Abstract
Background
Addressing violence along with drug use change goals is critical for women with coexisting intimate partner violence (IPV) and substance use disorders (SUD).
Methods
This was an acceptability and feasibility study of BSAFER, a brief Web-based program and booster phone call addressing violence and drug use. A screening survey identified women with recent drug use and IPV in the emergency department (ED). Participants were randomized to BSAFER or a Web-based control program and booster call providing education about home fire safety. Program completion, usability, satisfaction and MI adherence were primary outcomes. Drug use and IPV outcomes were measured at baseline, one and three months.
Results
Forty women were enrolled (21 BSAFER, 19 control); 50% were non-white and mean age was 30 years. Most commonly used drugs were marijuana (88%) and cocaine (30%); 45% reported physical abuse and 33% severe combined physical and sexual abuse. Thirty-nine (98%) completed the Web program, 30 (75%) completed the booster, and 29 (73%) completed 3-month follow up. Mean System Usability Scale (SUS) for the BSAFER Web program was 84 (95% CI 78–89) of 100; mean Client Satisfaction Questionnaire (CSQ-8) was 28 (95% CI 26–29) of 32. MI adherence scores were high and similar for both the Web program and the booster. Both intervention and control groups had small mean decreases in weekly drug use days (0.7 days vs. 1.5 days); participants using drugs other than marijuana demonstrated greater average reductions in drug use than those using marijuana only.
Conclusions
An ED Web-based intervention for SUD and IPV in women demonstrated feasibility and acceptability. Future studies will examine efficacy of the BSAFER program and investigate whether specific subgroups of drug using women may be most responsive to ED-based Web interventions.
Introduction
The link between intimate partner violence (IPV) and drug use in women has been well established. Drug use at baseline is a risk factor for the occurrence of partner violence, and the experience of violence predicts subsequent substance use.1–4 In addition, each problem serves as a potential barrier to intervening in the other. Women abused by their partners may be subject to controlling behaviors that prevent them from accessing treatment programs, may have few independent financial resources to be able to pay for treatment, and may fear retribution or escalation of violence if they try to make a positive change autonomously, particularly if substance use is an established activity in the abusive relationship. At the same time, trauma from the abuse itself may be an impetus for drug use and increased risk for substance use disorders.5 Substance use disorders may prevent women from being eligible for housing in domestic violence shelters and may impact responses of law enforcement to incidents involving assault by an intimate partner.6
The emergency department (ED) population has a high prevalence of patients with coexisting IPV and substance use,7 making the visit a unique opportunity to identify these problems and provide brief interventions and referrals to treatment. The ED visit has been described as a “teachable moment” in which behavior change may be more likely to occur, particularly if linked to a negative health consequence.8 Interventions for drug and alcohol use disorders have been conducted in the ED for more than 30 years, but rarely address common coexisting and gender-specific conditions such as partner abuse. In outpatient settings, women have been identified as having specific barriers to accessing and completing substance use treatment programs, and demonstrate improved participation, retention, and outcomes when offered gender-specific programming.9–12 Addressing violence and linking women to IPV services in parallel with drug change goals is also critical to helping women cope with past or ongoing violence, optimize safety, and, in the long term, avoid further abusive relationships.
Addressing these kinds of complex and chronic problems in an integrated manner within the constraints of a single healthcare visit may seem implausible, particularly in the emergency department. Barriers to brief interventions in this setting include the high acuity of conditions seen, high volume of patients, provider workload, lack of physical space to ensure privacy, lack of provider training in counseling skills, low provider confidence for addressing IPV or substance use, and limited resources and staffing to support such a program.13 However, many of these barriers can be overcome with the use of technology.14–18
Computer or Web-based programs provide a sense of anonymity and privacy, which may actually increase reporting of unhealthy behaviors and IPV.15,19,20 They require little direct clinician involvement. They can be adapted to be culturally and linguistically specific and audio capabilities allow interventions to engage low-literacy individuals. They can deliver assessments and, based on the results, provide immediate, individualized feedback and recommendations for change. They minimize the bias that can arise in interpersonal relationships between the provider and patient. An effective intervention can be widely disseminated while maintaining treatment fidelity across diverse clinical sites. Adult women have reported high comfort seeking health information online.17 The majority of ED patients use computers, access the Internet, and feel comfortable receiving technology-based health information.21
Technology, therefore, may provide an alternate means of delivery of screening and brief interventions for women with IPV and substance use disorders. Our preliminary work demonstrated that women in the ED who use drugs and report IPV victimization would be receptive to technology-delivered screening and advice,22 and informed the development of a brief, Web-based intervention by providing insight into the content, format, and language desirable to the target population.23 Testing feasibility and acceptability of this innovative intervention was an important step prior to efficacy testing in a large trial.
The purpose of this study was to examine the feasibility and acceptability of a computer-based program and telephone booster for drug-using women reporting IPV, called “B-SAFER” (Brief Intervention for Substance Use and Partner Abuse for Females in the Emergency Room), randomizing participants recruited from the ED to intervention and control groups. We also secondarily examined drug use and IPV outcomes as a preliminary evaluation of potential responses to treatment to provide estimates of effect size for future larger-scaled trials of the intervention.
Methods
Setting and Population
Participants were recruited from the adult ED of a level I trauma center with more than 100,000 annual adult visits by an ethnically and racially diverse patient population. Recruitment took place 15 hours a day (8 am – 11 pm, seven days a week). Research assistants (RAs) used a random number generator to select a random sample of rooms. Within this subset of patients, screening took place in two steps. First, RAs reviewed the electronic medical record and identified those determined to be English-speaking adult women aged 18 to 59; those failing to meet these criteria were excluded. Second, RAs invited the remaining, potentially eligible patients to complete a “Women’s Health Survey,” self-administered on an iPad (Apple, Inc.). Those who completed the screen and reported both drug use and IPV in the past three months were eligible for the study. We excluded those who were critically ill (triaged to the critical care area of the ED), had suicidal ideation or psychosis, were combative or in police custody, or were treated in a supervised setting for alcohol or drug dependence. Eligible patients who provided informed consent were enrolled in the study and were asked to provide demographic information and baseline assessments. Participants were then given headphones, a tablet computer, and a brief tutorial from the RA on navigating through the program. Participants launched the program themselves, completed more detailed assessments of drug use and IPV, and then were automatically randomized to intervention or control groups by the software. RAs provided privacy by stepping outside the room; however, they informed participants that they would be just outside the door in case there were any problems with or questions about navigating the program. Data collection forms included a section for RAs to make notes about any obstacles participants encountered in the course of completing the program.
At the conclusion of the program, all participants were given a brochure with general health resources, including contact information for domestic violence agencies and substance use treatment services as well as primary care centers and women’s health-specific resources. We also asked participants to provide three locators, or individuals who might be able to help us find the participants if we were not able to reach them through their primary phone number. Participants were given CVS gift cards for participation at baseline ($25), at the booster ($20), and at each of the two follow up assessments ($25/each), for a potential total of $95. The Institutional Review Board (IRB) of the participating hospital approved all study procedures.
Intervention Condition
BSAFER is a brief Web-based program, designed to be taken on a small tablet-style laptop computer and to be completed in the room during a single ED visit. An overview of the structure and content of the intervention is provided in Table 1. BSAFER was created using intervention design software, Computerized Intervention Authoring Software (CIAS, Interva, Inc).24 The program uses a female parrot avatar (“Polly”), who addresses the participant by name, serves as a guide and narrator for the program, and reads all content aloud, allowing low-literacy participants to complete the program. Participants wore headphones to maintain privacy; all visitors were required to leave the room from initial screening through the duration of the program to ensure safety and confidentiality. The program was administered via a tablet computer and could be stopped and restarted as needed for interruptions related to clinical care, such as for nursing or physician care or imaging or other testing. The study protocol included the option for participants who were discharged before completing the program to be offered a chance to finish it in a private research office in the ED.
Table 1.
BSAFER Intervention Overview
| Component | Content |
|---|---|
|
Automated Feedback |
Using the answers provided in the baseline assessments, the Web-based program provides feedback on drugs used, known health consequences of drug use, and estimated annual cost of their drug use. |
|
Identification of Core Values |
Women are asked to reflect on the things that “matter most to them” and then select a single “core value” from a menu of options (e.g., Children, God/Spirituality, Wealth/Prosperity, Physical Health) |
| Empowerment | A series of empowerment videos are offered throughout the program, depicting real women who tell stories of how drug use and IPV affected their core values, how they were able to reduce drug use and IPV, and the positive outcomes of these changes. |
| Goal Setting | Participants are asked to select one goal for reducing the use of their self-identified problem drug; after doing this, the program raises the possibility that IPV or a history of IPV may make changes in drug use challenging and asks the participant to select one goal around seeking help for relationship safety. |
| Social Supports | Participants are asked to identify one person they can care share their goals with who can support them. |
| Advice | Participants receive information about alternate behaviors to drug use. |
| Referrals | Participants are provided IPV, substance use and primary care resources. |
| Summary | Participants receive a one-page print out of their goals, social supports, empowerment messages evoking video content, and referral resources. |
The intervention included a booster session conducted by phone within two weeks after the initial ED visit. The booster was intended to enhance the effect of the necessarily brief ED-based intervention; in our preliminary work, participants reported high satisfaction with such a booster session and reported high consistency with the key elements of motivational interviewing.25 The booster conversation consisted of: 1) Review of core values and drug use goals established at baseline; 2) Discussion of current drug use; 3) Discussion of any discrepancy between goals and motivators and current drug use; 4) Discussion of barriers to achieving goals and problem solving; 5) Reinforcement of SUD treatment services and IPV resources; 6) Reinforcement and encouragement of drug use change goals.
Control Condition
The control arm received a time-matched Web-based program on home fire safety, including videos from the National Fire Protection Association. This topic was selected as it seemed likely to be viewed as acceptable and appropriate content to receive in a healthcare setting, yet unlikely to have an effect on study outcomes. The control program was designed using the same software as for the intervention; however, the parrot was not used, as it relayed empathy and compassion, which we thought might be too “active” of an ingredient. The control did mimic the content structurally, including the interactive question-answer components and ratio of spoken content to videos. The control group also received a telephone booster; however, this conversation consisted of a reminder and brief discussion of the topics covered in the home fire safety Web program and resources for those wishing more information on home fire safety.
Measures
Immediately following the intervention, participants were asked to complete a brief post survey that included the 8-item Client Satisfaction Questionnaire [CSQ-8],26 which asks participants about their satisfaction with the program and the extent to which it met their needs and helped them with their problems, and the 10-item Systems Usability Scale [SUS],27 which asks participants about their experience with the technical aspects of the program, including the need for support or training and general complexity. The post survey also included questions developed for an earlier ED-based study for patients with injury and risky alcohol use28 that assessed how well the program was consistent with MI principles and processes, including providing feedback, empathy, collaboration, and a sense of regard and respect; helping the participant develop discrepancy and change goals; emphasizing personal values; evoking feelings and emotions; guiding the participant to a “eureka” moment; and rolling with resistance.
The primary clinical outcome measure was past month drug use, measured by a modified version of the Timeline Followback (TLFB).29 For ease of administration and brevity, participants were asked to report drug use over a representative week that reflected “usual” use over the past month, rather than to complete the full 30-day TLFB. Secondary outcomes included readiness and confidence for changing drug use and the Composite Abuse Scale (CAS),30 a 30-question measure for the occurrence of psychological, physical and sexual violence. CAS consists of a list of specific behaviors and relationship dynamics that may be associated with IPV, such as stalking, victim-blaming, isolation from friends and family, and specific acts of physical violence. Respondents are asked to report how often these behaviors have occurred in their most recent intimate relationship. Participants completed these measures at baseline, one-month and three-month follow up, with the exception of readiness and confidence rulers, which were administered immediately pre- and post-intervention and after the two-week telephone booster.
Data Analysis
For this pilot study, we evaluated primary and secondary outcomes using descriptive summaries (median, mean, proportions) and associated confidence intervals. The main study objective was the feasibility and acceptability of the BSAFER intervention using evaluation of program completion and participant feedback. No formal significance testing of differences between BSAFER and control on drug use outcomes was conducted, as the study was not powered for such an analysis. However, as a preliminary examination of the change we might expect to see in a larger clinical trial, we did examine estimates of changes in drug use and IPV occurrence, both for all participants and in the subset of participants reporting use of drugs other than marijuana, given evidence for stronger motivation to change illicit drug use in this population.31,32
Results
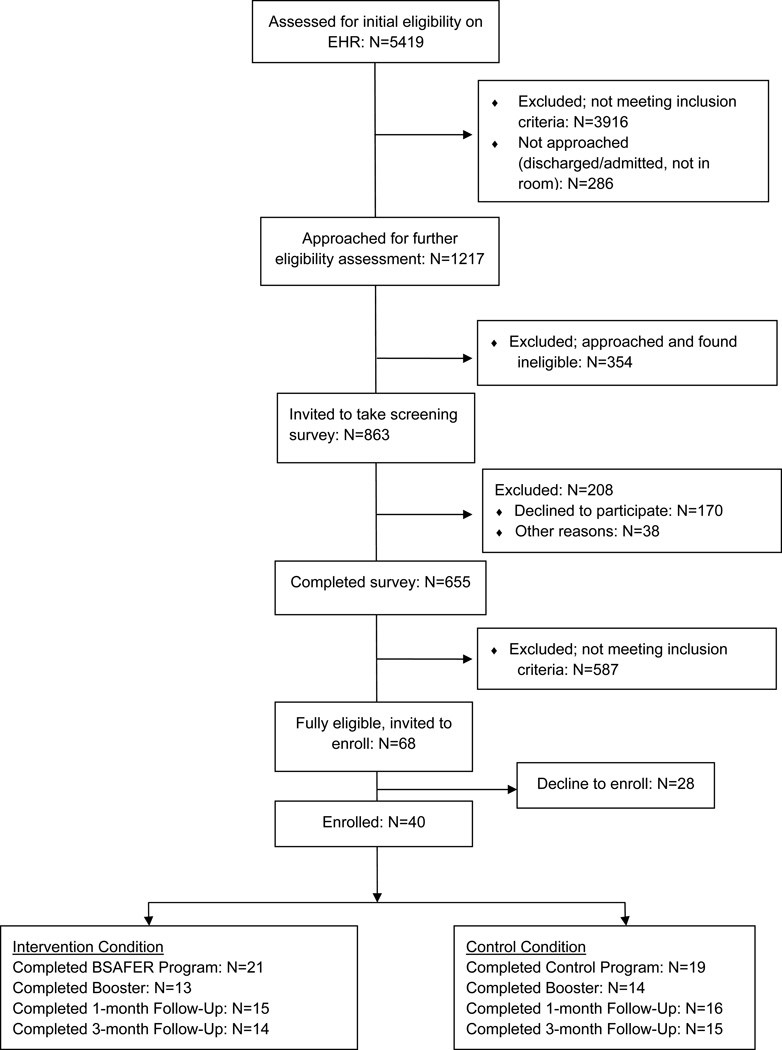
Forty women were recruited into the study; 21 were randomized to the intervention arm and 19 to the control arm (see Figure 1). See Table 2 for demographic and other baseline characteristics of the study participants. The most common drugs used were marijuana (88%) and cocaine (30%); 45% of participants reported intimate partner physical abuse and 33% severe combined intimate partner physical and sexual abuse.
Figure 1.
CONSORT Diagram
Table 2.
BSAFER Participant Baseline Characteristics (N=40)
| Control (n=19)* | Intervention (n=21)* | |
|---|---|---|
| Age (median, range) | 24.5 (19–53) | 26 (19–48) |
| Race (% nonwhite) | 47.4 (22.6–72.1) | 52.4 (29.1–75.7) |
| Ethnicity (% Hispanic/Latino) | 36.8 (13.0–60.7) | 20.0 (0.7–39.2) |
| Education (% high school or more) |
23.1 (17.7–66.6) | 50.0 (26.0–74.0) |
| Marital Status (% single never married) |
63.2 (39.3–87.0) | 65.0 (42.1–87.9) |
| Children (% with at least one child) |
47.4 (22.5–72.1) | 60.0 (36.5–83.5) |
| Past-week drug use (median, range) |
5 (0, 7) | 6 (0, 7) |
| CAS scores (median, range) | 8 (0, 41) | 8 (0, 44) |
| ASSIST scores, baseline (mean, across drugs) |
11.7 (8.1–15.4) | 8.1 (5.9–10.3) |
| Readiness to change drug use (mean, 5-point scale) |
1.6 (0.9 – 2.4) | 2.7 (1.9–3.4) |
| Confidence to change drug use (mean, 5-point scale) |
2.5 (1.7–3.3) | 3.0 (2.3–3.6) |
Percentage with 95% CI, unless otherwise indicated
Feasibility
Twenty (95%) completed all portions of the BSAFER Web program and 19 (100%) completed all portions of the control Web program. The option to complete the program in the research office after discharge was not used by any of the participants. The average time for completion of the active components of the BSAFER Web program (excluding assessments) was 15 minutes (18 minutes for the control). Thirty participants (75%) completed the two-week telephone booster; the average time to complete the BSAFER booster was 20 minutes (9 minutes for the control). Thirty-one (78%) completed the one-month follow up and 29 (73%) completed the three-month follow up.
Acceptability
In the intervention group, mean overall usability score (SUS) for the BSAFER Web program was 83.5 (95% CI 78.1–88.9) out of a possible 100. The mean overall satisfaction score (CSQ-8) was 27.7 (95% CI 26.3–29.1) out of a possible 32. Intervention arm participants’ agreement with statements about the consistency of the BSAFER Web-based program and the telephone booster with specific principles or qualities of MI are demonstrated in Tables 3 and 4, respectively. Overall, participants in both arms scored both the BSAFER program and the booster high for all aspects of consistency with MI, with the intervention scoring higher on several individual components.
Table 3.
Consistency of Web-based Program with Motivational Interviewing Principles*
| MI Scale Statements | Control (% answering “agree” or “strongly agree”) |
Intervention (% answering “agree” or “strongly agree”) |
p value (chi square) |
|---|---|---|---|
| “I felt understood” | 68% (45–91%) | 95% (85–100%) | 0.03** |
| “We worked well together” |
95% (84–100%) | 95% (85–100%) | 0.97 |
| “…encouraged me to express my thoughts and feelings” |
89% (74–100%) | 80% (61–99%) | 0.41 |
| “I felt like my thoughts and feelings were paid attention to” |
84% (66–100%) | 90% (76–100%) | 0.59 |
| “I felt respected” | 95% (84–100%) | 100% | 0.30 |
| “Helped me realize the difference between what my life is like now and what I would like my life to be like.” |
63% (39–97%) | 75% (54–96%) | 0.42 |
| “I feel more able to change” |
42% (18–67%) | 80% (61–99%) | 0.02** |
| “I felt judged or looked down upon” |
11% (0–26%) | 0% | 0.14 |
| “Helped me to think of ways to change” |
89% (74–100%) | 100% | 0.14 |
| “I have developed some new understanding about how my choices affect my life” |
79% (59–99%) | 95% (85–100%) | 0.13 |
| “Hearing about the possible consequences of my choices helped me consider changing” |
74% (52–95%) | 80% (61–99%) | 0.64 |
| “Conversation about what is important to me gave me a reason to change my drug use” |
53% (28–77%) | 80% (61–99%) | 0.07 |
On 5-point Likert scale, 1=”Strongly disagree”; 5 = “Strongly agree”
Statistically significant
Table 4.
Consistency of Telephone Booster with Motivational Interviewing Principles*
| MI Scale Statements | Control (% answering “agree” or “strongly agree”) |
Intervention (% answering “agree” or “strongly agree”) |
p value (chi square) |
|---|---|---|---|
| “I felt understood” | 85% (65–100%) | 100% | 0.17 |
| “We worked well together” | 100% | 100% | -- |
| “…encouraged me to express my thoughts and feelings” |
71% (44–98%) | 100% | 0.04** |
| “I felt like my thoughts and feelings were paid attention to” |
93% (77–100%) | 100% | 0.35 |
| “I felt respected” | 100% | 100% | -- |
| “Helped me realize the difference between what my life is like now and what I would like my life to be like.” |
71% (44–98%) | 83% (59–100%) | 0.47 |
| “I feel more able to change” | 57% (27–87%) | 92% (73–100%) | 0.05** |
| “I felt judged or looked down upon” |
7% (0–23%) | 17% (0–41%) | 0.45 |
| “Helped me to think of ways to change” |
64% (36–93%) | 83% (59–100%) | 0.28 |
| “I have developed some new understanding about how my choices affect my life” |
79% (54–100%) | 83% (59–100%) | 0.76 |
| “Hearing about the possible consequences of my choices helped me consider changing” |
71% (44–98%) | 75% (46–100%) | 0.84 |
| “Conversation about what is important to me gave me a reason to change my drug use” |
43% (13–73%) | 83% (59–100%) | 0.03** |
On 5-point Likert scale, 1=”Strongly disagree”; 5 = “Strongly agree”
Clinical Outcomes
Readiness for drug use change increased from baseline to the two-week booster by a mean of 1.4 points in the intervention group (on a 5-point scale), compared to a mean increase of 0.5 in the control group. Confidence for drug use change increased from baseline to the two-week booster by a mean of 0.6 points in the intervention group (on a 5-point scale) compared to a mean increase of 0.4 in the control group.
Overall, estimates of drug use and IPV occurrence demonstrated potential modest improvements in three-month outcomes in both groups. The intervention group had a mean decrease in drug use of 0.7 days per week (median decrease of 0.5 days) compared to a mean decrease in drug use of 1.5 days per week (median decrease of 2 days) in the control group. Among those using drugs other than marijuana, however, the intervention group demonstrated a mean decrease of 2.5 using days per week (median decrease of 4.5 days), compared to a decrease of 1.3 using days per week (median decrease of 1 day) in the control group. CAS scores decreased by a mean of 4.1 points (median decrease of 7.5) in the intervention group (on a 30-point scale) compared to a mean decrease of 3.3 points (median decrease of 8) among controls.
Discussion
We found administration of a brief, Web-based intervention for women with coexisting SUD and IPV plus telephone booster highly feasible in the emergency care setting. Most study participants were able to complete the Web program within the timeframe of their ED stay, even with the time burden of the study assessments. This was reassuring considering the nature of the ED, with its frequent interruptions and high burden of diagnostic testing and interactions with multiple types of healthcare providers. In a real world setting, using only the active program components, which took only an average of 15 minutes to complete, the intervention would be even more feasible to complete within the four to five hour span of a typical ED visit. Because the program can be paused and resumed at any point, the program time may be spread out over the course of the stay.
Acceptability was also high among study participants. High average scores for general satisfaction with the service provided validation of the usefulness and relevance of the program for our patient population; high scores for usability are consistent with the high prevalence of technology use among ED patients in general observed in other studies,21 and our preliminary work with this population,22 which suggested that facility and confidence with technology would not itself pose a barrier to screening and interventions in the ED.
One unknown of delivering brief interventions through a Web-based platform is how well MI can be replicated. Technology could, theoretically, alter the essential components of MI, many of which rely on an individual therapist’s ability to provide a tone of respect and empathy, direct participants to a plan uniquely suited to their values and motivators, and develop discrepancy by steering conversation to the gap between participants’ goals and current actions. Replicating this kind of complex and intuitive interaction via a computer interface promised to be a challenge; however, surprisingly, feedback on a wide spectrum of ideal MI features was generally positive.
Consistency in terms of the MI “spirit” of the program was likely aided by several program components. First, the speaking parrot avatar was a human-like presence throughout the program; in an earlier study using the same software, pregnant women at risk for alcohol use responded favorably to a similar avatar and many felt it preferable to talking to a human, potentially replacing some of the role of a therapist.33 Second, the videos used throughout the BSAFER program incorporated a virtual connection to women with similar experiences and may also have enhanced the sense of empathy and respect. Third, the telephone booster promised the opportunity for a human interaction for a truly personalized connection and a chance to discuss individual problems and solutions, although the fact that the Web program itself received high scores for MI consistency supports the fact that even the in-ED program alone was able to offer many of the essential ingredients of an MI-based intervention. Finally, it may be that the privacy and confidentiality of the computer interface provided women with the freedom to communicate about these topics and engage in reflection around their drug use. It is important to acknowledge, however, that the MI consistency or “spirit” of the intervention does not necessarily represent the full value of having a face-to-face interaction: Walton et al.34 found that a computer-assisted therapist was more effective in reducing risky behaviors in a cohort of adolescents involved in peer violence and alcohol use than a self-administered computer alone, even though the program included many of the components mentioned above, including a life-like avatar.
One expected study finding was the positive response to the home fire safety control condition; the high scores in the acceptability measures – even for questions specifically related to drug use, which was not addressed in the home fire safety content – indicated that the control may not have been as inactive as we intended. It may be that women experiencing abuse, who are powerless in other areas of their lives, found that the fire safety content suggested simple, positive actions they could take to improve their home lives. Or, women may have been responding to the concern they perceived from receiving any positive health related information above and below routine clinical care. Finally, these scores may reflect assessment reactivity,35,36 the tendency of control arm participants to change behaviors in response to survey instruments, likely due to increased self-awareness of the behavior and its negative consequences. As the study assessments were delivered within the same software as the control program, they may have been perceived as part of the program itself.
The ability of technology to occur in parallel with clinical care and to circumvent the need to train the emergency workforce directly makes it highly appealing as a means to address public health problems such as substance use. Indeed, the difficulty in delivering brief interventions skillfully and consistently may be a factor in the modest effect sizes of therapist- or clinician-delivered ED-based alcohol and drug SBIRT interventions demonstrated to date. Multiple Web- or computer-based programs have been created and shown to be feasible for providing brief interventions for substance use, mental health problems and injury in the emergency care setting.37 Few of these programs, however, have used technology to simultaneously address multiple, co-occurring problems in an integrated fashion. While doing so may seem ambitious for a single point of contact, practically speaking, issues such as mental health, substance use, violence, unintentional injuries, and sexual risk tend to co-exist and affect the ability of clinicians to intervene effectively in any one issue in isolation. Simply replicating brief interventions that were designed for human, face-to-face delivery, may not be taking advantage of the functionality of the available programs, which may allow for patients to explore in-depth the single or multiple issues they are ready to change at the time of the visit.
Whether to address marijuana along with other illicit drugs is increasingly becoming a dilemma for those involved in substance use care and research, as individual states have legalized marijuana for medical use, decriminalized marijuana possession and/or cultivation, or fully legalized its recreational use. Therefore, marijuana use is increasingly normalized; in this study, many patients who used marijuana described therapeutic uses of the drug and seemed unenthusiastic about engaging in discussions around changing drug use.32 Although recent SBIRT drug studies38,39 have had broad inclusion criteria with regards to types of substance use, our subgroup analysis hinted that the population of ED patients whose only drug use was marijuana may not be a target receptive to change. Future studies powered to examine the differences between subgroups of individuals using drugs will be needed to inform us more about the specific populations most likely to benefit from ED-based interventions.
Limitations
As a trial for feasibility and acceptability, this was, by design, a small sample at a single clinical setting; further, out of convenience, it only enrolled English-speaking patients. Future work studying this intervention will need to be powered to detect a clinical difference in relevant clinical outcomes and to occur in a broader range of patients and settings for greater generalizability. The length of the program, even though relatively brief, may limit the feasibility intervention in some EDs or for some patients, particularly those with shorter visit times. Other challenges to adoption may include cost of equipment and need for a robust Internet connection; the need for the hardware and software to be updated periodically; and the need for staff to be trained on introducing the program to patients. Further, even with the program’s content, increased identification of problems like IPV and substance use may create more of a need for clinicians to address these issues. Future work will be needed not only to address efficacy but to estimate the incremental cost of incorporating this type of program into emergency care.
The study findings may also be limited by selection bias. Forty-one percent of patients who were fully eligible for the study declined to participate; if patients less comfortable with technology or less receptive to technology-based behavioral interventions were the ones who chose not to participate, this might bias results towards positive responses regarding acceptability. As mentioned above, this study included all types of drug misuse. The advantage of this approach is broad applicability to the ED population with substance use disorders; the disadvantage, as alluded to above, is the lack of information about how specific groups of drug users might respond differently to the BSAFER intervention. Future work on subsets of populations engaged in drug use may identity those most likely to benefit from technology-based interventions or information further development work to address group-specific needs.
Finally, although our screening and participation rates were reasonable, only a small number of ED patients screened were fully eligible for this intervention, which targeted a specific subset of the population and required participants to be female, with both recent drug use and IPV victimization. Ultimately this type of intervention may best have a public health impact as a component of a broader intervention that can be tailored to multiple combinations of risk factors, including drug or alcohol use alone, IPV alone, or a combination of these high risk health behaviors.
Conclusions
The BSAFER intervention to address drug use and IPV among female patients was feasible for administration in the emergency care setting. Participants assigned to the BSAFER intervention reported high satisfaction with the program and rated the program favorably in terms of technical usability. Most BSAFER participants agreed that the program adhered to motivational interviewing principles. Future research is needed to examine the efficacy of the intervention for the targeted population. Participants reporting drug use other than marijuana may experience a greater overall reduction in drug use after completing the program than participants who used marijuana alone; additional work will be needed to determine if this finding is indeed true, and if such interventions may be more effective if focused on this subgroup.
Table 5.
Drug Use and IPV Outcomes
| Baseline | 1 Month | 3 Month | Mean/Median Change from Baseline to 3 Month Absolute (%) |
|||||
|---|---|---|---|---|---|---|---|---|
| Control vs. Intervention | C | I | C | I | C | I | C | I |
| Weekly Drug Use Episodes Mean (95% CI)1 Median (range) |
4.8 (3.8, 5.9) 5 (0,7) |
5.0 (4.0, 6.1) 6 (0,7) |
4.5 (3.2, 5.8) 5 (0,7) |
5.1 (4.1, 6.1) 5 (2,7) |
3.4 (1.9, 4.9) 3 (0,7) |
4.4 (2.8, 6.1) 5.5 (0,7) |
−1.5 (−26%) −2 (−40%) |
−0.7 (−26%) −0.5 (−8%) |
| Weekly Drug Use Episodes (mean)1 for Participants with Drug Use Other than Only Marijuana2 (n=18) Mean (95% CI) Median (range) |
5.8 (4.9, 6.9) 6.5 (3,7) |
5.7 (3.6, 7.7) 7 (2,7) |
5.0 (3.2, 6.8) 5 (0,7) |
4.8 (2.8, 6.9) 4.5 (2,7) |
4.5 (2.1, 6.9) 5.5 (0,7) |
3.2 (0, 6.5) 2.5 (0,7) |
−1.3 (−20%) −1 (−15%) |
−2.5 (−54%) −4.5 (−64%) |
| Past Month CAS Mean(95% CI)3 Median (range) |
9.5 (3.1, 16.9) 8 (0, 41) |
9.7 (4.7, 15.0) 8 (0, 44) |
6.2 (0.3, 12.0) 0.5 (0, 31) |
4.3 (0.8, 7.7) 2 (0, 19) |
6.2 (0, 12.8) 0 (0, 40) |
5.6 (0, 8.7) 0.5 (0, 34) |
−3.3 (−40%) −8 (−100%) |
−4.1 (37%) −7.5 (−94%) |
Using a 1-week Timeline Followback representing a “typical week over the past month”
I.e., polysubstance use or single non-marijuana drug use
Out of 150 points total; >7 has a sensitivity of 95% and a specificity of 100% for abuse
Acknowledgments
The authors wish to acknowledge the contributions of Susie Ahn, Madeline Benz, Emily Chang, Lauren Colwell, Marie DeLuca, Jessica Faraj, Kimberly Glerum, Emily Gudbranson, Andrea Haynes, Alexander Krotow, Sumitha Raman, Hyun Ju Ryoo, and Sarah Stern.
Funding: This work was supported by NIH/NIDA grant K23DA031881. NIDA provided support for conducting the study but did not play any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Author Contributions:
Esther K. Choo, MD MPH was responsible for research conception and design, collection of data, data analysis, interpretation of the results, and drafting and finalizing the manuscript.
Caron Zlotnick, PhD participated in conceiving and designing the research study, planning the data analysis, interpreting the results, and editing the manuscript.
David R. Strong, PhD participated in designing the research study, planning the data analysis, interpreting the results, and editing the manuscript.
Daniel D. Squires, PhD MPH participated in designing the research study, planning the data analysis, interpreting the results of the data analysis, and editing the manuscript.
Chantal Tapé participated in study planning, data collection and editing the manuscript.
Michael J. Mello, MD MPH participated in conceiving and designing the research study, planning the data analysis, interpreting the results, and editing the manuscript.
References
- 1.Testa M, Livingston JA, Leonard KE. Women’s substance use and experiences of intimate partner violence: a longitudinal investigation among a community sample. Addict Behav. 2003;28(9):1649–1664. doi: 10.1016/j.addbeh.2003.08.040. [DOI] [PubMed] [Google Scholar]
- 2.Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, Best CL. A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. J Consult Clin Psychol. 1997;65(5):834–847. doi: 10.1037//0022-006x.65.5.834. [DOI] [PubMed] [Google Scholar]
- 3.Golinelli D, Longshore D, Wenzel SL. Substance use and intimate partner violence: clarifying the relevance of women’s use and partners' use. J Behav Health Serv Res. 2009;36(2):199–211. doi: 10.1007/s11414-008-9114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gilbert L, El-Bassel N, Chang M, Wu E, Roy L. Substance use and partner violence among urban women seeking emergency care. Psychol Addict Behav. 2012;26:226–235. doi: 10.1037/a0025869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Najavits LM, Sonn J, Walsh M, Weiss RD. Domestic violence in women with PTSD and substance abuse. Addict Behav. 2004;29(4):707–715. doi: 10.1016/j.addbeh.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Stewart A, Maddren K. Police officers’ judgements of blame in family violence: The impact of gender and alcohol. Sex Roles. 1997;37(11–12):921–933. [Google Scholar]
- 7.Hankin A, Smith LS, Daugherty J, Houry D. Correlation Between Intimate Partner Violence Victimization and Risk of Substance Abuse and Depression among African-American Women in an Urban Emergency Department. West J Emerg Med. 2010;11(3):252–256. [PMC free article] [PubMed] [Google Scholar]
- 8.Bernstein SL, D’Onofrio G. The clinical impact of health behaviors on emergency department visits. Acad Emerg Med. 2009;16(11):1054–1059. doi: 10.1111/j.1553-2712.2009.00564.x. [DOI] [PubMed] [Google Scholar]
- 9.Grella CE, Scott CK, Foss MA. Gender differences in long-term drug treatment outcomes in Chicago PETS. J Subst Abuse Treat. 2005;28(Suppl 1):S3–S12. doi: 10.1016/j.jsat.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 10.Grella CE. From generic to gender-responsive treatment: changes in social policies, treatment services, and outcomes of women in substance abuse treatment. J Psychoactive Drugs. 2008;(Suppl 5):327–343. doi: 10.1080/02791072.2008.10400661. [DOI] [PubMed] [Google Scholar]
- 11.Grella CE, Scott CK, Foss MA, Dennis ML. Gender similarities and differences in the treatment, relapse, and recovery cycle. Eval Rev. 2008;32(1):113–137. doi: 10.1177/0193841X07307318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greenfield SF, Grella CE. What is “women-focused” treatment for substance use disorders? Psychiatr Serv. 2009;60(7):880–882. doi: 10.1176/appi.ps.60.7.880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McGrath ME, Bettacchi A, Duffy SJ, Peipert JF, Becker BM, St Angelo L. Violence against women: provider barriers to intervention in emergency departments. Acad Emerg Med. 1997;4(4):297–300. doi: 10.1111/j.1553-2712.1997.tb03552.x. [DOI] [PubMed] [Google Scholar]
- 14.Hester RK, Miller JH. Computer-based tools for diagnosis and treatment of alcohol problems. Alcohol Res Health. 2006;29(1):36–40. [PMC free article] [PubMed] [Google Scholar]
- 15.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280(5365):867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 16.Rhodes K, Drum M, Anliker E, Frankel R, Howes D, Levinson W. Lowering the threshold for discussions of domestic violence: a randomized controlled trial of computer screening. Arch Intern Med. 2006;166(10):1107–1114. doi: 10.1001/archinte.166.10.1107. [DOI] [PubMed] [Google Scholar]
- 17.Cohen R, Stussman B. Health Information Technology Use among Men and Women Aged 18–64: Early Release of Estimates from the National Health Interview Survey, January–June 2009. 2005 [Google Scholar]
- 18.Houry D, Kaslow NJ, Kemball RS, et al. Does screening in the emergency department hurt or help victims of intimate partner violence? Ann Emerg Med. 2008;51(4):433–442. 442.e1–442.e7. doi: 10.1016/j.annemergmed.2007.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rhodes KV, Lauderdale DS, He T, Howes DS, Levinson W. “Between me and the computer”: increased detection of intimate partner violence using a computer questionnaire. Ann Emerg Med. 2002;40(5):476–484. doi: 10.1067/mem.2002.127181. [DOI] [PubMed] [Google Scholar]
- 20.Hankin A, Haley L, Baugher A, Colbert K, Houry D. Kiosk versus In-person Screening for Alcohol and Drug Use in the Emergency Department: Patient Preferences and Disclosure. West J Emerg Med. 2015;16(2):220–228. doi: 10.5811/westjem.2015.1.24121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ranney ML, Choo EK, Wang Y, Baum A, Clark M, Mello MJ. ED Patients’ Preferences for Technology-Based Behavioral Interventions. Ann Emerg Med. 2012;60(2):218–227. doi: 10.1016/j.annemergmed.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 22.Choo EK, Ranney ML, Wetle TF, et al. Attitudes Toward Computer Interventions for Partner Abuse and Drug Use Among Women in the Emergency Department. [epub ahead of print] Addict Disord Their Treat. 2014 doi: 10.1097/ADT.0000000000000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Choo EK, Guthrie KM, Mello MJ, et al. “I need to hear from women who have ‘been there’”: Designing a woman-focused intervention for drug use and partner violence in the emergency department. Accepted for publication, in press. Partner Abuse. 2015 doi: 10.1891/1946-6560.7.2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ondersma SJ, Svikis DS, Schuster CR. Computer-based brief intervention a randomized trial with postpartum women. Am J Prev Med. 2007;32(3):231–238. doi: 10.1016/j.amepre.2006.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choo E, Zlotnick C, Strong D, Squires D, Mello M. A Pilot RCT of a Novel Web-Based Intervention for Drug Use Among Victimized Women in the ED. Abstract Presented at the Conference on Problems of Drug Dependence (CPDD); June 2015; Phoenix, AZ. [Google Scholar]
- 26.Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann. 1982;5(3):233–237. doi: 10.1016/0149-7189(82)90074-x. [DOI] [PubMed] [Google Scholar]
- 27.US Department of Health & Human Services; Usability.gov: Your guide for developing usable & useful Web sites. [Google Scholar]
- 28.Lee C, Longabaugh R, Baird J, Strezsak V, Nirenberg T, Mello M. Active ingredients in a telephone-delivered motivational intervention predict taking steps towards change. Published online ahead of print. Addict Res Ther. 2015 doi: 10.3109/16066359.2015.1025062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: psychometric properties. J Consult Clin Psychol. 2000;68(1):134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- 30.Hegarty KL, Sheehan M, Schonfeld C. A multidimensional definition of partner abuse: Development and preliminary validation of the Composite Abuse Scale. J Fam Violence. 1999;14(4):399–414. [Google Scholar]
- 31.Fernández-Artamendi S, Fernández-Hermida JR, García-Fernández G, Secades-Villa R, García-Rodríguez O. Motivation for change and barriers to treatment among young cannabis users. Eur Addict Res. 2013;19(1):29–41. doi: 10.1159/000339582. [DOI] [PubMed] [Google Scholar]
- 32.Choo EK, Morrow K, Tape C, Glerum K, Zlotnick C. Acceptability and Content of Motivational Booster Phone Calls for Drug Use and IPV Among Women Emergency Department Patients. Manuscript in preparation. [Google Scholar]
- 33.Pollick SA, Beatty JR, Sokol RJ, et al. Acceptability of a Computerized Brief Intervention for Alcohol Among Abstinent But At-Risk Pregnant Women. Subst Abus. 2015;36(1):13–20. doi: 10.1080/08897077.2013.857631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walton MA, Chermack ST, Shope JT, et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA. 2010;304(5):527–535. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.D’Onofrio G, Pantalon MV, Degutis LC, et al. Brief intervention for hazardous and harmful drinkers in the emergency department. Ann Emerg Med. 2008;51(6):742.e2–750.e2. doi: 10.1016/j.annemergmed.2007.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bernstein SL, Bijur P, Cooperman N, et al. A randomized trial of a multicomponent cessation strategy for emergency department smokers. Acad Emerg Med. 2011;18(6):575–583. doi: 10.1111/j.1553-2712.2011.01097.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Choo EK, Ranney ML, Aggarwal N, Boudreaux ED. A systematic review of emergency department technology-based behavioral health interventions. Acad Emerg Med. 2012;19(3):318–328. doi: 10.1111/j.1553-2712.2012.01299.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bogenschutz MP, Donovan DM, Mandler RN, et al. Brief intervention for patients with problematic drug use presenting in emergency departments: a randomized clinical trial. JAMA Intern Med. 2014;174(11):1736–1745. doi: 10.1001/jamainternmed.2014.4052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saitz R, Palfai TPA, Cheng DM, et al. Screening and brief intervention for drug use in primary care: the ASPIRE randomized clinical trial. JAMA. 2014;312(5):502–513. doi: 10.1001/jama.2014.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]