Abstract
Background:
Text message interventions are feasible, preferable, and sometimes effective for youth with diabetes. However, few, if any studies, have examined the personalized use of text messages with youth repeatedly hospitalized for diabetic ketoacidosis (DKA) and their caregivers. This study characterizes the use of personalized text messages in Novel Interventions in Children’s Healthcare (NICH).
Methods:
Approximately 2 months of text messages sent to youth with repeat DKA and their caregivers were logged regarding the following text characteristics: (1) content, (2) intervention type, (3) timing, and (4) recipient characteristics.
Results:
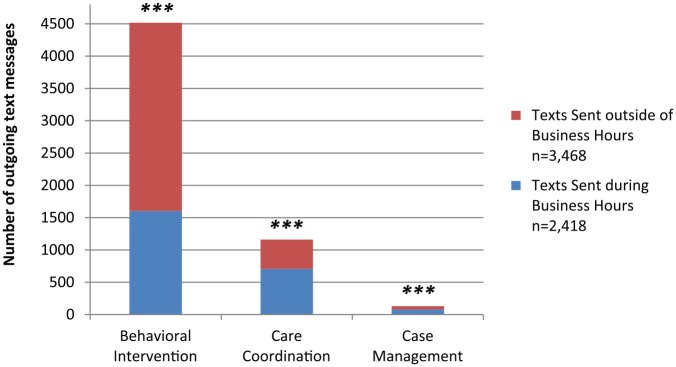
NICH interventionists sent 2.3 and 1.5 texts per day to patients and caregivers, respectively. Approximately 59% of outgoing texts occurred outside of typical business hours, and roughly 68% of texts contained some form of support and/or encouragement. The relation between type of intended intervention and day/time of text was significant, χ2(2, N = 5,808) = 266.93, P < .001. Interventionists were more likely to send behavioral intervention text messages outside of business hours, whereas they were more likely to send care coordination and case management text messages during business hours.
Conclusions:
To our knowledge, this is the first study to specifically categorize and describe the personalized use of text messages with youth repeatedly hospitalized for DKA and their caregivers. Findings indicate that a promising treatment program for these youth frequently used text interventions to deliver praise and encouragement to patients and caregivers alike, often outside of typical business hours, and tailored text content based on patient and caregiver characteristics.
Keywords: adolescence, mHealth, NICH, SMS, text message, type 1 diabetes
Suboptimal adherence is relatively common amongst patients with type 1 diabetes, with only 21% of pediatric patients in the United States estimated to achieve the International Society of Pediatric and Adolescent Diabetes target glycated hemoglobin.1,2 In particular, adolescents and emerging adults are especially vulnerable to the burden associated with diabetes management and are disproportionately at risk of suboptimal diabetes management.3,4 Unfortunately, such adherence difficulties are associated with increased risk of both acute and chronic medical problems, negative psychological outcomes, and increased health care costs.5-8
In addition to patient age, several demographic, psychosocial and environmental factors put a subset of youth with diabetes at greater risk for suboptimal adherence and associated negative outcomes.9 Specifically, adolescents and emerging adults of ethnic minority status,10,11 lower socioeconomic status,12,13 and with mental health problems (eg, depression and anxiety)14,15 are at increased risk for low adherence to treatment regimens and poorer glycemic control. Family factors (eg, high marital conflict, low family cohesion, low parental involvement in diabetes management) have also been identified as having negative implications for diabetes management and glycemic control.16-21 Patients with a combination of these risk factors may be particularly vulnerable.22-24
Behavioral interventions (eg, Wysocki et al,25 Harris et al26) are commonly used to improve adherence and glycemic control among youth with diabetes,27 and most are moderately successful.28 Traditionally, however, behavioral interventions for youth are office-based, constrained to a small temporal window, and are infrequent (ie, once per week or less), thereby limiting youth access to care delivered in their natural environment and at the time, frequency, and level of intensity that best matches their unique situation. Given that 75-90% of youth in the United States send and receive text messages regularly,29 mobile health strategies (eg, text interventions) may provide an opportunity to augment the effectiveness of and increase patient access to multicomponent behavioral interventions while allowing providers to deliver immediate feedback on clinically relevant behaviors as they occur within the relevant ecological environment. In addition, racial and socioeconomic differences in text messaging rates are decreasing, potentially making mobile technology a means to reach previously underserved populations.29
As noted in a recent review,30 numerous studies have evaluated the use of text messaging as an intervention component to improve pediatric diabetes management by targeting blood glucose monitoring,31-34 use of insulin,31,35 diabetes education,35 physical activity,36 and adherence barriers.37 With few exceptions, the vast majority of studies of text use, or short message service (SMS), do not predominantly focus on youth with poorly controlled diabetes and comorbid psychosocial vulnerability. In addition, studies which utilize “personalized” messages (not automated) do not typically include text content, intervention purpose, and message timing.32,35 Related to this, those studies often rely on a predetermined list of text selections, thereby limiting provider flexibility to adapt texts to best fit the individual and context. Moreover, our literature review identified only 1 previous study that involved caregivers in the text-messaging program.31 Overall, SMS findings suggest that text messaging interventions are both feasible and preferable for youth;30 however, there are few treatments that utilize personalized communications to enhance interventions and a limited understanding of the content and utility of such intervention components.
Novel Interventions in Children’s Healthcare (NICH)38 was developed for youth repeatedly hospitalized for diabetic ketoacidosis (DKA). NICH services involve intensive home- and community-based treatment for patients and their families to reduce barriers to disease management. Text messaging is used whenever possible to increase patient and family contact, provide immediate reinforcement for diabetes management, assist with on-the-fly problem solving, build rapport, and provide skills coaching. Although NICH has been associated with improvements in diabetes management (eg, decreased HbA1c, reduced frequency of DKA),38,39 the use of SMS interventions in this treatment model has yet to be characterized. To better understand how treatment programs might utilize personalized communications to intervene with vulnerable populations, this study examined the manner in which text messages were used in NICH.
Method
Procedure and Eligibility
The current study evaluates text messages sent by NICH interventionists to youth with diabetes and their caregivers. Youth were referred to NICH by providers at a children’s hospital at a major academic medical center in the United States. Eligible youth were identified by medical staff as having experienced poor metabolic control (ie, HbA1c > 10), at least 1 diabetes-related hospitalization (eg, DKA, hypoglycemic event) in the past 6 months, presence of psychosocial vulnerability (eg, family financial insecurity, involvement of child protective services), and limited response to medical interventions. Youth and families included in this study had already received NICH services, and retrospective chart reviews were conducted to collect text data.
Only patients and caregivers who had received at least 2 months of NICH services with associated text records were included. Overall, data for 26 youth (11 males and 15 females) and 24 primary caregivers (17 mothers, 4 fathers, 1 sister, 1 grandmother, and 1 girlfriend) were collected. Twenty-four of the participating patients were diagnosed with type 1 diabetes, and 2 patients with type 2 diabetes and insulin dependence. In families with more than 1 identified caregiver, only texts sent to the interventionist’s primary contact person were included. If the patient or caregiver did not have access to a phone, the NICH program provided one. Patient mean age at onset of treatment was 15.6 years (SD = 1.7 years), and mean duration of diabetes was 6.4 years (SD = 4.3 years). During the year prior to NICH enrollment, mean patient HbA1c was 12.3 (SD = 1.5), and patients averaged 5.1 days admitted (SD = 6.5 days) due to diabetes-related complications (eg, DKA). The mean length of NICH treatment for patients in this study was 17.7 months (SD = 7.8 months; range = 8.9-37.9 months). All research procedures were approved by the university Institutional Review Board.
NICH Program Description
The interventions that comprise NICH and a case example have been described in detail previously (see Harris et al38 for a more thorough description). Briefly, NICH services include a combination of case management, care coordination, and behaviorally based interventions. NICH interventionists are on call 24 hours per day, 7 days per week. NICH services are delivered in all contexts in which the patient and family are embedded (eg, hospitals, clinics, schools, homes) to facilitate collaboration between medical providers and families, improve families’ abilities to problem-solve, improve adherence, and reduce unnecessary hospitalizations. NICH interventionists average 3 hours per week in face-to-face service provision with patients and families. Regarding technology use, anecdotal reports of NICH interventionists and supervisors suggested that outgoing text messages are sent frequently, often occur outside of business hours, are positive and encouraging, and are modified to best fit the individual traits of the recipient (eg, more emoji and meme use with adolescents than caregivers).
At the time of this study, NICH services were being provided by 8 interventionists with caseloads of approximately 8 to 10 patients. NICH interventionists are typically masters-level providers with backgrounds in medicine, psychology, public health, and/or social work. Weekly supervision was provided by doctoral-level professionals in psychology and included, on average, 2 hours of group supervision, 1 hour of individual supervision, and phone support as needed.
Data Collection
Two months of interventionists’ text records were collected, and incoming and outgoing text frequencies were calculated. Because the aim of the current study is to better understand how treatment programs might utilize personalized communications to enhance interventions, only content from outgoing text messages was coded. Trained research assistants coded outgoing texts for micro (eg, positive reinforcement, problem-solving, scheduling) and macro level intervention content (ie, behavioral intervention, care coordination, case management). Patient age and sex, and caregiver sex and status, were recorded. Each text received a primary content code (PCC) and a care type code (CTC). If applicable, some texts also received a secondary content code (SCC). Table 1 displays brief code definitions and examples.
Table 1.
Care and Content Code Definitions and Examples.
| Text content category | Text includes | Examples |
|---|---|---|
| Care codes | ||
| Behavioral intervention | An interaction intended to influence patient or caregiver behavior and not directly related to coordinating care or accessing resources. | Positive reinforcement, parent training, problem solving, coaching |
| Care coordination | An interaction related to ensuring that patient is receiving the recommended medical care. | Scheduling, assisting with supply access |
| Case management | An interaction related to helping the family access requested resources and/or interface with other nonmedical providers/organizations | Interfacing with mental health, school, child protective resources |
| Content codes | ||
| Positive interaction | Praising desired behaviors, thanking, validating. | “Great job checking your BGLs!” |
| Care interaction | Sending reminders/requests directly related to diabetes management. | “Remember to send carb count.” |
| Checking in | Requesting information that is unrelated to medical care | “How was school today?” |
| Problem solving | Providing and assessing value of potential solutions | “One option would be to call 911.” |
| Coaching | Providing directions related to ongoing skills training | “Take a deep breath.” |
| Scheduling | Communicating related to scheduling or attending an appointment | “We’ll see your endo at 3pm.” |
| Providing information | Offering information unrelated to other content codes | “The food bank opens at 9am.” |
| Rapport building | Attempts to build rapport that don’t clearly fit other content codes | “Enjoy the weather!” |
| Strategic questioning | Guiding decision-making through use of questions. | “Which support could you call?” |
| Tech fun | Sending memes, pictures, emoticons, or videos | “☺” |
| Empathizing/normalizing | Displaying empathy or attempting to normalize experiences | “Parenting can be stressful!” |
Text Coding
In phase 1 of text coding, a list of potential PCC/SCC categories was created by a focus group of 5 interventionists and 1 supervisor. Categories that appeared overly similar were combined, and those judged likely to be poorly represented were removed. Coders were trained to categorize the primary theme of each text as the PCC and any secondary theme as the SCC. In phase 2, the outgoing texts from interventionists to 20 youth and caregivers were coded, interrater reliability was analyzed, and new categories were subsequently created to address identified problems in coding. A second round of coding was then conducted and resulted in improved interrater reliability and fewer texts coded as “unknown.” The outcomes from round 2 are represented in the Results section. Kappas for PCC, SCC, and CTC were .74, .59, and .77, respectively, ranging from moderate to substantial agreement.40
Content Codes
Coders recorded the PCC/SCC of each text into 1 of 11 content categories (see Table 1). If text content did not fit in a category, it was coded as “unknown.” To estimate how many total texts contained some form of positive valence, an encouragement/support category was created that combined the positive interaction, rapport building, tech fun, and empathizing/normalizing categories.
Care Type Code
Consistent with the 3 types of services delivered in NICH, coders also recorded whether the overall message sent was most consistent with a behavioral- and/or family-based intervention, care coordination, or case management.
Results
Descriptive Information
Interventionists sent a total of 5,909 text messages to patients and caregivers, ranging from 6 to 468 texts per participant (mean = 118.2, SD = 94.3) and received a total of 7,217 text messages from patients and caregivers, ranging from 10 to 506 texts per participant (mean = 144.3, SD = 130.4). Bivariate correlations examined relations among frequencies of text messages sent to and from patients (r = .74, P < .001) and text messages sent to and from caregivers (r = .89, P < .001). Because the above analyses revealed significant associations between the number of incoming and outgoing text messages, we did not control for frequency of incoming text messages in further analyses.
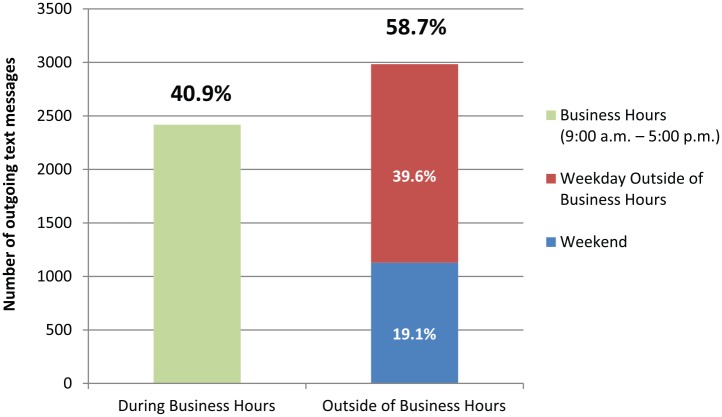
NICH interventionists texted patients 2.3 times per day (SD = 1.6) and caregivers 1.5 times per day (SD = 1.0). Descriptive data for time and content of outgoing text messages appear in Tables 2 and 3, respectively. Text message frequencies by day/time of text (Table 2) reveal that, of the 5,909 text messages sent, 40.9% were sent during business hours and 58.7% were sent outside of business hours. Text messages sent outside of business hours were most often sent on weekdays prior to or after business hours (39.6%; Figure 1). Table 3 indicates that texts were sent with the purpose of behavioral intervention (76.4%), care coordination (19.6%), and case management (2.2%). The primary purpose of 52.0% of sent text messages was to provide encouragement/reinforcement, and positive interactions were the most commonly represented text content (42.2%).
Table 2.
Frequencies and Percentages of Outgoing Texts by Day/Time.
| Day and time of outgoing texts | Total outgoing texts | Average texts per participant | Percentage |
|---|---|---|---|
| During business hours | |||
| Week (Monday-Friday) | 2418 | 48.4 | 40.9 |
| Outside of business hours | 3468 | 69.4 | 58.7 |
| Week (Monday-Friday) | 4758 | 95.2 | 80.9 |
| Morning | 485 | 09.7 | 08.2 |
| Evening | 1855 | 37.1 | 31.4 |
| Weekend (Saturday and Sunday) | 1128 | 22.6 | 19.1 |
| Morning | 44 | 0.9 | 00.7 |
| Day | 581 | 11.6 | 09.8 |
| Evening | 503 | 10.1 | 08.5 |
| Missing | 23 | 0.5 | 00.4 |
| Total | 5909 | 118.2 | 100.0 |
Morning = 12:00AM-8:59AM; Day = 9:00AM-5:00PM; Evening = 5:01PM-11:59PM. During business hours = 9:00AM-5:00PM.
Table 3.
Frequencies and Percentages of Outgoing Texts by Content Category.
| Text contentCategories | Primary Content code | Secondary Content code | Content Present (PCC and/or SCC) |
|---|---|---|---|
| Care codes | |||
| Behavioral intervention | 4517 (76.4)a | — | — |
| Care coordination | 1161 (19.6) | — | — |
| Case management | 131 (2.2) | — | — |
| Missing | 100 (1.7) | — | |
| Content codes | |||
| Positive interaction | 2217 (37.5)b | 276 (4.7)c | 2492 (42.2) |
| Care interaction | 667 (11.5) | 297 (5.0) | 1004 (17.0) |
| Checking in | 522 (8.8) | 193 (3.3) | 690 (11.7) |
| Problem solving | 68 (1.2) | 42 (0.7) | 109 (1.8) |
| Coaching | 110 (1.9) | 112 (1.9) | 214 (3.6) |
| Scheduling | 837 (14.2) | 318 (5.4) | 1099 (18.6) |
| Providing information | 408 (6.9) | 122 (2.1) | 520 (8.8) |
| Rapport building | 499 (8.4) | 203 (3.4) | 674 (11.4) |
| Strategic questioning | 82 (1.4) | 65 (1.1) | 147 (2.5) |
| Tech fun | 204 (3.5) | 442 (7.5) | 651 (11.0) |
| Empathizing/normalizing | 152 (2.6) | 81 (1.4) | 225 (3.8) |
| TOTAL | 5776 (97.7) | 2151 (36.4) | — |
|
| |||
| Unknown/noned | 91 (1.5) | 3735 (63.2)d | 3465 (58.6)d |
|
| |||
| Missing | 42 (0.7) | 23 (0.4) | 19 (0.3) |
|
| |||
| Encouragement/support | 3072 (52.0) | 1002 (17.0) | 4042 (68.4) |
PCC, primary content code; SCC, secondary content code. an (%) = n of care code category (percentage of care code category relative to total outgoing texts). bn (%) = n of PCC texts (percentage of PCC texts relative to total outgoing texts). cn (%) = n of SCC texts (percentage of SCC texts relative to total outgoing texts). dAll text messages were given a PCC, therefore unclear content was coded as “unknown.” SCCs were not required and thus, many text messages were not given a secondary code (ie, coded as “none”).
Figure 1.
Frequencies of outgoing texts by day/time. Percentages reflect the percentages of all text messages that were sent during each time period; the figure does not include missing data (n = 23; 0.4% of texts).
Tests of Independence Among Study Variables
Chi-square tests of independence were performed to examine the relation between text content and text recipient (Table 4). The relation between care codes and text recipient was significant, suggesting that patients were more likely to receive care coordination texts than were caregivers, χ2(1, N = 5714) = 5.83, P < .01, and caregivers were more likely than patients to receive behavioral intervention texts (χ2 = 3.72, P < .05). In addition, chi-square results suggest that patients were more likely than caregivers to receive care interaction, χ2(1, N = 5794) = 92.03, P < .001, rapport building (χ2 = 15.12, P < .001), tech fun (χ2 = 120.74, P < .001), and encouragement/support (χ2 = 6.23, P < .05) texts, whereas caregivers were more likely than patients to receive positive interaction (χ2 = 12.73, P < .001), coaching (χ2 = 25.85, P < .001), informative (χ2 = 126.52, P < .001), strategic questioning (χ2 = 11.65, P < .001), and empathizing/normalizing (χ2 = 81.48, P < .001) texts.
Table 4.
Text Content Categories by Text Recipient (Patient vs Caregiver) and Day/Time of Text (During vs Outside of Business Hours).
| Text content categories | Text to patient, n = 3709 | Text to caregiver, n = 2104 | χ2 | Texts sent during business hours, n = 2418 | Texts sent outside of business hours, n = 3468 | χ2 |
|---|---|---|---|---|---|---|
| Care codes | ||||||
| Behavioral intervention | 2823 (76.1)a | 1632 (77.6)a | 3.72* | 1604 (66.3)b | 2913 (84.0)b | 266.91*** |
| Care coordination | 757 (20.4) | 371 (17.6) | 5.83** | 707 (29.2) | 453 (13.1) | 234.61*** |
| Case management | 78 (02.1) | 53 (02.5) | 1.17 | 79 (30.3) | 52 (1.5) | 20.31*** |
| Content codes | ||||||
| Positive interaction | 1507 (40.6) | 960 (45.6) | 12.73*** | 866 (35.8) | 1621 (46.7) | 69.81*** |
| Care interaction | 758 (20.4) | 225 (10.7) | 92.03*** | 330 (13.6) | 672 (19.4) | 33.11*** |
| Checking in | 413 (11.1) | 257 (12.2) | 1.39 | 334 (13.8) | 352 (10.1) | 18.59*** |
| Problem solving | 60 (01.6) | 47 (02.2) | 2.74 | 41 (01.7) | 68 (02.0) | 0.55 |
| Coaching | 99 (02.7) | 111 (05.3) | 25.85*** | 81 (03.3) | 133 (03.8) | 0.96 |
| Scheduling | 680 (18.3) | 385 (18.3) | 0.01 | 659 (27.3) | 434 (12.5) | 204.92*** |
| Providing information | 209 (5.6) | 305 (14.5) | 126.52*** | 238 (09.8) | 276 (08.0) | 6.36* |
| Rapport building | 475 (12.8) | 199 (09.5) | 15.12*** | 227 (09.4) | 447 (12.9) | 17.22*** |
| Strategic questioning | 74 (02.0) | 73 (03.5) | 11.65*** | 64 (02.6) | 83 (02.4) | 0.38 |
| Tech fun | 541 (14.6) | 109 (05.2) | 120.74*** | 244 (10.1) | 405 (11.7) | 3.65 |
| Empathizing/normalizing | 78 (02.1) | 144 (06.8) | 81.48*** | 87 (03.6) | 138 (04.0) | 0.56 |
| Encouragement/support | 2235 (60.3) | 1203 (57.2) | 6.23* | 1235 (51.1) | 2224 (64.1) | 100.53*** |
Each text has only 1 care code, but may have 1 or multiple intervention codes. an (%) = n of content category texts to patient/caregiver (percentage content category texts to parent/caregiver relative to total texts to patient/caregiver). bn (%) = n of content category texts sent during/outside of business hours (percentage content category texts sent during/outside of business hours relative to total texts sent during/outside of business hours).
P ≤ .05. **P ≤ .01. ***P ≤ .001.
Chi-square tests of independence were performed to examine the relation between text content and day/time of messages (Table 4). The relation between care codes and day/time of text was significant. Interventionists were more likely to send behavioral intervention text messages outside of business hours than during business hours, χ2(1, N = 5808) = 266.91, P < .001, whereas they were more likely to send care coordination (χ2 = 234.61, P < .001) and case management (χ2 = 20.31, P < .001) text messages during business hours than outside of business hours (Figure 2). In addition, chi-square results suggest that interventionists were more likely to send positive interaction, χ2(1, N = 5867) = 69.81, P < .001, care interaction (χ2 = 33.11, P < .001), rapport building (χ2 = 17.22, P < .001), and encouragement/support (χ2 = 100.53, P < .001) texts outside of business hours than during business hours and were more likely to send scheduling text messages (χ2 = 204.92, P < .001) and text messages providing information (χ2 = 6.36, P < .05) during business hours than outside of business hours.
Figure 2.
Care codes of outgoing texts by day/time of text. ***P < .001.
The relation between text content and sex of text recipient was also examined. Among patients, interventionists were more likely to send positive interaction, χ2(1, N = 2103) = 4.41, P < .05, care interaction (χ2 = 14.36, P < .001), problem solving (χ2 = 5.65, P < .05), rapport building (χ2 = 5.54, P < .05), and tech fun (χ2 = 44.17, P < .001) texts to females than to males and were more likely to provide information through text (χ2 = 4.10, P < .05) to males than females. Among patients, both the relation between care codes and sex, and the relation between sex of text recipient and the use of encouragement/support texts were null. Among caregivers, the relation between care codes and sex was significant, suggesting that interventionists were more likely to send behavioral intervention text messages to female caregivers than male caregivers, χ2(1, N = 2056) = 17.82, P < .001, and were more likely to send care coordination text messages to male caregivers than female caregivers (χ2 = 17.35, P < .001). Interventionists were also more likely to send care interaction (χ2 = 9.73, P < .01), scheduling (χ2 = 7.15, P < .05), and tech fun (χ2 = 10.45, P < .01) text messages to male caregivers than to female caregivers and were more likely to send empathizing/normalizing text messages (χ2 = 2.47, P < .05) to female caregivers than male caregivers. Among caregivers, the relation between sex of text recipient and use of encouragement/support texts was also null.
Discussion
The results of this study are relevant to the growing body of literature describing text interventions for youth with medical complexity. Findings indicate that NICH interventionists frequently text both NICH patients and their primary caregivers, and that text content is consistent with program efforts to use texting to provide more opportunities for immediate positive reinforcement and behavioral intervention.
NICH interventionists frequently provided positive/encouraging texts to patients and primary caregivers. Given the high rate of “diabetes burnout” reported by adolescents and youth adults with diabetes, NICH providers are coached to intervene consistent with the research of Gottman,41 by providing a 5:1 ratio of positive/encouraging messages compared to diabetes-specific reminders with a potentially negative valence. However, the frequent need for problem-solving, scheduling, and care-related texts may result in a less-than-optimal ratio of encouraging to reminding texts. Fortunately, more than 68% of outgoing messages were coded as containing some form of encouragement and/or support, including use of compliments, empathy, humor, and positive reinforcement of desired behaviors.
In addition, caregivers were more likely than patients to receive behavioral intervention texts. This is not entirely surprising, given that NICH aims to improve caregivers’ abilities to problem-solve and effectively support patient adherence. For example, interventionists are trained to identify signs of “miscarried helping” and to modify caregiver-patient interactions to reduce diabetes-related conflict. Caregivers are also coached, as needed, to successfully address other patient behaviors (eg, illicit drug use, association with delinquent peers, school truancy) directly or indirectly related to diabetes management that often result in increased caregiver-child conflict. The strong correlation between incoming and outgoing texts suggests that interventionists were able to maintain communication with both patients and caregivers. While we cannot be sure whether it is the supportive/encouraging nature of outgoing texts, the high need for and acceptability of in-the-moment parent training, or the personalized nature of this intervention, we hypothesize that these intervention components may be driving patient engagement.
Interestingly, the majority of texts were sent outside of business hours. This finding is consistent with interventionists’ anecdotal reports that much of their communication with families does not occur from 9 to 5, Monday through Friday. Related to this, SMS use outside of business hours was significantly more likely to involve behavioral interventions, suggesting the need for assistance (ie, problem-solving) at times when providers are traditionally unavailable or difficult to access. These results should be considered when creating future text interventions, as even automated/scheduled texting programs may benefit from enhancing care outside of business hours.
Interventionist SMS use varied depending on the sex of the recipient. However, although recipient sex appeared to be related to frequency of specific outgoing content, the frequency of texts that were perceived to be encouraging and/or supportive did not differ based on sex for caregivers or patient. It is unclear whether content differences were driven by interventionist perceptions of content efficacy, interventionist biases when interacting with individuals of different sex, and/or the incoming messages received; however, results reflect the tailored nature of the intervention and interventionists’ efforts to personalize interactions, while maintaining efforts to incorporate encouragement and positive reinforcement.
Regarding limitations, the data presented here are retrospective, program-specific, and may not generalize well to other clinical programs or patient populations. These findings were not compared to treatment outcomes, and the sample size was relatively small. There was also a large range in the number of texts sent. This range is indicative of the flexible nature of NICH to modify forms of communication as needed to best fit patient and family needs (eg, 1 individual received only 6 texts due to their lack of comfort with SMS). Future studies would benefit from utilizing a larger sample size, examining associations between use of text and treatment change, coding characteristics of incoming texts, and including a control group.
Conclusion
To our knowledge, this is the first study to specifically describe the personalized use of text messages with youth repeatedly hospitalized for DKA and their caregivers. Personalized text messages were used, on average, more than once per day with youth and primary caregivers, and often included encouragement outside of typical business hours. A strong correlation was demonstrated between the frequency of incoming and outgoing texts, which, although not definitive, suggests that the communications had value for the patients and caregivers served. Although speculative, findings indicate that frequent use of personalized and positive text messages may be an acceptable supplement to programs designed to engage and treat youth experiencing multiple DKA events. These findings may be particularly relevant to providers caring for similar youth, as well as treatment developers, researchers, and health care systems interested in using mobile technology to augment treatment efficacy.
Acknowledgments
We want to acknowledge the patients and families who have participated in NICH.
Footnotes
Abbreviations: CTC, care type code; DKA, diabetic ketoacidosis; NICH, Novel Interventions in Children’s Healthcare; PCC, primary content code; SCC, secondary content code; SMS, short message service.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Rewers M, Pihoker C, Donaghue K, Hanas R, Swift P, Klingensmith G. Assessment and monitoring of glycemic control in children and adolescents with diabetes. Pediatr Diabetes. 2009;10:71-81. [DOI] [PubMed] [Google Scholar]
- 2. Wood JR, Miller KM, Maahs DM, et al. Most youth with type 1 diabetes in the T1D Exchange Clinic Registry do not meet American Diabetes Association or International Society for Pediatric and Adolescent Diabetes clinical guidelines. Diabetes Care. 2013;36(7):2035-2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Harris MA, Hood KK, Weissberg-Benchell J. Teens with Diabetes: A Clinicians Guide. Alexandria, VA: American Diabetes Association; 2014. [Google Scholar]
- 4. Weissberg-Benchell J, Glasgow AM, Tynan WD, Wirtz P, Turek J, Ward J. Adolescent diabetes management and mismanagement. Diabetes Care. 1995;18(1):77-82. [DOI] [PubMed] [Google Scholar]
- 5. Klafke A, Bartholow Duncan B, Stevens A, et al. The decline in mortality due to acute complications of diabetes mellitus in Brazil, 1991-2010. BMC Pub Health. 2015;15(1):772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Diabetes Control and Complications Trial Research Group (DCCT Research Group). Effects of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: diabetes control and complications trial. N Engl J Med. 1994;125(2):177-188. [DOI] [PubMed] [Google Scholar]
- 7. Hood KK, Beavers DP, Yi-Frazier J, et al. Psychosocial burden and glycemic control during the first 6 years of diabetes: results from the SEARCH for diabetes in youth study. J Adolesc Health. 2014;55(1):498-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hoey H. Psychosocial factors are associated with metabolic control in adolescents: research from the Hvidoere Study Group on Childhood Diabetes. Pediatr Diabetes. 2009;10(suppl 13):9-14. [DOI] [PubMed] [Google Scholar]
- 10. Bernstein CM, Stockwell MS, Gallagher MP, Rosenthal SL, Soren K. Mental health issues in adolescents and young adults with type 1 diabetes: prevalence and impact on glycemic control. Clin Pediatr. 2013;52(1):10-15. [DOI] [PubMed] [Google Scholar]
- 11. Petitti DB, Klingensmith GJ, Bell RA, et al. Glycemic control in youth with diabetes: the SEARCH for Diabetes in Youth Study. J Pediatr. 2009;155(5):668-672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Drew LM, Berg C, King P, et al. Depleted parental psychological resources as mediators of the association of income with adherence and metabolic control. J Fam Psychol. 2011;25(5):751-758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Willi SM, Miller KM, Dimeglio LA, et al. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135(3):424-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. La Greca AM, Swales T, Klemp S, et al. Adolescents with diabetes: gender differences in psychological functioning and glycemic control. Child Health Care. 1995;24:61-78. [Google Scholar]
- 15. Piette JD, Richardson C, Valenstein M. Addressing the needs of patients with multiple chronic illnesses: the case of diabetes and depression. Am J Manag Care. 2004;10(2):152-162. [PubMed] [Google Scholar]
- 16. Cameron FJ, Skinner TC, De beaufort CE, et al. Are family factors universally related to metabolic outcomes in adolescents with Type 1 diabetes? Diabet Med. 2008;25(4):463-468. [DOI] [PubMed] [Google Scholar]
- 17. Cohen DM, Lumley MA, Naar-King S, et al. Child behavior problems and family functioning as predictors of adherence and glycemic control in economically disadvantaged children with type 1 diabetes: a prospective study. J Pediatr Psychol. 2004;29(3):171-184. [DOI] [PubMed] [Google Scholar]
- 18. Hilliard ME, Wu YP, Rausch J, Dolan LM, Hood KK. Predictors of deteriorations in diabetes management and control in adolescents with type 1 diabetes. J Adolesc Health. 2013;52(1):28-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jacobson AM, Hauser ST, Lavori P, et al. Family environment and glycemic control: a four-year prospective study of children and adolescents with insulin-dependent diabetes mellitus. Psychosom Med. 1994;56(5):401-409. [DOI] [PubMed] [Google Scholar]
- 20. Anderson BJ, Vangsness L, Connell A, et al. Family conflict, adherence, and glycaemic control in youth with short duration type 1 diabetes. Diabet Med. 2002;19(8):635-642. [DOI] [PubMed] [Google Scholar]
- 21. Lancaster BM, Gadaire DM, Holman K, Leblanc LA. Association between diabetes treatment adherence and parent-child agreement regarding treatment responsibilities. Fam Syst Health. 2015;33(2):120-125. [DOI] [PubMed] [Google Scholar]
- 22. Wagner DV, Stoeckel ME, Tudor M, Harris MA. Treating the most vulnerable and costly in diabetes. Curr Diab Rep. 2015;15(6):32-38. [DOI] [PubMed] [Google Scholar]
- 23. Delamater AM, Shaw KH, Applegate EB, et al. Risk for metabolic control problems in minority youth with diabetes. Diabetes Care. 1999;22(5):700-705. [DOI] [PubMed] [Google Scholar]
- 24. Urbach SL, Lafranchi S, Lambert L, Lapidus JA, Daneman D, Becker TM. Predictors of glucose control in children and adolescents with type 1 diabetes mellitus. Pediatr Diabetes. 2005;6(2):69-74. [DOI] [PubMed] [Google Scholar]
- 25. Wysocki T, Harris MA, Buckloh LM, et al. Effects of behavioral family systems therapy for diabetes on adolescents’ family relationships, treatment adherence, and metabolic control. J Pediatr Psychol. 2006;31(9):928-938. [DOI] [PubMed] [Google Scholar]
- 26. Harris MA, Freeman KA, Beers M. Family therapy for adolescents with poorly controlled diabetes: initial test of clinical significance. J Pediatr Psychol. 2009;34(10):1097-1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hood KK, Rohan JM, Peterson CM, Drotar D. Interventions with adherence-promoting components in pediatric type 1 diabetes: meta-analysis of their impact on glycemic control. Diabetes Care. 2010;33(7):1658-1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Winkley K, Ismail K, Landau S, Eisler I. Psychological interventions to improve glycaemic control in patients with type 1 diabetes: systematic review and meta-analysis of randomised controlled trials. BMJ. 2006;333 (7558):65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lenhart A. Teens, smartphones & texting. Pew Internet and American Life Project; 2012. Available at: www.pewinternet.org/Reports/2012/Teens-and-smartphones/Summary-of-findings.aspx. Accessed October 13, 2015.
- 30. Herbert L, Owen V, Pascarella L, Streisand R. Text message interventions for children and adolescents with type 1 diabetes: a systematic review. Diabetes Technol Ther. 2013;15(5):362-370. [DOI] [PubMed] [Google Scholar]
- 31. Wangberg SC, Arsand E, Andersson N. Diabetes education via mobile text messaging. J Telemed Telecare. 2006;12(suppl 1):55-56. [DOI] [PubMed] [Google Scholar]
- 32. Rami B, Popow C, Horn W, Waldhoer T, Schober E. Telemedical support to improve glycemic control in adolescents with type 1 diabetes mellitus. Eur J Pediatr. 2006;165(10):701-705. [DOI] [PubMed] [Google Scholar]
- 33. Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006;23:1332-1338. [DOI] [PubMed] [Google Scholar]
- 34. Hanauer DA, Wentzell K, Laffel N, Laffel LM. Computerized Automated Reminder Diabetes System (CARDS): email and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technol Ther. 2009;11:99-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Froisland DH, Arsand E, Skarderud F. Improving diabetes care for young people with type 1 diabetes through visual learning on mobile phones: mixed-methods study. J Med Internet Res. 2012;14(4):e111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Newton KH, Wiltshire E, Elley CR. Pedometers and text messaging to increase physical activity: randomized controlled trial of adolescents with type 1 diabetes. Diabetes Care. 2009;32:813-815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mulvaney SA, Anders S, Smith AK, Pittel EJ, Johnson KB. A pilot test of a tailored mobile and web-based diabetes messaging system for adolescents. J Telemed Telecare. 2012;18:115-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Harris MA, Spiro K, Heywood M, et al. Novel Interventions in Children’s Healthcare (NICH): innovative treatment for youth with complex medical conditions. Clin Pract Pediatr Psychol. 2013;1(2):137-145. [Google Scholar]
- 39. Harris MA, Spiro K, Heywood M, et al. Piloting intensive behavioral health for youth with type 1 diabetes: avoiding avoidable hospitalizations [abstract]. Diabetes. 2013;73:827-P. [Google Scholar]
- 40. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159-174. [PubMed] [Google Scholar]
- 41. Gottman J. The Analysis of Change. New York, NY: Psychology Press; 2013. [Google Scholar]