Abstract
Background:
Adolescence is a developmental period associated with increased difficulty managing diabetes. During adolescence family functioning, including miscarried helping, family conflict, and acceptance of illness, is an important predictor of adherence to treatment recommendations. Multiple barriers exist to receiving behavioral health interventions to address suboptimal adherence. We hypothesized that behavioral family systems therapy–diabetes (BFST-D) delivered via telehealth would yield changes in family functioning that were not significantly different than changes in clinic-based treatment. Furthermore, that BFST-D would significantly improve overall family functioning.
Methods:
Ninety adolescent participants and their parents were randomized to receive BFST-D via telehealth or traditional (Clinic) treatment conditions. Repeated measures ANOVAs were used to assess changes in mean scores across pre, post, and follow-up assessments. Mediation analyses were conducted using methods outlined by Sobel and were confirmed by bootstrapping.
Results:
Changes in miscarried helping, family conflict and adjustment to illness were not significantly different across groups. Overall, clinically significant improvements were identified in youth- and parent-reported miscarried helping, family conflict, and acceptance of illness. Reductions in family conflict mediated the relationship between changes in miscarried helping and acceptance of illness. In addition, improvements in family functioning were associated with changes in adherence and glycemic control.
Conclusions:
Results provide strong support for BFST-D (and similar interventions) delivered via telehealth as yielding outcomes no different than clinic-based treatment. In addition, further support was provided for the effectiveness of BFST-D.
Keywords: type 1 diabetes, adolescence, family factors, randomized clinical trial, teleconferencing, telehealth
Management of type 1 diabetes (T1D) is complex and difficult to accomplish during adolescence.1-3 Suboptimal adherence to treatment recommendations increases the risk of youth with T1D of experiencing acute (eg, diabetic ketoacidosis)4 and chronic medical complications (eg, retinopathy, nephropathy, neuropathy),5 and is associated with poor psychological outcomes (eg, depression symptoms).6 In addition, suboptimal adherence is known to increase health care costs for individuals, medical systems, payers, and society at large.7
Effective interventions to address suboptimal adherence should address barriers to adherence.8,9 Important risk factors include impaired family functioning, maladaptive parent-child interactions, and difficulty accepting diabetes. For example, both family conflict10,11 and miscarried helping12,13 have been associated with decreased adherence and suboptimal glycemic control in adolescents with T1D. Furthermore, lower illness acceptance has been linked with poor psychosocial outcomes (eg, depression), and is both indirectly and directly related to diabetes management.14 Thus, it is reasonable to posit that interventions designed to effectively address these risk factors would result in improved short- and long-term diabetes-related outcomes.
Fortunately, several intervention models have been developed to address youth and family functioning, and parent-child interactions for youth with T1D. In particular, behavioral family systems therapy–diabetes (BFST-D) has become a well-established intervention for adolescents with diabetes and their families that has produced improvements in both family functioning and health outcomes.15 BFST-D has led to decreased parent-child conflict, increased adherence, and improved glycemic control.15-17
Despite the notable success of BFST-D to improve adherence and health outcomes, families who reside in rural areas often lack access to BFST-D or other similar evidence-based interventions. Such behavioral health resources are often affiliated with academic institutions and located in urban population centers. In general, pediatric patients who reside distant from resources experience reduced access and engagement with health care services.18 Patients who have limited access to specialized diabetes care services may be less likely to routinely attend clinic visits, have suboptimal adherence, and be at greater risk for poor psychosocial and health outcomes.19-24 Thus, the development and application of telehealth technologies and methods to deliver virtual medical, health, and education services has tremendous potential for delivering evidence-based interventions to pediatric patients who would otherwise have limited or no access to such services.
Telehealth is a widely studied means of health care service delivery for patients who would not otherwise have reasonable access to health care.25 Telehealth has become more feasible given the increasing adoption of Internet services across all socioeconomic status households.26 The use of telehealth has been linked to improved problem solving, self-management, and family functioning in youth with T1D27 as well as improved functioning in youth with a host of psychological conditions.28 In addition, findings from a BFST-D trial suggest that telehealth can positively affect therapeutic alliance,29 depressive symptoms adherence,30 and glycemic control.31 The current study examines whether BFST-D delivered via telehealth resulted in improvements in other relevant areas of functioning (miscarried helping, family conflict, and acceptance of illness) for youth with T1D and their families.
We developed 5 a priori hypotheses, as follows:
BFST-D delivered via telehealth would not yield significantly different outcomes than BFST-D delivered in a traditional face-to-face clinic setting.
Furthermore, we hypothesized that BFST-D would demonstrate effectiveness regardless of treatment arm, as follows:
BFST-D would decrease parent and youth reports of miscarried helping.
BFST-D would decrease parent and youth reports of family conflict.
BFST-D would improve parent and youth reports of acceptance of illness.
Finally, adherence and glycemic control would be significantly associated with improvements in family functioning (miscarried helping, family conflict, and acceptance of illness).
Methods
Participants
Participants were primarily recruited through a regional diabetes center affiliated with an academic medical center and teaching hospital located in the US Pacific Northwest. Participants included adolescents who had been diagnosed with diabetes for at least 1 year, were 12 to 19 years old, had suboptimal glycemic control at enrollment (HbA1c ≥ 9.0% [74.9 mmol/mol]), resided with and were accompanied by their primary caretaker, intended to reside with their caretaker for the duration of the study (6 months), had no history of intellectual disability or mental health condition that would preclude understanding and completing study measures, and had no uncontrolled comorbid health condition (eg, cystic fibrosis) that would confound assessment of adherence to diabetes treatment recommendations.
An a priori power analysis suggested a sample size of 80 (40 in each group). A total of 138 families were approached to participate in the study; 9 were ineligible and 39 declined. A final total of 90 adolescent/caregiver dyads participated. Adolescent participants were a mean age of 15.02 (SD = 1.75) years of age, and 45% identified as female (Table 1). Most caregivers (76.7%) self-identified as mothers, with 21.1% as fathers, and 2.2% as grandmothers. In all, 40% endorsed residing in a 2-parent household. Caregivers endorsed youth race/ethnicity as 87.8% Caucasian, 4.4% Hispanic/Latin American, 1.1% Native American, 1.1% Hawaiian/Pacific Islander, and 5.6% biracial or multiethnic. Socioeconomic status was calculated for each stratum using methods recommended by Hollingshead (Hollingshead Index),32 as follows: lower: 5.6%; lower middle: 8.0%; middle: 41.0%; upper middle: 37.4%; and upper: 8.0%. Adolescent and caregivers dyads who declined to participate were not significantly different from participants on demographic variables (eg, age, duration of diabetes, gender).
Table 1.
Demographic Characteristics: Mean (SD).
| Clinic | Skype™ | Combined | |
|---|---|---|---|
| Females, n (%) | 18 (51.4) | 17 (48.6) | 35 (38.9) |
| Males, n (%) | 26 (47.3) | 29 (52.7) | 55 (61.1) |
| Age | 15.04 (1.79) | 14.94 (1.77) | 15.02 (1.75) |
| Diabetes duration | 6.51 (3.24) | 6.93 (3.85) | 6.72 (3.54) |
| Baseline HbA1c (pre) | 11.03 (1.68) | 11.14 (1.69) | 11.13 (1.71) |
| Hollingshead Index | 37.02 (11.90) | 37.64 (9.93) | 37.46 (10.23) |
Intervention
BFST-D comprises 4 primary intervention components:29 (1) problem solving, (2) communication training, (3) cognitive reframing (dispelling strong beliefs), and (4) family restructuring; the focus of implementing these components was on diabetes care. Problem-solving training includes teaching families formal problem solving that includes defining the problem, generating solutions, group decision-making, implementing and monitoring solution(s), and refining ineffective solutions. Communication training includes instruction, feedback, modeling, and rehearsal of approaches to address common parent/adolescent communication errors. Cognitive restructuring includes addressing and altering irrational beliefs, attitudes, and attributions that could impede effective parent/adolescent interactions. Family restructuring involves both functional and structural approaches to target maladaptive or ineffective family system patterns and characteristics (eg, weak parental coalitions and cross-generational coalitions) that could impede effective problem solving and communication.
Measures
Demographic Information
A Demographic Information Form (DIF) was completed by caregivers. Youth and/or families who declined to participate completed a shortened DIF form.
Adherence
The Diabetes Self-Management Profile–Diabetes (DSMP)33 is a 23-item semistructured interview; higher total scores indicate increased adherence. The DSMP typically requires 15-20 minutes to complete. Questions assess 5 key aspects of diabetes management including insulin administration, blood-glucose monitoring, exercise, diet, and management of hypo- and hyperglycemia. Previous research has demonstrated good psychometric properties, including significant correlations with objective measures of adherence (eg, blood glucose testing).34 Both adolescent and caregiver reports were used. For the current study, internal consistency (Cronbach’s alpha) was good at Pre (baseline) for adolescents (α = .75) and caregivers (α = .81), and was similar at Post and Follow-up assessments.
Glycemic Control
Glycemic control was estimated by a routine glycosylated HbA1c assay (Bayer DCA-2000), which provided an estimate of average blood glucose over the preceding 2-3 months.35 The equivalence of DCA-2000 and reference laboratory measurements has been well established.36
Miscarried Helping
Adolescent and caregiver participants completed analogous versions of the Helping for Health Inventory (HHI),37 a 15-item questionnaire designed to assess miscarried helping occurring between youth with diabetes and their caregivers. Miscarried helping is a maladaptive interaction pattern in which a parent’s attempts to assist their adolescent with diabetes management results in increased conflict, resistance, and, ultimately, parental withdrawal from assisting with disease management. Items are rated on a 5-point scale, from 1 = “rarely” to 5 = “always,” and are summed to create a total score. Higher scores indicate increased frequency of miscarried helping. The HHI includes items such as “I find that the more I try to help my child with his/her chronic illness, the more he/she resists my involvement” and “My parents get upset with me when my health doesn’t improve.” The HHI has demonstrated good reliability and validity.38 Internal consistency for the present study was good for adolescents (α = .82) and caregivers (α = .83) at the Pre assessment, with very similar alphas at Post and Follow-up.
Family Conflict
The Conflict Behavior Questionnaire Short Form (CBQ)39,40 is a 20-item true/false self-report that measures parent-adolescent conflict. Examples of items include “My mom screams a lot” and “My mom doesn’t understand me.” Scores for the short form have correlated strongly with the original long form (r = .96).39 Higher scores on the CBQ represent more conflict.15 Adequate internal consistency and discriminant validity have been established.40 Internal consistency in the present study at Pre assessment was good for adolescents (α = .82) and caregivers (α = .87), with very similar alphas at Post and Follow-up.
Acceptance of Illness
Adolescent and caregiver acceptance of illness was assessed using the Acceptance of Illness Scale (AIS),41 which consists of statements that describe negative consequences of ill-health. The AIS assesses the extent to which respondents accept the health condition without experiencing negative feelings or responses. The measure is an 8-item scale administered in analogous self and parent report formats. Respondents report their agreement with items such as “I have a hard time adjusting to the limitations of my illness” and “My child’s health makes me feel inadequate.” Items are rated on a 5-point scale, from 1 = “Strongly Agree” to 5 = “Strongly Disagree.” Higher scores indicate increased acceptance of illness. Acceptable internal consistency has been established (α = .81).41 In the present study alphas at Pre were good for adolescents (α = .87) and caregivers (α = .82), with very similar alphas at Post and Follow-up.
Procedures
Primary recruitment occurred during regularly scheduled diabetes clinic appointments (n = 85). Several participants (n = 5) were identified through other hospital-based clinics. Informed consent was obtained following institutional review board guidelines. Following institutional review board–approved consent/assent procedures, participants were randomized via a block design to receive BFST-D through either Telehealth (n = 46) or Clinic (n = 44) conditions. Participants in both treatment arms received up to 10 sessions of BFST-D of 1 to 1.5 hours duration per session; sessions were completed within a 12-week period following preintervention assessment. All participants received routine medical diabetes care over the course of the study.
Assessments occurred at 3 time points, Pre (within 4 weeks preceding the first session), Post (within 4 weeks of the final treatment session), and at Follow-up (3 months posttreatment). HbA1c assays were conducted concurrent with Pre, Post, and Follow-up assessments.
Adolescent participants received a monetary incentive for each completed assessment. Families randomized to the Telehealth condition were offered the loan of a laptop computer with webcam and mobile hotspot, but could use their personal computer and Internet service, if preferred. In addition, those traveling more than 50 miles round trip for study visits that were not part of routine medical care were reimbursed for mileage up to $250 total.
Treatment
BFST-D was delivered by clinicians having masters or doctoral degrees in psychology. Clinicians received training in BFST-D and direct weekly supervision. Clinicians cross-delivered BFST-D in both arms of the study approximately equally. BFST-D interventionists were directive and active in treatment delivery; they provided instructions, feedback, modeling, and guided rehearsal. Progress was reviewed, and family-based assignments were provided during each session. Sessions included didactic information with an emphasis on independently applying skills in real-life settings. A focus on addressing barriers to improved diabetes care was integrated throughout.
BFST-D was delivered either via clinic-based visits (Clinic) or via videoconferencing (Telehealth). For the Telehealth arm, a free Internet-based teleconferencing platform was used that facilitated direct synchronous audio-video communication in real time between the interventionist and participants. Families randomized to this condition were provided written instructions regarding how to download the software; technical assistance was offered if they experienced difficulties. At preestablished appointment times clinicians initiated communication with families from a secure setting, typically a private office. Participants participated in the session from their homes.
All participants received a reminder call 2 to 3 days prior to the next scheduled appointment. For those who missed appointments, attempts to reschedule continued until the appointment was established or the study treatment period expired.
Analyses
Data were initially checked for normality, outliers, or data entry errors prior to analyses. An intent-to-treat (ITT) analytic approach was used that included multiple imputation procedures to replace missing data.42,43 Associations were examined for relevant covariates that may differ by treatment condition. Treatment groups were compared for any mean differences in demographic or outcome variables at baseline (Pre). Repeated measures analyses of variance (ANOVA) were conducted to examine between subjects effects (Telehealth vs Clinic) and within subjects change across Pre, Post, and Follow-up assessments. Effect sizes were estimated by calculating Cohen’s d.
Results
Analyses found no statistically significant group (Telehealth vs Clinic) differences in demographic characteristics (Table 1). No significant differences (P = .14) were identified in mean number of sessions completed, Telehealth (mean = 5.84, SD = 3.25), Clinic (mean = 6.82, SD = 3.39). In addition, drop-out rates were not significantly different by treatment condition (see CONSORT statement; Figure 1).
Figure 1.
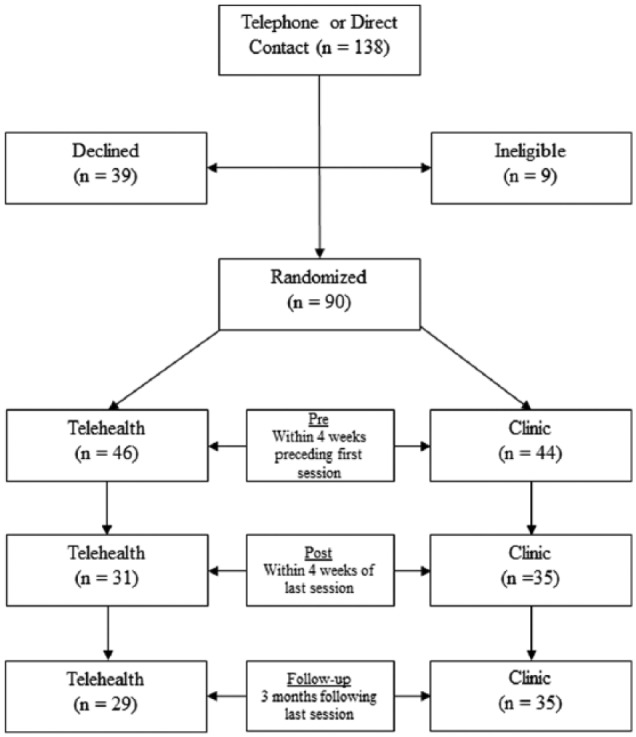
Consolidated Standards of Reporting Trials Statement of Youth Recruitment.
Hypothesis 1: Telehealth Versus Clinic Comparison
ANOVA identified no between-group differences (Telehealth vs Clinic) in youth-reported miscarried helping (Y-HHI), F(1) = 0.08, P = .78; family conflict (Y-CBQ), F(1) = 0.32, P = .57; and acceptance of illness (Y-AIS), F(1) = 3.87, P = .052 across Pre, Post, and Follow-up assessments. Also, no between group differences were identified in parent-reported miscarried helping (P-HHI), F(1) = 0.98, P = .33; family conflict (P-CBQ), F(1) = 0.27, P = .60; and acceptance of illness (P-AIS), F(1) = 1.00, P = .32, across Pre, Post, and Follow-up assessments.
Given no significant differences were identified between Telehealth and Clinic treatment, the groups were collapsed to further analyze the overall effects of BFST-D on youth and parent reports of miscarried helping, family conflict, and acceptance of illness (hypotheses 2-5).
Hypothesis 2: Miscarried Helping (HHI)
Youth
Within-subjects analysis of Y-HHI found the assumption of sphericity was not violated, χ2(2) = 4.48, P = .11. A significant main effect for Y-HHI was identified, F(2) = 4.82, P < .01, η2p = .052. Pairwise comparisons identified no significant changes in scores (P = .06) occurred from Pre (mean = 43.04, SD = 9.47) to Post (mean = 41.14, SD = 9.34), d = .20. However, significant changes (P < .01) were identified from Pre to Follow-up (mean = 40.11, SD = 8.97), d = .32 (Figure 2).
Figure 2.
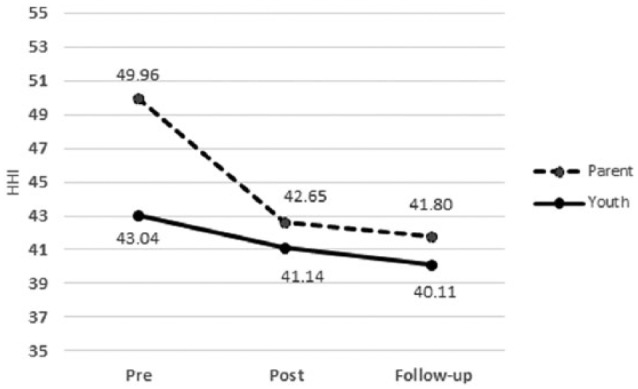
Miscarried helping (HHI) across Pre, Post, and Follow-up assessments.
Parent
Within-subjects analysis of P-HHI found the assumption of sphericity was violated, χ2(2) = 7.04, P = .03. Therefore, degrees of freedom were corrected (ε = .96),38 and a significant main effect for P-HHI was identified, F(1.92) = 44.5, P < .001, η2p = .336. Pairwise comparisons identified significant changes in scores (P < .001) occurred from Pre (mean = 49.96, SD = 9.64) to Post (mean = 42.65, SD = 9.31), d = .77 and from Pre to Follow-up (mean = 41.80, SD = 8.15), d = .91 (Figure 2).
Hypothesis 3: Family Conflict (CBQ)
Youth
Within-subjects analysis of Y-CBQ found the assumption of sphericity was violated, χ2(2) = 18.57, P < .001. Therefore, degrees of freedom were corrected (ε = .86),38 and a significant main effect for Y-CBQ was identified, F(1.73) = 14.21, P < .001, η2p = .139. Pairwise comparisons found significant changes in scores (P < .01) occurred from Pre (mean = 5.06, SD = 4.06) to Post (mean = 3.63, SD = 4.13), d = .35, and (P < .001) from Pre to Follow-up (mean = 3.03, SD = 3.37), d = .52 (Figure 3).
Figure 3.
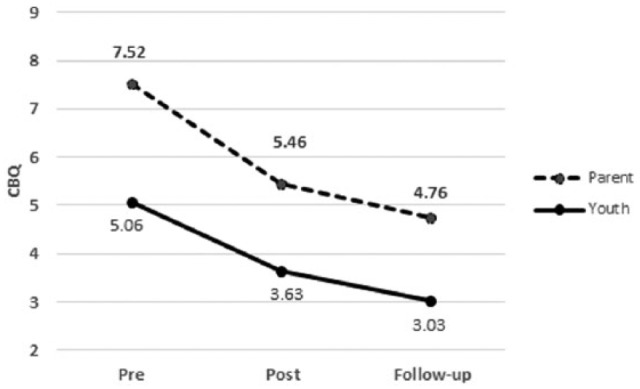
Family conflict (CBQ) across Pre, Post, and Follow-up assessments.
Parent
Within-subjects analysis of P-CBQ found the assumption of sphericity was violated, χ2(2) = 19.21, P < .001. Therefore, degrees of freedom were corrected (ε = .86),38 and a significant main effect for P-CBQ was identified, F(1.92) = 25.64, P < .001, η2p = .226. Pairwise comparisons found significant changes in scores (P < .001) occurred from Pre (mean = 7.52, SD = 4.81) to Post (mean = 5.46, SD = 4.77), d = .43, and from Pre to Follow-up (mean = 4.76, SD = 3.74), d = .64 (Figure 3).
Hypothesis 4: Acceptance of Illness
Youth
Within-subjects analysis of Y-AIS found the assumption of sphericity was violated, χ2(2) = 7.27, P = .026. Therefore, degrees of freedom were corrected (ε = .96),38 and a significant main effect for Y-AIS was not identified, F(1.91) = 0.54, P = .57, η2p = .006. Pairwise comparisons found no significant changes in scores (P = .38) occurred from Pre (mean = 28.22, SD = 6.95) to Post (mean = 28.98, SD = 7.79), d = .10, or (P = .82) from Pre to Follow-up (mean = 27.95, SD = 7.72), d = .03 (Figure 4).
Figure 4.
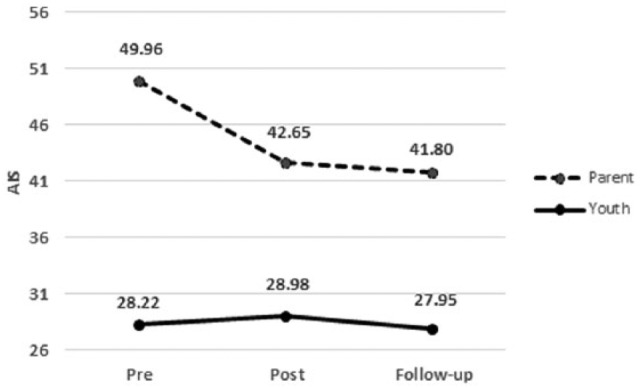
Acceptance of illness (AIS) across Pre, Post, and Follow-up assessments.
Parent
Within-subjects analysis of P-AIS found the assumption of sphericity was violated χ2(2) = 7.95, P = .019. Therefore, degrees of freedom were corrected (ε = .95),38 and a significant main effect for P-AIS was identified, F(1.89) = 14.28, P < .001, η2p = .140. Pairwise comparisons found significant changes in scores (P < .01) occurred from Pre (mean = 31.67, SD = 5.97) to Post (mean = 33.44, SD = 5.63), d = .31, and (P < .001) from Pre to Follow-up (mean = 34.22, SD = 4.97), d = .46 (Figure 4).
Hypothesis 5: Associations Between Adherence and Glycemic Control, and Family Functioning
Family Functioning and Adherence
To examine whether changes in adherence were associated with changes in miscarried helping, family conflict, and acceptance of illness, Pre to Follow-up change scores were generated and correlations calculated (see Table 2). Reductions in P-CBQ scores were significantly associated with improvements in parent- (r = .30, P ≤ .01) and youth- (r = .22, P ≤ .05) reported adherence (P-DSMP). Improvements in P-AIS scores were significant associated with improvements in P-DSMP (r = .28, P ≤ .01) and Y-DSMP (r = .32, P ≤ .01). Finally, improvement in Y-AIS scores was significantly associated with improvement in P-DSMP scores, but not youth report (Table 2).
Table 2.
Change Scores Correlated to Adherence (DSMP) and Glycemic Control (HbA1c).
| Pre to FU difference scores | Parent adherence (P-DSMP) | Youth adherence (Y-DSMP) | Glycemic control (HbA1c) |
|---|---|---|---|
| Parent–miscarried helping (P-HHI) | –.08 | –.14 | .20* |
| Youth–miscarried helping (Y-HHI) | .02 | .01 | .18* |
| Parent–family conflict (P-CBQ) | –.30** | –.22* | .15 |
| Youth–family conflict (Y-CBQ) | .02 | –.06 | .02 |
| Parent–acceptance of illness (P-AIS) | .28** | .32** | –.13 |
| Youth–acceptance of illness (Y-AIS) | .26** | .06 | .07 |
P ≤ .05. **P ≤ .01.
Family Functioning and Glycemic Control
Changes in parent (r = .20, P ≤ .05) and youth (r = .18, P ≤ .05) reported miscarried helping scores (HHI) were significantly associated with changes in Glycemic Control (Table 2).
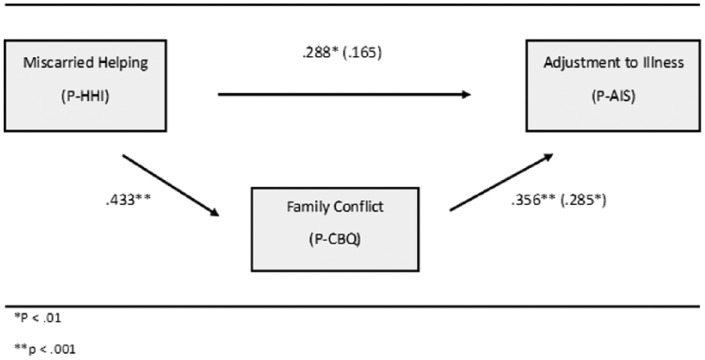
Post Hoc Hypothesis and Analysis
An examination of associations suggested changes in parent-reported family conflict may mediate the relationship between changes in parent reported miscarried helping and adjustment to illness (Figure 5). To test a longitudinal model of the proposed relationships, we calculated Pre to Follow-up change scores for the 3 variables of interest (P-HHI, P-CBQ, P-AIS). Modeling the hypothesized relationships identified full mediation, z = 2.25, P < .0544 (Figure 5). Mediation was further tested through the use of bootstrapping methods.45 Results identified good model fit, F = 7.62, P < .01, and similar full mediation results, z = 2.21, P < .05.
Figure 5.
Family conflict mediating miscarried helping and adjustment to illness.
Conclusions
Our findings provide strong support for the delivery of BFST-D via telehealth. Results suggest the effectiveness of BFST-D can be retained while being delivered in a telehealth format. Our results have important implications for providing behavioral health services to families who may otherwise reside significant distances from qualified treatment providers or have other barriers to receiving care in a traditional clinic setting.
One potential explanation for the effectiveness of BFST-D, regardless of whether it is delivered face-to-face or via telehealth technology, may be the directive, skills-based nature of BFST-D. Many examples of interventions shown to be effective using synchronous audio-visual communications between patients and providers are similar to BFST-D in that they are structured and rely heavily on psychoeducation and direct skills teaching, modeling, and rehearsal to facilitate change.45,46 Whether it is these characteristics or others that facilitate effectiveness when delivering behavioral health care through traditional means or using technology remains unclear. Further research is needed to identify the specific intervention characteristics that predict effectiveness through telehealth delivery.
The current findings provide further support of BFST-D as an effective intervention for youth with T1D in suboptimal glycemic control. The intervention specifically targeted reducing miscarried helping (HHI) and significant improvements were demonstrated from Pre to Follow-up (Figure 1). Furthermore, general family conflict (CBQ) was also reduced from Pre to Follow-up despite not being a direct target of the treatment (Figure 2). Presumably, the skills conveyed through targeting reducing miscarried helping were generalized to reduce overall family conflict. Although caregivers reported improved acceptance of illness (AIS), youth did not. It may be that parents rely on the parent-child relationship as an indicator of their own adjustment to illness. Post hoc mediation analysis suggested that reducing miscarried helping caused improvements in overall family conflict, which contributed to parent acceptance of illness.
A variety of clinical, legal, and practice implications must be considered when adopting the use of technology to deliver health care services in clinical versus research contexts.47 For example, while free and easily accessible to those with high speed Internet connection, the technology used in this study was primarily developed for personal and business applications, has not been approved by most institutions for the communication of protected health information, and is generally not appropriate for adoption in routine clinical practice. Furthermore, behavioral health practitioners must ensure competence in delivering telehealth services. Simply having expertise in the specific intervention being delivered does not ensure that one is adequately trained to deliver the intervention via telehealth technology. Given this, national behavioral and mental health organizations have been developing guidelines for the practice of telehealth.48
Study limitations include participants being predominately white and of middle socioeconomic status. Further studies should examine telehealth delivery of BFST-D to racial and ethnic minorities and to youth and families of lower socioeconomic status residing in other regions or countries. Future research should also consider evaluation of primary outcomes over longer periods of time (eg, 1 or 1.5 year(s) postintervention).
Finding no differences in outcomes across Telehealth and Clinic conditions provides strong support for the use of telehealth to deliver BFST-D to address difficulties known to be associated with adherence problems. Results emphasize the importance of assessing family functioning and implementing interventions to address family functioning in youth with T1D in suboptimal glycemic control.
Footnotes
Abbreviations: ADA, American Diabetes Association; AIS, Acceptance of Illness Scale; ANOVA, analysis of variance; BFST-D, behavioral family systems therapy–diabetes; CBQ, Conflict Behavior Questionnaire Short Form; CONSORT, Consolidated Standards of Reporting Trials; DIF, Demographic Information Form; DSMP, Diabetes Self-Management Profile–Diabetes; FU, follow-up; HHI, Helping for Health Inventory; ITT, intent to treat; P, parent; T1D, type 1 diabetes; Y, youth.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by the American Diabetes Association, Clinical Trial NCT02274103, clinicaltrials.gov.
References
- 1. Cohen DM, Lumley MA, Naar-King S, Partridge T, Cakan N. Child behavior problems and family functioning as predictors of adherence and glycemic control in economically disadvantaged children with type 1 diabetes: a prospective study. J Pediatr Psychol. 2004;29(3):171-184. [DOI] [PubMed] [Google Scholar]
- 2. Ellis DA, Naar-King S, Frey M, Rowland M, Greger N. Case study: feasibility of multisystemic therapy as a treatment for urban adolescents with poorly controlled type 1 diabetes. J Pediatr Psychol. 2003;28(4):287-293. [DOI] [PubMed] [Google Scholar]
- 3. Weissberg-Benchell J, Glasgow AM, Tynan WD, Wirtz P, Turek J, Ward J. Adolescent diabetes management and mismanagement. Diabetes Care. 1995;18(1):77-82. [DOI] [PubMed] [Google Scholar]
- 4. Klafke A, Bartholow Duncan B, Stevens A, et al. The decline in mortality due to acute complications of diabetes mellitus in Brazil, 1991-2010. BMC Pub Health. 2015;15:772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Diabetes Control and Complications Trial Research Group. Effects of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: diabetes control and complications trial. N Engl J Med. 1994;125(2):177-188. [DOI] [PubMed] [Google Scholar]
- 6. Hood KK, Beavers DP, Yi-Frazier J, et al. Psychosocial burden and glycemic control during the first 6 years of diabetes: results from the SEARCH for diabetes in youth study. J Adolesc Health. 2014;55(1);498-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36:1033-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Anderson BJ, Miller B, Auslander WF, Santiago JV. Family characteristics of diabetic adolescents: relationships to metabolic control. Diabetes Care. 1981;4(1):586-594. [DOI] [PubMed] [Google Scholar]
- 9. Wysocki T. Associations among parent-adolescent relationships, metabolic control and adjustment to diabetes in adolescents. J Pediatr Psychol. 1993;18(1):443-454. [DOI] [PubMed] [Google Scholar]
- 10. Harris MA, Greco P, Wysocki T, White NH. Family therapy for adolescents with diabetes: a litmus test for clinically meaningful change. Families Syst Health. 2001;19(1);159-168. [Google Scholar]
- 11. Anderson BJ, Wolpert HA. A developmental perspective on the challenges of diabetes education and care during the young adult period. Patient Couns Health Educ. 2004;53(3):347-352. [DOI] [PubMed] [Google Scholar]
- 12. Anderson BJ, Coyne JC. Miscarried Helping in the Families of Children and Adolescents With Chronic Diseases. Washington, DC: University of Florida Press; 1991. [Google Scholar]
- 13. Drotar D, Bonner MS. Influences on adherence to pediatric asthma treatment: a review of correlates and predictors. J Dev Behav Pediatr. 2009;30(6):574-582. [DOI] [PubMed] [Google Scholar]
- 14. Linkowski DC. A scale to measure acceptance of disability. Rehabilitation Counseling Bull. 1971;14(4):236-244. [Google Scholar]
- 15. Wysocki T, Harris MA, Buckloh LM, et al. Effects of behavioral family systems therapy for diabetes on adolescents’ family relationships, treatment adherence, and metabolic control. J Pediatr Psychol. 2006;31:928-938. [DOI] [PubMed] [Google Scholar]
- 16. Harris MA, Freeman KA, Beers M. Family therapy for adolescents with poorly controlled diabetes: initial test of clinical significance. J Pediatr Psychol. 2009;34:1097-1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wysocki T, Harris MA, Buckloh LM, et al. Randomized, controlled trial of behavioral family systems therapy for diabetes: maintenance and generalization of effects on parent-adolescent communication. Behavior Ther. 2009;39(1):33-46. [DOI] [PubMed] [Google Scholar]
- 18. Newacheck PW, Hughes DC, Stoddard JJ. Children’s access to primary care: differences by race, income, and insurance status. J Pediatr. 1996;91(1):26-32. [PubMed] [Google Scholar]
- 19. Zgibor JC, Songer TJ, Kelsey SF, et al. The association of diabetes specialist care with health care practices and glycemic control in patients with type 1 diabetes: a cross sectional analysis from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care. 2000;23:472-476. [DOI] [PubMed] [Google Scholar]
- 20. Freeborn DK, Pope CR, Davis MA, Mullooly JP. Health status, socioeconomic status, and utilization of outpatient services for members of a prepaid group practice. Med Care. 1997;15:115-128. [DOI] [PubMed] [Google Scholar]
- 21. Connolly VM, Kesson CM. Socioeconomic status and clustering of cardiovascular disease risk factors in diabetic patients. Diabetes Care. 1996;19:419-422. [DOI] [PubMed] [Google Scholar]
- 22. Klein R, Klein BEK, Jensen SC, Moss SE. The relation of socioeconomic factors to the incidence of proliferative diabetic retinopathy and loss of vision. Ophthalmology. 1994;101:68-76. [DOI] [PubMed] [Google Scholar]
- 23. Jacobson AM, Hauser ST, Willett J, et al. Consequences of irregular versus continuous medical follow-up in children and adolescents with insulin-dependent diabetes mellitus. J Pediatr. 1997;131:727-733. [DOI] [PubMed] [Google Scholar]
- 24. Kaufman FR, Halvorson M, Carpenter S. Association between diabetes control and visits to a multidisciplinary pediatric diabetes clinic. Pediatrics. 1999;103:948-951. [DOI] [PubMed] [Google Scholar]
- 25. Sood S, Mbarika V, Jugoo S, et al. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J e-Health. 2007;13:573-590. [DOI] [PubMed] [Google Scholar]
- 26. Horrigan J. Home broadband adoption 2009. Washington, DC: Pew Internet & American Life Project; 2009. [Google Scholar]
- 27. Mulvaney SA, Rothman RL, Lybarger C, Wallston KA. Modeling problem solving with an Internet-based self-management intervention for adolescents with type 1 diabetes. Diabetes. 2009;58(A482):602-604. [Google Scholar]
- 28. Duncan AB, Velasquez SE, Nelse EL. Using videoconferencing to provide psychological services to rural children and adolescents: a review and case example. J Clin Child Adolesc Psychol. 2014;43:115-127. [DOI] [PubMed] [Google Scholar]
- 29. Freeman KA, Duke DC, Harris MA. Behavioral health care for adolescents with poorly controlled diabetes via Skype™: does working alliance remain intact? J Diabetes Sci Technol. 2013;7(3):727-735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Riley AR, Duke DC, Freeman KA, Hood KK, Harris MA. Depressive symptoms in a trial behavior family systems therapy for diabetes: a post hoc analysis of change. Diabetes Care. 2015;38:1435-1440. [DOI] [PubMed] [Google Scholar]
- 31. Harris MA, Freeman KA, Duke DC. Seeing is believing: using Skype® to improve diabetes outcomes in youth. Diabetes Care. 2015;38:1427-1434. [DOI] [PubMed] [Google Scholar]
- 32. Hollingshead AB. Four factor index of social position. New Haven, CT: Yale University; 1975. [Google Scholar]
- 33. Harris MA, Wysocki T, Sadler M, et al. Validation of a structured interview for the assessment of diabetes self- management. Diabetes Care. 2000;23:1301-1304. [DOI] [PubMed] [Google Scholar]
- 34. Teló GH, de Souza MS, Andrade TS, Schaan BD. Comparison between adherence assessments and blood glucose monitoring measures to predict A1c in type 1 diabetes. Diabetol Metab Syndr. 2015;7(suppl 1):A170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Diabetes Research in Children Network Study Group. Performance of the DCA2000 for measurement of HbA1c levels in children with T1DM in a DirecNet outpatient clinical trial. Pediatr Diabetes. 2005;6:13-16. [DOI] [PubMed] [Google Scholar]
- 36. Harris MA, Antal H, Oelbaum R, Buckloh LM, White NH, Wysocki T. Good intentions gone awry: assessing parental “miscarried helping” in diabetes. Families Syst Health. 2008;26(4):393. [Google Scholar]
- 37. Prinz RJ, Foster S, Kent RN, O’Leary KD. Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. J Appl Behav Anal. 1979;12(4):691-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Robin AL, Sharon LF. Problem-solving communication training: a behavioral-family systems approach to parent-adolescent conflict. Adv Child Dev Behav. 1984;3(1):195-240. [Google Scholar]
- 39. Robin AL, Weiss JG. Criterion-related validity of behavioral and self-report measures of problem-solving communication skills in distressed and nondistressed parent-adolescent dyads. Behav Assess. 1980;2(4):339-352. [Google Scholar]
- 40. Felton BJ, Revenson TA, Hinrichsen GA. Stress and coping in the explanation of psychological adjustment among chronically ill adults. Ethics Sci Med. 1984;18(10):889-898. [DOI] [PubMed] [Google Scholar]
- 41. Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Meth. 2002;7(2):147. [PubMed] [Google Scholar]
- 42. Schafer JL. Analysis of Incomplete Multivariate Data. Boca Raton, FL: CRC Press; 1997. [Google Scholar]
- 43. Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol. 1982;13(1):290-312. [Google Scholar]
- 44. Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(1):717-731. [DOI] [PubMed] [Google Scholar]
- 45. Stinson J, Wilson R, Gill N, Yamada J, Holt J. A systematic review of Internet-based self-management interventions for youth with health conditions. J Pediatr Psychol. 2009;35:495-510. [DOI] [PubMed] [Google Scholar]
- 46. Van Allen J, McGrath Davis A, Lassen S. The use of telemedicine in pediatric psychology: research review and current applications. Child Adolesc Psychiatr Clin N Am. 2011; 20:55-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Richardson LK, Frueh CB, Grubaugh AL, Egede L, Alhai JD. Current directions in videoconferencing tele-mental health research. Clin Psychol. 2009;16(3):323-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. American Psychological Association. Guidelines for the practice of telepsychology. 2013. Available at: http://www.apapracticecentral.org/ce/guidelines/telepsychology-guidelines.pdf?_ga=1.184221221.227197664.1434995171. Accessed February 18, 2016.