Abstract
Malaria infection begins when the sporozoite stage of Plasmodium is inoculated into the skin of a mammalian host through a mosquito bite. The highly motile parasite not only reaches the liver to invade hepatocytes and transform into erythrocyte-infective form. It also migrates into the skin and to the proximal lymph node draining the injection site, where it can be recognized and degraded by resident and/or recruited myeloid cells. Intravital imaging reported the early recruitment of brightly fluorescent Lys-GFP positive leukocytes in the skin and the interactions between sporozoites and CD11c+ cells in the draining lymph node. We present here an efficient procedure to recover, identify and enumerate the myeloid cell subsets that are recruited to the mouse skin and draining lymph node following intradermal injection of immunizing doses of sporozoites in a murine model. Phenotypic characterization using multi-parametric flow cytometry provides a reliable assay to assess early dynamic cellular changes during inflammatory response to Plasmodium infection.
Keywords: Immunology, Issue 111, Plasmodium, rodent, innate immunity, skin, lymph node, myeloid cells, enzymatic digestion
Introduction
Malaria is one of the deadliest infectious diseases in the world, killing more than half a million people per year. Infection by Plasmodium, the causal agent of the disease, begins by a pre-erythrocytic (PE) phase. During this phase, sporozoites injected into the host skin by a female Anopheline mosquito reach the liver via the bloodstream and differentiate inside hepatocytes into the parasite forms that infect red blood cells and cause the symptoms of the disease.
The PE stages of Plasmodium represent a privileged target for anti-malaria vaccination. Indeed, live attenuated vaccines against these stages, such as radiation attenuated sporozoites (RAS), genetically arrested parasites (GAP) or chemoprophylaxis and sporozoites (CPS) have demonstrated their capacity to protect both rodent and human hosts1-9. In the rodent model, most vaccination studies are conducted utilizing intravenous immunization, which is the gold standard in terms of protective efficacy. However, the description of a skin stage and the importance of the skin-associated draining lymph node (dLN) in eliciting protection has changed our perception of the PE phase and emphasized the importance of the intradermal route of injection. Intravital imaging of P. berghei sporozoites injected into the skin of rodents has shown that only ~25% of the inoculum reaches the liver via the bloodstream. The remaining ~75% distributes between the proximal dLN (~15%) and the skin (~50%)10,11, where a small proportion can transform and remain alive for weeks inside skin cells12,13. Moreover, subsequent studies described that the establishment of effective protective immunity after intradermal immunization mainly takes place in the skin-dLN, where parasite specific CD8+ T cells are activated, and only marginally in the spleen or liver-dLNs14,15.
While most studies have concentrated on the characterization of the effector cells implicated in the establishment of protective immune response, much less is known about the fate of live attenuated parasites injected into the skin, especially their interactions with the innate immune system. In particular, characterization of antigen-presenting cells involved in parasite antigen uptake, processing and presentation to CD8+ T cells is of critical importance, knowing that PE antigen acquisition can occur both in the skin and dLN compartments. Previous intravital imaging studies described an early influx of brightly fluorescent Lys-GFP positive cells in the skin following an infectious mosquito bite16 while early interactions between sporozoites and dendritic cells were observed in the dLN10,17. More recently, it has been reported that sporozoites inoculated in the skin by mosquitoes increases the motility of both dendritic and regulatory T cells in the skin of mice, while a decrease number of antigen presenting cells was observed in the dLN18.
We aimed to identify and quantify more precisely the leukocyte subsets recruited in the skin and corresponding dLN as well as those interacting with the parasite following intradermal injection of immunizing doses of RAS19. In this context, we isolated myeloid cells (CD45+CD11b+) from both tissues and characterized subpopulations of interest by multi=parametric flow cytometry. Consistent with the immune response described in the early stage of Leishmania major skin infection20, the primary host response to sporozoite injection consists of a successive recruitment of polymorphonuclear neutrophils (CD45+CD11b+Ly6G+Ly6Cint) followed by inflammatory monocytes (CD45+CD11b+Ly6G-Ly6C+) which are identified on the basis of differential expression of the Ly6G and Ly6C surface markers.
We describe here a protocol for isolating myeloid cells from the mouse skin and dLN following intradermal injection of immunizing doses of RAS extracted from infected mosquito salivary glands. Reproducible intradermal injections and tissue processing are critical steps to quantify phenotypic changes of infiltrating cell population within infected tissues. The approach detailed below provides a reliable assay to assess the skin and dLN inflammatory response to Plasmodium parasite and can be extended to various experimental systems.
Protocol
All procedures were approved by the committee of the Pasteur Institute and by the local Ethics Committee on Animal Experimentation (Ethical committee IDF-Paris 1, Paris, France; agreement number: 2012-0015) and performed in accordance with the applicable guidelines and regulations.
1. Materials and Reagents
Use female Anopheles stephensi mosquitoes (Sda500 strain) that feed on infected mice 3-5 days after emergence and rear as described previously21.
Use parasites Plasmodium berghei ANKA clone expressing the Green Fluorescent Protein (GFP) gene under the control of the constitutive Heat Shock Protein 70 (HSP70) promoter. This yields bright fluorescence throughout the parasite life cycle22.
Use female C57BL/6JRj mice (7 week-old). NOTE: All the reagents used in the described protocol are listed in the Table of Materials/Equipment.
2. Radiation-attenuated Sporozoite Isolation from Mosquito Salivary Glands
Between 18-25 days after the infectious blood meal, collect and cold-anesthetize mosquitoes into a 15 ml tube on ice as described previously21. Carefully transfer them onto a Petri dish by inverting the tube. Maintain the insects on ice and expose the mosquitoes to a 12 krad dose of γ- or x-irradiation.
Isolate attenuated sporozoites from irradiated mosquito salivary glands as previously described21. Collect infected salivary glands in a small volume (around 15 μl) of 1x Dulbecco's phosphate-buffered saline (DPBS) on ice and gently crush them to release sporozoites. NOTE: The injection of a highly concentrated parasite suspension in a small volume being critical, it is therefore essential to harvest a sufficient number of salivary glands from a high number of preselected well-infected mosquitoes, as evidenced by their robust expression of green-fluorescence.
Filter the sporozoite suspension through a 35 µm cell strainer cap adapted to a low adhesion 1.5 ml microcentrifuge tube in order to eliminate clumps and mosquito debris.
Count the total number of isolated sporozoites as previously described21 and adjust the concentration of parasite suspension with cold 1x DPBS to obtain 83,000 sporozoites/μl. Store the parasites on ice while continuing the next steps.
Collect the equivalent number of salivary glands from uninfected mosquitoes that will be used as negative control and process the sample as described in steps 2.2 and 2.3. Dilute the sample as indicated above to obtain similar concentration of salivary gland extracts in the suspension. NOTE: Sporozoites can be stored on ice for a maximum of 2 hr. However, ideally they are injected within an hour after crushing the salivary glands.
3. Injection of Sporozoites into the Dermal Layer of the Ear
Anesthetize animals by intraperitoneal injection of ketamine (50 mg/kg)/xylazine (5 mg/kg) mixture. Wait 5-8 min for the mouse to be in a state of unconsciousness and apply ophthalmic ointment to the eyes to prevent corneal drying. Evaluate the depth of anaesthesia by performing a gentle toe pinch on both rear feet. NOTE: The dose of anaesthesia lasts for less than 20 min, so the next steps must be done quickly.
Stabilize the ear pinna of the mouse by fixing the ventral side with clear tape previously placed under a stereomicroscope (Figure 1A). Gently press the ear to avoid damage of the vasculature.
Load a 10 μl syringe/35 gauge bevelled needle with 0.6 µl of resuspended parasites10.
Deliver the sporozoite suspension in 4 injection sites (0.15 µl per site) by carefully inserting the needle on the dorsal side of the ear (Figure 1A), beneath the epidermis, with the bevel up, taking care to avoid any blood vessels. Allow the needle to remain in the dermis for few sec to prevent backflow of the injectant before removing it. Observe a characteristic papule at each injection site at the end of the procedure (Figure 1B and 1C).
After injection, carefully remove the ear from the tape.
Inject the contralateral ear with the same dose of parasites by following the steps 3.2-3.4.
Inject 2 additional mice with either 0.6 µl of 1x DPBS or 0.6 µl of 1x DPBS + salivary gland extract from uninfected mosquitoes in order to evaluate the inflammatory response mediated by the injection alone and the deposition of mosquito material in the dermis.
Monitor mouse recovery from anaesthesia before placing it back into the cage. NOTE: The proper sporozoite deposition in the skin can be monitored by fluorescence microscopy (Figure 2A and 2B), the mouse being prepared as described previsously23.
4. Skin and Draining Lymph Node Dissection
Prepare standard medium (SM) as follows: Dulbecco's Modified Eagle Medium (DMEM) + 25 mM 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) supplemented with 400 U/ml collagenase and 50 μg/ml deoxyribonuclease (DNase).
Prepare two 6 well flat-bottom tissue culture plates on ice with 4.5 ml SM + 70 μm cell strainer per well for dLN samples (Plate A) and 4.5 ml SM per well for skin samples (Plate B).
At the desired time point following sporozoite inoculation, deeply anesthetize the mouse by intraperitoneal injection of ketamine (125 mg/kg)/xylazine (12.5 mg/kg) mixture prior cervical dislocation. Make sure the mouse demonstrates signs of clinical death and start the dissection immediately. NOTE: The kinetics of myeloid cell recruitment can be examined at different times after injection (i.e. 2 hr, 4 hr and 24 hr as previously described14).
Disinfect the inoculated ear and the corresponding neck region with 70% ethanol to reduce the possibility of contamination.
Using sterile scissors and forceps, aseptically dissect the proximal auricular dLN without collecting the surrounding fat. Perform a first incision in the jugulo-carotidian sulcus and remove the hairs from the operating field. Stretch the incision with 2 forceps to expose the dLN that appears grayish compared to the surrounding tissue.
Pinch the connective tissues carefully on the top of the dLN with forceps to facilitate its removal. Extract the dLN by placing a forceps underneath the lymphoid tissue (Figure 3A and 3B). Place the dLN in a well containing 4.5 ml SM + 70 μm cell strainer (Plate A).
Harvest the entire inoculated ear using sterile sharp scissors and forceps (Figure 4A). Separate the dorsal and ventral aspects of the ear by pinching and spacing apart the cut ends with two forceps (Figure 4B-4E). Place them into a well containing 4.5 ml SM (Plate B) making sure both tissues are completely immersed in the medium. NOTE: In order to improve the reliability of the experiment and increase the number of cells of interest, pool 2 injected ears or 2 dLNs from the same mouse per sample.
Harvest and process in parallel the ears and dLNs of mice inoculated with either 1x DPBS or salivary gland extracts. Include 2 additional ear and lymph node samples harvested from a naive mouse for negative and single staining compensation controls.
5. Cell Isolation from Lymph Nodes
Incubate the lymph nodes (Plate A) at 37 °C + 5% CO2 for 15 min under gentle agitation. Add 10 mM final Ethylenediaminetetraacetic acid (EDTA) per well to neutralize collagenase and DNase activities. Perform the next steps on ice.
Dissociate lymph nodes using the top end of a 5 ml syringe plunger. Press in circular motions against the strainer until all that remains is white connective tissues.
Rinse the cell strainer twice with 500 μl 1x DPBS + 2% Fetal bovine serum (FBS) + 2mM EDTA. Transfer entire volume of the well in a 15 ml tube.
Rinse the well twice with 500 μl 1x DPBS + 2% FBS + 2mM EDTA and transfer the volume into the 15 ml tube. Keep tubes on ice.
6. Cell Isolation from Skin of the Ear
Incubate the ear leaflets (Plate B) at 37 °C + 5% CO2 for 1 hr under gentle agitation. NOTE: After 20 min of incubation, cut the ear leaflets with scissors into small pieces to facilitate tissue digestion and put the sample back in the incubator for the remaining 40 min. Single cells can be observed in the medium at the end of the incubation time.
Add 10 mM final EDTA per well to neutralize collagenase and DNase activities. Perform the next steps on ice.
Transfer the ear tissue fragments and the whole volume of medium in a new well containing a 70 μm cell strainer using a 1ml pipette. Cut 2 to 3 mm from the end of the tip to collect the ear tissue fragments more easily.
Dissociate ear tissue fragments using the top end of a 5 ml syringe plunger. Press in circular motions against the strainer until all that remains is white connective tissues.
Rinse the cell strainers twice with 500 μl 1x DPBS + 2% FBS + 2 mM EDTA.
Transfer the entire volume of the well into a 50 ml-tube through a 70 μm cell strainer.
Rinse the well with 500 μl 1x DPBS + 2% FBS + 2 mM EDTA and transfer the volume into the 50 ml tube. Keep the tube on ice. NOTE: The different steps to isolate total cells from the skin and dLN tissues are summarized in Figure 5.
7. Count and Viability of Collected Cells
Centrifuge the skin and dLN samples for 5 min at 450 x g at 4 °C and discard the supernatant. Gently resuspend the pellet with 300 μl 1x DPBS + 2% FBS + 2 mM EDTA.
Collect a small volume of each sample to count the total number of cells isolated from the skin and dLN using a hemocytometer. Add 0.04% trypan blue to determine the cell viability.
8. Blocking of Non Antigen-specific Binding
Add 10 µg/ml of unlabelled CD16/CD32 Fc-block antibody. Incubate 20 min at 4 °C (can go longer).
Add 2 ml of cold 1x DPBS + 2% FBS + 2 mM EDTA. Centrifuge the sample for 5 min at 450 x g at 4 °C and discard the supernatant. Gently resuspend the pellet with 300 μl 1x DPBS + 2% FBS + 2 mM EDTA and maintain the samples on ice.
9. Staining Skin and Lymph Node Myeloid Cells
Incubate previously blocked skin and dLN isolated cells with Live/Dead tracker (i.e. 4',6-diamidino-2-phenylindole or DAPI), anti-CD45 and anti-CD11b specific antibodies. NOTES: In order to enrich the myeloid cell subpopulations of interest, especially rare ones, CD45+ cells and lymphocytes can be respectively purified from the skin or depleted from the dLN by magnetic bead facilitating cell sorting. Since most of the cells isolated from the dLN are CD45+, the use of anti-CD45 is not mandatory. Other markers can be included to identify myeloid cell subpopulations of interest by positive or negative-gating strategy. In this protocol, the myeloid cells recruited in the dLN were enriched by excluding CD8α+ cells (the whole T cell compartment can be targeted by using anti-CD3 specific antibody).
Incubate 30 min at 4 °C in the dark. Add 500 μl 1x DPBS + 2% FBS + 2 mM EDTA, centrifuge the sample 5 min at 450 x g at 4 °C and discard the supernatant. Repeat the wash step twice.
Resuspend the samples with 300 μl 1x DPBS + 2% FBS + 2 mM EDTA. Transfer the entire volume in a FACS tube through a 35 µm cell strainer. Rinse the filter with 100 μl 1x DPBS + 2% FBS + 2 mM EDTA.
Run the stained cells in a flow cytometer. Gate live single cells (DAPI-,FSC-W) to exclude dead cells and doublets. Plot CD45+CD11b+ events for the skin (Figure 6A) and (CD45+)CD8α-CD11b+ events for the dLN (Figure 6B).
Representative Results
We recently demonstrated that needle-syringe injection of immunizing doses of P. berghei sporozoites in the mouse skin induces a successive recruitment of polymorphonuclear neutrophils followed by inflammatory monocytes in the skin and dLN19. The Protocol Section described above details the procedure used to successfully isolate live myeloid cells from both tissues following multiple injections of large number of sporozoites in the ear dermis (Figures 1 and 2). Within the first 24 hr, the dLN (Figure 3) and the skin injection site (Figure 4) were isolated and processed as summarized in Figure 5 to analyse the cellular infiltration by multi-parametric flow cytometry. Overall, this technique allowed us to isolate an average 104 CD45+CD11b+ and 2.104 CD11b+ live single cells for the skin and dLN respectively. The acceptable viability of non-debris single cells ranged from 40-70% for the skin and 70-90% for the dLN. As shown in Figure 6, the frequency of myeloid cells in the skin (CD45+CD11b+) and the dLN (CD8α-CD11b+) strongly increases following intradermal injection of RAS compared with non-infected mice.
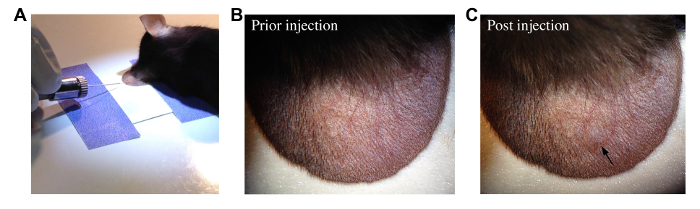 Figure 1: Intradermal Injection of Sporozoites into the Ear of Mouse. (A) Image showing intradermal injection of sporozoites in the ear pinna of an anesthetized mouse. The ventral side of the ear is stabilized with clear tape previously placed under a dissecting microscope. The needle is carefully inserted on the dorsal side of the ear, beneath the epidermis, with the bevel up. (B-C) Pictures showing the dorsal side of the ear pinna prior (B) and after (C) intradermal injection of 0.1-0.2 μl of parasite suspension. A characteristic papule (black arrow) is observable at the injection site at the end of the operation. Please click here to view a larger version of this figure.
Figure 1: Intradermal Injection of Sporozoites into the Ear of Mouse. (A) Image showing intradermal injection of sporozoites in the ear pinna of an anesthetized mouse. The ventral side of the ear is stabilized with clear tape previously placed under a dissecting microscope. The needle is carefully inserted on the dorsal side of the ear, beneath the epidermis, with the bevel up. (B-C) Pictures showing the dorsal side of the ear pinna prior (B) and after (C) intradermal injection of 0.1-0.2 μl of parasite suspension. A characteristic papule (black arrow) is observable at the injection site at the end of the operation. Please click here to view a larger version of this figure.
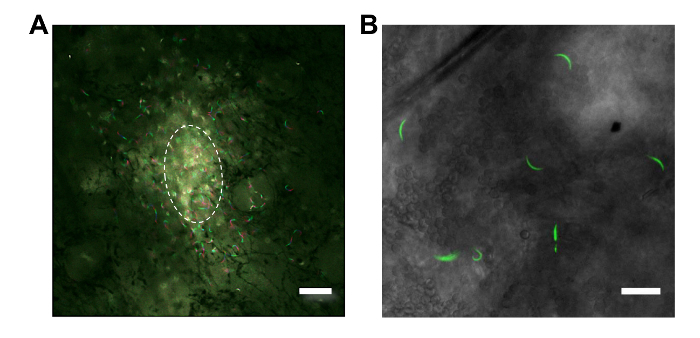 Figure 2: Imaging of Sporozoites Deposited in the Ear Dermis of Mouse. (A) Fluorescence microscopy showing RAS migrating from the injection site (indicated by the dashed lines) in the mouse skin 15 min post-injection (Scale bar = 60 μm; 10X magnification). The path of sporozoites is represented by the maximum intensity projection of the fluorescent signal. Green and red fluorescence respectively show parasite position in the skin at the beginning and after 10 sec of acquisition. (B) Higher magnification of RAS (green) injected in the skin (Scale bar = 20 μm; 25X magnification). Please click here to view a larger version of this figure.
Figure 2: Imaging of Sporozoites Deposited in the Ear Dermis of Mouse. (A) Fluorescence microscopy showing RAS migrating from the injection site (indicated by the dashed lines) in the mouse skin 15 min post-injection (Scale bar = 60 μm; 10X magnification). The path of sporozoites is represented by the maximum intensity projection of the fluorescent signal. Green and red fluorescence respectively show parasite position in the skin at the beginning and after 10 sec of acquisition. (B) Higher magnification of RAS (green) injected in the skin (Scale bar = 20 μm; 25X magnification). Please click here to view a larger version of this figure.
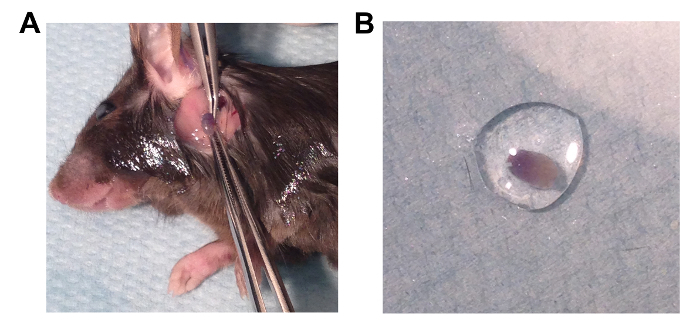 Figure 3: Draining Lymph Node Processing. (A) Picture showing the dissection of the proximal auricular dLN following intradermal injection of Evans blue for demonstration purposes. After cervical dislocation of the mouse, the neck is disinfected with 70% ethanol. A first incision is made in the jugular-carotid area with sharp scissors and the skin is removed from the operating field. The incision is stretched with 2 forceps to expose the dLN that appears grayish compared to the surrounding tissue. The connective tissues are then carefully pinched with forceps on the top of the dLN and progressively separated from it. Finally, the dLN is extracted by placing a forceps underneath the lymphoid tissue. (B) Picture showing the extracted dLN in a drop of PBS. Please click here to view a larger version of this figure.
Figure 3: Draining Lymph Node Processing. (A) Picture showing the dissection of the proximal auricular dLN following intradermal injection of Evans blue for demonstration purposes. After cervical dislocation of the mouse, the neck is disinfected with 70% ethanol. A first incision is made in the jugular-carotid area with sharp scissors and the skin is removed from the operating field. The incision is stretched with 2 forceps to expose the dLN that appears grayish compared to the surrounding tissue. The connective tissues are then carefully pinched with forceps on the top of the dLN and progressively separated from it. Finally, the dLN is extracted by placing a forceps underneath the lymphoid tissue. (B) Picture showing the extracted dLN in a drop of PBS. Please click here to view a larger version of this figure.
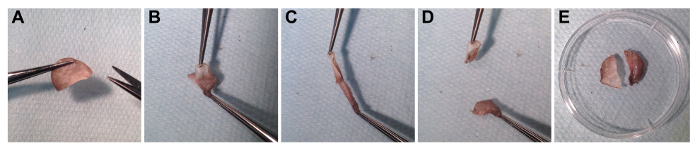 Figure 4: Ear Skin Processing. Pictures showing the successive steps to process the inoculated ear. (A) After cervical dislocation of the mouse, the ear is disinfected with 70% ethanol and removed using sterile sharp scissors and forceps. (B-D) The dorsal and ventral aspects of the ear are lightly separated by pinching and spacing apart the cut ends with two forceps. (E) Picture showing the dorsal and ventral aspects of the ear prior enzymatic treatment. Please click here to view a larger version of this figure.
Figure 4: Ear Skin Processing. Pictures showing the successive steps to process the inoculated ear. (A) After cervical dislocation of the mouse, the ear is disinfected with 70% ethanol and removed using sterile sharp scissors and forceps. (B-D) The dorsal and ventral aspects of the ear are lightly separated by pinching and spacing apart the cut ends with two forceps. (E) Picture showing the dorsal and ventral aspects of the ear prior enzymatic treatment. Please click here to view a larger version of this figure.
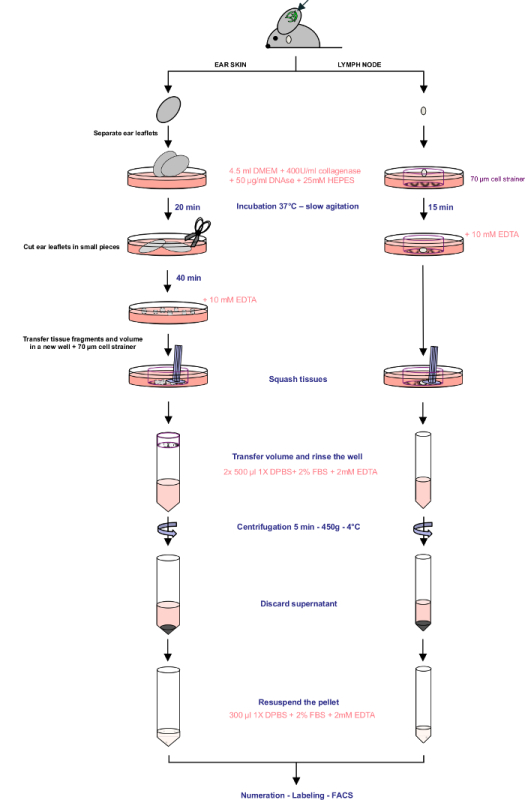 Figure 5: Protocol Summary. Schematic representation of the key steps to isolate total cells from the skin and dLN tissues. Please click here to view a larger version of this figure.
Figure 5: Protocol Summary. Schematic representation of the key steps to isolate total cells from the skin and dLN tissues. Please click here to view a larger version of this figure.
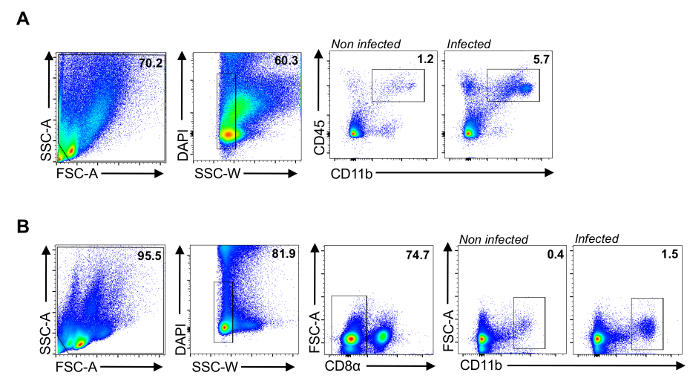 Figure 6: Myeloid Cell Population Isolated From the Ear Skin and the Proximal dLN. Representative FACS plots showing the gating strategy to analyse the myeloid compartment in the skin (A) and the dLN (B). CD45+CD11b+ and CD8α-CD11b+ cells were gated on total live singlet events for the skin and dLN respectively. For each condition, 5 x 105 total events were acquired (2 ears and 2 dLN pooled per sample). Please click here to view a larger version of this figure.
Figure 6: Myeloid Cell Population Isolated From the Ear Skin and the Proximal dLN. Representative FACS plots showing the gating strategy to analyse the myeloid compartment in the skin (A) and the dLN (B). CD45+CD11b+ and CD8α-CD11b+ cells were gated on total live singlet events for the skin and dLN respectively. For each condition, 5 x 105 total events were acquired (2 ears and 2 dLN pooled per sample). Please click here to view a larger version of this figure.
Discussion
In the perspective of large-scale vaccination of humans using a whole sporozoite malaria vaccine, one of the main challenges to overcome is to develop optimized routes and methods of parasite administration to ensure successful immunization and protection24,25. In humans, the evaluation of protective efficacy mediated by live attenuated parasites (LAP) has been performed following natural mosquito bites2, as well as intradermal, subcutaneous25,26 and IV immunizations27. As reported in rodents28 and non-human primates25, IV administration of LAP induces stronger protective immune responses compared to the above-mentioned routes. Nevertheless, non-IV routes of administration using needle and syringe still remains more suitable for human mass vaccination and efforts are currently being made to optimize their protective efficacy.
Recent studies conducted in mice demonstrated, especially in the case of the ID route, that the deposition of a small volume of sporozoite suspension (range of 1 µl) in multiple injection sites (4 points) significantly increased parasite infectivity compared to a single inoculation of parasites diluted in larger volumes (50 µl)24. In our experimental system (C57BL/6 mouse - P. berghei), complete protection was achieved after multiple injections in the ear dermis of highly concentrated suspension of parasites (50,000 RAS in 0.6 µl, 4 injection sites)19. In this context, we established the protocol described above to analyze more precisely the local host immune response to immunizing doses of RAS that allowed us to identify 2 major myeloid cell subsets recruited in the skin and dLN in response to the parasite19.
Multi-parametric flow cytometry allows accurate identification and quantification of immune cell changes in the context of host response to infection19,20. Isolation of large number of viable cells is therefore critical to perform reproducible phenotypic analysis. For this purpose, the enzyme concentration and the duration of tissue digestion must be optimized. Indeed, low concentration of enzymes or insufficient incubation time may lead to incomplete digestion with low yield of cells while prolonged tissue digestion may result in decrease cell viability and alteration of cell surface antigen expression29. Nevertheless, well-established protocols using collagenase treatment have been shown to have marginal impact on the detectability of relevant surface molecules frequently used for phenotypic analyses30.
Among the several parameters that can optimize the quality of cell isolation, the separation of the dorsal and ventral sections of the ear skin is essential, since it allows the collagenase/DNAse to access the dermis. In addition, mincing the skin into small pieces increases the surface area accessible to the enzymes, therefore allowing shorter duration of digestion. Finally, the use of mechanical dissociation helps to increase the yield in cell number for both the skin and dLN. However, excessive dissociation can cause additional stress that could negatively impact cell viability.
We favoured acquisition of live cells since fixation leads to suboptimal staining, complicating distinction of rare positive events of interest (data not shown). Moreover, the discrimination of dead cells was more problematic. In cases where cell fixation is required, we would suggest the use of LIVE/DEAD fixable dead cell stains.
Using the defined protocol, we successfully isolated myeloid cells infiltrating into the skin and dLN in response to parasite injection (Figure 6A and B). We usually obtain higher levels of viable single cells from the dLN (70-90%) compared to the skin (40-70%). This difference can be explained by the longer incubation time needed for efficient enzymatic digestion together with additional steps of mechanical dissociation to isolate skin cells (skin layer separation, mincing and stronger mashing).
Finally, an important parameter to take into account when analysing the host response to ID injection of sporozoites is the level of inflammation induced by both needle insertion and mosquito salivary gland extract deposition in the skin19,20. We therefore suggest to inject additional mice with either 1x PBS alone or salivary gland extracts from the same number of non-infected mosquitoes to evaluate the immune response specifically induced by the parasite. Altogether, we advise to dissect infected mosquitoes with high parasite load in the salivary glands and to filter the parasite suspension to limit the amount of mosquito material that could be deposited in the skin.
In summary, the isolation of myeloid cells from the skin and dLN through the described protocol provides a reliable assay to assess dynamic cellular changes during inflammatory response to Plasmodium infection and can be extended to other pathogens transmitted into the skin of the host.
Disclosures
The authors declare that they have no competing financial interests.
Acknowledgments
The authors thank Patricia Baldacci, Vanessa Lagal and Sabine Thiberge for critical reading, Irina Dobrescu and Sabine Thiberge for help in taking pictures and Pauline Formaglio for teaching in vivo imaging of sporozoite motility in the mouse skin. We also would like to thank Marek Szatanik and the Center for Production and Infection of Anopheles (CEPIA-Institut Pasteur) for mosquito rearing. This study was supported by the AXA Research Fund and funds from the Laboratoire d’Excellence “Integrative Biology of Emerging Infectious Diseases” (grant no. ANR-10-LABX-62-IBEID).
References
- Nussenzweig RS, Vanderberg J, Most H, Orton C. Protective immunity produced by the injection of x-irradiated sporozoites of plasmodium berghei. Nature. 1967;216(5111):160–162. doi: 10.1038/216160a0. [DOI] [PubMed] [Google Scholar]
- Hoffman SL, et al. Protection of humans against malaria by immunization with radiation-attenuated Plasmodium falciparum sporozoites. J Infect Dis. 2002;185(8):1155–1164. doi: 10.1086/339409. [DOI] [PubMed] [Google Scholar]
- Mueller AK, et al. Plasmodium liver stage developmental arrest by depletion of a protein at the parasite-host interface. Proc Natl Acad Sci U S A. 2005;102(8):3022–3027. doi: 10.1073/pnas.0408442102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller AK, Deckert M, Heiss K, Goetz K, Matuschewski K, Schlüter D. Genetically attenuated Plasmodium berghei liver stages persist and elicit sterile protection primarily via CD8 T cells. Am J Pathol. 2007;171(1):107–115. doi: 10.2353/ajpath.2007.060792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarun AS, et al. Protracted sterile protection with Plasmodium yoelii pre-erythrocytic genetically attenuated parasite malaria vaccines is independent of significant liver-stage persistence and is mediated by CD8+ T cells. J Infect Dis. 2007;196(4):608–616. doi: 10.1086/519742. [DOI] [PubMed] [Google Scholar]
- van Dijk MR, et al. Genetically attenuated, P36p-deficient malarial sporozoites induce protective immunity and apoptosis of infected liver cells. Proc Natl Acad Sci U S A. 2005;102(34):12194–12199. doi: 10.1073/pnas.0500925102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler NS, Schmidt NW, Vaughan AM, Aly AS, Kappe SH, Harty JT. Superior antimalarial immunity after vaccination with late liver stage-arresting genetically attenuated parasites. Cell Host Microbe. 2011;9(6):451–462. doi: 10.1016/j.chom.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belnoue E, et al. Protective T cell immunity against malaria liver stage after vaccination with live sporozoites under chloroquine treatment. J Immunol. 2004;172(4):2487–2495. doi: 10.4049/jimmunol.172.4.2487. [DOI] [PubMed] [Google Scholar]
- Behet MC, et al. Sporozoite immunization of human volunteers under chemoprophylaxis induces functional antibodies against pre-erythrocytic stages of Plasmodium falciparum. Malar J. 2014;13:136. doi: 10.1186/1475-2875-13-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amino R, et al. Quantitative imaging of Plasmodium transmission from mosquito to mammal. Nat Med. 2006;12(2):220–224. doi: 10.1038/nm1350. [DOI] [PubMed] [Google Scholar]
- Yamauchi LM, Coppi A, Snounou G, Sinnis P. Plasmodium sporozoites trickle out of the injection site. Cell Microbiol. 2007;9(5):1215–1222. doi: 10.1111/j.1462-5822.2006.00861.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gueirard P, et al. Development of the malaria parasite in the skin of the mammalian host. Proc Natl Acad Sci U S A. 2010;107(43):18640–18645. doi: 10.1073/pnas.1009346107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voza T, Miller JL, Kappe SH, Sinnis P. Extrahepatic exo- erythrocytic forms of rodent malaria parasites at the site of inoculation: clearance after immunization, susceptibility to primaquine, and contribution to blood-stage infection. Infect Immun. 2012;80(6):2158–2164. doi: 10.1128/IAI.00246-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakravarty S, Cockburn IA, Kuk S, Overstreet MG, Sacci JB, Zavala F, editors. CD8+ T lymphocytes protective against malaria liver stages are primed in skin-draining lymph nodes. Nat Med. 2007;13(9) doi: 10.1038/nm1628. [DOI] [PubMed] [Google Scholar]
- Obeid M, et al. Skin-draining lymph node priming is sufficient to induce sterile immunity against pre-erythrocytic malaria. EMBO Mol Med. 2013;5(2):250–263. doi: 10.1002/emmm.201201677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amino R, et al. Host cell traversal is important for progression of the malaria parasite through the dermis to the liver. Cell Host Microbe. 2008;3(2):88–96. doi: 10.1016/j.chom.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Radtke AJ, et al. Lymph-node resident CD8α+ dendritic cells capture antigens from migratory malaria sporozoites and induce CD8+ T cell responses. PLoS Pathog. 2015;11(2):e1004637. doi: 10.1371/journal.ppat.1004637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva HB, et al. Early skin immunological disturbance after Plasmodium-infected mosquito bites. Cell Immunol. 2012;277(1-2):22–32. doi: 10.1016/j.cellimm.2012.06.003. [DOI] [PubMed] [Google Scholar]
- Mac-Daniel L, et al. Local immune response to injection of Plasmodium sporozoites into the skin. J Immunol. 2014;193(3):1246–1257. doi: 10.4049/jimmunol.1302669. [DOI] [PubMed] [Google Scholar]
- Ribeiro-Gomes FL, Peters NC, Debrabant A, Sacks DL. Efficient capture of infected neutrophils by dendritic cells in the skin inhibits the early anti-leishmania response. PLoS Pathog. 2012;8(2):e1002536. doi: 10.1371/journal.ppat.1002536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiberge S, et al. In vivo. imaging of malaria parasites in the murine liver. Nat Protoc. 2007;2(7):1811–1818. doi: 10.1038/nprot.2007.257. [DOI] [PubMed] [Google Scholar]
- Ishino T, Orito Y, Chinzei Y, Yuda M. A calcium-dependent protein kinase regulates Plasmodium ookinete access to the midgut epithelial cell. Mol Microbiol. 2006;59(4):1175–1184. doi: 10.1111/j.1365-2958.2005.05014.x. [DOI] [PubMed] [Google Scholar]
- Amino R, et al. Imaging malaria sporozoites in the dermis of the mammalian host. Nat Protoc. 2007;2(7):1705–1712. doi: 10.1038/nprot.2007.120. [DOI] [PubMed] [Google Scholar]
- Ploemen IH, et al. Plasmodium liver load following parenteral sporozoite administration in rodents. Vaccine. 2013;31(34):3410–3416. doi: 10.1016/j.vaccine.2012.09.080. [DOI] [PubMed] [Google Scholar]
- Epstein JE, et al. Live attenuated malaria vaccine designed to protect through hepatic CD8 T cell immunity. Science. 2011;334(6055):475–480. doi: 10.1126/science.1211548. [DOI] [PubMed] [Google Scholar]
- Roestenberg M, et al. Long-term protection against malaria after experimental sporozoite inoculation: an open-label follow-up study. Lancet. 2011;377(9779):1770–1776. doi: 10.1016/S0140-6736(11)60360-7. [DOI] [PubMed] [Google Scholar]
- Seder RA, et al. Protection against malaria by intravenous immunization with a nonreplicating sporozoite vaccine. Science. 2013;341(6152):1359–1365. doi: 10.1126/science.1241800. [DOI] [PubMed] [Google Scholar]
- Douradinha B, et al. Genetically attenuated P36p-deficient Plasmodium berghei sporozoites confer long-lasting and partial cross-species protection. Int J Parasitol. 2007;37(13):1511–1519. doi: 10.1016/j.ijpara.2007.05.005. [DOI] [PubMed] [Google Scholar]
- Geem D, Medina-Contreras O, Kim W, Huang CS, Denning TL. Isolation and Characterization of Dendritic Cells and Macrophages from the Mouse Intestine. J Vis Exp. 2012. p. e4040. [DOI] [PMC free article] [PubMed]
- Autengruber A, Gereke M, Hansen G, Hennig C, Bruder D. Impact of enzymatic tissue disintegration on the level of surface molecule expression and immune cell function. Eur J Microbiol Immunol (Bp. 2012;2(2):112–120. doi: 10.1556/EuJMI.2.2012.2.3. [DOI] [PMC free article] [PubMed] [Google Scholar]


