Abstract
Purpose
Decision-making by dental and medical experts can be influenced by their biases, interests, and experiences, and academic arguments about controversial issues may additionally be considered indirect experiences capable of affecting decision-making. This study reports on the use of interactive communication devices to evaluate preferences and flexibility in decision-making among dental care providers who attended two distinct academic conferences.
Methods
Two debates were presented by a team of two lecturers at two academic conferences (focusing on periodontology and implant dentistry, respectively) and the audience members of each session were surveyed. Before each lecture, two case modules about the diagnosis and treatment of multirooted molar lesions were provided, and interactive communication devices were used to collect responses about decision-making preferences in treatment planning immediately before and after a debate about treatment strategies.
Results
In total, 81 and 84 completed answers from both conferences were obtained for the first and second case modules, respectively. The preferred treatment plan differed significantly according to the focus of the conference, and a tendency emerged for the clinicians participating in each conference to express uniform preferences. However, attending the debates resulted in significant changes in decision-making preferences regardless of the conference focus or the characteristics of the participants.
Conclusions
Our findings suggest that providing continuing education via debates on controversial issues may be effective in widening conceptual knowledge and reducing biases among experts in the dental and medical fields.
Keywords: Clinical protocols, Continuing dental education, Decision making, Dental implants, Periodontics
Graphical Abstract
INTRODUCTION
Periodontitis is one of the most frequent reasons for tooth extraction, and both conventional prosthetic procedures and therapy involving dental implants therapy should be performed based on the periodontal treatment status and/or the prognosis of the diseased teeth. However, evaluating the prognosis and determining whether a tooth can be saved requires an evaluation of several factors, including the level of bone loss, tooth mobility, self-control of oral hygiene, genetic factors, and compliance with supportive periodontal treatment [1]. Several clinicians have developed decision trees for periodontally compromised teeth, but no clear criteria exist for decision-making or classification [1,2,3]. Especially in the posterior dentition, periodontally compromised and furcation-involved molars were found to be 2.54 times more likely to be lost during the maintenance period relative to teeth without furcation involvement [4].
The use of dental implants has changed treatment strategies in both contemporary prosthodontics and periodontics. Several researchers have recommended choosing dental implants rather than periodontal or endodontic treatment for severely compromised teeth, because the use of dental implants has been associated with high survival and success rates [5], lower technique sensitivity [6], and better cost-effectiveness [7] compared to traditional treatments. However, recent systematic reviews have identified higher complication rates in dental implantation, with the authors favoring periodontal and endodontic treatment strategies for saving teeth [8,9]. Nevertheless, in many cases encountered by dental clinicians, it is unclear whether the tooth should be extracted or saved due to uncertainty about the prognosis and the various factors that influence the outcomes of conventional and conservative treatments.
Technique sensitivity, which refers to the presence of a wide variety in clinical results among clinicians, can also result in general practitioners or specialists other than periodontal specialists preferring the simplest methodology for producing a predicted result regardless of their clinical expertise, such as in the use of dental implants [6]. In addition, periodontal specialists have various preferences regarding the use of nonsurgical, surgical, resective, and regenerative approaches according to their clinical philosophies and experiences. This situation means that it is important for clinicians to share their clinical experiences and debate scientific issues in order to broaden their base of insights and to ensure the emergence of an evidence-based consensus regarding clinical decisions. However, individual experiences and characteristics may limit each clinician’s scope of thinking and promote inflexibility about concepts that others advocate.
The present study used interactive communication devices to evaluate preferences and flexibility in decision-making among dental care providers who attended two distinct academic conferences.
MATERIALS AND METHODS
Study design
Two debates, each lasting 60 minutes, based on specific case modules were presented at two academic conferences focusing on periodontology (the General Session of the Korean Academy of Periodontology in October 2012) and implant dentistry (the ITI First Korea Forum day in April 2013). In a session entitled ‘Debate on strategies and tactics for the treatment of multirooted teeth,’ two lecturers (J.S.L. and M.S.K.) attempted to persuade the audiences to adopt opposite positions about two case modules (extraction and periodontal therapy). The audiences attending this session at each conference comprised 70 to 100 participants, who were each given a wireless remote electric device (Cricket, Interwrite Learning, Columbia, MD, USA) for real-time voting and automatic counting based on a prepared questionnaire. After using the devices to collect the characteristics of the audiences, information including clinical photographs and radiographs was provided to the audience of each module. Preferences about the treatment plans were collected from the audience before and after the debates.
Case modules
Case 1
A 48-year-old female patient without any systemic disease presented with a complaint of mobility of the lower right molars. Decementation of the crown on the first molar and tooth mobility (less than 1 mm) with the formation of a deep periodontal pocket (10–12 mm) on the mesial side of the second molar were identified (Figure 1). In radiographic and further clinical examinations, advanced root dental caries was detected on the mesial root of the first molar. A large area of radiolucency was found around the mesial root of the second molar, extending to the apical area, but positive tooth vitality was found in ice and electronic pulp tests.
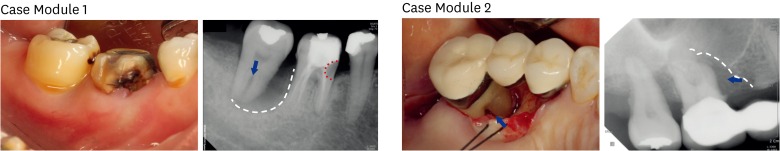
Figure 1.
Clinical and radiographic photographs associated with the first and second case modules. In the first case, subgingival dental caries was observed on the mesiobuccal aspect of the first molar, and a deep periodontal pocket (10–12 mm) was detected on the mesial side of the second molar by clinical probing. Radiographic imaging revealed a radiolucent caries lesion extending to the mesial root canal of the first molar (red dotted line) and an extensive bony lesion including to the furcal (arrow) and apical areas of the second molar (white dotted line). In the second case, extensive bony destruction on the mesial side of the first molar was found clinically and radiographically (white dotted line) with involvement of the mesial furcation (arrows).
One lecturer recommended extracting both teeth due to the aforementioned advantages of dental implants, namely, reliably high long-term survival rates and lower technique sensitivity. Another lecturer suggested periodontal treatment (root resection for the first molar and regenerative periodontal treatment for the second molar) due to the importance of patient-centered decision-making, the requirement for scientific evidence supporting each periodontal treatment intervention, and the high risk of complications such as peri-implantitis or screw or fixture fracture.
Case 2
A 53-year-old female patient presented with a deep periodontal pocket (probing depth, 9 mm) in the mesial area of the right maxillary second molar, with mesial furcation involvement. Minimal tooth mobility was present (within the normal range) and positive pulp vitality was observed using the ice test. A radiographic examination revealed extensive alveolar bone destruction on the mesial side, but no other furcation involvement was found clinically via bone sounding using a periodontal probe under local anesthesia. The elevation of a mucoperiosteal flap revealed a severely exposed palatal and mesiobuccal root (10 mm from the cementoenamel junction) around the mesial furcation (Figure 1).
The first lecturer criticized the use of regenerative periodontal treatment as an unrealistic regimen, based on scientific literature showing this treatment to be unreliable, leading to only a limited enhancement of clinical parameters, and having a risk of complications such as infection or membrane exposure. In cases of regenerative periodontal treatment with incomplete results, a periodontal pocket with a long junctional epithelium could remain as a risk factor. His final recommendation was not to use a regenerative periodontal approach, but instead to use dental implants due to their high reliability. The other lecturer provided a counterargument based on the fact that many studies have reported regenerative periodontal therapy to be reliable and realistic. He suggested that correctly identifying the indications for this treatment strategy is the most important factor for clinical success, using the example of choosing between class II and class III furcation involvement. His final recommendation was regenerative periodontal treatment (application of enamel matrix derivatives with bone graft biomaterials) based on clinical results reported in the literature.
Design of the questionnaire
In order to obtain basic information about the participants, a questionnaire was completed by audience members before presenting the case modules. This questionnaire included items about their gender, age, specialization, duration of clinical experience, and whether they were competent in advanced periodontal and implant surgery. The two case modules involved making a choice between performing dental implantation after tooth extraction or periodontal treatment intended to save the tooth. The preferences of the participants were collected for the first and second molars separately, as well as before and after they attended the debating lectures.
Statistical analysis
After collecting responses from the audience members, only data with no blank responses to the questions about treatment preferences were included for each case module. In cases where the data included all responses to the case module questions but not the basic information, the responses to the case module questions were included in the statistical analyses. The Pearson χ2 test was used to analyze the effects of each characteristic (expressed as a categorical value) on each participant’s treatment preference and flexibility in decision-making. SPSS version 21 (IBM Corp., Armonk, NY, USA) was used for all statistical analyses, with a cutoff for statistical significance of P<0.05.
RESULTS
Characteristics of the participants
Data from 81 and 84 participants for the first and second case modules, respectively, were used in the statistical analyses. All participants were provided with interactive devices, but data that included blank responses for decision preferences in each module were excluded. Of particular note, fewer data were available from the participants in the periodontal conference because they were permitted to stop participating during the lecture.
The characteristics of the participants are presented in Table 1, and the participants were classified into two categories for the chi-square test as follows: conference focus (periodontology or implant dentistry), gender (male or female), age (under or over 45 years), specialization (periodontist or other), clinical experience (under or over 10 years), and level of competence or expertise (in periodontal treatment and implant therapy). For competency, resective and regenerative periodontal operations were considered to represent complicated periodontal therapy, and the clinical experience level in implant dentistry was classified according the number of operations (with a cutoff of 50 surgical procedures).
Table 1. Demographic and clinical practice-related characteristics of the participants.
| Characteristics of participants | Case I | Case II | ||
|---|---|---|---|---|
| Total number of participants who responded | 81 | 84 | ||
| Conference | Periodontal conference | 34 | 32 | |
| Implant conference | 47 | 52 | ||
| Gender | Male | 46 | 48 | |
| Female | 21 | 20 | ||
| Total responses to the gender question | 67 | 68 | ||
| Age | Under 45 yr | 47 | 47 | |
| Over 45 yr | 9 | 10 | ||
| Total responses to the age question | 56 | 57 | ||
| Specialization | Periodontology | 32 | 29 | |
| Non-periodontology | 38 | 41 | ||
| Total responses to the specialization question | 70 | 70 | ||
| Experiences related to clinical practice | Clinical experience | Under 10 years | 46 | 45 |
| Over 10 years | 29 | 30 | ||
| Total responses to the question about clinical experience | 75 | 75 | ||
| Periodontal therapy | Simple | 23 | 24 | |
| Complicated | 50 | 51 | ||
| Total responses to the question about periodontal therapy | 73 | 75 | ||
| Dental implant therapy | Fewer than 50 cases | 36 | 38 | |
| More than 50 cases | 33 | 32 | ||
| Total responses to dental implant therapy | 69 | 70 | ||
Preferences in decision-making about periodontally compromised teeth
The first case module included two distinct issues related to two different teeth: a dental implant versus resective and regenerative periodontal therapy on the first (#46) and second (#47) molars, respectively. However, similar proportions of participants preferred tooth extraction and implantation (65.43% and 62.96% for #46 and #47, respectively) rather than periodontal treatment (34.57% and 37.04%, respectively). The chi-square test demonstrated that participants choosing dental implants or periodontal therapy for one tooth chose the same category of treatment for the other tooth (P<0.001) within the first case module. Table 2 lists the preferences for periodontal treatment according to the characteristics of the participants. For the tooth (#46) that presented the issue of resective periodontal therapy, participants in the two different conferences showed significantly different preferences for periodontal treatment, tooth extraction, or implantation (P<0.001), whereas their preferences were similar for the other tooth (#47) for all participants. In addition, periodontal specialists showed a significantly greater preference for resective periodontal therapy than practitioners with other specializations (P=0.003; Case 1 #46 in Table 2).
Table 2. Proportions (%) of preferences regarding periodontal treatment before the debate (frequency/number of responses).
| Characteristics of participants | Case I | Case II | |||
|---|---|---|---|---|---|
| #46 | #47 | ||||
| Total number of participants who responded | 34.57 | 37.04 | 57.14 | ||
| Conference | Periodontal conference | 58.82 (20/34)a) | 35.29 (12/34) | 83.87 (26/31)a) | |
| Implant conference | 17.02 (8/47)a) | 38.30 (18/47) | 42.31 (22/52)a) | ||
| P-value | <0.001a) | 0.78 | <0.001a) | ||
| Gender | Male | 30.43 (14/46) | 34.78 (16/46) | 54.17 (26/48) | |
| Female | 47.62 (10/21) | 47.62 (10/21) | 63.16 (12/19) | ||
| P-value | 0.34 | 0.46 | 0.73 | ||
| Age | Under 45 yr | 34.04 (16/47) | 36.17 (17/47) | 51.06 (24/47) | |
| Over 45 yr | 55.56 (5/9) | 66.67 (6/9) | 90.00 (9/10) | ||
| P-value | 0.33 | 0.12 | 0.08 | ||
| Specialization | Periodontology | 40.63 (13/32)a) | 37.50 (12/32) | 62.07 (18/29) | |
| Non-periodontology | 18.42 (7/38)a) | 28.95 (11/38) | 55.00 (22/40) | ||
| P-value | 0.003a) | 0.11 | 0.84 | ||
| Experiences related to clinical practice | Clinical experience | Under 10 yr | 34.78 (16/46) | 39.13 (18/46) | 54.54 (24/22) |
| Over 10 yr | 31.03 (9/29) | 37.93 (11/29) | 63.33 (19/30) | ||
| P-value | 0.67 | 0.56 | 0.75 | ||
| Periodontal therapy | Simple | 30.43 (7/23) | 30.43 (7/23) | 69.57 (16/23) | |
| Complicated | 32.00 (16/50) | 38.00 (19/50) | 52.94 (27/51) | ||
| P-value | 0.21 | 0.60 | 0.40 | ||
| Dental implant therapy | Fewer than 50 cases | 38.89 (14/36) | 36.11 (13/36) | 51.35 (19/37)a) | |
| More than 50 cases | 30.30 (10/33) | 39.39 (13/33) | 75.00 (24/32)a) | ||
| P-value | 0.75 | 0.92 | 0.03a) | ||
a)Statistically significant difference.
The preference for periodontal therapy was higher in the second case module than in the first case module (57.14%; Table 2). The conference focus also significantly affected treatment preferences (P<0.001), and participants with more experience in the use of dental implants preferred periodontal therapy (P=0.026). Periodontal therapy tended to be preferred more by the older group (>45 years) than the younger group (90.00% and 51.06%, respectively), but this difference was not statistically significant (P=0.077), possibly due to the small sample size of the older group.
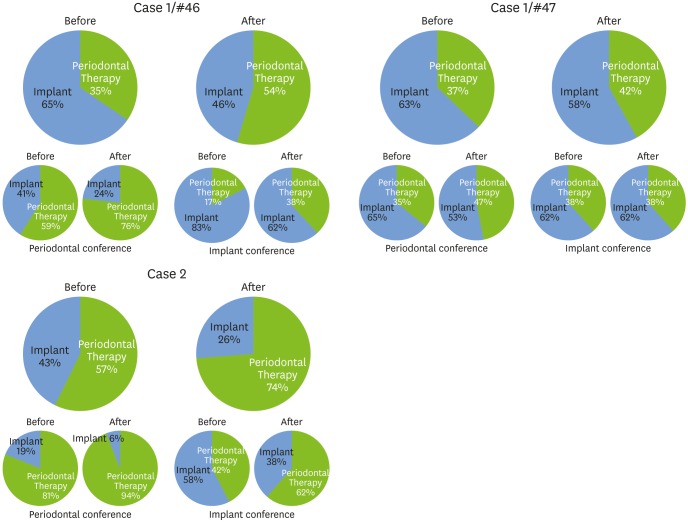
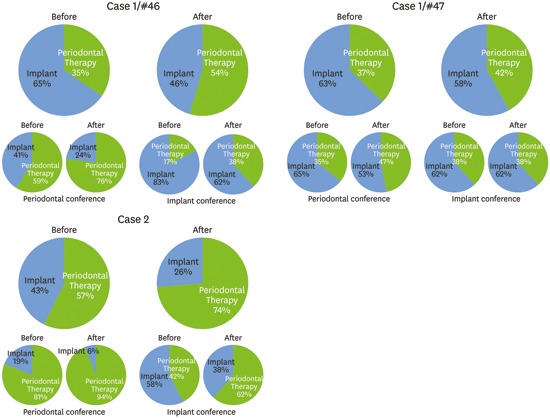
The preference for periodontal therapy increased in all cases after the lecture, regardless of the conference focus (Figure 2). This preference was also higher in the second case module than the first case module, which may have been due to the learning effects of the first module. However, the preference for periodontal therapy increased more after the lecture in the second case module (from 57% to 74%), and most of the participants (94%) in the periodontal conference chose periodontal therapy over dental implant therapy (6%).
Figure 2.
Preferences of the participating dental clinicians regarding treatment decisions for each multirooted tooth in the first and second case modules. The upper two circle graphs in each panel present the proportion of preferences for periodontal therapy (to save the tooth) or placement of a dental implant (after removing the tooth), immediately before and after the debates. The lower graphs show subcategorized results from the periodontal and implant conferences. A tendency was noted among the participants in the periodontal conference to prefer periodontal therapy over dental implants. The preference for periodontal therapy increased after the debates and was also greater in the second case than in the first case.
Effects of the debates on flexibility in decision-making
The results regarding flexibility in decision-making are presented in Table 3, which lists the proportions of participants who changed their decision after the debates. Approximately one-quarter (21%–26%) of participants changed their original treatment plan in the two case modules, but no characteristics of the participants demonstrated a statistically significant effect on flexibility in decision-making. Interestingly, in the second case, 16 of 36 participants choosing a dental implant showed flexibility, in contrast to only two of 48 participants choosing periodontal therapy who did so (P<0.001).
Table 3. Flexibility of decision-making in the treatment plan (%), as indicated by the proportion of participants who changed their initial decision after the debate.
| Characteristics of participants | Case I | Case II | ||
|---|---|---|---|---|
| Total number of participants who responded | 25.93 | 21.43 | ||
| Conference | Periodontal conference | 32.35 | 12.50 | |
| Implant conference | 21.28 | 26.92 | ||
| Gender | Male | 19.57 | 27.08 | |
| Female | 38.10 | 15.00 | ||
| Age | Under 45 yr | 27.66 | 25.53 | |
| Over 45 yr | 33.33 | 10.00 | ||
| Specialization | Periodontology | 37.50 | 20.69 | |
| Non-periodontology | 15.79 | 21.95 | ||
| Experiences related to clinical practice | Clinical experiences | Under 10 yr | 28.26 | 24.44 |
| Over 10 yr | 20.69 | 16.67 | ||
| Periodontal therapy | Simple | 17.39 | 16.67 | |
| Complicated | 28.00 | 25.49 | ||
| Dental implant therapy | Fewer than 50 cases | 22.22 | 26.32 | |
| More than 50 cases | 27.27 | 15.63 | ||
DISCUSSION
Decision-making by experts is influenced by their direct and indirect experiences [10]. Although conceptual knowledge, such as the classification or categorization of diseases and treatments, is fundamental in medical and dental education, perceptual knowledge reflecting, for example, one’s own practical experiences in diagnosis and treatment can modify or strengthen a domain of expertise. This means that only a range of consensus opinions can exist for decision-making by experts, rather than a unified solution. However, in a field with controversial issues, one-sided experiences can lead to biases, which can be reduced by sharing experiences and through communication among experts with distinct opinions in the same field [11,12].
The introduction of dental implants has made the decision between traditional treatment to save a tooth and implantation following tooth extraction into a major point of contention [13,14,15]. In the present results for both case modules, decisions between periodontal therapy and a dental implant appeared to be significantly affected by the focus of the conference and the training of the participants. The participants in the periodontal conference showed a tendency to prefer periodontal therapy, whereas an inclination toward dental implants was evident among the participants in the implant conference. Previous studies have likewise found that the experience and training of dentists affected decisions regarding dental treatment plans [16,17]. In addition, the participants in the present study choosing each category (dental implant or periodontal therapy) almost completely overlapped in their decision-making on the two other teeth of the first case module. These results suggest that a tendency exists for bias in decision-making by dental care providers to reflect their own interests and experience.
Even though participants’ area of training and the conference focus significantly affected the initial decision-making in this study, a large proportion of participants nonetheless changed their decision after the debate. The flexibility in decision-making in this study was not affected by any characteristics of the participants, even age or quantity of clinical experience. In general, more experience may be expected to facilitate inflexible thinking, due to the way it strengthens restrictions on one’s decision-making domain [18]. However, in this study, the older participants demonstrated flexibility in their decision-making based on information received in lectures, with no significant difference observed in this parameter relative to the younger group. This might be due to the development of perceptual knowledge through exposure to a large variety of clinical cases in dental and medical educational courses [10]. Dental and medical experts encounter a wide range of patients with completely different situations and responses in their everyday clinical practices, which might make them more open-minded to diverse possibilities in decision-making.
One particularly interesting finding was that all responses indicated a trend toward the increasing use of periodontal therapy, even though both approaches—dental implants and periodontal therapy—were presented in the debates for the same length of time. Dental implants produce more reliable and stable outcomes relative to periodontal therapy, which is associated with responses that may vary from clinical failure due to infection to successful periodontal regeneration [19,20]. Therefore, the information provided in lectures on dental implants may have fallen within the range of the expectations of the participants, whereas lectures on periodontal therapy may have broadened their domain of clinical experience, especially among participants who would normally initially choose dental implantation. Quantitatively, in the two conferences, 29.41% and 44.44% of participants who initially chose dental implants changed their choice to periodontal therapy, respectively (15/51 in case 1 and 16/36 in case 2), whereas 4.17% and 20.00% of participants in each conference who initially chose periodontal therapy changed their decision. Statistical analysis also revealed that the initial choice of participants significantly affected their flexibility in decision-making in the second case module (P<0.001).
The aim of the present study was to evaluate preferences and flexibility in decision-making, especially regarding the use of traditional periodontal therapy versus dental implantation. In the initial decision regarding treatment planning, most of the participants preferred dental implants. However, exposure to debates addressing this issue changed the initial decisions of many participants and increased the preference for periodontal therapy. Experience-related and interest-related characteristics of dentists (area of training and conference topic) affected their preferences regarding decision-making in treatment, but the effects of debates on flexibility in decision-making did not appear to be affected by the experiences or competencies of the participants.
A critical limitation of this study is that the survey reflected the preferences and reactions of participants in an imaginary clinical situation, which may have induced clinicians to take unrealistically rigid points of view potentially affected by the presentation skills of the lecturer. However, the two lecturers in this study deliberately presented alternating opinions in an alternating order with the goal of reducing bias stemming from this limitation. Despite these limitations of this study, it was clear that the debates modified the decisions made by the clinicians in all of the case modules. Therefore, providing continuing education via debates on controversial issues can be effective for widening conceptual knowledge and reducing biases among experts in dentistry and medicine.
ACKNOWLEDGEMENTS
This study was supported by the Basic Science Research Program of the National Research Foundation of Korea (NRF) funded by the Ministry of Education (No. NRF-2014R1A1A1A05002953).
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Nunn ME, Fan J, Su X, Levine RA, Lee HJ, McGuire MK. Development of prognostic indicators using classification and regression trees for survival. Periodontol 2000. 2012;58:134–142. doi: 10.1111/j.1600-0757.2011.00421.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Halperin-Sternfeld M, Levin L. Do we really know how to evaluate tooth prognosis? A systematic review and suggested approach. Quintessence Int. 2013;44:447–456. doi: 10.3290/j.qi.a29182. [DOI] [PubMed] [Google Scholar]
- 3.Avila G, Galindo-Moreno P, Soehren S, Misch CE, Morelli T, Wang HL. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009;80:476–491. doi: 10.1902/jop.2009.080454. [DOI] [PubMed] [Google Scholar]
- 4.Wang HL, Burgett FG, Shyr Y, Ramfjord S. The influence of molar furcation involvement and mobility on future clinical periodontal attachment loss. J Periodontol. 1994;65:25–29. doi: 10.1902/jop.1994.65.1.25. [DOI] [PubMed] [Google Scholar]
- 5.Thomas MV, Beagle JR. Evidence-based decision-making: implants versus natural teeth. Dent Clin North Am. 2006;50:451–461. doi: 10.1016/j.cden.2006.05.001. [viii.] [DOI] [PubMed] [Google Scholar]
- 6.Kinsel RP, Lamb RE, Ho D. The treatment dilemma of the furcated molar: root resection versus single-tooth implant restoration. A literature review. Int J Oral Maxillofac Implants. 1998;13:322–332. [PubMed] [Google Scholar]
- 7.Brägger U, Krenander P, Lang NP. Economic aspects of single-tooth replacement. Clin Oral Implants Res. 2005;16:335–341. doi: 10.1111/j.1600-0501.2005.01112.x. [DOI] [PubMed] [Google Scholar]
- 8.Holm-Pedersen P, Lang NP, Müller F. What are the longevities of teeth and oral implants? Clin Oral Implants Res. 2007;18(Suppl 3):15–19. doi: 10.1111/j.1600-0501.2007.01434.x. [DOI] [PubMed] [Google Scholar]
- 9.Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs) Clin Oral Implants Res. 2007;18(Suppl 3):97–113. doi: 10.1111/j.1600-0501.2007.01439.x. [DOI] [PubMed] [Google Scholar]
- 10.Hutton RJ, Klein G. Expert decision making. Syst Eng. 1999;2:32–45. [Google Scholar]
- 11.Milkman KL, Chugh D, Bazerman MH. How can decision making be improved? Perspect Psychol Sci. 2009;4:379–383. doi: 10.1111/j.1745-6924.2009.01142.x. [DOI] [PubMed] [Google Scholar]
- 12.Pommer B, Becker K, Arnhart C, Fabian F, Rathe F, Stigler RG. How meta-analytic evidence impacts clinical decision making in oral implantology: a Delphi opinion poll. Clin Oral Implants Res. 2016;27:282–287. doi: 10.1111/clr.12528. [DOI] [PubMed] [Google Scholar]
- 13.Brånemark PI, Adell R, Albrektsson T, Lekholm U, Lundkvist S, Rockler B. Osseointegrated titanium fixtures in the treatment of edentulousness. Biomaterials. 1983;4:25–28. doi: 10.1016/0142-9612(83)90065-0. [DOI] [PubMed] [Google Scholar]
- 14.Laney WR, Tolman DE, Keller EE, Desjardins RP, Van Roekel NB, Brånemark PI. Dental implants: tissue-integrated prosthesis utilizing the osseointegration concept. Mayo Clin Proc. 1986;61:91–97. doi: 10.1016/s0025-6196(12)65193-3. [DOI] [PubMed] [Google Scholar]
- 15.Wang G, Gao X, Lo EC. Public perceptions of dental implants: a qualitative study. J Dent. 2015;43:798–805. doi: 10.1016/j.jdent.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 16.Aminoshariae A, Teich S, Heima M, Kulild JC. The role of insurance and training in dental decision making. J Endod. 2014;40:1082–1086. doi: 10.1016/j.joen.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Lang-Hua BH, McGrath CP, Lo EC, Lang NP. Factors influencing treatment decision-making for maintaining or extracting compromised teeth. Clin Oral Implants Res. 2014;25:59–66. doi: 10.1111/clr.12142. [DOI] [PubMed] [Google Scholar]
- 18.Matzel LD, Light KR, Wass C, Colas-Zelin D, Denman-Brice A, Waddel AC, et al. Longitudinal attentional engagement rescues mice from age-related cognitive declines and cognitive inflexibility. Learn Mem. 2011;18:345–356. doi: 10.1101/lm.2034711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moshaverinia A, Kar K, Chee WW. Treatment planning decisions: implant placement versus preserving natural teeth. J Calif Dent Assoc. 2014;42:859–868. [PubMed] [Google Scholar]
- 20.Esposito M, Ardebili Y, Worthington HV. Interventions for replacing missing teeth: different types of dental implants. Cochrane Database Syst Rev. 2014;7:CD003815. doi: 10.1002/14651858.CD003815.pub4. [DOI] [PubMed] [Google Scholar]