Abstract
Background
S. pneumoniae is the leading cause of acute bacterial meningitis (ABM) in children. Vaccination using the 10-valent conjugate vaccine (PCV-10) was recently introduced into the National Immunization Program in Mozambique, but data on serotype coverage of this vaccine formulation are scarce. In this study, we investigated the serotype distribution and antimicrobial resistance of isolates of S. pneumoniae causing ABM in children < 5 years at the two largest hospitals in Mozambique.
Methods
Between March 2013 and March 2014, a total of 352 cerebrospinal fluid (CSF) samples were collected from eligible children, of which 119 (33.8 %) were positive for S. pneumoniae. Of these, only 50 samples met the criteria for serotyping and were subsequently serotyped using sequential multiplex PCR (SM-PCR), but 15 samples were non-typable.
Results
The most common serotypes of S. pneumoniae were 1 (18.2 %), 5 (15.2 %), 14 (12.1 %), 9 V (12.1 %), 23 F (9.1 %), 6A (9.1 %), 4 (9.1 %) and 6B (6.1 %). Serotypes 1, 5, 9 V, 6A and 12 were mostly prevalent in Northern Mozambique, while serotypes 23 F, 4, 6B, 3 and 15B were predominant in Southern. Serotype coverage of PCV-10 and PCV-13 vaccine formulations were 81.8 % and 93.9 %, respectively. Serotypes 1, 3, 4, 6B, 14, 23 F were resistant to penicillin and sensitive to ceftriaxone.
Conclusions
Our findings shows that changing the current in use PCV-10 vaccine formulation to PCV-13 formulation might increase substantially the protection against invasive strains of S. pneumoniae as the PCV-10 vaccine formulation does not cover the serotypes 3 and 6A, which are prevalent in Mozambique.
Keywords: Pneumococcal meningitis, Mozambique
Background
Streptococcus pneumoniae is the leading cause of otitis media, sinusitis, bacteremia, pneumonia, meningitis and sepsis in children. Worldwide, an estimated 1.6 million of children under the age of 5 die every year as a consequence of S. pneumoniae related diseases [1–3]. The elderly and immunosuppressed individuals are also vulnerable [4].
Meningitis is a serious consequence of invasive disease caused by S. pneumoniae, leading to more than 100,000 deaths annually in children under the age of 5 [2, 3]. Recent estimates demonstrate that up to 90 % of these deaths occurs in resource-limited settings, mostly in sub-Saharan Africa and Asia [3, 5].
Pneumococcus is an antigenically complex bacteria and currently, more than 95 serotypes have been described [6–8]. These serotypes differ in term of pathogenesis, target organ, age, geographical distribution, virulence and susceptibility to antibiotics [9].
Globally, the most common serotypes are 1, 5, 14, 6A, 6B, 19 F and 23 F, of which serotypes 1, 5, 6A and 14 occur predominantly in developing countries, whereas serotypes 19 F, 6B, 23 F and 14 occur mostly in developed countries [10, 11]. In recent years, the rapid spread of antimicrobial resistant S. pneumoniae strains and the emergence of multidrug-resistant strains (MDRSP), has increased the global concern for pneumococcal infection [12].
In regard to Mozambique, data on serotype distribution of S. pneumoniae are scarce, and with the exception of one study conducted in Manhiça district, a rural area in southern Mozambique [13], no other study has yet been conducted. Therefore, data from Manhiça district has few limitations, such as, they are more than 10 years old and, taken into consideration that Manhiça is a rural village, these data are difficult to generalize to the entire country given the size and geographic diversity of Mozambique, particularly in terms of climate, demographic, socio-economic and cultural aspects [14]. In this regard, it is possible that serotype distribution and antimicrobial sensitivity of S. Pneumoniae may vary in different regions of the country. This is particularly important in a time in which Mozambique recently introduced the PCV-10 vaccine formulation into the Extended Program of Immunization.
In this context, this study was conducted with the purpose of determining the frequency and distribution of capsular serotypes of S. pneumoniae causing acute bacterial meningitis in children under 5 years of age at the two largest hospitals in the country, Maputo Central Hospital, in the Southern region, and Nampula Central Hospital, in the Northern region of the country. This study will generate information on the serotype coverage of pneumococcal conjugate vaccine formulations and present baseline data for future assessments of the impact of pneumococcal vaccination in Mozambique.
Methods
Study design, study sites and target population
This study was implemented as part of the routine sentinel surveillance system for pediatric acute bacterial meningitis (ABM), implemented by the National Institute of Health (INS) in Mozambique. The sentinel surveillance system for ABM was established in March 2013 at two regional hospitals, Maputo Central Hospital (HCM) and Nampula Central Hospital (HCN). Both are regional referral hospitals and offer several specialized medical services, including inpatient and outpatient care across all age groups.
The HCN is situated in Nampula province, the most populous in the country, has 23 districts with a total of 3,985,613 inhabitants [14]. The paediatric ward at HCN has 184 beds. The HCM is situated in Maputo city, the capital of Mozambique, with a total of 1,766,823 inhabitants [14]. HCM is the largest hospital in the country, with 322 beds in the paediatric ward. All children admitted to these health facilities with clinical presentation of ABM between March 2013 and March 2014 were eligible for enrolment.
Case definition
Per WHO guidelines, suspected case of ABM is defined as a child aged < 5 years with sudden onset of fever (>38.5 °C rectal or 38.0 °C axillary) and at least 1 of the following signs: neck stiffness or flaccid neck, bulging fontanel, convulsion, irritability, or drowsiness.
Samples collection and questionnaire
Upon admission, lumbar puncture (LP) was aseptically performed by a trained pediatrician on each child who met the case definition for ABM.
A standard case investigation form was used to collect clinical and demographic data.
Laboratory testing
Bacteriological testing of CSF samples at sentinel site
As part of routine surveillance for ABM, cerebrospinal fluid (CSF) samples were initially cultured at the sentinel sites onto 5 % sheep blood agar plates (MAST, Merseyside, UK) and all growing isolates were stored between 2-8 °C and shipped to the National Reference Microbiology Laboratory (NRML) in Maputo for further testing.
Identification of S. pneumoniae by culture at NRML
At the NRML, all isolates received from the sentinel site were frozen at -80 °C until further testing. Isolates were recovered by plating onto 5 % sheep blood and chocolate agar plates (MAST, Merseyside, UK). Twenty-four hours after incubation at 35 ° C ±2 ° C with 5 % of CO2, bacterial isolates were identified by colony morphologic analysis and growth requirement. Pneumococci were identified based on morphological features in Gram stain, optochin susceptibility test (OXOID – DD1 OPTOCHIN, Basingstoke, England) and bile solubility (BD – BBL Desoxycholate Reagent Droppers, Becton Dickinson and Company, USA) [15]. All isolates of S. pneumoniae, were used for molecular serotyping.
DNA extraction from CSF samples and S. pneumoniae isolates
Two hundred microliters of all CSF samples and isolates of S. pneumoniae previously identified by culture were used for DNA extraction. DNA was extracted using either Biopour mini kit (BIOPUR, Biometrix diagnostic, Brazil), or High pure PCR template kit (Roche Diagnostics Corporation, US), according to the manufacturer’s instructions. Total DNA was eluted in 200 μl of appropriated elution buffer and stored at −20 °C until use.
Diagnosis of S. pneumoniae using PCR
Molecular diagnosis of S. pneumoniae was performed as part of the routine diagnosis of meningitis within the national surveillance system for pediatric ABM, implemented by the National Institute of Health. Routinely, the molecular diagnosis of meningitis is performed using M-qPCR. This assay was based on SYBER detection system (Platinum SYBR Green qPCR Supermix-UDG, Invitrogen, California, UK) using the LightCycler 2.0 instrument (Roche Diagnostic GmbH, Mannheim, Germany). This detects simultaneously Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae using a set of specific primers as described by Ke et al., 2000 [16]; Corless et al., 2001[17] and El Aila et al., 2011 [18].
Serotyping of S. pneumoniae
Serotyping was performed on all isolates of S. pneumoniae and all CSF samples from PCR positive children, whose cycle threshold (ct) value was lower than 30. CSF samples from PCR positive children whose ct value was higher than 30, were excluded, due to insufficient DNA for serotyping. Serotyping was performed using the Sequential multiplex PCR (SM-PCR), adapted for regional algorithm, and covering the 39 most common serotypes involved in the etiology of invasive pneumococcal diseases (IPD) in Africa, and grouped into 8 multiplex PCR reactions [19]. The capsular polysaccharide (cps) was used as internal control. The reaction was performed in a final volume of 25 μl. Each reaction mix contained buffer solution at 2x, 0.2 mM concentration of each deoxynucleoside triphosphate (dNTPs), reaction buffer 10x (100 mM of Tris-HCl, pH 8.5 and 500 mM of KCl), 1.7 mM of MgCl2, 1.5U⁄ μl of Taq DNA polymerase, primers at the concentration from 0.1 to 0.5 uM and 5 μl of template DNA. The PCR assays were performed in a thermocycler (GeneAmp PCR System 9700, PE Applied Biosystems). Samples were amplified as follows: an initial denaturation step at 95 °C for 15 min, followed by 35 cycles at 95 °C for 30 seconds (denaturation), 54 °C for 90 seconds (annealing) and 72 °C for 1 min (elongation). After amplification, PCR products were analyzed by gel electrophoresis.
Antimicrobial susceptibility test
Minimum inhibitory concentrations (MICs) to penicillin, erythromycin, vancomycin, trimethoprim-sulfamethoxazole, tetracycline and ceftriaxone were determined using E-test® (Biomereux, SA) strips. The results were interpreted according to Clinical and Laboratory Standards Institute guidelines (CLSI, 2014) [20]. The reference strain S. pneumoniae ATCC 49619 was used as the quality control.
Statistical analysis
Data were entered into a database developed using Epi Info version 3.5.4 (CDC U.S.A.) and was analyzed using SPSS statistical software version 20 (IBM, U.S.A.). Categorical variables were reported as proportion and statistical significance differences were assessed using Pearson Chi-square test with a significance level of less than 0.05.
Results
General characteristics of study participants
Between March 2013 and March 2014, a total of 352 CSF samples were collected from children clinically suspected of ABM who were admitted to two referral hospitals. The median age of study participants was 9 months (IQR 4 - 30 months) and 52.8 % (186/352) of them were male. More than half of the children were aged less than 12 months, while children of the age group 12-23 months and 24-59 months comprised 11 % (39/352) and 31 % (109/352) of the study group (Table 1). Children from Nampula Central Hospital, represented 73.6 % from the sample (n = 259), while children from Maputo Central Hospital represented 26.4 % (n = 93). Children from HCM and HCN were similar in term of their age (median: 17.4 months for HCN and 20.3 months for HCN, respectively) and gender (male gender = 51.6 % in HCM and 53.3 % in HCN, respectively). S. pneumoniae was identified in a total of 119 (33.8 %) samples, of which 17 were initially identified by culture and the remaining 102 were identified by PCR. Serotyping for S. pneumoniae using SM-PCR was performed in a total of 50 samples, comprising the 17 isolates of S. pneumoniae identified by culture and 33 PCR positive CSF samples for which their ct value was inferior to 30. Most of children with positive result for S. pneumoniae and children with typable CSF sample were aged below 12 months, following the same pattern of enrolled children (Table 1).
Table 1.
Age and gender distribution of enrolled patients, patients with positive and negative CSF results and patients with typable CSF samples
| Characteristics | Total (n = 352) | S. pneumoniae positive (n = 119) | Children with typable CSF (n = 33) |
|---|---|---|---|
| Age | |||
| 0-11 months | 204 (58.0 %) | 77 (64.7 %) | 24 (72.7 %) |
| 12-23 months | 39 (11.0 %) | 18 (15.1 %) | 3 (9.1 %) |
| 24-59 months | 109 (31.0 %) | 24 (20.2 %) | 6 (18.2 %) |
| Gender | |||
| Male | 186 (52.8 %) | 66 (55.5 %) | 13 (39.4 %) |
| Female | 166 (47.2 %) | 53 (44.5 %) | 20 (60.6 %) |
Serotype distribution and coverage rate of pneumococcal vaccine formulations
Of the 50 samples for which serotyping was performed, a total of 33 (66.0 %) were typable and their corresponding serotype was identified, the remaining 17 samples were not-typeable (SM-PCR NT), as shown in Fig. 1. The most frequent serotypes were 1 (18.2 %, 6/33), 5 (15.2 %, 5/33), 14 (12.1 %, 4/33), 9 V (12.1 %, 4/33), 23 F (9.1 %, 3/33), 6A (9.1 %, 3/33), 4 (9.1 %, 3/33), 6B (6.1 %, 2/33), 12 (3.0 %, 1/33), 15B (3 %, 1/33) and 3 (3.0 %, 1/33). Serotype distribution of children older than 2 years old was significantly different of that of children younger than 2 years old (Chi-Square = 28; p = 0.001).
Fig. 1.
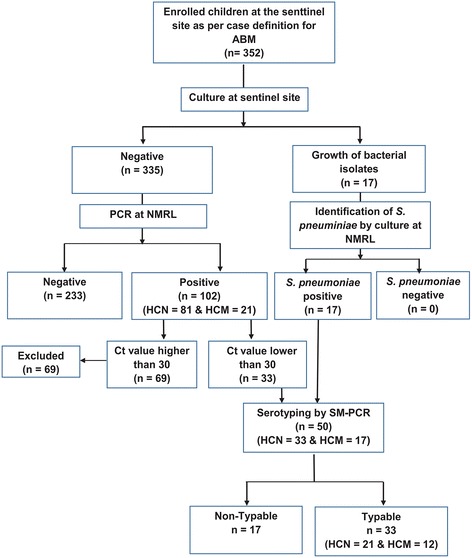
Flowchart of sample collection and testing. The flow chart depicts the number of CSF samples collected from of children under 5 years old at each sentinel site and tested at sentinel site and NMRL between March 2013 and study March 2014. Abbreviations. CSF: Cerebrospinal fluid; HCM: Hospital Central de Maputo; HCN: Hospital Central de Nampula; SM-PCR: sequential multiplex polymerase chain reaction; NMRL: National Reference Microbiology Laboratory
Figure 2 shows that the rate of vaccine coverage against the serotypes of S. pneumoniae causing pediatric meningitis in Mozambique was 48.5 % (16/33), 81.8 % (27/33), and 93.9 % (31/33) for PCV-7, PCV-10, and PCV-13, respectively.
Fig. 2.
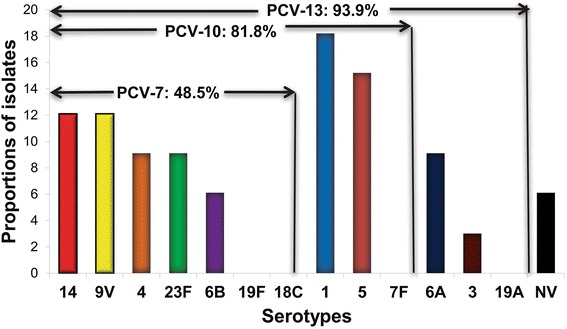
Distribution of serotypes of S. pneumoniae and vaccine coverage rates for PCV-7, PCV-10 and PCV-13 vaccine formulations. Each bar represents the relative frequency of each serotype of S. pneumoniae. The value in the arrows above the bars depicts the vaccine coverage rates for PCV-7, PCV-10 and PCV-13, respectively NV, serotypes not included in 13-valent pneumococcal conjugate vaccine. NV, nonvaccine serotypes (serotypes 12 and 15B)
The serotypes 1, 5, 9 V, 6A and 12 were mostly found in Northern Mozambique, while serotypes 23 F, 4, 6B, 3 and 15B were reported mostly in the Southern Mozambique (Fig. 3). In addition, the non-PCV-10 serotype 3 and 15B (frequency of 3.0 % for both isolates) were found in Maputo city, situated in southern Mozambique, while the non-PCVs serotype 12 (frequency of 3.0 %) was found in Nampula city, situated in northern part of the country.
Fig. 3.
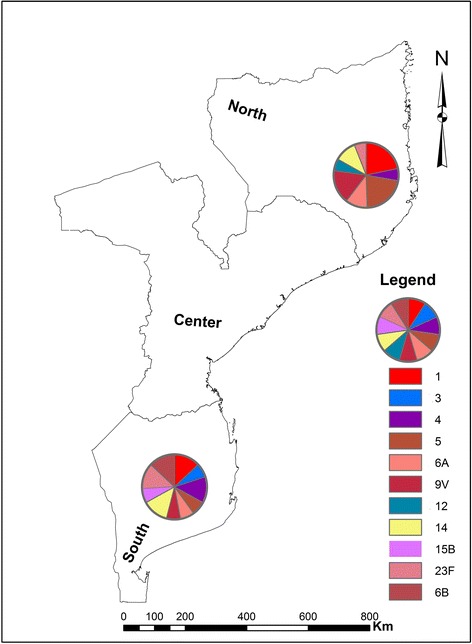
Distribution of serotypes of S. pneumoniae stratified by region, between March 2013 and March 2014. Figure depicts the distribution of S. pneumoniae serotypes in the southern (HCM) and northern (HCN). Each color represents one serotype
Antimicrobial susceptibility profile of isolates of S. pneumoniae
Table 2 summarises the antibiotic susceptibility profile of pneumococcal serotypes, and showed that 88.2 % of serotypes were resistant to penicillin (MIC > 0. 125 μg/mL), according to the revised CLSI breakpoints for parenteral penicillin (resistant ≥ 0.12 mg/mL for meningitis isolates), while for ceftriaxone all serotypes were susceptible (100 %). The susceptibility rate for erythromycin, vancomycin, chloramphenicol and tetracycline were 76.5 %, 88.2 % and 64.7 %, 35.3 %, respectively.
Table 2.
Antibiotic susceptibility profile of S. pneumoniae serotypes
| Serotype | No. of isolates | MIC (μg/ml) ofa | ||||||
|---|---|---|---|---|---|---|---|---|
| PEN (n/N) | ERY (n/N) | SXT (n/N) | VANC (n/N) | CRO (n/N) | TCY (n/N) | CHL (n/N) | ||
| Ra | R | R | R | R | R | R | ||
| 14 | 4 | 4/4 | 1/4 | 4/4 | 0/4 | 0/4 | 3/4 | 0/4 |
| 6A | 2 | 2/2 | 0/2 | 2/2 | 2/2 | 0/2 | 2/2 | 2/2 |
| 4 | 2 | 2/2 | 1/2 | 2/2 | 0/2 | 0/2 | 1/1 | 1/2 |
| 3 | 1 | 1/1 | 0/1 | 1/1 | 0/1 | 0/1 | 1/1 | 0/1 |
| 1 | 1 | 1/1 | 0/1 | 1/1 | 0/1 | 0/1 | 0/1 | 0/1 |
| 15B | 1 | 0/1 | 0/1 | 1/1 | 0/1 | 0/1 | 0/1 | 1/1 |
| 23 F | 2 | 2/2 | 2/2 | 2/2 | 0/2 | 0/2 | 2/2 | 1/1 |
| 9 V | 1 | 0/1 | 0/1 | 1/1 | 0/1 | 0/1 | 0/1 | 0/1 |
| NT | 3 | 3/3 | 0/3 | 3/3 | 0/3 | 0/3 | 2/3 | 1/3 |
| Total | 17 | 15/17 | 4/17 | 17/17 | 2/17 | 0/17 | 11/17 | 6/17 |
PEN, penicillin; ERY, erythromycin, SXT, trimethoprim-sulfamethoxazole; VANC, vancomycin; CRO, ceftriaxone; TCY, tetracycline; CHL, chloramphenicol. NT, not typeable
aResistant
Discussion
In this study we described for the first time the serotype distribution of S pneumoniae at the two largest hospitals in Mozambique, and provided baseline data for further assessments of the impact of pneumococcal vaccination.
Findings from our study show that in Mozambique, the predominant serotypes of S. pneumoniae causing ABM in children aged <5 year were 1, 5, 14, 9 V, 23 F, 6A and 4. This finding is similar to a recent study conducted in South Africa [21], but is different than that reported in studies conducted in Nigeria [22] Burkina Faso and Togo, which found that serotypes 14, 1 and 18 were the most prevalent [23].
Of note, our data suggests that the distribution S. pneumoniae serotypes in the Northern differs of that in the Southern, as shown in the Fig. 3. However, these findings should be interpreted with caution because of the small size of our sample, which is not representative of the entire population in the country. Studies with larger size should be conducted to confirm these results.
In regard to serotype coverage of PCV-10, data from our study show that this vaccine formulation covers 81.8 % (27/33) of S. pneumoniae strains identified in this study. Similar results were found in a previous study conducted in Manhiça District, a rural community situated in southern Mozambique [13], South Africa [21], and other sub-Saharan countries situated in the African meningitis belt, such as Burkina Faso, Togo [24, 25] and Nigeria [22]. Our data show that PCV-13 vaccine formulation would increase the serotype coverage from the current 81.8 %, to 93.9 % because PCV-13 formulation provide added protection against the serotypes 3, 6A and 19A.
Our results also show that serotype 1 was the most common cause of pneumococcal meningitis in Mozambique, which is in agreement with findings from other Sub-Saharan Africa countries [13, 22, 24]. The high prevalence of serotype 1 might be a consequence of a previous epidemics caused by this serotype in Mozambique, as has been reported in other settings, such as Ghana [10].
Additionally, data from our study show that serotype 3 occurs in children, although with low frequency. This is relevant because serotype 3 is an important cause of invasive disease in children [9] and has been associated with high fatality rates [26, 27].
Serotypes 12 and 15B, known as non-vaccine serotypes (NV) occurred in 6 % of the children. This is an important finding, because these serotypes are not included in the existing PCVs vaccine formulations. Similar findings were reported in studies conducted in South Africa and other sub-Saharan Africa countries [21, 28].
In regards to antimicrobial susceptibility profile, resistance of S. pneumoniae to penicillin was high, but this result cannot be generalized due to the small number of isolates tested in this study. This finding is in agreement with previous studies, which also suggest that the rate of resistance of S. pneumoniae to penicillin and other antibiotic classes is increasing [29–34]. Resistance to penicillin was also observed for serotypes 1, 3, 4, 6B, 14, 23 F. These results are similar to those reported in recent studies conducted in South Africa [21], Algeria [33] and China [35].
An important finding of this study was the fact that two S. pneumoniae strains belonging to serotype 6A presented a decreased susceptibility to vancomycin (MIC = 1.52 μg/mL, for both). Our results corroborate finding from a recent study conducted by Ataee et al, 2014 in Iran, which reported emergence of vancomycin tolerant, strains of S. pneumoniae. In his report, Ataee et al, 2014 found that 8 % (4/46) of S. pneumoniae strains presented a lower susceptibility to vancomycin as measured by assessment of MIC [36]. In fact, the number of studies reporting the emergence of meningitis caused by S. pneumoniae strains that are tolerant to vancomycin is increasing [37, 38]. These patients have been shown to have a poorer survival rate than patients with meningitis caused by nontolerant strains [37, 38]. Another study conducted by Sanaei et al found that among S. pneumoniae carrier’s children, the proportion of S. pneumoniae strains resistant to vancomicin was 1.5 % [39]. Altogether, this represents an important warning that vancomycin resistant or tolerant strains of S. pneumoniae are emerging as a serious public health threats.
We found that 17 out of 50 isolates were not-typeable. The reasons why these samples were not-typeable are unknown, however, molecular serotyping as it’s considered the gold standard method for serotyping. Moreover, multiplex PCR has been shown to be more accurate in determining the serotype of S. penumoniae as compared to serological methods [22, 40]. In term of sensitivity of this method, our sequential multiplex PCR (SM-PCR), was adapted for regional algorithm, and covers the 39 most common serotypes involved in the etiology of invasive pneumococcal diseases (IPD) in Africa. We argue that emerging isolates in Africa belonging to some other serotypes, not covered by the 39 serotypes scheme may be present and would need further consideration.
To our knowledge, this is the first description of S. pneumonieae serotype distribution in Northern Mozambique.
We would like to acknowledge some limitations of our study, which may influence the interpretation of the results and extrapolation to the entire population. For example, the relatively small size of our sample, in particular from Maputo Central Hospital might have influenced our results and findings, in particular, the number of strains used for determining the antibiotic susceptibility rate was very small. In addition, the information was incomplete in several of the standard case investigation forms such as vaccination status.
Conclusion
Our study provides preliminary findings on serotype distribution of S. pneumoniae causing ABM in Southern and Northern Mozambique showing that the serotype coverage of the recently introduced PCV-10 vaccine formulation against the serotypes of S. pneumoniae circulating in Mozambique is 81.8 %, as opposed to the coverage of 93.9 % if we were using PCV-13 vaccine formulation, suggesting that changing from the currently in use PCV-10 formulation to PCV-13 can save additional lives. Lower coverage of PCV-10 is attributed to the emergence of non-PCV-10 serotypes 3 and 6A.
Abbreviations
ABM, acute bacterial meningitis; ATCC, american type culture collection; CLSI, laboratory standards institute guidelines; CSF, cerebrospinal fluid; ct, cycle threshold; DNA, deoxyribonucleic acid; dNTP, deoxynucleoside triphosphate; HCN, nampula central hospital; INS, National Institute of Health; IPD, invasive pneumococcal diseases; IQR, interquartile range; LP, lumbar puncture; MDRSP, multidrug-resistant strains; MIC, minimum inhibitory concentration; M-qPCR, multiplex qualitative polymerase chain reaction; NRML, national reference microbiology laboratory; PCV-10, ten-valent conjugate vaccine; PCV-13, thirteen -valent conjugate vaccine; SM-PCR NT, not-typeable by sequential multiplex polymerase chain reaction; SM-PCR, sequential multiplex polymerase chain reaction; UDG, uracil DNA glycosylase; UFCSPA, Universidade Federal de Ciências de Saúde de Porto Alegre
Acknowledgements
We thank Siasa Mendes and Celso Gabriel of the bacteriology laboratory of the Hospital Central de Nampula (HCN), Aventina Artur Macuàcua and Timótio Bejamim of the bacteriology laboratory of the Hospital Central da Beira (HCB), and Raul Vaz and Calvina Langa of the bacteriology laboratory of the Hospital Central de Maputo, for culturing and identifying bacterial isolates. We also thank Mulaja Kabeya Etienne, Moisés Sithole, and Eugénia Macassa for collecting samples and completing necessary forms. We extend our thanks to all our colleagues at the National Reference Microbiology Laboratory (NRML) who tested the samples.
Funding
Funding provided by WHO Reference: 2014405143-0, creation DFC to support HIB & Surveillance System.
Availability of data and materials
All relevant data are within the paper.
Authors’ contributions
ESG, TFZ, IM, AMM, AAN, CEC, GCP, and CBS worked together on data collection. AAN and VVC performed molecular experiments. AAN and ESG wrote the manuscript. JC, CD VVC, CEC, IM, TFZ, CBS, MOM, AMM, CEC and MOM contributed to the design and writing of the manuscript. ESG and AAN performed statistical analysis. MOM, VVC, JC, CD, CEC, TFZ, and IM reviewed the manuscript. All authors have read and approved the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Our manuscript does not present any individual person's data, however, consent to participate was obtained from each participant as state in the ethics statement section.
Ethics approval and consent to participate
The study was approved by the Mozambican National Bioethics Committee (Ref #: IRB00002657). Verbal consent was obtained from the legal representative of each child per the requirements of the routine sentinel surveillance system for acute bacterial meningitis.
Contributor Information
Aquino Albino Nhantumbo, Phone: +258-21311038, FAX: +258-21311038, Email: aquinoalbinonhantumbo@yahoo.com.br.
Eduardo Samo Gudo, Email: esamogudojr@gmail.com.
Juliana Caierão, Email: julianaca@ufcspa.edu.br.
Alcides Moniz Munguambe, Email: mguambendole@yahoo.com.br.
Charlotte Elizabeth Comé, Email: lottacome@gmail.com.
Tomás Francisco Zimba, Email: zimbatf@gmail.com.
Milton Ozório Moraes, Email: mmoraes@fiocruz.br.
Cícero Dias, Email: cicero@ufcspa.edu.br.
Vlademir Vicente Cantarelli, Email: vlademir@feevale.br.
References
- 1.Greenwood B. The epidemiology of pneumococcal infection in children in the developing world. Philos Trans R Soc Lond B Biol Sci. 1999;354(1384):777–85. doi: 10.1098/rstb.1999.0430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mook-Kanamori B, Geldhoff M, Troost D, van der Poll T, van de Beek D. Characterization of a pneumococcal meningitis mouse model. BMC Infect Dis. 2012;12:71. doi: 10.1186/1471-2334-12-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Brien KL, Wolfson LJ, Watt JP, Henkle E, Deloria-Knoll M, McCall N, et al. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet. 2009;374(9693):893–902. doi: 10.1016/S0140-6736(09)61204-6. [DOI] [PubMed] [Google Scholar]
- 4.Black S, France EK, Isaacman D, Bracken L, Lewis E, Hansen J, et al. Surveillance for invasive pneumococcal disease during 2000-2005 in a population of children who received 7-valent pneumococcal conjugate vaccine. Pediatr Infect Dis J. 2007;26(9):771–7. doi: 10.1097/INF.0b013e318124a494. [DOI] [PubMed] [Google Scholar]
- 5.Cornick JE, Harris SR, Parry CM, Moore MJ, Jassi C, Kamng'ona A, et al. Genomic identification of a novel co-trimoxazole resistance genotype and its prevalence amongst Streptococcus pneumoniae in Malawi. J Antimicrob Chemother. 2014;69(2):368–74. doi: 10.1093/jac/dkt384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calix JJ, Porambo RJ, Brady AM, Larson TR, Yother J, Abeygunwardana C, et al. Biochemical, genetic, and serological characterization of two capsule subtypes among Streptococcus pneumoniae Serotype 20 strains: discovery of a new pneumococcal serotype. J Biol Chem. 2012;287(33):27885–94. doi: 10.1074/jbc.M112.380451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bratcher PE, Kim KH, Kang JH, Hong JY, Nahm MH. Identification of natural pneumococcal isolates expressing serotype 6D by genetic, biochemical and serological characterization. Microbiology. 2010;156(Pt 2):555–60. doi: 10.1099/mic.0.034116-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park IH, Pritchard DG, Cartee R, Brandao A, Brandileone MC, Nahm MH. Discovery of a new capsular serotype (6C) within serogroup 6 of Streptococcus pneumoniae. J Clin Microbiol. 2007;45(4):1225–33. doi: 10.1128/JCM.02199-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hausdorff WP, Feikin DR, Klugman KP. Epidemiological differences among pneumococcal serotypes. Lancet Infect Dis. 2005;5(2):83–93. doi: 10.1016/S1473-3099(05)70083-9. [DOI] [PubMed] [Google Scholar]
- 10.Leimkugel J, Adams Forgor A, Gagneux S, Pfluger V, Flierl C, Awine E, et al. An outbreak of serotype 1 Streptococcus pneumoniae meningitis in northern Ghana with features that are characteristic of Neisseria meningitidis meningitis epidemics. J Infect Dis. 2005;192(2):192–9. doi: 10.1086/431151. [DOI] [PubMed] [Google Scholar]
- 11.Yaro S, Lourd M, Traore Y, Njanpop-Lafourcade BM, Sawadogo A, Sangare L, et al. Epidemiological and molecular characteristics of a highly lethal pneumococcal meningitis epidemic in Burkina Faso. Clin Infect Dis. 2006;43(6):693–700. doi: 10.1086/506940. [DOI] [PubMed] [Google Scholar]
- 12.Organization. WH. Antimicrobial resistance. Global Report on Surveillance, 2014. (Accessed in December, 2014).
- 13.Valles X, Flannery B, Roca A, Mandomando I, Sigauque B, Sanz S, et al. Serotype distribution and antibiotic susceptibility of invasive and nasopharyngeal isolates of Streptococcus pneumoniae among children in rural Mozambique. Trop Med Int Health. 2006;11(3):358–66. doi: 10.1111/j.1365-3156.2006.01565.x. [DOI] [PubMed] [Google Scholar]
- 14.INE. Localizacao dos Hospitais Centrais em Mocambique. Instituto nacional de estatística (http://www.ine.gov.mz/) (Acessed in 2014). 2007.
- 15.Arbique JC, Poyart C, Trieu-Cuot P, Quesne G, Carvalho Mda G, Steigerwalt AG, et al. Accuracy of phenotypic and genotypic testing for identification of Streptococcus pneumoniae and description of Streptococcus pseudopneumoniae sp. nov. J Clin Microbiol. 2004;42(10):4686–96. doi: 10.1128/JCM.42.10.4686-4696.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ke D, Menard C, Picard FJ, Boissinot M, Ouellette M, Roy PH, et al. Development of conventional and real-time PCR assays for the rapid detection of group B streptococci. Clin Chem. 2000;46(3):324–31. [PubMed] [Google Scholar]
- 17.Corless CE, Guiver M, Borrow R, Edwards-Jones V, Fox AJ, Kaczmarski EB. Simultaneous detection of Neisseria meningitidis, Haemophilus influenzae, and Streptococcus pneumoniae in suspected cases of meningitis and septicemia using real-time PCR. J Clin Microbiol. 2001;39(4):1553–8. doi: 10.1128/JCM.39.4.1553-1558.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El Aila NA, Tency I, Claeys G, Verstraelen H, Deschaght P, Decat E, et al. Comparison of culture with two different qPCR assays for detection of rectovaginal carriage of Streptococcus agalactiae (group B streptococci) in pregnant women. Res Microbiol. 2011;162(5):499–505. doi: 10.1016/j.resmic.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 19.da Gloria CM, Pimenta FC, Jackson D, Roundtree A, Ahmad Y, Millar EV, et al. Revisiting pneumococcal carriage by use of broth enrichment and PCR techniques for enhanced detection of carriage and serotypes. J Clin Microbiol. 2010;48(5):1611–8. doi: 10.1128/JCM.02243-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.CLSI. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: 34th informational supplement. Wayne, PA: Clinical and Laboratory Standards Institute, M100–S24. . 2014.
- 21.von Gottberg A, Cohen C, de Gouveia L, Meiring S, Quan V, Whitelaw A, et al. Epidemiology of invasive pneumococcal disease in the pre-conjugate vaccine era: South Africa, 2003-2008. Vaccine. 2013;31(38):4200–8. doi: 10.1016/j.vaccine.2013.04.077. [DOI] [PubMed] [Google Scholar]
- 22.Collard JM, Alio Sanda AK, Jusot JF. Determination of pneumococcal serotypes in meningitis cases in Niger, 2003-2011. PLoS One. 2013;8(3) doi: 10.1371/journal.pone.0060432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gessner BD, Sanou O, Drabo A, Tamekloe TA, Yaro S, Tall H, et al. Pneumococcal serotype distribution among meningitis cases from Togo and Burkina Faso during 2007-2009. Vaccine. 2012;30(Suppl 6):G41–5. doi: 10.1016/j.vaccine.2012.10.052. [DOI] [PubMed] [Google Scholar]
- 24.Mueller JE, Yaro S, Ouedraogo MS, Levina N, Njanpop-Lafourcade BM, Tall H, et al. Pneumococci in the African meningitis belt: meningitis incidence and carriage prevalence in children and adults. PLoS One. 2012;7(12) doi: 10.1371/journal.pone.0052464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Traore Y, Tameklo TA, Njanpop-Lafourcade BM, Lourd M, Yaro S, Niamba D, et al. Incidence, seasonality, age distribution, and mortality of pneumococcal meningitis in Burkina Faso and Togo. Clin Infect Dis. 2009;48(Suppl 2):S181–9. doi: 10.1086/596498. [DOI] [PubMed] [Google Scholar]
- 26.Henriques B, Kalin M, Ortqvist A, Olsson Liljequist B, Almela M, Marrie TJ, et al. Molecular epidemiology of Streptococcus pneumoniae causing invasive disease in 5 countries. J Infect Dis. 2000;182(3):833–9. doi: 10.1086/315761. [DOI] [PubMed] [Google Scholar]
- 27.Mothibeli KM, du Plessis M, von Gottberg A, de Gouveia L, Adrian P, Madhi SA, et al. An unusual pneumococcal sequence type is the predominant cause of serotype 3 invasive disease in South Africa. J Clin Microbiol. 2010;48(1):184–91. doi: 10.1128/JCM.01011-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375(9730):1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 29.Mokaddas EM, Rotimi VO, Albert MJ. Increasing prevalence of antimicrobial resistance in Streptococcus pneumoniae in Kuwait: implications for therapy. Microb Drug Resist. 2007;13(4):227–33. doi: 10.1089/mdr.2007.774. [DOI] [PubMed] [Google Scholar]
- 30.Anagaw B, Gezachew M, Biadgelgene F, Anagaw B, Geleshe T, Taddese B, et al. Antimicrobial susceptibility patterns of Streptococcus pneumoniae over 6 years at Gondar University Hospital, Northwest Ethiopia. Asian Pac J Trop Biomed. 2013;3(7):536–41. doi: 10.1016/S2221-1691(13)60109-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Waisbourd-Zinman O, Bilavsky E, Tirosh N, Samra Z, Amir J. Penicillin and ceftriaxone susceptibility of Streptococcus pneumoniae isolated from cerebrospinal fluid of children with meningitis hospitalized in a tertiary hospital in Israel. Isr Med Assoc J. 2010;12(4):225–8. [PubMed] [Google Scholar]
- 32.Jones RN, Flonta M, Gurler N, Cepparulo M, Mendes RE, Castanheira M. Resistance surveillance program report for selected European nations (2011) Diagn Microbiol Infect Dis. 2014;78(4):429–36. doi: 10.1016/j.diagmicrobio.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 33.Tali-Maamar H, Laliam R, Bentchouala C, Touati D, Sababou K, Azrou S, et al. Serotyping and antibiotic susceptibility of Streptococcus pneumoniae strains isolated in Algeria from 2001 to 2010. Med Mal Infect. 2012;42(2):59–65. doi: 10.1016/j.medmal.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 34.Xue L, Yao K, Xie G, Zheng Y, Wang C, Shang Y, et al. Serotype distribution and antimicrobial resistance of Streptococcus pneumoniae isolates that cause invasive disease among Chinese children. Clin Infect Dis. 2010;50(5):741–4. doi: 10.1086/650534. [DOI] [PubMed] [Google Scholar]
- 35.Ma X, Zhao R, Ma Z, Yao K, Yu S, Zheng Y, et al. Serotype distribution and antimicrobial resistance of Streptococcus pneumoniae isolates causing invasive diseases from Shenzhen Children’s Hospital. PLoS One. 2013;8(6) doi: 10.1371/journal.pone.0067507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ataee RA, Habibian S, Mehrabi-Tavana A, Ahmadi Z, Jonaidi N, Salesi M. Determination of vancomycin minimum inhibitory concentration for ceftazidime resistant Streptococcus pneumoniae in Iran. Ann Clin Microbiol Antimicrob. 2014;13:53. doi: 10.1186/s12941-014-0053-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Henriques Normark B, Novak R, Ortqvist A, Kallenius G, Tuomanen E, Normark S. Clinical isolates of Streptococcus pneumoniae that exhibit tolerance of vancomycin. Clin Infect Dis. 2001;32(4):552–8. doi: 10.1086/318697. [DOI] [PubMed] [Google Scholar]
- 38.McCullers JA, English BK, Novak R. Isolation and characterization of vancomycin-tolerant Streptococcus pneumoniae from the cerebrospinal fluid of a patient who developed recrudescent meningitis. J Infect Dis. 2000;181(1):369–73. doi: 10.1086/315216. [DOI] [PubMed] [Google Scholar]
- 39.Sanaei Dashti AA, Karimi A. Nasopharyngeal Carrier Rate of Streptococcus pneumoniae in Children: Serotype Distribution and Antimicrobial Resistance. Arch Iran Med. 2012;15(8):500–3. [PubMed] [Google Scholar]
- 40.Njanpop Lafourcade BM, Sanou O, van der Linden M, Levina N, Karanfil M, Yaro S, et al. Serotyping pneumococcal meningitis cases in the African meningitis belt by use of multiplex PCR with cerebrospinal fluid. J Clin Microbiol. 2010;48(2):612–4. doi: 10.1128/JCM.01402-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.


