Abstract
This study was conducted in Iran in order to assess the distribution of CTX-M type ESBLs producing Enterobacteriaceae. From January 2012 to December 2013, totally 198 E. coli, 139 Klebsiella spp, 54 Salmonella spp and 52 Shigella spp from seven hospitals of six provinces in Iran were screened for resistance to extended-spectrum cephalosporins. After identification and susceptibility testing, isolates presenting multiple-drug resistance (MDR) were evaluated for ESBL production by the disk combination method and by Etest using (cefotaxime and cefotaxime plus clavulanic acid). All isolates were also screened for blaCTX-M using conventional PCR. A total of 42.92%, 33.81%, 14.81% and 7.69% of the E. coli, Klebsiella spp, Salmonella spp and Shigella spp isolates were MDR, respectively. The presence of CTX-M enzyme among ESBL-producing isolates was 85.18%, 77.7%, 50%, and 66.7%, in E. coli, Klebsiella spp, Salmonella spp and Shigella spp respectively. The overall presence of CTX-M genes in Enterobacteriaceae was 15.4% and among the resistant isolates was 47.6%. This study indicated that resistance to β-lactams mediated by CTX-M enzymes in Iran had similar pattern as in other parts of the world. In order to control the spread of resistance, comprehensive studies and programs are needed.
Keywords: Klebsiella spp, Salmonella spp, Shigella spp, Escherichia coli, Multi-drug resistant, ESBL, CTX-M
Introduction
The emergence of new enzyme groups that have a typical extended spectrum β-lactamase (ESBL) resistance phenotype, but are non-TEM and non-SHV derivatives, have been reported in Enterobacteriaceae.1 CTX-M-type β-lactamases constitute a novel group of molecular class A ESBLs encoded by transferable plasmids. These enzymes exhibit overall preference for cefotaxime (CTX; hence the name CTX-M) and ceftriaxone along with higher susceptibility to tazobactam than clavulanate.1, 2
The explosive dissemination of CTX-Ms around the world has been referred to as “CTX-M pandemic” due to their increasing description worldwide.3 These enzymes have different prevalence rates in various members of the Enterobacteriaceae family. They mostly exist in enterobacterial species such as Escherichia coli, Klebsiella pneumoniae, and Salmonella enterica serovar Typhimurium. In contrast, production of ESBLs is uncommon among the isolates of Shigella sonnei.4
Firstly, two CTX-M-type enzymes were reported in Europe in 1989.5 But, they did not become predominant over the other ESBL enzymes until the first decade of the XXI century, in which an extraordinary spread of these enzymes was observed both in hospital and community settings.6 Nowadays, a variety of different types of this enzyme has been identified.3 At the time of writing this article, more than 160 CTX-M-type β-lactamases have been identified in various clinical isolates (www.lahey.org/studies), classified in five families according to the amino acid sequence: CTX-M-1, CTX-M-2, CTX-M-8, CTX-M-9, and CTX-M-25; two additional groups have been reported recently: CTX-M-74 and CTX-M-75,6 two of which (CTX-M-2 and CTX-M-8 types) are shown to be similar (95–100%) to the chromosomally encoded β-lactamase of Kluyvera ascorbata and Kluyvera georgiana, respectively,7, 8 while the original sources of the other enzymes of this group remain unknown. The blaCTX-M genes have been found on a number of plasmids and are commonly associated with IS mobile elements, such as ISEcp1, found flanking the open reading frame region of the blaCTX-M genes.9
The CTX-M group has become the most common type of ESBL in Latin America, but is also becoming more common in Europe and has been recently reported in the UK.3 Also, in Asia, previous reports have identified CTX-M producing isolates in China, Korea, Japan, and India.10 Resistance to broad-spectrum β-lactams is becoming an ever-increasing problem in Iran.11 In this work, we investigate the distribution of CTX-M-type enzymes in the clinical isolates of Enterobacteriaceae, including Escherichia coli, Klebsiella spp, Salmonella spp, and Shigella spp in seven hospitals from six provinces of Iran.
Material and methods
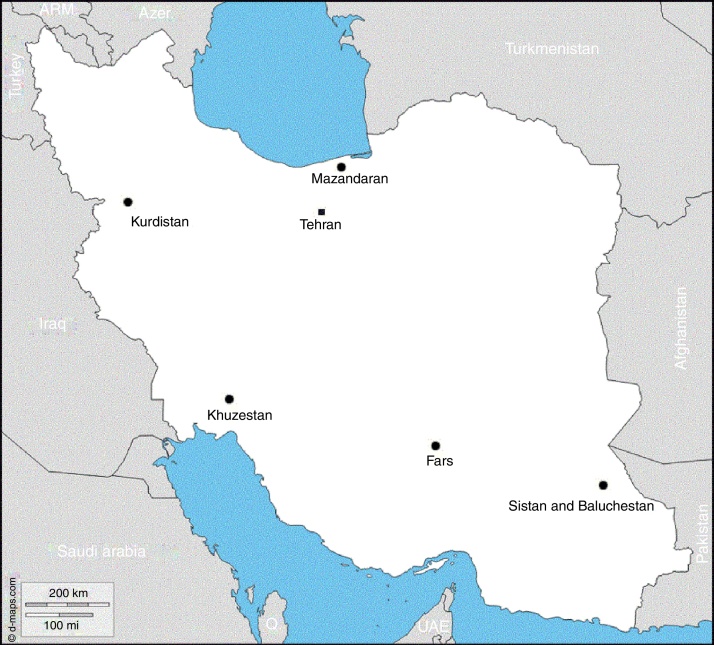
This cross-sectional study was performed on the isolates collected from seven hospitals of six provinces in Iran. They included the provinces of Tehran, Kurdistan, Sistan and Baluchestan, Mazandaran, Khuzestan, and Fars. Tehran isolates were collected from two hospitals, namely Milad and Mehr. The geographic distribution of the surveyed hospitals and isolates collected from different provinces are shown in Fig. 1 and Table 1, respectively. During the studied period, totally, 198 Escherichia coli, 139 Klebsiella spp, 54 Salmonella spp, and 52 Shigella spp were collected and used for further investigations. The studied samples included urine (mostly), blood, sputum, wound, respiratory and vaginal secretions, ascites, biopsies, and body fluids. Identification of the isolates was done using conventional standard biochemical tests, including plating in blood agar, chocolate agar, MacConkey agar, Salmonella–Shigella agar (Merck, Germany), triple sugar iron agar, urea agar, SIM medium, and IMVic (indole, methyl red, Voges-Proskauer, and citrate).12
Fig. 1.
Geographic locations of hospitals surveyed in this study.
Table 1.
Total isolates collected from different provinces in Iran.
| Bacteria | Province |
|||||||
|---|---|---|---|---|---|---|---|---|
| Tehran (Milad) | Tehran (Mehr) | Kurdistan | Sistan and Baluchestan | Mazandaran | Khuzestan | Fars | Total | |
| E. coli | 78 | 14 | 37 | 30 | 6 | 25 | 38 | 198 |
| Klebsiella spp | 80 | 6 | 11 | 2 | 1 | 9 | 30 | 139 |
| Salmonella spp | 46 | 1 | 2 | 0 | 0 | 4 | 1 | 54 |
| Shigella spp | 50 | 0 | 0 | 0 | 0 | 2 | 0 | 52 |
ESBL confirmatory test
To confirm ESBL production, those isolates that were identified as resistant to ceftriaxone using the disk diffusion susceptibility test were further subjected to the disk combination method.13, 14 The combination disk method utilized discs containing only cefotaxime (CTX) (30 mg) and other disk containing cefotaxime (CTX) (30 mg) combined with clavulanic acid (CLA) (10 mg) (MAST Diagnostics, Merseyside, UK). ESBL producing isolates were identified as those with a greater than 5 mm increase in the zone with the single antimicrobial compared with the combined antimicrobial, i.e. demonstrating ESBL inhibition.15
Antimicrobial susceptibility testing
The antimicrobial susceptibility test was done by Kirby-Bauer disk diffusion methodology according to the guidelines of Clinical and Laboratory Standards Institute.16 Antibiogram was done for tetracycline (30 μg), ampicillin (10 μg), amoxicillin (20 μg), cephalothin (30 μg), gentamicin (10 μg), amikacin (30 μg), cefotaxime (30 μg), ceftazidime (30 μg), cefixime (30 μg), imipenem (10 μg), ciprofloxacin (5 μg), and antibiotics (MAST Diagnostics, Merseyside, UK).
To assess the effectiveness of the antibiotic concentration gradient, E-test (AB Biodisk, Dalvagen, Sweden) using the cefotaxime concentration gradient strips was applied. For this purpose, E-test was studied in a medium containing clavulanic acid (4 μg/ml) and a simple medium simultaneously. The expected reduction in MIC in the presence of the β-lactamase inhibitor was ≥3 log2 dilution steps.17
Polymerase chain reaction (PCR)
Isolates with an ESBL phenotype were further investigated for blaCTX-M alleles. Bacterial DNA was extracted from the isolates by boiling the bacterial suspensions. DNA isolates with the concentration of 0.1 ng/μl were used as the templates for PCR analysis. PCR was done by CINNAGEN MsterMix (Cinnaclon, Iran), which was performed with the universal primers CTX-M-U1 (5′-ATG TGC AGY ACC AGT AAR GTK ATG GC-3′) and CTX-M-U2 (5′-TGG GTR AAR TAR GTS ACC AGA AYC AGC GG-3′), as described previously.18 Amplification was carried out in a Techne TC-512 thermocycler (Eppendorf, Hamburg, Germany) as follows: 30 cycles of 50 s for denaturation at 94 °C, 50 s for annealing at 58 °C, and 50 s for primer extension at 72 °C, followed by terminal extension at 72 °C for 10 min. Initial denaturation at 95 °C for 5 min was used for both amplifications. Electrophoresis of PCR products was performed on 1% agarose gel. The gel staining was performed in ethidium bromide for 20 min and visualized in gel documentation system (Bio-rad, Hercules, USA).
Sequencing
To confirm PCR products, sequencing was randomly done for 114 isolates by Takapozist Company, Iran (on behalf of Bioneer Company, Korea). All the sequencing results were interpreted by LaserGene software (DNASTAR, MADISON) including SeqMan, MegAlign, and EditSeq software.
Statistical analysis
Statistical analysis was performed in SPSS 12.0 (SPSS, Chicago, IL, USA). The variables were analyzed by univariate analysis using v2 or Fisher's exact test, as appropriate. Statistical significance was set at p < 0.05.
Results
During the studied period, 198 E. coli, 139 Klebsiella spp, 54 Salmonella spp, and 52 Shigella spp were totally investigated. In the present study, MDR was defined as acquired non-susceptibility to at least one agent in three or more antimicrobial categories. A total of 42.92%, 33.81%, 14.81% and 7.69% of the E. coli, Klebsiella spp, Salmonella spp and Shigella spp isolates were MDR, respectively. Increasing the diameter of the disk containing β-lactamase inhibitor (over 5 mm) represents the production of ESBL enzymes, whose data are shown in Table 2. The CTX-M was detected in 15.4% of the isolates and the presence of this gene in all of the resistant isolates was 47.6%.
Table 2.
Test result of E-test and double-disk diffusion for diagnosis of ESBL-producing and Cephalosporinase-producing isolates.
| Bacteria: | Total isolates | Resistant (%) | ESBL producing in resistant isolates | Total ESBL producing isolates | Cephalosporinase producers in resistance isolates |
|---|---|---|---|---|---|
| E. coli | 198 | 85 (42.92%) | 54 (63.52%) | 54 (27.27%) | 45 (52.94%) |
| Klebsiella spp | 139 | 47 (33.81%) | 36 (%6.59%) | 36 (25.9%) | 32 (68.08%) |
| Salmonella spp | 54 | 8 (14.81%) | 2 (25%) | 2 (25%) | 3 (75%) |
| Shigella spp | 52 | 4 (7.69%) | 3 (75%) | 3 (5.77%) | 2 (25%) |
Among E. coli isolates from the provinces of Fars, Sistan and Baluchestan, Kurdistan, Mazandaran, and Tehran's Mehr hospital, 100% of ESBL-producing isolates were CTX-M positive. Also, 50% of Kurdistan and 75% of Tehran's Milad hospital were CTX-M positive. Totally, 88.37% of the MDR and ESBL positive E. coli isolates (cephalosporinase) contained CTX-M and consisted of 46.91% of the total MDR isolates detected by PCR technique. In the case of Klebsiella spp, 87.09% of the MDR isolates were ESBL-producing and contained CTX-M genes, which consisted of 56.25% of the total MDR isolates. Among ESBL-producing Salmonella spp isolates, 50% contained CTX-M gene that consisted of 14.28% of the total MDR isolates.
Totally, out of 52 Shigella spp isolates, 7.69% were MDR, 5.77% of which was ESBL-producing. All the patients with drug resistance were under 10 years old and all resistant isolates were related to Tehran's Milad Hospital. Seventy-five percent of the resistant isolates belonged to male and 25% were female, and all the isolated bacteria were from stool. In the resistant isolates, 100% were resistant to ampicillin, amoxicillin, cephalothin, gentamicin, and ceftazidime. Also, 75% and 50% were resistant to tetracycline and ceftizoxime, respectively. All the isolates were sensitive to ciprofloxacin and imipenem. Seventy-five percent of the resistant isolates had ESBL-producing enzymes that were identified by the double disk diffusion method. All ESBL-producing isolates were determined by cefotaxime E-test for cephalosporinase production and the results of all the isolates were positive. In the genomic analysis of resistant genes, 75% of ESBL-producing Shigella spp isolates or nearly 50% of the MDR isolates contained CTX-M gene. Also, the sequencing results indicated that CTX-M15 present in all the isolates was examined.
Discussion
In the present study, we examined the presence of ESBL-producing isolates and identification of CTX-M enzymes involved in resistance to third-generation cephalosporins as possible. This study showed that resistance to β-lactams mediated by CTX-M enzymes in Iran had similar pattern as in other parts of the world.
There are different reports from different geographical regions on the specific focus of multi-drug resistance.19 So, to determine the prevalence of resistance in Iran, we decided to evaluate the occurrence of such resistance from different parts of the country. The presence of CTX-M in all of the resistant isolates was 47.6%, a rate that was similar to the prevalence in the studies of other parts of the world. In a similar study from South Korea on 603 Enterobacteriaceae, 6.8% of the total isolates and 44.1% of resistant isolates were carrying CTX-M genes.20
There are different reports on the prevalence of these enzymes in Enterobacteriaceae family from Iran and other parts of the world. In a study from Tehran hospitals, ESBL production rate in Klebsiella pneumoniae was 72.1%, 45.2% of which had blaCTX-M.21 Another study from Tehran on the clinical isolates of E. coli revealed 56.69% production of ESBL, 35.78% of which was positive for blaCTX-M genes from the CTX-M-I group and 2.1% was positive for blaCTX-M genes from the CTX-M-III group.22 A study in Kurdistan Province reported that 34.85% of Enterobacteriaceae family was ESBL producing.23
The low number of ESBL-producing isolates in the present study might be because of the diversity of clones examined in this study. In the studies that have been done in other parts of the world, different prevalence rates have been reported. The prevalence of these enzymes in European countries for E. coli and Klebsiella spp has been 5.4% and 23–25%, respectively.24 This rate is very low in Japan; i.e. in E. coli and Klebsiella spp, it was less than 0.1% and 0.3%, respectively.13 In other parts of Asia, 4.8% Korea,13 8.5% Taiwan,25 12% Hong Kong,26 and 28% in Malaysia27 have been reported.
E. coli is the predominant pathogen that carries CTX-M enzymes and the isolates carrying this gene are often isolated in UTI, bacteremia, and gastroenteritis.28 In this study, the most ESBL-producing E. coli carrying CTX-M genes was from urine, bacteremia, respiratory infections, and gastroenteritis isolates, respectively.
In the case of Klebsiella spp, CTX-M enzymes are important after SHV and TEM. ESBL producing isolates can be isolated from respiratory infections, intra-abdominal infections, and blood flow.28, 29 But, in the present study, most of the ESBL-producing Klebsiella carrying CTX-M genes were isolated from the samples of urinary tract infections and respiratory tract, wound, and blood. Sex distribution of the patients complied with the kind of infections. Most isolates of E. coli were in women with urinary tract infections. Conversely, most of the patients with Klebsiella spp with respiratory infections were men.
The presence of CTX-M enzyme among ESBL producing isolates of E. coli, Klebsiella spp, Salmonella spp, and Shigella spp was 85.18%, 77.7%, 50%, and 66.7%, respectively. In a similar study in the United Kingdom and Ireland, similar results to those stated in this study, i.e. 83% of ESBL-producing E. coli and 74% of ESBL-producing Klebsiella, were found which were due to CTX-M genes.30 It is obvious that β-lactam resistance due to CTX-M enzymes has similarly grown in Iran and other parts of the world, which shows the need for comprehensive studies and programs to control the spread of resistance.
The frequency and distribution of CTX-M genes in different geographic regions examined in this study showed that, due to the indiscriminate use of new generation antibiotics in the more developed regions, a higher level of resistant genes was identified. As a statistical comparison of the rates of resistant isolates of Tehran's Milad Hospital and Medical Center in Sanandaj (Kurdistan Province), significant differences were observed (p-value: 0.0007).
Certainly, as shown in the present study, comprehensive control of antibiotics is extremely important. The most important way to control the spread of resistance is control of risk factors. The present study suggested the necessity for identifying patterns of transmission and spread of antibiotic resistance in wider geographical areas and developing a comprehensive program to manage and control the use of antibiotics.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgments
The authors would like to thank Dr. Navidinia for his review of manuscript and all staff of Microbiology labs collaborated in this study (From All participated centers). Also, Authors thank Mr. Nikmaram in Imam Reza Hospital – Tabriz for help on sample collection. This study was granted by Drug applied research Center, Tabriz University of Medical Sciences.
Associate Editor: Afonso Luís Barth
References
- 1.Bradford P.A. Extended-spectrum β-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin Microbiol Rev. 2001;14:933–951. doi: 10.1128/CMR.14.4.933-951.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tzouvelekis L., Tzelepi E., Tassios P., Legakis N. CTX-M-type β-lactamases: an emerging group of extended-spectrum enzymes. Int J Antimicrob Agents. 2000;14:137–142. doi: 10.1016/s0924-8579(99)00165-x. [DOI] [PubMed] [Google Scholar]
- 3.Canton R., Coque T.M. The CTX-M beta-lactamase pandemic. Curr Opin Microbiol. 2006;9:466–475. doi: 10.1016/j.mib.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Lartigue M., Poirel L., Decousser J., Nordmann P. Multidrug-resistant Shigella sonnei and Salmonella enterica serotype Typhimurium isolates producing CTX-M β-lactamases as causes of community-acquired infection in France. Clin Infect Dis. 2005;40:1069–1070. doi: 10.1086/428667. [DOI] [PubMed] [Google Scholar]
- 5.Barthelemy M., Peduzzi J., Bernard H. ended-spectrum beta-lactamase MEN-1 and chromosomally encoded enzymes of Klebsiella oxytoca. Biochim Biophys Acta. 1992;1122:15–22. doi: 10.1016/0167-4838(92)90121-s. [DOI] [PubMed] [Google Scholar]
- 6.Lahlaoui H., Khalifa A.B.H., Moussa M.B. Epidemiology of Enterobacteriaceae producing CTX-M type extended spectrum β-lactamase (ESBL) Med Malad Infect. 2014;44:400–404. doi: 10.1016/j.medmal.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 7.Humeniuk C., Arlet G., Gautier V. β-Lactamases of Kluyvera ascorbata, probable progenitors of some plasmid-encoded CTX-M types. Antimicrob Agents Chemother. 2002;46:3045–3049. doi: 10.1128/AAC.46.9.3045-3049.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poirel L., Kämpfer P., Nordmann P. Chromosome-encoded Ambler class A β-lactamase of Kluyvera georgiana, a probable progenitor of a subgroup of CTX-M extended-spectrum β-lactamases. Antimicrob Agents Chemother. 2002;46:4038–4040. doi: 10.1128/AAC.46.12.4038-4040.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saladin M., Cao V.T., Lambert T. Diversity of CTX-M beta-lactamases and their promoter regions from Enterobacteriaceae isolated in three Parisian hospitals. FEMS Microbiol Lett. 2002;209:161–168. doi: 10.1111/j.1574-6968.2002.tb11126.x. [DOI] [PubMed] [Google Scholar]
- 10.Hawkey P.M. Prevalence and clonality of extended-spectrum β-lactamases in Asia. Clin Microbiol Infect. 2008;14:159–165. doi: 10.1111/j.1469-0691.2007.01855.x. [DOI] [PubMed] [Google Scholar]
- 11.Behrooozi A., Rahbar M., Yousefi J.V. Frequency of extended spectrum beta-lactamase (ESBLs) producing Escherichia coli and Klebsiella pneumoniae isolated from urine in an Iranian 1000-bed tertiary care hospital. Afr J Microbiol Res. 2010;4:881–884. [Google Scholar]
- 12.Koneman W., Allen Stephan D. Lippincott; Philadelphia, NY: 1997. Color atlas and text book of diagnostic microbiology. [Google Scholar]
- 13.Jarlier V., Nicolas M.H., Fournier G. Extended broad-spectrum beta-lactamases conferring transferable resistance to newer beta-lactam agents in Enterobacteriaceae: hospital prevalence and susceptibility patterns. Rev Infect Dis. 1988;10:867–878. doi: 10.1093/clinids/10.4.867. [DOI] [PubMed] [Google Scholar]
- 14.Thomson K.S., Sanders C.C. Detection of extended-spectrum beta-lactamases in members of the family Enterobacteriaceae: comparison of the double-disk and three-dimensional tests. Antimicrob Agents Chemother. 1992;36:1877–1882. doi: 10.1128/aac.36.9.1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.al Naiemi N., Duim B., Bart A. A CTX-M extended-spectrum beta-lactamase in Pseudomonas aeruginosa and Stenotrophomonas maltophilia. J Med Microbiol. 2006;55:1607–1608. doi: 10.1099/jmm.0.46704-0. [DOI] [PubMed] [Google Scholar]
- 16.Yershov G., Barsky V., Belgovskiy A. DNA analysis and diagnostics on oligonucleotide microchips. PNAS. 1996;93:4913–4918. doi: 10.1073/pnas.93.10.4913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sturenburg E., Mack D. Extended-spectrum beta-lactamases: implications for the clinical microbiology laboratory, therapy, and infection control. J Infect. 2003;47:273–295. doi: 10.1016/s0163-4453(03)00096-3. [DOI] [PubMed] [Google Scholar]
- 18.Monstein H.J., Östholm-Balkhed Å., Nilsson M. Multiplex PCR amplification assay for the detection of blaSHV, blaTEM and blaCTX-M genes in Enterobacteriaceae. Apmis. 2007;115:1400–1408. doi: 10.1111/j.1600-0463.2007.00722.x. [DOI] [PubMed] [Google Scholar]
- 19.Bialvaei A.Z., Kafil H.S. Colistin, mechanisms and prevalence of resistance. Curr Med Res Opin. 2015;31:707–721. doi: 10.1185/03007995.2015.1018989. [DOI] [PubMed] [Google Scholar]
- 20.Kim J., Lim Y.M. Prevalence of CTX-M extended-spectrum beta-lactamases in clinical isolates of entrobacteriaceae in Korea. J Bacteriol Virol. 2004;34:303–310. [Google Scholar]
- 21.Feizabadi M.M., Mahamadi-Yeganeh S., Mirsalehian A. Genetic characterization of ESBL producing strains of Klebsiella pneumoniae from Tehran hospitals. J Infect Dev Ctries. 2010;4:609–615. doi: 10.3855/jidc.1059. [DOI] [PubMed] [Google Scholar]
- 22.Mirzaee M., Pourmand M., Chitsaz M., Mansouri S. Antibiotic resistance to third generation cephalosporins due to CTX-M-type extended-spectrum β-lactamases in clinical isolates of Escherichia coli. Iran J Pub Health. 2009;38:10–17. [Google Scholar]
- 23.Ramazanzadeh R., Chitsaz M., Bahmani N. Prevalence and antimicrobial susceptibility of extended-spectrum beta-lactamase-producing bacteria in intensive care units of Sanandaj general hospitals (Kurdistan, Iran) Chemotherapy. 2009;55:287–292. doi: 10.1159/000224656. [DOI] [PubMed] [Google Scholar]
- 24.Stobberingh E., Arends J., Hoggkamp-Korstanje J. Occurrence of extended-spectrum betalactamases (ESBL) in Dutch hospitals. Infect. 1999;27:348–354. doi: 10.1007/s150100050041. [DOI] [PubMed] [Google Scholar]
- 25.Nordmann P., Poirel L., Kubina M. Biochemical-genetic characterization and distribution of OXA-22, a chromosomal and inducible class D beta-lactamase from Ralstonia (Pseudomonas pickettii) Antimicrob Agents Chemother. 2000;44:2201–2204. doi: 10.1128/aac.44.8.2201-2204.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ho P.L., Tsang D.N., Que T.L. Comparison of screening methods for detection of extended-spectrum beta-lactamases and their prevalence among Escherichia coli and Klebsiella species in Hong Kong. Apmis. 2000;108:237–240. doi: 10.1034/j.1600-0463.2000.d01-50.x. [DOI] [PubMed] [Google Scholar]
- 27.Cheong Y., Lim V., Jegathesan M., Suleiman A. Antimicrobial resistance in 6 Malaysian general hospitals. Med J Malaysia. 1994;49:317–326. [PubMed] [Google Scholar]
- 28.Pitout J.D., Laupland K.B. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis. 2008;8:159–166. doi: 10.1016/S1473-3099(08)70041-0. [DOI] [PubMed] [Google Scholar]
- 29.Bialvaei A.Z., Kafil H.S., Asgharzadeh M. Current methods for the identification of carbapenemases. J Chemother. 2015 doi: 10.1179/1973947815Y.0000000063. [DOI] [PubMed] [Google Scholar]
- 30.Reynolds R., Hope R.D.M.L. Activity of Doripenem in the context of rising antimicrobial resistance in invasive Entrobacteriaceae in the UK and Ireland. 46th ICAAC; San Francisco; 2006. pp. C2–C0065. [Google Scholar]