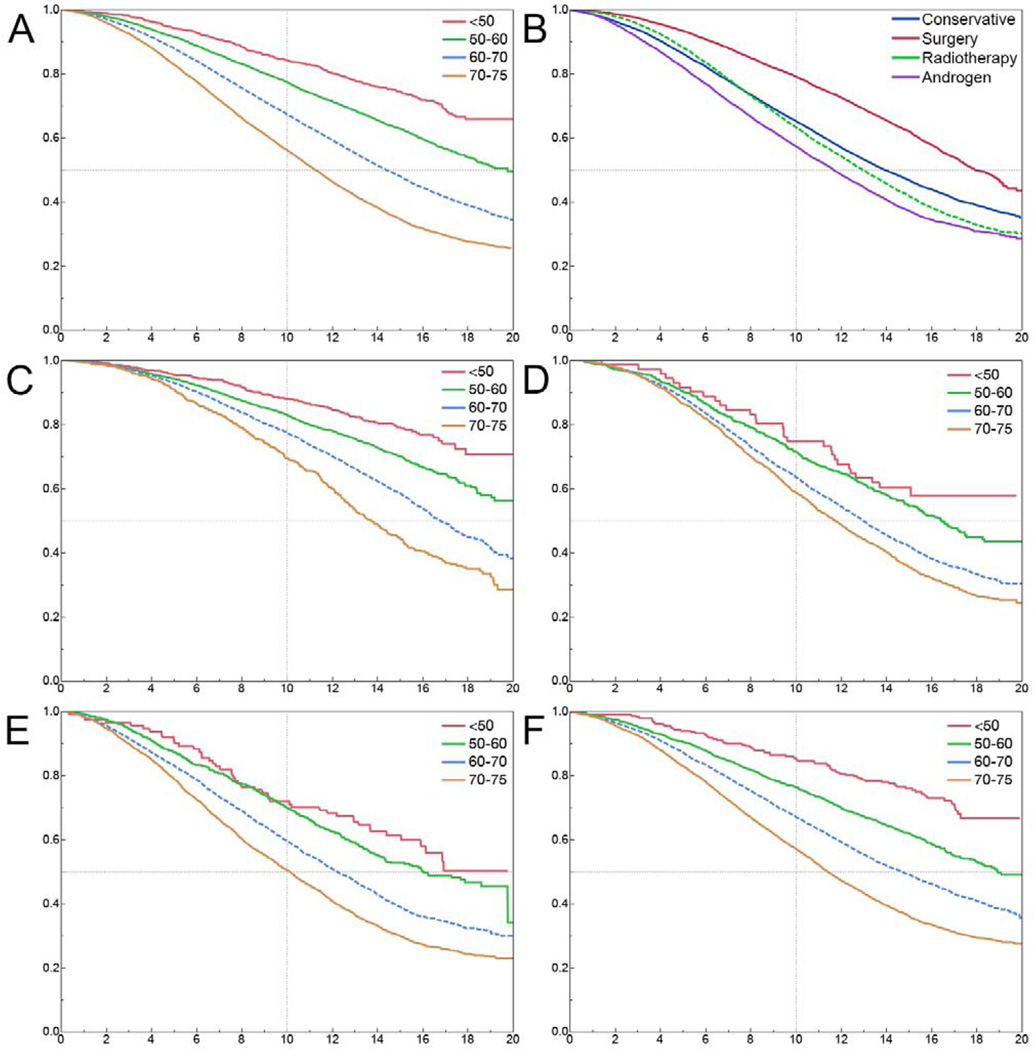
Median survival of the cohort was 14 yr (25th and 75th percentiles, range: 7.9–20 yr) and was similar for patients with clinical stage T1 and T2 cancers. Survival stratified by treatment type and age at diagnosis is shown in Figure 2.
Fig. 2.
The overall survival of patients with clinically localized prostate cancer in the US Veterans Health Administration stratified by patient age. (a) Survival decreased with increasing patient age. (b) Patients treated with surgery had the best survival. (c) Despite the selection of younger— and likely healthier—patients for surgery, 21% of patients had died after 10 yr of follow-up. (d) Median survival for patients treated with radiotherapy was 12.9 yr, whereas 36.7% of patients had died after 10 yr. (e) Median survival for patients treated with androgen deprivation therapy was 11.7 yr, whereas 57.3% of patients had died after 10 yr. (f) Median survival for patients receiving conservative management was 13.9 yr, whereas 34.8% of patients had died after 10 yr.
The low survival of patients with clinically localized PCa in this national VHA cohort is consistent with previous reports. Daskivich et al reported 70% non-PCa mortality at 10 yr among men with a Charlson comorbidity score ≥3 who were diagnosed with low-risk PCa at two VHA hospitals between 1997 and 2004 [12]. Although these data indicate poor overall survival, VHA patients with clinically localized PCa were unlikely to have died from their cancer. Lower survival rates in the VHA are also unlikely to be related to poorer quality care. Studies have demonstrated that the VHA often outperforms community medical systems on standard quality measures [15]. Moreover, patients diagnosed with cancer in the VHA are more likely to be diagnosed at an earlier stage and to have equal or better cancer-specific survival rates than age-matched Medicare beneficiaries [16,17]. Together, these findings suggest that the relatively low survival within the VHA reflects more substantial comorbid physical and mental illness. Our findings raise concerns about the validity of PIVOT. In this analysis, we draw attention to the poorer survival outcomes among PIVOT participants compared with a national cohort of patients with clinically localized PCa in the VHA. The lack of survival benefit among PIVOT participants might not be generalizable to all VHA patients in light of the lower mortality rates that we observed in the general VHA population with localized PCa.
Our findings also suggest that PIVOT findings also might not be generalizable to community-based practices. Several non-VHA registries show much lower all-cause mortality rates than those reported by PIVOT. Among 45 440 men with clinically localized PCa diagnosed in California from 1995 to 1998, 10-yr survival was 66% [18]. Data from the Prostate Cancer Outcomes Study examined mortality outcomes following surgery or radiation for men aged 55–74 yr with localized PCa. Among this cohort, only 34% of patients had died after 15 yr of follow-up [19]. Furthermore, PIVOT survival outcomes are inferior to published randomized studies comparing watchful waiting with radical prostatectomy. The Scandinavian Prostate Cancer Group Study 4 (SPCG-4) randomized 695 patients with a mean age of 65 yr and localized PCa to either radical prostatectomy or watchful waiting between 1989 and 1999. After 23.2 yr of follow-up, 36% of study participants were still alive [20]. More refined tools to estimate life expectancy of patients with localized PCa in the VHA and community settings are needed to inform clinical decision making in the face of varying burdens of competing risks.
Acknowledgments
Funding/Support and role of the sponsor: This work was supported by the US National Institutes of Health (grants DK089086 to J.T.L., CA152737 to J.D.B., and DK085446 to G.M.C.)..
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author contributions: John T. Leppert had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Barbosa, Thomas, Srinivas, Buyyounouski, Chung, Chertow, Asch, Wagner, Brooks, Leppert.
Acquisition of data: Barbosa, Thomas, Leppert.
Analysis and interpretation of data: Barbosa, Thomas, Srinivas, Buyyounouski, Chung, Chertow, Asch, Wagner, Brooks, Leppert.
Drafting of the manuscript: Barbosa, Thomas, Srinivas, Buyyounouski, Chung, Chertow, Asch, Wagner, Brooks, Leppert.
Critical revision of the manuscript for important intellectual content: Barbosa, Thomas, Srinivas, Buyyounouski, Chung, Chertow, Asch, Wagner, Brooks, Leppert.
Statistical analysis: Barbosa, Thomas, Srinivas, Buyyounouski, Chung, Chertow, Asch, Wagner, Brooks, Leppert.
Obtaining funding: None.
Administrative, technical, or material support: None.
Supervision: None.
Other (specify): None.
Financial disclosures: John T. Leppert certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/ affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
References
- 1.Brooks JD. Managing localized prostate cancer in the era of prostate-specific antigen screening. Cancer. 2013;119:3906–3909. doi: 10.1002/cncr.28301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Welch HG, Black WC. Overdiagnosis in cancer. J Nat Cancer Inst. 2010;102:605–613. doi: 10.1093/jnci/djq099. [DOI] [PubMed] [Google Scholar]
- 3.Wilt TJ, Brawer MK, Jones KM, et al. Radical prostatectomy versus observation for localized prostate cancer. N Engl J Med. 2012;367:203–213. doi: 10.1056/NEJMoa1113162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.NCCN clinical practice guidelines in oncology (NCCN Guidelines): prostate cancer, V.1.2011. National Comprehensive Cancer Network Web site. doi: 10.6004/jnccn.2010.0012. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#site. [DOI] [PubMed]
- 5.National Center for Veterans Analysis and Statistics. [Updated December 30, 2015];US Department of Veterans Affairs Web site. http://www.va.gov/vetdata/
- 6.Zullig LL, Jackson GL, Dorn RA, et al. Cancer incidence among patients of the U.S. Veterans Affairs Health Care System. Mil Med. 2012;177:693–701. doi: 10.7205/milmed-d-11-00434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Selim AJ, Berlowitz DR, Fincke G, et al. The health status of elderly veteran enrollees in the Veterans Health Administration. J Am Geriatr Soc. 2004;52:1271–1276. doi: 10.1111/j.1532-5415.2004.52355.x. [DOI] [PubMed] [Google Scholar]
- 8.Rogers WH, Kazis LE, Miller DR, et al. Comparing the health status of VA and non-VA ambulatory patients: the veterans’ health and medical outcomes studies. J Ambul Care Manage. 2004;27:249–262. doi: 10.1097/00004479-200407000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Kazis LE, Miller DR, Skinner KM, et al. Patient-reported measures of health: the Veterans Health Study. J Ambul Care Manage. 2004;27:70–83. doi: 10.1097/00004479-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160:3252–3257. doi: 10.1001/archinte.160.21.3252. [DOI] [PubMed] [Google Scholar]
- 11.Cooperberg M, Lubeck DP, Penson D, Mehta SS, Carroll PR, Kane CJ. Sociodemographic and clinical risk characteristics of patients with prostate cancer within the Veterans Affairs health care system: data from CaPSURE. J Urol. 2003;170:905–908. doi: 10.1097/01.ju.0000081200.63275.0b. [DOI] [PubMed] [Google Scholar]
- 12.Daskivich TJ, Chamie K, Kwan L, et al. Overtreatment of men with low-risk prostate cancer and significant comorbidity. Cancer. 2011;117:2058–2066. doi: 10.1002/cncr.25751. [DOI] [PubMed] [Google Scholar]
- 13.Daskivich TJ, Chamie K, Kwan L, Dash A, Greenfield S, Litwin MS. Matching tumor risk with aggressiveness of treatment in men with multiple comorbidities and early-stage prostate cancer. Cancer. 2013;119:3446–3453. doi: 10.1002/cncr.28226. [DOI] [PubMed] [Google Scholar]
- 14.Lorenz KA, Asch SM, Yano EM, Wang M, Rubenstein LV. Comparing strategies for United States veterans’ mortality ascertainment. Popul Health Metr. 2005;3:2. doi: 10.1186/1478-7954-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asch SM, McGlynn EA, Hogan MM, et al. Comparison of quality of care for patients in the Veterans Health Administration and patients in a national sample. Ann Intern Med. 2004;141:938–945. doi: 10.7326/0003-4819-141-12-200412210-00010. [DOI] [PubMed] [Google Scholar]
- 16.Landrum MB, Keating NL, Lamont EB, et al. Survival of older patients with cancer in the Veterans Health Administration versus fee-for-service Medicare. J Clin Oncol. 2012;30:1072–1079. doi: 10.1200/JCO.2011.35.6758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Program Evaluation of Oncology Programs in Veterans Health Adminsitration: Report on Prostate Cancer. Washington, DC: US Departmet of Veterans Affairs Office of Policy and Planning; 2009. [Google Scholar]
- 18.Sieh W, Lichtensztajn DY, Nelson DO, et al. Treatment and mortality in men with localized prostate cancer: a population-based study in California. Open Prost Cancer J. 2013;6:1–9. [PMC free article] [PubMed] [Google Scholar]
- 19.Hoffman RM, Koyama T, Fan KH, et al. Mortality after radical prostatectomy or external beam radiotherapy for localized prostate cancer. J Nat Cancer Inst. 2013;105:711–718. doi: 10.1093/jnci/djt059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bill-Axelson A, Holmberg L, Garmo H, et al. Radical prostatectomy or watchful waiting in early prostate cancer. N Engl J Med. 2014;370:932–942. doi: 10.1056/NEJMoa1311593. [DOI] [PMC free article] [PubMed] [Google Scholar]