Abstract
Objectives
Numerous studies have reported the epidemiological and clinical features of Malta fever incidence in Iran. Review and synthesis of the related literature through meta-analysis can provide an appropriate measurement for aforementioned indices. Therefore, the present study aimed to determine the epidemiological and clinical features of people with Malta fever in Iran.
Methods
The required documents were obtained through searching national and international databases. In each study, standard deviation of the indices was calculated using binomial distribution formulas. Finally, the heterogeneity index was determined between studies using Cochran (Q) and I2 tests.
Results
Combining the results of 47 articles in the meta-analysis indicated that 57.6% (55.02–60.1%) and 42.3% (49.8–44.9%) of the patients were male and female, respectively. Most of the patients lived in rural areas; 68.4% (63.6–73.2%) compared to 31.4% (26.7–36.3%). In addition, 20.8% (17.4–24.2%) of the patients were ranchers and farmers, 16.9% (14.5–19.4%) were students, and 31.6% (27–36.2%) were housewives. Of the patients studies, 50.5% (35.6–65.2%) experienced contact with animals and 57.1% (46.4–67.9%) used unpasteurized dairy products. Fever, joint pain, and sweating were detected among 65.7% (53.7–77.8%) and 55.3% (44.4–66.2%), respectively.
Conclusion
The present study revealed that the frequency of male patients with brucellosis was considerably more than that of female patients. The number of patients with Malta fever in rural areas was significantly more than in urban areas. High-risk behavior, unprotected contact with animals, and using unpasteurized dairy products were among the most significant factors affecting Malta fever incidence in Iran. Fever, joint pain, and sweating were detected among most of the patients with Malta fever.
Keywords: epidemiology, Iran, Malta fever, meta-analysis, systematic review
1. Introduction
Brucellosis or Malta fever is a bacterial infection that spreads from animals to humans. Despite the preventive measurements adopted throughout the world; particularly in the Mediterranean and Iran; the disease is still a thread to public health 1, 2. Iran stands in the second rank regarding the prevalence of Malta fever worldwide [3]. Malta fever is caused by Brucella bacteria, particularly by Brucella melitensis, Brucella abortus, and Brucella suis species. In advanced countries, men are more affected compared with women. Children are more affected than adults. In Iran and other areas, in which brucellosis is endemic, there is no significant difference between infection among children and adolescents. Moreover, since Iranian rural women cooperate with men in farming and animal husbandry, they are also highly susceptible to the disease [4].
The clinical manifestations of people with brucellosis include long-term fever, anorexia, fatigue, or involvement of local organs such as arthritis [5]. Malta fever is transmitted to humans through direct contact with animals or through ingestion of infected dairy products. Therefore, it is considered as an occupational hazard for people involved in cattle-related jobs (e.g., veterinarians, slaughterhouse workers, ranchers, and farmers) [2]. Different factors play a significant role in brucellosis infection in humans. Direct and indirect contact including using unpasteurized dairy products, animal husbandry, and giving birth to ewes are significantly correlated with the disease. Because of its long-lasting effects, Malta fever is known as the disease of a thousand faces [6]. Therefore, identifying and controlling it play a crucial role in improving public health [7]. Moreover, the wide spectrum of brucellosis symptoms in human has led to the fact that diagnosed people are considerably less than the actual number of the infected population 8, 9.
A database review indicates that numerous studies are carried out on the epidemiological features of Malta fever in Iran. An authentic measurement for the epidemiological and clinical features of Malta fever can be developed through combination of the research findings using meta-analysis [10]. Furthermore, through systematic review and meta-analysis of the results, we can provide well-grounded findings that can be used in public health policy-making and proposing suggestions for further research. The current research aimed to study the epidemiological and clinical features, and high-risk behaviors of people with Malta fever in Iran through carrying out a meta-analysis.
2. Materials and methods
2.1. Search strategy
Articles published in national and international journals, which were indexed in National Database, SID, Medlib, Magiran, Iranmedex, Scopus International Database, Science Direct, PubMed, and Google Scholar, were searched for relevant articles up to April 14, 2015. The search was looking for Persian and English keywords and the possible combination of important and sensitive terms. The keywords included Malta Fever, Iran, human brucellosis, brucellosis frequency, prevalence, epidemiology, along with using “AND” and “OR” operators in article subjects and abstracts. The Persian equivalents of the words were also searched among published articles. Some Persian databases were not sensitive to the operators, therefore, just Malta fever or brucellosis were searched. To prevent missing any studies and to increase the sensitivity, the references of the papers were also checked. The search was evaluated and reviewed randomly by two other researchers and the results indicated that no article was missed. Furthermore, paper databases were also searched for those articles that were not published electronically. Experts in this field were also consulted to find other unpublished works.
2.2. Study selection
Full text or abstracts, documents, and reports found in advanced searches were extracted. After excluding duplicates, irrelevant articles were also excluded through assessing titles, abstracts, and full texts, and finally the relevant studies were selected. To avoid publication bias (transverse and longitudinal), the studies were assessed and duplicate papers were excluded.
2.3. Quality assessment
The quality of the relevant articles was evaluated using the STROBE checklist (Strengthening the Reporting of Observational Studies in Epidemiology) [11] and another checklist used in a literature review [12]. Items related to study type, sample size, research objectives, population, inclusion and exclusion criteria for primary research, analysis method, and appropriate presentation of results were determined and a score was assigned to each item. Those studies scoring ≥ 8 were included in the research.
2.4. Data extraction
In each primary study, data were extracted based on title, first author name, publication year, sample size, the province in which the study was conducted, research type, residency status, average age, occupation (rancher and farmer, students, housewives), cattle contact history, unpasteurized dairy product usage, and the most common clinical signs (fever, joint pain, and sweating). Data were extracted by two researchers. We then examined the level of agreement between the results obtained by these two researchers.
2.5. Inclusion criteria
Persian and English studies with adequate sample size on epidemiological and clinical features and high-risk behaviors of patients with Malta fever were selected through the assessment procedure and scoring criteria.
2.6. Exclusion criteria
Studies that did not report the epidemiological and clinical features of Malta fever, those with unknown sample size, abstracts published in conference proceedings that did not include full text, and studies published before 1990 were not included. Case reports, case–control studies, and studies that did not score the minimum in quality assessment, were also excluded.
2.7. Statistical analysis
Stata version 11 (Stata version 11 Corporation, College Station, TX, USA) software was used to analyze the data. The standard error for frequency of epidemiological features, high-risk behavior and, clinical signs of people with Malta fever in each study was estimated using binomial distribution formula. Finally, heterogeneity index between the studies was determined using Cochran (Q) and I2 tests. Since the study incorporated sources of heterogeneity, a random-effect model was used to calculate the frequency of the epidemiological features, high-risk behavior, and clinical signs of people with Malta fever in Iran. Point estimation of the frequency percentage of epidemiological features, high-risk behavior, and clinical signs of people with Malta fever in Iran were calculated in accumulation graph (forest plots) with 95% confidence intervals.
3. Results
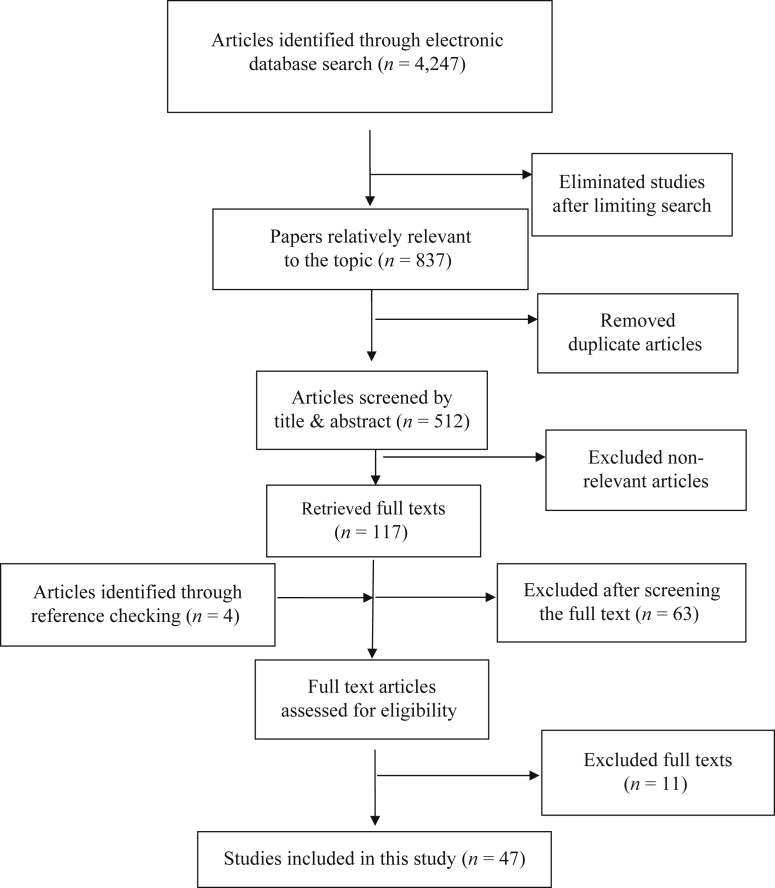
A total of 4,247 articles were found through our primary search in different databases, of which, 3,410 were excluded after narrowing the search results. Afterwards, the titles and abstracts of 837 primary studies were checked, of which, 442 relevant articles remained and 325 articles were excluded due to overlapping of databases. Finally, 117 articles were selected. The references were checked and four articles were found. Four articles were found to be duplicated and were published under two titles in different journals 4, 13, 14, 15, 16, 17, 18, 19. After assessing the full text of articles and excluding the irrelevant ones, 58 studies were controlled through assessment checklist and 11 articles were omitted. Finally, 47 articles were selected (Figure 1).
Figure 1.
Literature search and review flowchart for selection of primary studies.
In 47 studies selected for meta-analysis, we assessed the epidemiological features of 31,572 patients with Malta fever in Iran. Of 47 studies selected for this structural review, 42 articles followed analytical–descriptive methods and the remaining five articles did not follow any specific method. The publication year varied from 1998 to 2015 (Table 1).
Table 1.
Distribution of characteristics of primary studies included in meta-analysis.
| Id | First author (Ref) | Publication year | Sample size | Gender |
Area residence |
Job |
High Risk behavior |
Clinical sign |
Age |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Sex ratio | Urban | Rural | Ranchers and farmers | Student | Housewife | Animal contact | Unpasteurized dairy | Fever | Joint pain | Sweating | Average | least | high | ||||
| 1 | Hasanzadeh [20] | 2013 | 139 | 68.0 | 32.0 | 2.09 | 49.6 | 50.4 | 59.71 | 69.06 | 11–20 | ||||||||
| 2 | Almasi-Hashiani [21] | 2011 | 907 | 61.0 | 39.0 | 1.56 | 21.3 | 78.7 | 36.30 | 12.80 | 34.60 | 37.20 | |||||||
| 3 | Haddadi [22] | 2006 | 415 | 47.7 | 52.5 | 0.91 | 84.3 | 15.7 | 35.66 | 17.10 | 76.38 | 67.22 | 61.44 | 73.25 | 35.50 | <20 | 20–40 | ||
| 4 | Sharifi-Mood [23] | 2007 | 181 | 53.0 | 47.0 | 1.13 | 24.6 | 75.4 | 38.0 | 4.00 | 29.0 | 50.00 | 43.0 | 39.00 | |||||
| 5 | Sahargahi [24] | 2014 | 458 | 44.4 | 55.6 | 0.80 | 10.0 | 90.0 | 33.10 | 39.40 | 34.70 | ||||||||
| 6 | Ghasemi [25] | 2003 | 1,591 | 51.5 | 48.5 | 1.06 | 22.0 | 78.0 | 16.50 | 19.50 | 41.70 | 10.60 | 36.70 | 15–19 | |||||
| 7 | Ayazi [16] | 2012 | 175 | 61.0 | 39.0 | 1.56 | 43.0 | 57.0 | 50.00 | 58.00 | 65.0 | 78.00 | 22.50 | 44.0 | <1 | 7–12 | |||
| 8 | Eini [15] | 2012 | 230 | 56.5 | 43.5 | 1.30 | 23.8 | 72.6 | 39.70 | 60.30 | 77.40 | 70.00 | 46.90 | 40.84 | >80 | 21–60 | |||
| 9 | Kassiri [4] | 2013 | 43 | 65.1 | 34.9 | 1.87 | 17.1 | 82.9 | 20.90 | 6.70 | 30.20 | 20.90 | 79.10 | 33.34 | 0–4 | 15–24 | |||
| 10 | Shoraka [7] | 2010 | 64 | 68.8 | 31.2 | 2.20 | 9.4 | 90.6 | 12.50 | 15.60 | 26.60 | 82.80 | 23.40 | 62.50 | 56.20 | 32.80 | 30.70 | ||
| 11 | Karami [26] | 2009 | 194 | 45.0 | 55.0 | 0.83 | 37.0 | 63.0 | 17.53 | 16.49 | 39.69 | 60.00 | 40.00 | 70–79 | 10–29 | ||||
| 12 | Rajabzadeh [27] | 2013 | 1,310 | 55.3 | 44.7 | 1.24 | 28.5 | 71.5 | 19.80 | 13.10 | 36.30 | 77.80 | 60.89 | ||||||
| 13 | Golsha [28] | 2011 | 77 | 74.0 | 26.0 | 2.85 | 27.8 | 72.2 | 27.20 | 53.30 | 83.10 | ||||||||
| 14 | Fallah [29] | 1998 | 1,148 | 54.0 | 46.0 | 1.20 | >50 | <25 | |||||||||||
| 15 | Afsharpaiman [30] | 2008 | 40 | 65.9 | 34.1 | 2.10 | 61.0 | 39.0 | 65.90 | 77.40 | 50.0 | 52.30 | 7.31 | ||||||
| 16 | Beheshti [31] | 2001 | 130 | 61.0 | 39.0 | 2.51 | 45.0 | 55.0 | 58.50 | 49.00 | 98.00 | 72.0 | 92.0 | 30.00 | |||||
| 17 | Bokaie [32] | 2009 | 460 | 37.7 | 62.3 | 0.61 | 18.75 | 29.53 | 10–29 | ||||||||||
| 18 | Mamishi [33] | 2005 | 44 | 65.9 | 34.1 | 1.93 | 61.0 | 39.0 | 65.90 | 77.40 | 52.00 | 52.30 | 7.31 | ||||||
| 19 | Bokaie [34] | 2009 | 176 | 54.5 | 45.5 | 1.20 | 16.0 | 84.0 | <19 | 20–40 | |||||||||
| 20 | Ebrahimpour [35] | 2012 | 377 | 54.4 | 45.6 | 1.19 | 25.7 | 74.3 | 5.57 | 18.22 | 40.31 | 23.07 | <10 | >50 | |||||
| 21 | Hosseini [36] | 2009 | 115 | 68.7 | 32.2 | 2.11 | 34.80 | 13.90 | 23.50 | 80.90 | 89.60 | 86.10 | 77.40 | 73.90 | 29.40 | <2 | 17–35 | ||
| 22 | Farahani [37] | 2011 | 3,880 | 60.0 | 40.0 | 1.50 | 28.0 | 72.0 | >70 | 10–19 | |||||||||
| 23 | Bahador [38] | 2012 | 40 | 52.5 | 47.5 | 1.11 | 47.50 | 100.0 | 40.00 | >64 | 8–16 | ||||||||
| 24 | Kamran [39] | 2011 | 126 | 57.9 | 42.1 | 1.38 | 27.0 | 73.0 | 37.70 | 40.50 | 13.50 | 41.29 | 50–59 | ||||||
| 25 | Almasi [40] | 2012 | 210 | 69.9 | 30.1 | 2.32 | 46.20 | 52.90 | 61.40 | 34.30 | >60 | 15–30 | |||||||
| 26 | Soleimani [41] | 2012 | 5,732 | 54.9 | 45.1 | 1.22 | 14.4 | 85.6 | 80.00 | 86.40 | 30.90 | <5 | 15–25 | ||||||
| 27 | Ettehad [42] | 2007 | 51 | 76.5 | 23.5 | 3.25 | 34.0 | 66.0 | 62.00 | 84.20 | 44.00 | 60.20 | 6.25 | ||||||
| 28 | Soleimani [43] | 2010 | 42 | 68.8 | 24.4 | 2.82 | 33.0 | 67.0 | 33.30 | 83.0 | 76.40 | <5 | 10–15 | ||||||
| 29 | Maleki [44] | 2015 | 492 | 52.3 | 47.7 | 1.10 | 19.0 | 81.0 | 8.30 | 15.00 | 39.40 | >70 | 25–30 | ||||||
| 30 | Moradi [18] | 2006 | 3,880 | 52.1 | 47.9 | 1.09 | 18.2 | 81.8 | 20.80 | 20.60 | 39.40 | 62.10 | 30.03 | 45–54 | 16–44 | ||||
| 31 | Zeinalian Dastjerdi [45] | 2012 | 1,996 | 32.8 | 67.2 | 0.49 | 32.0 | 68.0 | 18.10 | 15.20 | 25.70 | 15–20 | |||||||
| 32 | Ghaffarpour [46] | 2007 | 15 | 60.0 | 40.0 | 1.50 | 33.0 | 67.0 | 33.30 | 53.30 | 37.70 | ||||||||
| 33 | Haj Abdolbaghi [47] | 2001 | 505 | 63.6 | 36.4 | 1.74 | 59.5 | 40.5 | 34.25 | 66.70 | 65.0 | 10–20 | |||||||
| 34 | Sasan [48] | 2012 | 82 | 60.0 | 40.0 | 1.21 | 29.8 | 70.2 | 76.0 | 91.60 | 5.0 | 79.70 | 8.02 | ||||||
| 35 | Hasanjani Roushan [49] | 2004 | 469 | 56.9 | 43.1 | 1.32 | 39.2 | 60.8 | 11.30 | 22.40 | 67.0 | 53.70 | 76.10 | 36.90 | |||||
| 36 | Pourahmad [50] | 2012 | 168 | 68.5 | 31.5 | 2.17 | 4.80 | 7.70 | 28.51 | ≥60 | 10–29 | ||||||||
| 37 | Hajia [51] | 2009 | 809 | 61.2 | 38.8 | 1.58 | 20.51 | 17.20 | 26.46 | 83.80 | 80.34 | 40.30 | >80 | 11–20 | |||||
| 38 | Moumen Heravi [52] | 2007 | 590 | 59.0 | 41.0 | 0.61 | 68.4 | 31.6 | 19.20 | 70.0 | 59.70 | ≥60 | 20–39 | ||||||
| 39 | Khalili [53] | 2014 | 32 | 75.0 | 25.0 | 3.00 | 39.00 | 41.0 | |||||||||||
| 40 | Mohammadian [54] | 2014 | 554 | 64.4 | 35.6 | 1.81 | 9.7 | 90.3 | 34.30 | <10 | 20–30 | ||||||||
| 41 | Noroozi [55] | 2012 | 1,253 | 53.0 | 47.0 | 1.13 | 28.0 | 72.0 | 16.50 | 11.50 | 35.50 | <10 | 20–29 | ||||||
| 42 | Esmaeilnasab [56] | 2007 | 1,059 | 50.8 | 49.2 | 1.03 | 10.0 | 90.0 | 27.10 | 12.70 | 44.20 | 34.05 | >55 | 25–44 | |||||
| 43 | Hamzavi [57] | 2014 | 777 | 52.6 | 47.4 | 1.11 | 12.4 | 87.6 | 32.30 | 37.80 | ≥70 | 20–29 | |||||||
| 44 | Sawadkohi [58] | 2002 | 116 | 1.60 | 97.0 | 44.0 | 6–24 | 60–144 | |||||||||||
| 45 | Fanni [59] | 2013 | 34 | 65.0 | 35.0 | 1.86 | 15.00 | 65.0 | 74.00 | 65.0 | 59.0 | 6.88 | 10–14 | 2–5 | |||||
| 46 | Mugahi [60] | 2014 | 81 | 59.3 | 40.7 | 1.45 | 46.9 | 53.1 | 12.30 | 18.50 | 58.0 | 85.20 | 42.0 | 38.30 | 38.10 | <20 | >40 | ||
| 47 | Dehnavi [61] | 2015 | 305 | 53.4 | 46.6 | 1.15 | 8.20 | 20.70 | 37.00 | 56.10 | 81.0 | 18.40 | 36.66 | >71 | 11–20 | ||||
Variables such as gender, residence, age, occupation, high-risk behavior, and clinical signs were assessed. Table 2 shows the frequency of the variables.
Table 2.
Estimation of frequency of brucellosis by epidemiological and clinical factors in Iran using meta-analysis.
| Variables | Frequency (95% CI) | Heterogeneity |
||
|---|---|---|---|---|
| Q | I2 (%) | p | ||
| Male | 57.6 (55.02–60.1) | 790.02 | 94.3 | <0.001 |
| Female | 42.3 (39.8–44.9) | 795.8 | 94.3 | <0.001 |
| Urban | 31.4 (26.7–36.3) | 3,308.9 | 98.9 | <0.001 |
| Rural | 68.4 (63.6–73.2) | 3,311.8 | 98.9 | <0.001 |
| Ranchers & farmers | 20.8 (17.4–24.2) | 740.4 | 96.9 | <0.001 |
| Students | 16.9 (14.5–19.4) | 210.5 | 92.9 | <0.001 |
| Housewife | 31.6 (27–36.2) | 862.2 | 97.6 | <0.001 |
| Animal contact | 50.4 (35.6–65.2) | 6,575.3 | 99.7 | <0.001 |
| Unpasteurized dairy | 57.1 (46.4–67.9) | 3,684 | 99.3 | <0.001 |
| Fever | 65.7 (53.7–77.8) | 2,832.04 | 99.2 | <0.001 |
| Joint pain | 58.1 (49.5–66.6) | 788.5 | 97.3 | <0.001 |
| sweating | 55.3 (44.4–66.2) | 849.6 | 98.1 | <0.001 |
CI = confidence limit.
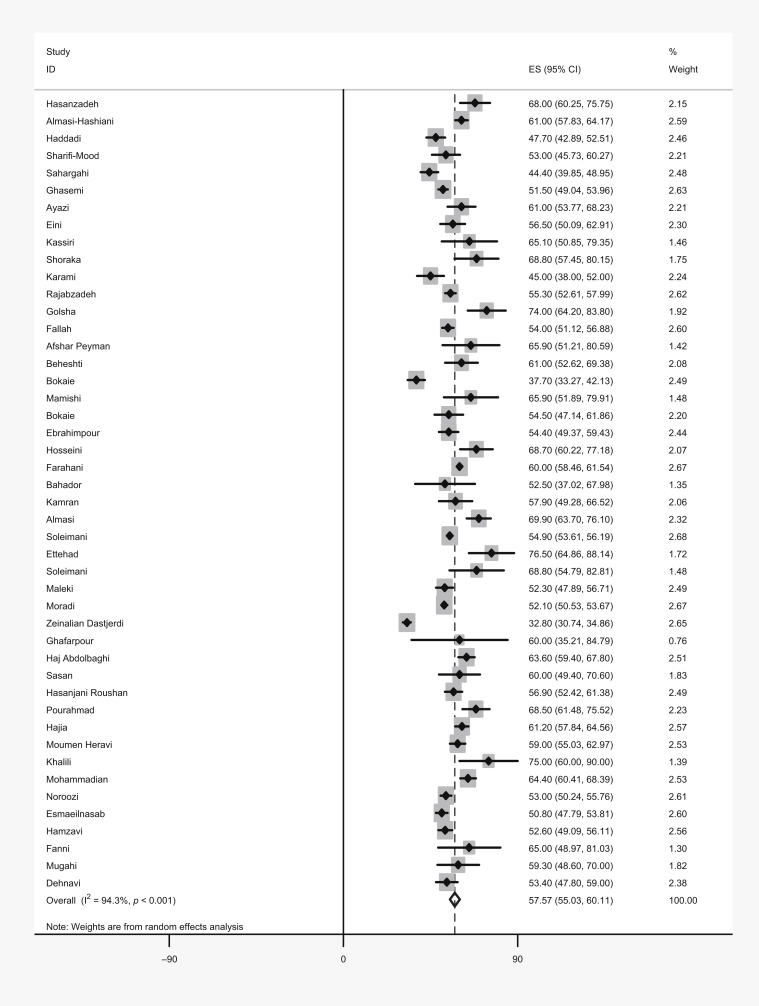
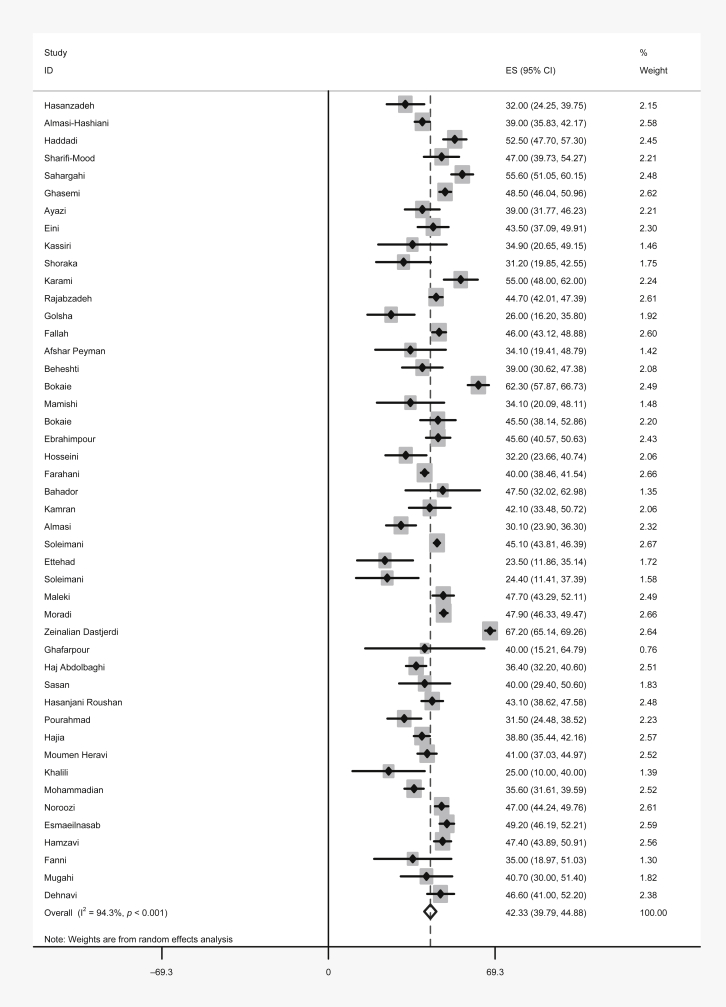
3.1. Gender
The gender distribution of patients with Malta fever was reported in 46 articles, which demonstrated that Malta fever in men varied from 32.8% (in Zeinalian Dastjerdi et al's [45] study) to 76.5% (in Ettehad et al's [42] study), and in women, it varied from 23.5% (in Ettehad et al's [42] study) to 67.2% (in Zeinalian Dastjerdi et al's [45] study). The ratio of male/female patients with Malta fever in 41 of 47 studies was > 1 and it varied from 0.49 (in Zeinlian Dastjedri's study) to 3.2 (in Ettehad et al's [42] study). Using meta-analysis, the frequency of Malta fever in men and women in Iran was estimated to be 57.6% (55.02–60.1%) and 42.3% (39.8–44.9%; Figure 2, Figure 3).
Figure 2.
Pooled estimate of brucellosis prevalence in Iranian men.
Figure 3.
Pooled estimate of brucellosis prevalence in Iranian women.
3.2. Residency
Thirty-six articles reported the residential status (rural and urban) of people with Malta fever. The prevalence of Malta fever in accordance with residential status varied from 9.4% (in Shoraka et al's [7] study) to 84.3% (In Haddadi et al's [22] study) in urban areas and 15.7% (in Haddadi et al's [22] study) to 90.6% (Shoraka et al's [7] study) in rural areas. The results of meta-analysis demonstrated that 31.4% (26.7–36.3%) and 68.4% (63.6–73.2%) of patients with Malta fever in Iran lived in urban and rural areas, respectively.
3.3. Age
The mean age of people with Malta fever was reported in 26 studies, which varied from 6.25 years (in Ettehad et al's [42] study) to 41.29 years (in Kamran et al's [39] study). The 10–40 years age group was the most frequent group with Malta fever in Iran. Age has not been estimated by using meta-analysis so far. The reason is that the standard error could not be calculated as a result of information deficiency in primary studies.
3.4. Occupation
The frequency of Malta fever among ranchers and farmers was reported in 24 studies, which varied from 4.8% (in Pourahmad et al's [50] study) to 47.5% (in Bahador et al's [38] study). The frequency of Malta fever among students was reported in 16 studies, which varied from 6.7% (in Kassiri et al's [4] study) to 50% (in Ayazi et al's [16] study). The frequency of Malta fever among housewives was reported in 22 studies, varying from 4% (in Sharifi-Mood's study) to 44.2% (in Esmaeilnasab et al's [56] study). The results of occupation meta-analysis were as follows: 20.8% (17.4–24.2%) of the patients with Malta fever in Iran were ranchers and farmers; 16.9% (14.5–19.4%) were students, and 31.6% (27–36.2%) were housewives.
3.5. High-risk behavior
Eighteen articles reported contact with animals and breathing in barns and stable environments among patients with Malta fever, which varied from 10.6% (in Ghasemi et al's [25] study) to 82.8% (in Shoraka et al's [7] study). The results of meta-analysis indicated that direct contact with animals in 50.4% (35.6–65.2%) of patients was reported as the cause of the disease. Twenty-six articles reported the frequency of using unpasteurized dairy products among patients with Malta fever; the results of which varied from 22.4% (in Hasanjani Roushan et al's [49] study) to 100% (Bahador et al's [38] study). The results of meta-analysis indicated that using unpasteurized dairy products was reported as the cause of the disease in 57.1% (46.4–67.9%) of the patients.
3.6. Clinical signs
Regarding the clinical signs, the frequency of fever was reported in 23 studies, which varied from 5% (in Sasan et al's [48] study) to 98% (in Beheshti et al's [31] study). The frequency of joint pain was reported in 22 studies, which varied from 13.5% (in Kamran et al's [39] study) to 83% (in Soleimani et al's [41] study). The frequency of sweating was reported in 17 studies, which varied from 18.4% (in Dehnavi et al [61]'s study) to 92% (in Beheshti et al's [31] study). According to the meta-analysis results, the frequency of fever, joint pain and sweating was 65.7% (53.7–77.8%) and 55.3% (44.4–66.2%), respectively.
4. Discussion
The current study investigated the epidemiology, clinical features and high-risk behavior among patients with Malta fever through a meta-analysis. The results revealed that 57.6% of the patients were male and 42.3% were female, which is a significant difference due to the 95% confidence interval and nonoverlapping. Of the patients studied, 31.4% and 68.4% resided in urban and rural areas, respectively, which was a significant difference. With respect to occupation, about 21% of the patients were ranchers and farmers, about 17% were students, and 31.6% were housewives. About 50% of the patients had contact with cattle and 57% used unpasteurized dairy products. Regarding the clinical signs, 58.1% of the patients had joint pain. Most of patients were aged 10–40 years.
Malta fever is more prevalent in men than women, therefore, gender is introduced as a risk factor in some studies 5, 62, 63. In a study conducted by Donev et al [64], it was demonstrated that Malta fever was more prevalent among villagers than people residing in urban areas due to having contact with infected animals and using unpasteurized products. A study conducted in Saudi Arabia indicated that brucellosis in rural areas was more prevalent as compared to urban areas [65]. Another study of Malta fever among children aged < 15 years in Jordan demonstrated that living in villages increased the chance of being infected with brucellosis [66].
The age range of patients with Malta fever in most studies was consistent with our research 65, 67, 68, 69, 70. In a study conducted by Mohammad Al-Sekait [71], high-risk behavior, direct contact with infected cattle, and using unpasteurized dairy products were considered as the most important factors affecting Malta fever in Madina. In a case–control study in Yemen, Al-Shamahy et al [72] reported that farmers and inhabitants who consumed unpasteurized dairy products were more affected with Malta fever than the control group. In yet another study carried out in a province of Saudi Arabia, the most infected occupational group included housewives, farmers, ranchers, and students [65]. Husseini et al [6] found that Palestinian farmers were more susceptible to being infected with Malta fever as compared with other occupations. The results of a study conducted in Oman revealed that consuming infected milk and contact with infected cattle were the main causes of Malta fever [73]. In a study on inhabitants of eight villages in Greece, it was demonstrated that using unpasteurized dairy products, being in the risky occupation group (i.e., ranchers and slaughterhouse workers), and having contact with infected animals were among the factors leading to more cases of Malta fever [74]. A study carried out in Northern Egypt reported that people who had contact with animals were more susceptible to Malta fever than those with no animal contact [70]. Earhart et al [75], in their study on Samarqand in Uzbekistan, found that Malta fever was more prevalent among people whom had more contact with cattle and those who used more dairy products.
In a study conducted in Turkey, using unpasteurized dairy products, raising cattle, and having risky occupations (veterinarians and butchers) were considered as factors affecting Malta fever, and fever and joint pain were reported as the most common symptoms of this disease [76]. Other studies carried out in Turkey also report fever, sweating, and joint pain as the most prevalent clinical signs 77, 78. In a systematic review study conducted by Dean et al [79], it was indicated that fever, sweating, and joint pain were the most prevalent symptoms of Malta fever.
In Macedonia, Bosilkovski et al [80] found that most people with Malta fever, had a history of direct animal contact and suffered mostly from joint pain and sweating.
Heterogeneity was a limitation of the current research. To resolve this, the research used a random-effect model. Another limitation was that epidemiological features and high-risk behavior, such as article selection criteria, were scattered and, therefore, they were not measured comprehensively in all articles.
The present study revealed that the frequency of male patients with brucellosis was considerably more than female patients. The number of patients with brucellosis in rural areas was significantly more than in urban areas. Most patients were economically active in society. High-risk behavior, unprotected contact with animals, and using unpasteurized dairy products were among the most significant factors determining brucellosis infection in Iran. A high incidence of the disease in some occupational groups, such as ranchers, farmers, and housewives, and rural areas (compared to urban areas), is probably due to the frequency of high-risk behavior. Fever, joint pain, and sweating were detected among most patients with Malta fever.
Conflicts of interest
The authors declare that there was no conflict interest.
References
- 1.Hasanjani Roushan M.R., Asgharzadeh Ahmadi S.A., Smailnejad Gangi S.M. Childhood brucellosis in Babol, Iran. Trop Doct. 2005 Oct;35(4):229–231. doi: 10.1258/004947505774938693. [DOI] [PubMed] [Google Scholar]
- 2.Sofian M., Aghakhani A., Velayati A.A. Risk factors for human brucellosis in Iran: a case–control study. Int J Infect Dis. 2008 Mar;12(2):157–161. doi: 10.1016/j.ijid.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 3.Pappas G., Akritidis N., Bosilkovski M. Brucellosis. N Engl J Med. 2005;352(22):2325–2336. doi: 10.1056/NEJMra050570. [DOI] [PubMed] [Google Scholar]
- 4.Kassiri H., Amani H., Lotfi M. Epidemiological, laboratory, diagnostic and public health aspects of human brucellosis in western Iran. Asian Pac J Trop Biomed. 2013 Aug 28;3(8):589–594. doi: 10.1016/S2221-1691(13)60121-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Minas M., Minas A., Gourgulianis K. Epidemiological and clinical aspects of human brucellosis in Central Greece. Jpn J Infect Dis. 2007 Aug 20;60(6):362–366. [PubMed] [Google Scholar]
- 6.Husseini A.S., Ramlawi A.M. Brucellosis in the West Bank, Palestine. Saudi Med J. 2004;25(11):1640–1643. [PubMed] [Google Scholar]
- 7.Shoraka H.R., Hosseini S.H., Safavizadeh A. Epidemiological study of brucellosis in Maneh & Semelghan town, North Khorasan province, in 2008-2009. J North Khorasan Univ Med Sci. 2010;2(2-3):65–72. [In Persian] [Google Scholar]
- 8.Dames S., Tonnerre C., Saint S. Clinical problem solving. Don't know much about history. N Engl J Med Overseas Ed. 2005;352(22):2338–2342. doi: 10.1056/NEJMcps041883. [DOI] [PubMed] [Google Scholar]
- 9.Mantur B.G., Biradar M.S., Bidri R.C. Protean clinical manifestations and diagnostic challenges of human brucellosis in adults: 16 years' experience in an endemic area. J Med Microbiol. 2006 Jul;55(7):897–903. doi: 10.1099/jmm.0.46097-0. [DOI] [PubMed] [Google Scholar]
- 10.Haghdoost A.A., Moosazadeh M. The prevalence of cigarette smoking among students of Iran's universities: A systematic review and meta-analysis. J Res Med Sci. 2013 Aug;18(8):717–725. [PMC free article] [PubMed] [Google Scholar]
- 11.Von Elm E., Altman D.G., Egger M. The Strengthening the Reporting of Observational Studies in Epidemiology [STROBE] statement: guidelines for reporting observational studies. Prev Med. 2007;45(4):247–251. doi: 10.1016/j.ypmed.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 12.Moosazadeh M., Nekoei-moghadam M., Emrani Z. Prevalence of unwanted pregnancy in Iran: a systematic review and meta-analysis. Int J Health Plann Mgmt. 2014 Jul-Sep;29(3):e277–e290. doi: 10.1002/hpm.2184. [DOI] [PubMed] [Google Scholar]
- 13.Kassiri H., Amani H., Lotfi M. Epidemiological aspects of human brucellosis in Azna County, Lorestan Province, West of Iran (2007–2008) Jundishapur J Health Res. 2011 Apr;1(2):1–9. [Google Scholar]
- 14.Eini P., Esna-Ashari F., Mobaien A.R. A retrospective evaluation of epidemiological, clinical and laboratory features of brucellosis in 230 patients in Hamadan, Iran: a brief report. Tehran Univ Med J. 2012 May;70(2):130–135. [In Persian] [Google Scholar]
- 15.Eini P., Keramat F., Hasanzadehhoseinabadi M. Epidemiologic, clinical and laboratory findings of patients with brucellosis in hamadan, west of Iran. J Res Health Sci. 2012;12(2):105–108. [PubMed] [Google Scholar]
- 16.Ayazi P., Mahyar A., Rasoli A. Brucellosis in children. J Comprehens Pediatr. 2012 Nov;3(1):12–15. [Google Scholar]
- 17.Ayazi P., Rasoli A. Epidemiological, clinical and laboratory features of brucellosis: a retrospective evaluation of 175 children. J Comprehens Pediatr. 2007 Jan;1(2):31–36. [Google Scholar]
- 18.Moradi G., Esmaiel Nasab N., Ghaderi E. Brucellosis in Kurdistan Province from 1997 to 2003. Ann Alquds Med. 2006 Jan;2(1):32–37. [Google Scholar]
- 19.Moradi G., Kanani S., Majidpour M. Epidemiological status survey of 3880 case of brucellosis in Kurdistan. Iran J Infect Dis Trop Med. 2006 Jun;11(33):27–33. [In Persian] [Google Scholar]
- 20.Hasanzadeh A., Rahimi I., Shakerian A. survey of epidemiology brucellosis in Mobarakeh, Esfahan from 2003 to 2010. Bull Env Pharmacol Life Sci. 2013 Nov;2(12):87–90. [Google Scholar]
- 21.Almasi-Hashiani A., Khodayari M., Eshrati B. Factors affecting the interval between the onset and diagnosis of brucellosis in Markazi Province, Iran (2010-11) J Arak Univ Med Sci. 2012 Apr;14(7):21–30. [In Persian] [Google Scholar]
- 22.Haddadi A., Rasoulinejad M., Afhami S. Epidemiological, clinical, para clinical aspects of brucellosis in Imam Khomeini and Sina Hospital of Tehran (1998-2005) J Kermanshah Univ Med Sci. 2006 Fall;10(3):242–251. [In Persian] [Google Scholar]
- 23.Sharifi-Mood B., Metanat M., Moradian M. Poor nutrition, behavioral patterns and medical myths: important risk factors for Malta fever in Sistan and Baluchestan. Iran J Clin Infect Dis. 2007;12(38):59–62. [Google Scholar]
- 24.Sahargahi B., Rezaei M., Naderi M. Comparison of the human brucellosis incidence trend in Eslam Abad-e-Gharb town, Kermanshah province and Iran (2006–2010) J Kermanshah Univ Med Sci. 2014 May;18(2):122–124. [In Persian] [Google Scholar]
- 25.Ghasemi B., Mohammadian B., Soofimajidpour M. Epidemiology of human and animal brucellosis in Kurdistan Province in 1997–2001. Sci J Kurdistan Univ Med Sci. 2004 Winter;8(30):23–32. [In Persian] [Google Scholar]
- 26.Karami K., Saeidi Kia N., Kazemi F. The epidemiological study of brucellosis patients referred to the laboratories and health centers in Andimeshk Township (2005–2006) Jundishapur J Health Sci. 2009 Dec;1(1):29–35. [Google Scholar]
- 27.Rajabzadeh R., Shoraka H., Arzamani K. Epidemiological aspects of brucellosis in North Khorasan province, during 2006–2011. J North Khorasan Univ Med Sci. 2013;5(4):753–761. [Google Scholar]
- 28.Golsha R., Hezareh A., Golshah E. Presentation of brucellosis in Northeast of Iran: a 5-year study. Electronic Physician. 2011;3:407–408. [Google Scholar]
- 29.Fallah R., Alipour M. Evaluation of brucellosis referring to the health network in Mazandaran province and its relationship with some demographic factors. J Zanjan Univ Med Sci. 1998;6(25):23–27. [In Persian] [Google Scholar]
- 30.Afsharpaiman S., Mamishi S. Brucellosis: review of clinical and laboratory features and therapeutic regimens in 44 children. Acta Med Iran. 2008;46(6):489–494. [Google Scholar]
- 31.Beheshti S., Rezaian G., Aghasadeghi K. Brucellosis in Iran: the Fars province experience. Med J Islam Repub Iran. 2001;15(2):67–71. [Google Scholar]
- 32.Bokaie S., Latibari S.H., Abbaszadeh S. Ecological study of brucellosis in humans and animals in Khoy, a mountainous District of the IR. of Iran. Iran J Microbiol. 2009 Dec;1(4):14–17. [Google Scholar]
- 33.Mamishi S., Afshar P.S., Satvati J. Brucellosis; clinical manifestation, laboratory finding and management in children admitted to children medical center. Iran J Infect Dis Trop Med. 2005 Aug;10(29):7–11. [Google Scholar]
- 34.Bokaie S., Sharifi L., Alizadeh H. Epidemiological survey of brucellosis in human and animals in Birjand, east of Iran. J Anim Vet Adv. 2008 Apr;7(4):460–463. [Google Scholar]
- 35.Ebrahimpour S., Youssefi M.R., Karimi N. The prevalence of human brucellosis in Mazandaran province, Iran. Afr J Microbiol Res. 2012 May 23;6(19):4090–4094. [Google Scholar]
- 36.Hosseini S., Hosseini Shokouh S.J., Alishirei G. Epidemiology of human brucellosis in Ferdows, Sarayan and Boshrooyeh counties of southern Khorasan province in 2004–2005. Ann Mil Health Sci Res. 2009;7(2):117–122. [Google Scholar]
- 37.Farahani S., Shah Mohamadi S., Navidi I. An investigation of the epidemiology of brucellosis in Arak City, Iran,(2001–2010) J Arak Univ Med Sci. 2011;14(6):49–54. [In Persian] [Google Scholar]
- 38.Bahador A., Mansoori N., Esmaeili D. Brucellosis: prevalence and retrospective evaluation of risk factors in western cities of Tehran province, Iran. J Bacteriol Res. 2012 Aug;4(3):33–37. [Google Scholar]
- 39.Kamran A., Farahani A., Bakhtiyar K. Epidemiological, clinical, and treatment aspects of brucellosis in Khorramabad, Iran. J Health Syst Res. 2011;7(6):1235–1242. [In Persian] [Google Scholar]
- 40.Almasi A., Hashemian A., Azizi A. Epidemiology of brucellosis in population under coverage of Mahidasht health and Curative center through 2004-2010 based on Geographical Information System (GIS) Arch Sci. 2012 Nov;65(11):406–412. [Google Scholar]
- 41.Soleimani A., Alizadeh S., Seif F.M. Descriptive epidemiology of human brucellosis in east Azerbaijan, 2001-2009. Med J Tabriz Univ Med Sci. 2012 Apr-May;34(1):63–69. [Google Scholar]
- 42.Ettehad G., Derakhshani F., Habibzadeh S.H. Evaluation of clinical, laboratory and therapeutic findings of brucellosis among children hospitalized at Ardabil hospitals. Res J Biol Sci. 2007;2(2):150–154. [Google Scholar]
- 43.Soleimani G. Evaluation of clinical findings and treatment of childhood brucellosis in Zahedan. Iranian J Pediatr Soc. 2010 Apr-Jun;2(2):53–57. [Google Scholar]
- 44.Maleki F., RafieManesh H., Abbasi-Ghahramanloo A. Epidemiological characteristics of human brucellosis in Shahin Dezh, Western Azarbaijan, Iran, 2008–2012. Arch Clin Infect Dis. 2015 Jan 24;10(1):1–4. [Google Scholar]
- 45.Zeinalian Dastjerdi M., Fadaei Nobari R., Ramazanpour J. Epidemiological features of human brucellosis in central Iran, 2006–2011. Public Health. 2012 Dec;126(12):1058–1062. doi: 10.1016/j.puhe.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 46.Ghaffarpour M., Khoshroo A., Harirchian M. Clinical, epidemiological, laboratory and imaging aspects of brucellosis with and without neurological involvemen. Acta Med Iran. 2007;45(1):63–68. [Google Scholar]
- 47.Haji Abdolbagi M., Rasooli Nejad M., Yaghoob Zadeh M. Epidemiological, clinical, diagnostic and therapeutic survey in 505 cases with brucellosis. Tehran Univ Med J. 2001;59(1):34–46. [In Persian] [Google Scholar]
- 48.Sasan M.S., Nateghi M., Bonyadi B. Clinical features and long term prognosis of childhood brucellosis in northeast Iran. Iran J Pediatr. 2012 Sep;22(3):319–325. [PMC free article] [PubMed] [Google Scholar]
- 49.Hasanjani Roushan M., Mohrez M., Smailnejad Gangi S. Epidemiological features and clinical manifestations in 469 adult patients with brucellosis in Babol, Northern Iran. Epidemiol Infect. 2004 Dec;132(6):1109–1114. doi: 10.1017/s0950268804002833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pourahmad M., Tadayon S., Fadaei S. Demographic characteristics and wright test titers in patients treated for brucellosis. J Jahrom Univ Med Sci. 2012;10(1):17–22. [Google Scholar]
- 51.Hajia M., Rahbar M., Keramat F. Epidemiological, clinical, diagnostic and treatment aspects of hospitalized brucellosis patients in Hamadan. Ann Trop Med Public Health. 2009;2(2):42–45. [Google Scholar]
- 52.Momen Heravi M., Afzali H. Clinical manifestations of brucellosis in hospitalized patients in Beheshti Hospital of Kashan 1996–2003. Feyez. 2007;11(1):67–72. [In Persian] [Google Scholar]
- 53.Khalili M., Sharifi-Mood B., Metanat M. Epidemiology, clinical presentation, and treatment outcome of brucellosis among children. Int J Infect. 2014 Sep 10;1(3):e21570. [Google Scholar]
- 54.Mohammadian M., Mohammadian Hafshejani A. Epidemiological characteristics and incidence rate of brucellosis over a period of 14 years in the Tiran-Karvan Township, Isfahan, Iran. J Isfahan Med Sch. 2014 Sep;32(293):1–7. [Google Scholar]
- 55.Noroozi M., Saghafipour A., Zia Sheikholeslami N. Investigation of the Epidemiology of brucellosis and its associated risk factors in Qom Province (2001–2011) Alborz Univ Med J. 2012;1(4):193–199. [Google Scholar]
- 56.Esmaeilnasab N., Banafshi O., Ghaderi E. Epidemiologic change investigation of brucellosis in Kurdistan province in 2006–2007. J Large Animal Clin Sci Res (J Vet Med) 2007 Fall;1(3):53–58. [In Persian] [Google Scholar]
- 57.Hamzavi Y., Khademi N., Ghazi Zadeh M.M. Epidemiology of malt fever in Kermanshah province in 2011. J Kermanshah Univ Med Sci. 2014 May;18(2):114–121. [In Persian] [Google Scholar]
- 58.Sawadkohi R., Siadati S., Zoughi E. Evaluation of under 12 year-old patients with Malta fever In Tehran Children Medical Center & Amirkola Children Hospital, Babol-1995–99. J Mazandaran Univ Med Sci. 2002;11(33):46–52. [In Persian] [Google Scholar]
- 59.Fanni F., Shahbaznejad L., Pourakbari B. Clinical manifestations, laboratory findings, and therapeutic regimen in hospitalized children with brucellosis in an Iranian referral children medical centre. J Health Popul Nutr. 2013 Jun;31(2):218–222. doi: 10.3329/jhpn.v31i2.16386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mugahi S., Nashibi R., Alavi S.M. Epidemiological features, clinical manifestation and laboratory findings of patients with brucellosis. Arch Clin Infect Dis. 2014 Jan;9(1):1–4. [Google Scholar]
- 61.Dehnavi S., Sohrabi N., Afshari Safavi A. Demographic characteristics, clinical signs and laboratory findings in brucellosis hospitalized patients in Kermanshah. J Clin Res Paramed Sci. 2015;3(4):216–222. [Google Scholar]
- 62.Čekanac R., Mladenović J., Ristanović E. Epidemiological characteristics of brucellosis in Serbia, 1980–2008. Croat Med J. 2010 Aug;51(4):337–344. doi: 10.3325/cmj.2010.51.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li Y.J., Li X.L., Liang S. Epidemiological features and risk factors associated with the spatial and temporal distribution of human brucellosis in China. BMC Infect Dis. 2013 Nov;16(13):547. doi: 10.1186/1471-2334-13-547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Donev D., Karadzovski Z., Kasapinov B. Epidemiological and public health aspects of brucellosis in the Republic of Macedonia. Prilozi. 2010;31(1):33–54. [PubMed] [Google Scholar]
- 65.Elbeltagy K. An epidemiological profile of brucellosis in Tabuk Province, Saudi Arabia. East Mediterr Health J. 2001 Jul-Sep;7(4-5):791–798. [PubMed] [Google Scholar]
- 66.Al-Majali A.M., Shorman M. Childhood brucellosis in Jordan: prevalence and analysis of risk factors. Int J Infect Dis. 2009 Mar;13(2):196–200. doi: 10.1016/j.ijid.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 67.Fallatah S.M., Oduloju A.J., Al-Dusari S.N. Human brucellosis in Northern Saudi Arabia. Saudi Med J. 2005 Oct;26(10):1562–1566. [PubMed] [Google Scholar]
- 68.Buzgan T., Karahocagil M.K., Irmak H. Clinical manifestations and complications in 1028 cases of brucellosis: a retrospective evaluation and review of the literature. Int J Infect Dis. 2010 Jun;14(6):469–478. doi: 10.1016/j.ijid.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 69.Aypak C., Altunsoy A., Kutta Celik A. Epidemiological and clinical aspects of human brucellosis in eastern Anatolia. J Nippon Med Sch. 2012;79(5):343–348. doi: 10.1272/jnms.79.343. [DOI] [PubMed] [Google Scholar]
- 70.Meky F., Hassan E., Abdel Hafez A. Epidemiology and risk factors of brucellosis in Alexandria governorate. East Mediterr Health J. 2007 May-Jun;13(3):677–685. [PubMed] [Google Scholar]
- 71.Al-Sekait M.A. Epidemiology of brucellosis in Al Medina region, Saudi Arabia. J Family Community Med. 2000 Apr;7(1):47–53. [PMC free article] [PubMed] [Google Scholar]
- 72.Al-Shamahy H., Whitty C., Wright S. Risk factors for human brucellosis in Yemen: a case control study. Epidemiol Infect. 2000 Oct;125(2):309–313. doi: 10.1017/s0950268899004458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.El-Amin E.O., George L., Kutty N.K. Brucellosis in children of Dhofar Region, Oman. Saudi Med J. 2001 Jul;22(7):610–615. [PubMed] [Google Scholar]
- 74.Hadjichristodoulou C., Papatheodorou C., Soteriades E. Epidemiological study of brucellosis in eight Greek villages using a computerised mapping programme. Eur J Epidemiol. 1999 Aug;15(7):671–680. doi: 10.1023/a:1007673318947. [DOI] [PubMed] [Google Scholar]
- 75.Earhart K., Vafakolov S., Yarmohamedova N. Risk factors for brucellosis in Samarqand Oblast, Uzbekistan. Int J Infect Dis. 2009 Nov;13(6):749–753. doi: 10.1016/j.ijid.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 76.Demiroglu Y.Z., Turunc T., Aliskan H. [Brucellosis: retrospective evaluation of the clinical, laboratory and epidemiological features of 151 cases] Mikrobiyol Bul. 2007 Oct;41(4):517–527. [in Turkish] [PubMed] [Google Scholar]
- 77.Sit D., Kadiroglu A.K., Kayabasi H. [Retrospective evaluation of brucellosis cases inhabiting in Mus province] Mikrobiyol Bul. 2006 Jul;40(3):289–290. [in Turkish] [PubMed] [Google Scholar]
- 78.Zribi M., Ammari L., Masmoudi A. [Clinical manifestations, complications and treatment of brucellosis: 45-patient study] Pathol Biol (Paris) 2009 Jul;57(5):349–352. doi: 10.1016/j.patbio.2008.02.003. [in French] [DOI] [PubMed] [Google Scholar]
- 79.Dean A.S., Crump L., Greter H. Clinical manifestations of human brucellosis: a systematic review and meta-analysis. PloS Negl Trop Dis. 2012 Dec;6(12):e1929. doi: 10.1371/journal.pntd.0001929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bosilkovski M., Krteva L., Dimzova M. Human brucellosis in Macedonia – 10 years of clinical experience in endemic region. Croat Med J. 2010 Aug;51(4):327–336. doi: 10.3325/cmj.2010.51.327. [DOI] [PMC free article] [PubMed] [Google Scholar]